Artigo Original
Correspondence address: Marina Morettin
Centro de Pesquisas Audiológicas, Hospital de Reabilitação de Anomalias Craniofaciais, Universidade de São Paulo R. Silvio Marchioni, 3-20, Bauru (SP), Brasil, CEP: 17012-900.
E-mail: mmorettin@usp.br Received on: 08/08/2012
Accepted on: 03/27/2013
Study carried out at the Epidemiology Department, School of Public Health, Universidade de São Paulo – USP – São Paulo (SP), Brazil; Center for Audiological Research, Hospital de Reabilitação de Anomalias Craniofaciais, Universidade de São Paulo – USP – Bauru (SP), Brazil.
(1) Graduate Program (Doctorate) in Public Health, School of Public Health, Universidade de São Paulo – USP – São Paulo (SP), Brazil.
(2) Epidemiology Department, School of Public Health, Universidade de São Paulo – USP – São Paulo (SP), Brazil. (3) Hospital de Reabilitação de Anomalias Craniofaciais, Universidade de São Paulo – USP – Bauru (SP), Brasil. (4) Speech-Language Pathology and Audiology Course, Bauru School of Dentistry, Universidade de São Paulo – USP – Bauru (SP), Brazil.
(5) Speech-Language Pathology and Audiology Department, Bauru School of Dentistry, Universidade de São Paulo – USP; Center for Audiological Research, Hospital de Reabilitação de Anomalias Craniofaciais, Universidade de São Paulo – USP – Bauru (SP), Brazil.
Conlict of interest: nothing to declare.
Descritores
Audição Perda auditiva Implante coclear Criança Classiicação Internacional de Funcionalidade, Incapacidade e Saúde
Disability and Health for monitoring patients using
Cochlear Implants
O uso da Classiicação Internacional de Funcionalidade,
Incapacidade e Saúde para acompanhamento de pacientes
usuários de Implante Coclear
ABSTRACT
Purpose: To characterize the proile of patients with cochlear implant as proposed by the International Classiication of Functioning, Disability and Health for Children and Youth (ICF-CY). Methods: This is a descriptive, cross-sectional retrospective study, which examined 30 medical records of patients using the cochlear implant of Centro de Pesquisas Audiológicas. To characterize the proile of the patients, the ICF-CY was used. Regarding the assessment, researchers relied on procedures performed in clinical routine, besides information registered in the medical record. After reviewing the information, it was related to codes from the ICF-CY; with the addition of a qualiier afterwards. Results: Overall, 55 codes from the ICF were related to the instruments to characterize this population. Regarding the Body Functions ield, most participants did not have disabilities related to reception and expression of oral language and auditory functions, with only written language disabilities being found. These same indings were observed in the Activity and Participation Field. Regarding environmental factors, noise and the non-availability of technology resources to assist in the auditory comprehension of noise were characterized as a barrier, as well as the absence of speech therapy. Conclusion: This study concluded that most of the participating children showed no deiciency in the body functions, with dificulties being only reported in relation to school performance. Environmental factors (noise, non-availability of technological resources, absence of speech therapy) were characterized as a barrier. The need to expand assessments in the clinical routine was also noted.
RESUMO
Objetivo: Caracterizar o peril dos pacientes usuários de Implante Coclear a partir do proposto pela Classiicação Internacional de Funcionalidade, Incapacidade e Saúde para Crianças e Jovens (CIF-CJ). Métodos: Tratou-se de um estudo descritivo, retrospectivo transversal, em que foram analisados 30 prontuários de pacientes usuários de Implante Coclear do Centro de Pesquisas Audiológicas. Para caracterização do peril dos pacientes, foi utilizada a CIF-CJ. Para avaliação, os pesquisadores basearam-se em procedimentos realizados na rotina clínica, além de informações registradas no prontuário. Após a revisão dessas informações, estas foram relacionadas com o código da CIF-CJ, sendo acrescido posteriormente um qualiicador. Resultados: No total, 55 códigos da CIF foram relacionados com os instrumentos para caracterização desta população. Com relação ao domínio Funções do Corpo, a maioria dos participantes não apresentava deiciência quanto aos aspectos relacionados à recepção e expressão da linguagem oral e funções auditivas, sendo apenas encontrada deiciência na linguagem
Marina Morettin1
Maria Regina Alves Cardoso2
Aline Malavasi Delamura3
Julia Speranza Zabeu4
Regina Célia Bortoleto Amantini3
Maria Cecília Bevilacqua5
Keywords
INTRODUCTION
In the ield of intervention in childhood deafness, the cochlear implantation represents the most important advancement in the treatment of children with severe/profound prelingual deafness(1).
By providing adequate electrical stimulation to the auditory nerve, the cochlear implant (CI) enables these children to have access to the sounds of which they were previously deprived(2).
In the Brazilian Sistema Único de Saúde (SUS), this resource was added as part of the procedures in 1993, by Ordinance 126. Two more ordinances came later on, establish-ing the Standards for Registration of Centers for performestablish-ing cochlear implantation, and Indication and the Criteria for Indication and Contraindication of Cochlear Implants(3,4).
Thus, these ordinances established indication and contrain-dication criteria of CI for adults and children, the infrastructure a center needs (to be licensed by SUS), the minimum profes-sional staff and equipment required, the amount of monitoring in each case and the realization of rehabilitation. However, as this type of prosthesis is funded by SUS for a limited group of patients, many questions are raised on the results of the use of this device in children, making the selection and indication process of the CI a complex and multidimensional one(5,6).
In clinical practice, there are countless aspects to be investi-gated in an evaluation. However, it is not always possible to have a multidisciplinary team in charge of services, or to have uniied evaluation models that facilitate the detailed understanding of the child’s or adult’s disability. This may explain why it is possible to observe that evaluations in care services to the population using CI are usually focused on the acoustic beneits, and few describe the effects of the intervention on the functioning of the individual, such as their engagement in social activities, advance-ment in education, psychological aspects related to the disability and social aspects, such as occupational issues.
Considering this situation, the World Health Organization published, in 2001, the International Classification of Functioning, Disability and Health (ICF)(7),which refers to a
new interactive and multidimensional classiication system, whose goal is to establish a common and standardized lan-guage for the description of functioning and disabilities related to health conditions and health-related states, allowing the comparison of data from these conditions between countries, services, and health care sectors, as well as the monitoring of its evolution in time.
With the ICF, the patient’s functionality became the central perspective in health and came to be seen as an asset associated with the health condition, and not merely a consequence of it.
All aspects of the patient experience began to be categorized(8).
Thus, this classiication system consists of four components: Body Functions, Body Structure, Activity and Participation and Environmental Factors(9).
Therefore, the ICF has become a major breakthrough in the classiication of functionalities and disabilities, allowing a variety of uses in the health domain, as well as having im-plications in the use of social security and in the formulation of public policies. It has also being used to meet the needs of research aimed at evaluating the effectiveness of the treatment. It is hoped that it can be applied to a population level in the future, since its use has been restricted to research or speciic services for now(10).
It is a valuable tool to evaluate individuals with hearing impairment. The concepts presented in the ICF portray the multidimensional experience reported by individuals with hearing loss. In clinics, its use allows for obtaining an initial proile of the patients, monitoring their progress, evaluating the therapeutic approach proposed and measuring the disability caused by the different levels of each illness or injury. In short, it involves relating diseases to the quality of life of patients(11).
The use of the ICF framework to evaluate results obtained with implanted children over time may help to evaluate other important aspects in the development of a hearing impaired CI user child, besides those related to auditory function and language, and the interactions between these aspects in the treatment planning.
Furthermore, in the case of CI programs in which the care staff proposed by the SUS ordinances consists of different health professionals, such as doctors, speech-language patholo-gists, psycholopatholo-gists, social workers, among others, the use of a common tool may facilitate the monitoring of the intervention in this population, helping to verify that the outcomes of this rehabilitation program are being achieved. This enables SUS to reorganize and implement their actions, resizing them to accommodate the needs of its audience, further rationalizing the use of resources.
Thus, this study aimed to characterize the proile of CI user patients from the context proposed by the ICF.
METHODS
This is a descriptive, cross-sectional retrospective study, developed in the original institution, in partnership with Centro de Pesquisas Audiológicas (CPA) of Hospital de Reabilitação de Anomalias Craniofaciais of Universidade de São Paulo, campus Bauru, the same place where the participating population of
individuals with hearing loss and CI users was selected, as well as where the collection of data needed for this study took place.
The study was approved by the Research Ethics Committee of the institution of origin – Research Protocol No. 299/2006, on 10/31/2006. All volunteers received an informative letter and signed an informed consent form regarding their participa-tion in the study and the disclosure of the results, according to Resolution 196/96.
Thirty medical records from CI user patients were surveyed, randomly selected according to the following inclusion criteria: being a CI user; being regularly monitored after surgery in the institution’s ambulatory care center (CPA); being between 3 and 18 years of age, of both genders. Medical records relating to patients who did not use the CI for a period greater than 6 months and patients with hypoplasia of the auditory nerve were excluded from the sample.
The sociodemographic and clinical data of the study popu-lation were raised to contextualize the research participants.
To characterize the proile of the CI user patients, the Children and Youth version of the International Classiication of Functioning, Disability and Health (ICF-CY) was used(12).
In the ICF, the information is organized into two parts, each containing two components: functioning and disability (part 1), divided into body functions and structure, activity and participation; and contextual factors (part 2), consisting of environmental and personal factors.
Each of the classiication component/ield (Body Structure, Body Function, Activity and Participation and Environmental Factors) can be described in positive or negative terms. In each component/ield, there are several classiication categories or units, which are expressed by a code to which one or more numerical scales are added, called qualiiers, used to describe the extent or magnitude of the functionality or disability in the category chosen for the study (Chart 1).
In this study, for the assessment of Body Functions, Activities and Participation and Environmental Factors (the ield Body Structure was not included), the researchers were based on procedures performed and protocols applied in the study participants’ follow-up routine, in addition to information available in the registry of the records of the speech-language pathologist and other professionals responsible for the patient’s
care in the CPA, such as social workers and psychologists. After review of the information in medical records (data from the last follow-up visit), each piece of information was related to the ICF-CY code that best represented them, with the addition of a qualiier later on, according to each ield (Body Functions, Activities/Participation and Environmental Factors), that best suited each individual case.
The procedures applied in the clinical routine that supported this evaluation were the following:
• Hearing skills evaluation procedures:
• Free ield audiometry – assesses the audibility threshold.
In this examination, patients are positioned at a distance of 1 m from the speaker at 0 azimuth, and asked not to move their head, signaling every time they listen to sound stimuli, even if it is weak.
• Speech perception test – applied according to the patient’s
age. Thus, for children aged 6 years and 11 months, the Phonemes and Words Recognition Index was ap-plied(13). For children aged 7 years and above, the Words
Recognition Index: Dissyllable List was applied(14).
Besides these, the Meaningful Auditory Integration Scale was applied to assess speech perception in children aged 4 years and above with profound hearing loss(15).
The hearing skills were classiied according to the Hearing Categories that classify the child’s auditory development stage regarding his/her hearing abilities(16). The six Hearing
Categories include: 0 – Unable to detect speech; 1 – Speech detection, however, without differentiating stimuli in their supra-segmental aspects; 2 – Perception standard (able to dif-ferentiate words by their supra-segmental traces); 3 – Starting words identiication (able to differentiate words, in a closed set, based on phonetic information; 4 – Word identiication by means of vowel recognition; 5 – Word identiication by means of consonant recognition; 6 – Word recognition in an open set.
• Language skills evaluation procedures:
• Meaningful Use of Speech Scale (MUSS)(17). It evaluates
the use of oral language by hearing impaired children in their daily lives.
• Observation of oral communication in playful and
directed situations.
Chart 1. Qualifiers from the International Classification of Functioning, Disability and Health used to indicate the extent of change
Qualifiers
Fields Body Functions and
Structure Activities and Participation Environmental Factors
Quantitative definition (%)
0 No problem No difficulty No facilitator/no barrier 0–4
+1 Mild facilitator 5–24
+2 Moderate facilitator 25–49
+3 Substantial facilitator 50–95
+4 Complete facilitator 96–100
1 Mild problem Mild difficulty Mild barrier 5–24
2 Moderate problem Moderate difficulty Moderate barrier 25–49
3 Severe problem Severe difficulty Severe barrier 50–95
4 Complete problem Complete difficulty Complete barrier 96–100
8 Not specified Not specified Not specified
Language skills were classiied into ive language categories that classify the child’s language development stage(18). The
ive language categories include: 1 – This child does not speak and may present undifferentiated vocalization; 2 – This child speaks isolated words; 3 – This child builds two to three ele-ment phrases; 4 – This child builds four- or ive-word phrases and begins to use connecting elements (pronouns, articles, prepositions); 5 – This child builds phrases with over ive words, uses connecting elements, conjugates verbs, uses plurals, etc.
Results analysis methods
The results analysis was performed by the descriptive analysis of the following variables for the description of the study population: gender, age, age at surgery, duration of CI use, hearing category, language category, literacy, education of the mother or guardian, etiology, therapy and socioeconomic status. The results in each ield of the ICF-CY (Body Functions, Activities/Participation and Environmental Factors) were re-ported in percentage, according to the qualiier that is best suited for the population. For the analysis, the data were converted to the statistical software Stata, version 10.0.
RESULTS
The 30 study participants underwent CI surgery at the age of 2 years, with the group being at the age of 10 years (minimum of 6 years and maximum of 18 years old) at the time of evaluation and had 8 years of use of the device, on average.
Data on the sociodemographic aspects of the population showed that 93% of the children attended school, and of those, only two were illiterate at the time of evaluation (Table 1).
Regarding the results focused on etiology, Hearing and Language Categories (Table 2), it was noted that, with respect to the last two aspects, 56.67% of children were in therapy at the time of evaluation, 30% of children have been discharged and 13.33% of children had no access to rehabilitation in their city.
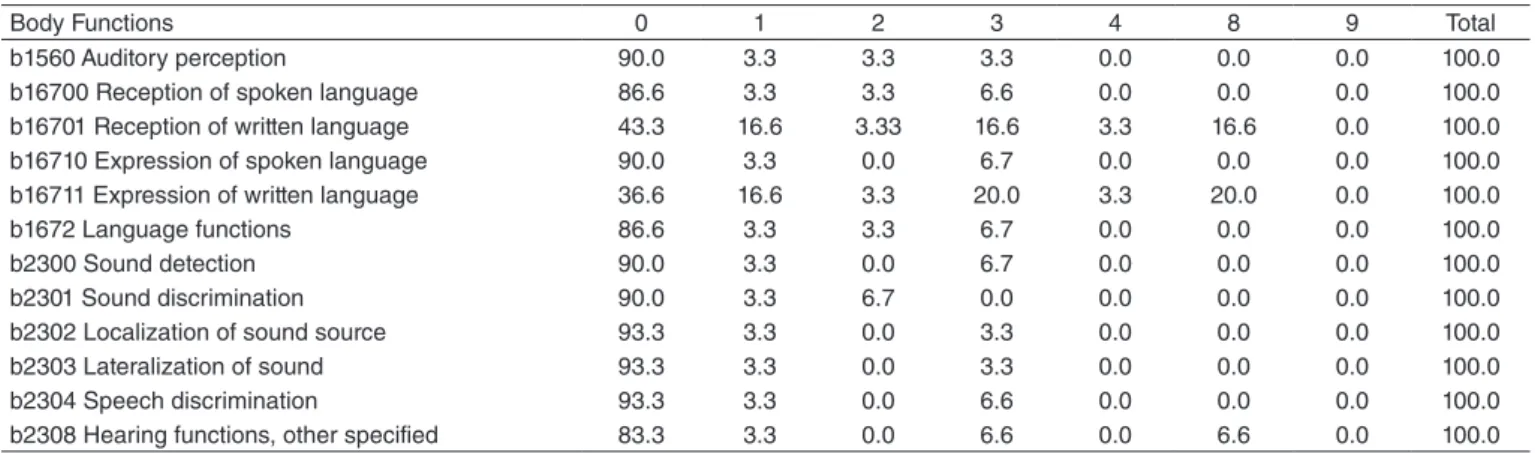
When the results of the evaluations carried out in the clinical routine were related to the ICF-CY, 55 codes were obtained: 12 for the description of Body Function, 36 codes for Activity and Participation and seven for Environmental Factors. No code from the Structure Body ield was included.
After relating the ICF-CY codes, a qualiier was assigned for each child, which represented their performance regarding the selected category.
In the indings regarding the Body Functions ield (Table 3), it was observed that the majority of participants had no disability (qualiier 0) in aspects regarding reception and ex-pression of oral language. As for the detection, discrimination, localization, sound lateralization and speech discrimination auditory functions, most patients had no current disability. It is noteworthy that the ability of auditory comprehension was related to code b2308 (auditory functions, other speciied). Two participants had severe deiciency in detecting sounds, discriminating and understanding speech. Regarding the func-tion related to written language, patients still had disabilities.
There were no speciic data on this skill in the medical re-cords for about 20% of the participants, with no possibility, therefore, of evaluating it.
Codes related to the Production and Quality of Voice (b3100, b3101), Joint Functions (b320) and Fluency of Speech (b3300) were not related, because there was no information in the medical records.
Table 2. Description of the etiology of hearing loss, language and auditory findings of the study population (n=30)
n %
Etiology
Anoxia 3 10.0
High fever 1 3.3
Jaundice 1 3.3
Meningitis 3 10.0
Ototoxicity 1 3.3
Rubella 3 10.0
Congenital rubella 1 3.3
Wanderburg 1 3.3
“No access to information” 16 53.3 Hearing category
1 1 3.3
2 1 3.3
3 0 0.0
4 0 0.0
5 1 3.3
6 27 90.0
Language category
1 0 0.00
2 1 3.5
3 0 0.00
4 8 27.5
5 21 70.0
Total 30 100.0
Table 1. General characterization of the participating population (n=30)
n %
Gender
Female 12 40.0
Male 18 60.0
Socioeconomics
UM-M 2 6.6
M-LM 10 33.3
LM-UL 16 53.3
W-U 2 6.6
Level of education of the mother or guardian
Higher education 7 23.3
Incomplete higher education 14 46.6
Secondary education 4 13.0
Incomplete secondary education 3 10.0 Incomplete middle school 1 3.3 Incomplete primary school 1 3.3
Total 30 100.00
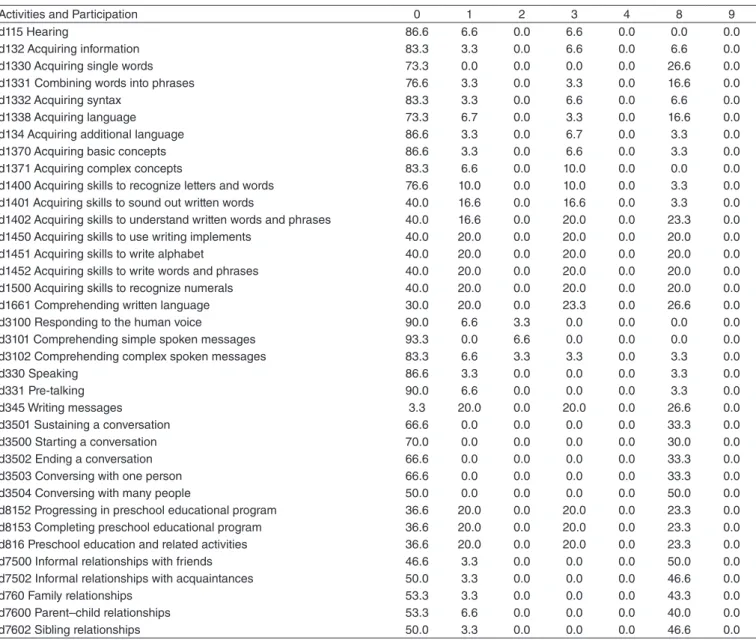
For evaluation of the Activity and Participation ield, 36 codes were selected, and the results regarding the qualiiers in this ield are shown in Table 4.
The children showed dificulties regarding school-related activities. In some cases, it was not possible to characterize aspects of the children’s participation (relationships with friends, family, siblings), due to the absence of information on these aspects in their medical records, as well as data on phone use by these patients (use of communication devices) and communication techniques.
Environmental factors were evaluated according to the orientation on ICF-CY to check the inluence of these factors on people’s performance. They can be qualiied as facilitators or barriers to the patient’s development. In this study, most of the related codes acted as facilitators in the cases of the 30 participating children, and only the codes related to environ-mental noise (e250 Sound and e130 Products and technology for education; in this case, using the frequency modulation system – FM) were considered as a barrier to 86% of children (Table 5). In this case, the non-availability of FM in environ-ments such as the classroom can interfere with the performance of the CI user student.
For 13% of children, not undergoing speech therapy was not considered as a barrier or as a facilitator, as these children did not have access to this service with speech-language pa-thologists (e580 services, systems and health policies, e355 Health professionals).
DISCUSSION
This study aimed to characterize the proile of CI user pa-tients from the context proposed by the ICF-CY(12).
It was found that most CI user children who participated in the study showed no deiciency in the Body Functions regarding auditory and language skills, with the only disability reported being regarding the development of reading and writing skills. The same occurred in the Activities and Participation ields, as many children had dificulties in the school performance evalu-ated by data from medical records. Regarding Environmental factors, noise and non-availability of technological resources
to assist in the auditory comprehension of the noise, such as the FM system, were characterized as a barrier for the majority of the population.
Thus, the ICF-CY helped expand the vision on the develop-ment of the CI user child. The use of this tool, which emphasizes the role of contextual factors in the individual’s welfare, can help professionals from the CI service and the therapist in the treat-ment planning(19) and in the choice of evaluation instruments(20).
As this model recognizes that a complex interaction of contextual factors (environmental and personal) can shape the development of children with hearing loss, we can, through its use, identify which factors inluence the outcomes of children and families(21). In the case of this study, it was found that noise, which
is considered an environmental factor, served as a barrier for most children, interfering with their performance in these situations.
Another relevant factor that was characterized was the dif-iculty of access to therapy. In Brazil, there are few programs that support the (re)habilitation of hearing impaired children, and the detection of sound alone through the CI does not guarantee the development of oral language, because it does not ensure the interpretation of speech sounds. The child needs to be enabled to make use of the perceived sounds and assign them meaning(22). For this reason, society shall not be exempted
from its responsibilities as a provider of effective intervention programs, organized and founded, with the support from com-petent professionals that specialize in the development of oral language with an emphasis on auditory function(23).
Some dificulties were encountered while using the ICF-CY to assess these patients, because, to qualify each of the evalu-ated aspects, there was a need to base on the results of the procedures performed in the last follow-up visit and the records made by health professionals, and the necessary information was often not available, making it dificult to trace the patients’ proile, particularly regarding social aspects. Furthermore, many codes that are essential to the understanding of the whole life perspective of this population, such as aspects related to voice, interactions with people other than family members, use of telephone and communication techniques, such as lip reading, school progression and even data on occupation for older children, were not listed.
Table 3. Distribution (%) of qualifiers related to “Body Functions” field from the International Classification of Functioning, Disability and Health, Children and Youth version on the study population
Body Functions 0 1 2 3 4 8 9 Total
b1560 Auditory perception 90.0 3.3 3.3 3.3 0.0 0.0 0.0 100.0
b16700 Reception of spoken language 86.6 3.3 3.3 6.6 0.0 0.0 0.0 100.0 b16701 Reception of written language 43.3 16.6 3.33 16.6 3.3 16.6 0.0 100.0 b16710 Expression of spoken language 90.0 3.3 0.0 6.7 0.0 0.0 0.0 100.0 b16711 Expression of written language 36.6 16.6 3.3 20.0 3.3 20.0 0.0 100.0
b1672 Language functions 86.6 3.3 3.3 6.7 0.0 0.0 0.0 100.0
b2300 Sound detection 90.0 3.3 0.0 6.7 0.0 0.0 0.0 100.0
In this sense, the evaluation of other aspects of the life of CI users, besides auditory and language skills, can lead to more personalized interventions for this population, thus providing the achievement of better results in all areas of the implant user’s life(10).
The deiciency related to written language and performance regarding school activities among patients draws attention in this study. Although the CI allows greater access to informa-tion and more beneits related to speech percepinforma-tion and oral
Table 4. Distribution (%) of qualifiers related to “Activities and Participation” field from the International Classification of Functioning, Disability and Health, Children and Youth version on the study population
Activities and Participation 0 1 2 3 4 8 9
d115 Hearing 86.6 6.6 0.0 6.6 0.0 0.0 0.0
d132 Acquiring information 83.3 3.3 0.0 6.6 0.0 6.6 0.0
d1330 Acquiring single words 73.3 0.0 0.0 0.0 0.0 26.6 0.0
d1331 Combining words into phrases 76.6 3.3 0.0 3.3 0.0 16.6 0.0
d1332 Acquiring syntax 83.3 3.3 0.0 6.6 0.0 6.6 0.0
d1338 Acquiring language 73.3 6.7 0.0 3.3 0.0 16.6 0.0
d134 Acquiring additional language 86.6 3.3 0.0 6.7 0.0 3.3 0.0
d1370 Acquiring basic concepts 86.6 3.3 0.0 6.6 0.0 3.3 0.0
d1371 Acquiring complex concepts 83.3 6.6 0.0 10.0 0.0 0.0 0.0 d1400 Acquiring skills to recognize letters and words 76.6 10.0 0.0 10.0 0.0 3.3 0.0 d1401 Acquiring skills to sound out written words 40.0 16.6 0.0 16.6 0.0 3.3 0.0 d1402 Acquiring skills to understand written words and phrases 40.0 16.6 0.0 20.0 0.0 23.3 0.0 d1450 Acquiring skills to use writing implements 40.0 20.0 0.0 20.0 0.0 20.0 0.0 d1451 Acquiring skills to write alphabet 40.0 20.0 0.0 20.0 0.0 20.0 0.0 d1452 Acquiring skills to write words and phrases 40.0 20.0 0.0 20.0 0.0 20.0 0.0 d1500 Acquiring skills to recognize numerals 40.0 20.0 0.0 20.0 0.0 20.0 0.0 d1661 Comprehending written language 30.0 20.0 0.0 23.3 0.0 26.6 0.0 d3100 Responding to the human voice 90.0 6.6 3.3 0.0 0.0 0.0 0.0 d3101 Comprehending simple spoken messages 93.3 0.0 6.6 0.0 0.0 0.0 0.0 d3102 Comprehending complex spoken messages 83.3 6.6 3.3 3.3 0.0 3.3 0.0
d330 Speaking 86.6 3.3 0.0 0.0 0.0 3.3 0.0
d331 Pre-talking 90.0 6.6 0.0 0.0 0.0 3.3 0.0
d345 Writing messages 3.3 20.0 0.0 20.0 0.0 26.6 0.0
d3501 Sustaining a conversation 66.6 0.0 0.0 0.0 0.0 33.3 0.0
d3500 Starting a conversation 70.0 0.0 0.0 0.0 0.0 30.0 0.0
d3502 Ending a conversation 66.6 0.0 0.0 0.0 0.0 33.3 0.0
d3503 Conversing with one person 66.6 0.0 0.0 0.0 0.0 33.3 0.0 d3504 Conversing with many people 50.0 0.0 0.0 0.0 0.0 50.0 0.0 d8152 Progressing in preschool educational program 36.6 20.0 0.0 20.0 0.0 23.3 0.0 d8153 Completing preschool educational program 36.6 20.0 0.0 20.0 0.0 23.3 0.0 d816 Preschool education and related activities 36.6 20.0 0.0 20.0 0.0 23.3 0.0 d7500 Informal relationships with friends 46.6 3.3 0.0 0.0 0.0 50.0 0.0 d7502 Informal relationships with acquaintances 50.0 3.3 0.0 0.0 0.0 46.6 0.0
d760 Family relationships 53.3 3.3 0.0 0.0 0.0 43.3 0.0
d7600 Parent–child relationships 53.3 6.6 0.0 0.0 0.0 40.0 0.0
d7602 Sibling relationships 50.0 3.3 0.0 0.0 0.0 46.6 0.0
Table 5. Distribution (%) of qualifiers related to “Environmental Factors” field from the International Classification of Functioning, Disability and Health, Children and Youth version on the study population
Environmental Factors Barrier (B) or Facilitator (F) Qualifiers
0 1 2 3 4 8 9
e125 Products and technologies for
communication (cochlear implant) F 0.0 0.0 0.0 0.0 100.0 0.0 0.0 e130 Products and technologies for
education B 0.0 0.0 0.0 0.0 86.60 13.40 0.0
e250 Sound B 0.0 0.0 0.0 0.0 86.60 13.40 0.0
e310 Immediate family F 0.0 3.3 3.30 0.0 86.60 0.0 0.0
e320 Friends F 0.0 0.0 0.0 0.0 86.60 13.40 0.0
e580 Health services, systems and
policies F 13.0 0.0 0.0 0.0 87.0 0.0 0.0
language in individuals with severe and profound hearing loss, this result shows that greater attention should be given to the de-velopment of reading and writing skills, allowing these patients to achieve similar levels of development to that of their peer listeners. Another issue is the need for better education (training and capacity building) of human resources within the school to receive such children and thus promote their learning(24).
Regarding environmental factors, we observed that most patients had no dificulty in relating to parents and siblings. The environment in which the child lives and the stimulation it receives, especially from their family, are essential for the fostering of their development and play an important role in language acquisition. Therefore, there is a great concern among professionals about how to support parents and guide them as to the conduct regarding the child who received the CI(25).
While social relations are crucial to the children’s develop-ment, many children with hearing loss and CIs have dificul-ties initiating and sustaining relationships with colleagues who have normal hearing(26). For children who go to regular
schools, poor speech intelligibility can increase the feeling of loneliness(27), and this can lead to dificulties in social
integra-tion, becoming a serious concern for parents, educators and mental health professionals. As few studies to date document the area of social welfare on children’s CIs and suggest ways of dealing with these dificulties(28), it is necessary that the
speech-language pathologist consider this aspect in the CI user child’s rehabilitation, identifying risk behaviors and referring them to specialists when needed.
CONCLUSION
This study showed that the majority of the participating CI user children showed no deiciency in Body Functions related to auditory and language skills, with deiciencies being only reported in relation to the development of reading and writing skills. The participating children showed dificulties in school performance evaluated from the data on their medical records, and regarding environmental factors, noise and non-availability of technological resources to assist in the auditory comprehen-sion of noise, such as the FM system, were characterized as a barrier to the majority of the population, as well as the absence of speech therapy.
These results suggest that evaluations in the clinical routine must be expanded regarding the following aspects of CI user patients: reading and writing skills, voice, participation in social activities and veriication of environmental factors, such as im-mediate family, extended family, friends, health professionals and the attitude of people around them.
*MM was responsible for the preparation of the study, data collection and tabulation, and the drafting of the manuscript; MRAC assisted in the preparation and outlining of the study and with the general guidance of the implementation stages, supervision of the data collection and drafting of the manuscript; AMD and JSZ assisted in data collection and tabulation, as well as the drafting of the manuscript; RCBA and MCB assisted in the preparation and outlining the study and in the general guidance of the implementation stages, supervision of the data collection and in drafting the manuscript.
REFERENCES
1. Bevilacqua MC, Costa OA, Nascimento LT, Ventura LMP, Resegue-Coppi MM. Implante coclear: da seleção à reabilitação. In: Berretin-Felix G, Alvarenga KF, Caldana ML, Sant’Ana NC, Santos MJD, Santos PRJ, organizadores. (Re)Habilitação Fonoaudiológica: Avaliação da Eicácia. São José dos Campos: Pulso Editorial; 2009. p. 212-27.
2. Stuchi RF, Nascimento LT, Bevilacqua MC, Brito Neto RV. Linguagem oral de crianças com cinco anos de uso do implante coclear. Pró-Fono. 2007;19(2):167-76
3. Brasil. Ministério da Saúde. Secretaria de Assistência à Saúde. Portaria nº 211, de 8 de Novembro de 1996. Estabelece as normas para Cadastramento de Centros/Núcleos para realização de Implante Coclear e os Critérios de Indicação e Contra-Indicação de Implante Coclear. Brasília: Ministério da Saúde; 1996.
4. Brasil. Ministério da Saúde. Secretaria de Assistência à Saúde. Portaria nº 1.278, de 20 de Outubro de 1999. Aprovar, na forma do Anexo I, os Critérios de Indicação e Contra-Indicação de Implante Coclear e Aprovar, na forma do Anexo II, as Normas para Cadastramento de Centros/ Núcleos para realização de Implante Coclear. Brasília: Ministério da Saúde; 1999.
5. Bevilacqua MC, Costa AO, Moret ALM. Implante coclear em criança. In: Tratado de Otorrinolaringologia da Sociedade Brasileira de Otorrinolaringologia. São Paulo: Roca; 2003. p. 268-77.
6. O’Neill C, O’Donoghue GM, Archbold SM, Nikolopoulos TP, Sach T. Variations in gains in auditory performance from pediatric cochlear implantation. Otol Neurotol. 2002;23(1):44-8.
7. Organização Mundial da Saúde (Brasil). CIF: Classiicação Internacional de Funcionalidade, Incapacidade e Saúde. Centro Colaborador da Organização Mundial da Saúde para a Família de Classificações Internacionais, organizadores; coordenação da tradução – Cassia Maria Buchalla. São Paulo: EDUSP; 2003.
8. Farias N, Buchalla CM. A Classiicação Internacional de Funcionalidade, Incapacidade e Saúde da Organização Mundial da Saúde: Conceitos, Usos e Perspectivas. Rev Bras Epidemiol. 2005;8(2):187-93.
9. Bornman J. The World Health Organization’s terminology and classification: application to severe disability. Disabil Rehabil. 2004;26(3):182-8.
10. Morettin M, Bevilacqua MC, Cardoso MRA. A aplicação da Classiicação Internacional de Funcionalidade, Incapacidade e Saúde (CIF) na Audiologia. Distúrb Comum. 2008;20(3):395-402.
11. Buchalla CM. A Classificação Internacional de Funcionalidade, Incapacidade e Saúde. Acta Fisiátrica. 2003;10(1):29-31.
12. Organização Mundial da Saúde. CIF-CJ: Classiicação Internacional de Funcionalidade, Incapacidade e Saúde: versão para Crianças e Jovens. Centro Colaborador da Organização Mundial da Saúde para a Família de Classiicações Internacionais, org.; coordenação da tradução – Heloisa Ventura Dinubila. São Paulo: EDUSP; 2011.
13. Delgado EMC, Bevilacqua MC. Lista de palavras como procedimento de avaliação da percepção dos sons da fala para crianças deicientes auditivas. Pró-fono. 1999;11:59-64.
14. Lacerda AP. Audiologia Clínica. Rio de Janeiro: Guanabara Koogan; 1976.
15. Castiquini EAT, Bevilacqua MC. Escala de integração auditiva signiicativa: procedimento adaptado para a avaliação da percepção da fala. Rev Soc Bras Fonoaudiologia. 2000;6(1):51-60.
16. Geers AE. Techniques for assessing auditory speech perception and lipreading enhancement in young deaf children. Volta Review. 1994;96(5):85-96.
17. Nascimento LT. Uma proposta de avaliação da linguagem oral [Monograia]. Bauru: Especialização em Audiologia, Universidade de São Paulo; 1997.
19. Palisano RJ. A collaborative model of service delivery for children with movement disorders: a framework for evidence-based decision making. Phys Ther. 2006;86(9):1295-305.
20. Andrade PMO, Ferreira FO, Haase VG. Classiicação Internacional de Funcionalidade, Incapacidade e Saúde (CIF) e o trabalho interdisciplinar no Sistema Único de Saúde (SUS) In:Haase VG, Ferreira FO, Penna F, organizadores. O enfoque biopsicossocial à saúde da criança e do adolescente. Belo Horizonte: COOPMED, 2009. p. 67-88.
21. Fitzpatrick E. A Framework for Research and Practice in Infant Hearing. CJSLPA. 2010;34(1):25-32.
22. Simser J. Parents: the essential partners in the habilitation of children with hearing impairment. Aust J Educ Deaf. 1999;5(1):1-13.
23. Boothroyd A, Geers AE, Moog JS. Practical implications of cochlear implants in children. Ear Hear. 1991;12(4):81-9.
24. Brazorotto JS. Desempenho acadêmico em crianças surdas usuárias de Implante Coclear [Tese]. São Carlos: Universidade Federal de São Carlos; 2002.
25. Preisler G, Ahlström M, Tvingstedt AL. The development of communication and language in deaf preschool children with cochlear implants. Int J Pediatr Otorhinolaryngol. 1997;41(3):263-72.
26. Weisel A, Most T, Efron C. Initiations of social interactions by young hearing impaired preschoolers. J Deaf Stud Deaf Educ. 2005;10(2):161-70. 27. Martin D, Bat- Chava Y, Lalwani A, Waltzman SB. Peer relationships of deaf children with cochlear implants: predictors of peer entry and peer interaction success. J Deaf Stud Deaf Educ. 2011;16(1):108-20. 28. Percy-Smith L, Jensen JH, Cayé-Thomasen P, Thomsen J, Gudman M,