REVISTA
BRASILEIRA
DE
ANESTESIOLOGIA
PublicaçãoOficialdaSociedadeBrasileiradeAnestesiologiawww.sba.com.br
SCIENTIFIC
ARTICLE
Use
of
tranexamic
acid
in
primary
total
knee
replacement:
effects
on
perioperative
blood
loss
Daniel
Volquind
a,b,c,∗,
Remi
Antônio
Zardo
d,
Bruno
Costamilan
Winkler
d,
Bruno
Bertagnolli
Londero
e,
Natália
Zanelatto
e,
Gisele
Perondi
Leichtweis
eaUnidadedeEnsinoMédicoPropedêuticaAnestésicoCirúrgicadaUniversidadedeCaxiasdoSul,CaxiasdoSul,RS,Brazil bSociedadeBrasileiradeAnestesiologia(SBA),RiodeJaneiro,RJ,Brazil
cClínicadeAnestesiologiadeCaxiasdoSul(CAN),CaxiasdoSul,RS,Brazil dHospitalPompeiadeCaxiasdoSul,CaxiasdoSul,RS,Brazil
eUniversidadedeCaxiasdoSul,CaxiasdoSul,RS,Brazil
Received17September2014;accepted4November2014
Availableonline12March2016
KEYWORDS
Anesthesia; Tranexamicacid; Kneeprosthesis; Bleeding; Bloodtransfusion
Abstract
Backgroundandobjectives: Theuseoftranexamicacidinprimarytotalkneereplacement sur-gerieshasbeenthesubjectofconstantstudy.Thestrategiestoreducebleedingareaimedat reducingtheneedforbloodtransfusionduetotherisksinvolved.Inthisstudyweevaluated theuseoftranexamicacidinreducingbleeding,needforbloodtransfusion,andprevalenceof postoperativedeepveinthrombosisinprimarytotalkneereplacement.
Method: 62patientsundergoingprimarytotalkneereplacementwereenrolledinthestudy, fromJune2012toMay2013,andrandomizedtoreceiveasingledoseof2.5gofintravenous tranexamicacid(GroupTA)orsaline(GroupGP),5minbeforeopeningthepneumatic tourni-quet,respectively.Hemoglobin,hematocrit,andbloodlosswererecorded24haftersurgery. Deepveinthrombosiswasinvestigatedduringpatient’shospitalizationand15and30daysafter surgeryinreviewvisits.
Results:Therewasnodemographicdifferencebetweengroups.GroupTAhad13.89%decreased hematocrit(p=0.925)comparedtoplacebo.GroupTAhadadecreaseof12.28%(p=0.898)in hemoglobincomparedtoGroupGP.GroupTAhadameandecreaseof187.35mLinbloodloss (25.32%)compared togroupGP(p=0.027).Thenumberofbloodtransfusionswas higherin GroupGP(p=0.078).Thromboemboliceventswerenotseeninthisstudy.
∗Correspondingauthor.
E-mail:danielvolquind@gmail.com(D.Volquind).
http://dx.doi.org/10.1016/j.bjane.2014.11.004
Conclusion: Tranexamicacidreducedpostoperativebleedingwithoutpromoting thromboem-bolicevents.
© 2015SociedadeBrasileirade Anestesiologia.Publishedby ElsevierEditoraLtda.Allrights reserved.
PALAVRAS-CHAVE
Anestesia;
Ácidotranexâmico; Prótesedojoelho; Sangramento; Transfusãodesangue
Usodoácidotranexâmicoemartroplastiatotalprimáriadejoelho:repercussõesna perdasanguíneaperioperatória
Resumo
Justificativaeobjetivos: O uso do ácido tranexâmico, em cirurgias de artroplastia total primária de joelho, tem sido objeto de constante estudo. Asestratégias para reduc¸ão de sangramentovisamàreduc¸ãodanecessidadedetransfusãodesanguedevidoaosriscosque apresentam.Nesteestudo,propomosaavaliac¸ãodousodoácidotranexâmiconareduc¸ãodo sangramento,nanecessidadedetransfusãodesangueenaprevalênciadetrombose venosa profunda(TVP)pós-operatóriaemartroplastiatotalprimáriadejoelho.
Método: Foram estudados 62 pacientes submetidos à artroplastia primária total de joelho, de junho de 2012 a maio de 2013, randomizados para receber ácido tranexâmico 2,5gendovenoso(grupoAT),emdoseúnica,ousorofisiológico(grupoGP),cincominutosantes daaberturadotorniquetepneumático,respectivamente.Foramfeitasdosagensdehemoglobina e hematócritoe medida aperdasanguínea 24 horas apósa cirurgia.A TVPfoi pesquisada duranteainternac¸ãodopaciente,15e30diasapósacirurgianasconsultasderevisão.
Resultados: Nãohouvediferenc¸asdemográficasentreosgruposestudados.OgrupoGT apre-sentou quedado hematócrito13,89% (p=0,925)comparado como grupo placebo. Ogrupo GTapresentoudiminuic¸ãode12,28%(p=0,898)dahemoglobinacomparadocomogrupoGP. OgrupoGT apresentouuma diminuic¸ãomédiade187,35ml nasperdassanguíneas(25,32%) quandocomparadocomogrupoGP(p=0,027).Onúmerodetransfusõessanguíneasfoimaior nogrupoGP(p=0,078).Eventostromboembólicosnãoforamevidenciadosnesteestudo.
Conclusões: Oácidotranexâmicodiminuiuosangramentopós-operatóriosempromovereventos tromboembólicos.
©2015SociedadeBrasileira deAnestesiologia.PublicadoporElsevierEditoraLtda.Todosos direitosreservados.
Introduction
Theproposaltousetranexamicacidasastrategytoreduce bloodlossinsurgeryofprimarytotalkneereplacementhas been thesubjectofconstantstudy,becauseitisa proce-dure associated withsignificant amounts of bleeding that can reach 20% of the volume in patients with significant comorbidities related to cardiovascular, cerebrovascular, andmetabolicsystems,duetotheepidemiological charac-teristicsofkneeosteoarthritis/arthrosis.1
In thesepatients,blood lossleadingtoaperioperative
anemia promotes high morbidity and mortality.2 Patients
withperioperativeanemiahavealongerhospitalstay
asso-ciatedwithagreaterneedfortheuseofresources,including
blood transfusions, blood products, and admission to the
intensivecareunit.3---5
Strategies for reducing bleeding have been used to
reducetheneedfortransfusionofbloodanditsproductsdue totheassociatedrisks.4 Notonly thetransmissionofviral
andbacterialdiseases,buttheimmunomodulationrelated
to homologous transfusion has been a growing concern,
especiallyasweevidenceanincreaseintheprevalenceof
prosthesesinfections,immunosuppression,andthealready
seenrelationshipofneoplasmsarisinginpatientsreceiving thistypeoftransfusion.4,6---8
Inthisstudy,weproposetoevaluatetheuseof
tranex-amicacidinreducingbleeding,needfortransfusionofblood
andbloodproducts,andprevalenceofpostoperativedeep
venousthrombosisinprimarytotalkneereplacement.
Methods
AfterapprovalbythelocalResearchEthicsCommitteeand
obtaining written informedconsent, 62 patients
undergo-ingprimarytotalkneereplacementduetoosteoarthrosisor
rheumatoidarthritis,fromJune2012toMay2013,were
ran-domizedtoreceiveintravenoustranexamicacid2.5g(Group
TA)asasingledoseorsalinesolution(GroupP)5minbefore
the opening of the pneumatic tourniquet, respectively.
Exclusioncriteriawerepatient’srefusaltoparticipateinthe
study,allergiestodrugs used,changesrelatedto
coagula-tion,useof nonsteroidalanti-inflammatoryor antiplatelet
pregnancy,andprevioushistoryofdeepvenousthrombosis
orpulmonaryembolism.
Randomization was performed using a software: the
http://www.randomizer.orgbythehospitalpharmacist,not participatinginthestudyandconfidentially.Toeachpatient ofbothgroups,a0.9%saline100mLwasgivenwithout iden-tification,withtranexamicacidorsalinesolution.Allstudy
participantswereblindtowhatwasinsidethesaline
solu-tionofferedbythehospitalpharmacy.Anesthetictechnique
wasfreelychosenbytheanesthesiologiststobeappliedto
studyparticipants,aswellasthesurgicaltechnique.Total
kneereplacementwasperformedwithcemented
prosthe-sisusingpneumatictourniquetinflatedwithcompressedair
withpressureof150mmHgabovethesystolicbloodpressure
ofthe patient.All patients receivedprophylaxis for deep
venous thrombosiswithunfractionated heparinat 5000UI
subcutaneouslyevery8hafterthefirstdoseappliedbefore
pneumatictourniquetinflationandusedcompression
stock-ingsonbothlegsduringthesevendaysfollowingsurgery.
Postoperativeblood losswasmeasuredin drainage
sys-tem installed by the surgeon in the surgical wound and
recorded in the first 24h after surgery. Hematocrit and
hemoglobinvalueswere measured 24h after surgery. The
need for blood transfusion was observed in both groups
at24hfollowing surgery.Thecriteriafortransfusionwere
establishedaccordingtotheprotocolusedbythesurgeon:
bleedinggreaterthan20%ofbloodvolumeorpostoperative
hemoglobinlessthan8gdL−1.
Postoperative deep vein thrombosis (DVT) was
inves-tigated through clinical history and physical examination
duringthe patient’s hospitalstay,and Dopplerultrasound
performed withflow analysisin the region withclinically
suspectedDVT.Inthefollow-upvisit,15and30daysafter
surgery,the systematic investigationwasrepeated bythe
surgeon.
Statistical analysis was performed with SPSS software
version22.0.DatawereanalyzedwiththeStudent’st-test
forquantitativevariablesandchi-squaretestforqualitative variables.
Results
Datafrom62patientswereanalyzed,30patientsinplacebo
group (Group P) and 32 in tranexamic acid group (Group
TA), where30.64% (n=19) ofthe patients weremaleand
69.35%(n=43)female.Therewerenodemographic
differ-encesbetweenthetwogroups(Table1).
Table1 Demographicdata.
Groupplacebo
n=30
GroupTA
n=32
p
Age(years) 63.96±4 67.87±5 0.180
Sex
Male 9 10
Female 21 22
Weight(kg) 82.96±3 83.46±11 0.729
ASA
I/II 3/27 0/22 0.212
740.16
552.18
0 200 400 600 800
Group GT (Group GP)
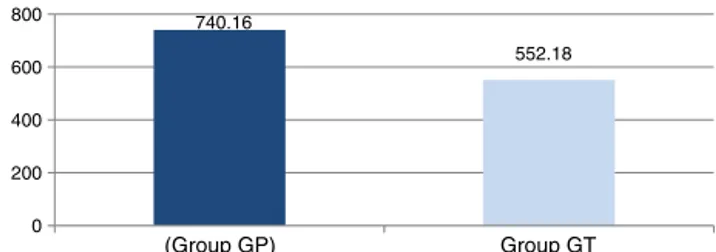
Figure1 Graphshowing thedifference inbleedingvolume (mL)in24hbetweengroups(p=0.027).
Themeaninitialhematocrit(Hti)was40.03±0.006%in groupTAandthemeanfinalhematocrit (Htf)was31.19±
0.017%,demonstratingahematocritreductionof22.08%.In groupP,Htiwas42.08±0.024%andHtf31.27±0.010%, pre-sentingahematocritreductionof25.64%.GroupTAshowed ahematocritfallof13.89%(p=0.925)comparedtoplacebo group.
Meaninitial hemoglobin(Hbi) ingroup TA was13.36±
0.05gdL−1. The mean hemoglobin after the procedure
(Hbf) was 10.52±1.342gdL−1, showing a decrease in Hb
of 21.26% in this groupafter surgery. In group P,Hbi was 13.96±1gdL−1andHbfwas10.57
±0.95gdL−1,showinga
decreaseinHbof24.29%.ThegroupTAshowedadecrease inHbof12.28%(p=0.898)comparedtogroupP.
The mean postoperative bleeding in group TA was 552.81±107mL and in group P it was 740.16 ±205mL. GroupTAshowedameandecreaseofbloodlossof187.35mL (25.32%)comparedtogroupP(p=0.027)(Fig.1).
GroupPneededthedoublepackedredbloodcells(RBC)
unitstransfused(8)comparedtogroupTA(4)(p=0.078).
Deepvenousthrombosiswasnotobservedinbothgroups.
Discussion
The present study showed a reduction in postoperative
bleedinginpatientswhoreceivedtranexamicacidbecause
antifibrinolyticdrugspromotereductionoffibrinolysis. Sur-gicaltraumareleasesthetissueplasminogenactivator(t-PA) andthefibrinolyticsystemisactivated.Thet-PAisthemain
enzymeresponsibleforplasminogenconversiontoplasmin.
Thrombinalsoactivatesfibrinolysisbyvascularendothelium
t-PArelease.9Surgicalstressincreasesplasminreleaseatthe
siteofvasculardamageandamplifiesfibrinolysis.
Tranexamic acid (trans-4-(aminomethyl)cyclohexane
carboxylic acid),whichis asynthetic fibrinolysisinhibitor,
acts throughcompetitiveinhibitionofplasminogen
activa-tioninplasmin,10,11whichresultsinafibrinolysisdelaydue
tonon-plasminformation,bindingtofibrinogenortofibrin
monomersdoesnotoccurandresultsinaclotstabilization.4
The choiceofdrugsforthestudywasbasedonthesafety
profileanditsefficacyreportedintheliterature.
Amongthestrategiestoreduceperioperativebleedingin
kneereplacementthereistheuseofpneumatictourniquet
duringtheperioperativeperiod.12However,thistourniquet
decreases intraoperativeblood loss,butwhendeflatedan
increaseinbleedingisseen,whichisexplainedbythe hyper-fibrinolysisduetoplasminreleasefromthesurgicalbed.13,14
Severalauthorsstudiedtranexamicacidtoestablishits
effect in reducing bleeding and need for transfusion of
However,therewasnoconsensusregardingdoseandtime toadministerthedrugunderstudy.15---17
Orpenetal.reportedasignificantbloodlossreductionof
43.5%(p=0.006)intheimmediatepostoperativeperiodin
thegroupreceiving15mgkg−1intravenoustranexamicacid
at thetimeof cemented kneeprosthesisplacement
com-pared to the group receiving saline solution at the same
time.Therewerenoreportsofdeepveinthrombosisinboth
groups.12
Inastudyofpatientswithhipfracture,theintravenous
administrationoftranexamicacid(15mgkg−1)atthetime
ofskinincisionandrepeated3hlater(totalof30mgkg−1)
reducedtheneedforbloodtransfusion.18
Studying theefficacyofantifibrinolytic,Camarasaused
intravenoustranexamicacidatadoseof10mgkg−1before
deflating the pneumatic tourniquet, and repeated it 3h
after the same intravenous dose and demonstrated a
decreased blood loss in patients undergoing total knee
replacement.19
Recent systematicreviewof randomizedcontrolled
tri-alsconcludedthattheuseoftranexamicacidasableeding
reductionstrategyreducedtheneedforbloodtransfusions
by at least50% anditscomplications, indicating that this
drugreducesbloodlossinatleast300mL----suchfindingsare similartothatfoundbytheauthors.20
Inthisstudy,weusetranexamicacidinequaldose(2.5g)
for all patients, which resulted in a mean of 30mgkg−1
applied5min beforeopeningthe pneumatictourniquetin
rapidinfusion.Astudyofbleedingreductioninsurgeriesin
whichthereis fibrinolysis activationadvocated theuseof
tranexamicaciddosesbetween2and7g.21
Regardinghematocritandhemoglobinlevelsinthisstudy,
althoughtherewasagreaterdecreaseinHbingroupTA,it
wasnot enough torequire blood transfusionaccording to
the protocol adopted bythe surgeon.In the surgical
pro-tocol,patientswhopresentedHb<8gdL−1orpostoperative
bloodloss>20%ofbloodvolumewouldbesubmittedtoblood transfusion.
This approach is consistent with the literature with
regardtolowerthepatient’sexposuretohomologousblood
transfusion.Byusingasimpleprotocol,similartothat
pro-posedbythesurgeoninthepresentstudy,Ballantyneetal.
showeda31%reductioninbloodtransfusionswhenadopted
asatransfusioncriterionaHbof8.5gdL−1comparedtoHb
of11gdL−1.22
Withthesamepurpose,Zadzilkaetal.recommendedas
astrategytoreducepreoperativetransfusionofbloodand
bloodproductstheestablishmentofatolerableHblevelin
ordertoperformthetransfusion.23
Inthisstudy,theneedforunitsofbloodtransfusedwas
double in group P. However, we cannot claim a
relation-shipwithorwithouttheuseoftranexamicacidbecausethe
resultwasnotstatisticallysignificant.
Studieshavereportedthepossibilityofincreased
throm-boembolic events related to the use of tranexamic acid
inpatientsundergoingmediumtomajororthopedic
proce-dures.Thisincreaseisbasedontheeffectsofantifibrinolytic
drugsassociatedwithprolongedbedrestandprothrombotic
activity of the inflammatory response tosurgical trauma.
However,in the present study,in which the drug
prophy-laxiswasused(subcutaneousunfractionatedheparin5000IU
every8h)associatedwithuseofcompressionstockingsfor
sevendaysperioperatively,therewasnoevidenceof
throm-boemboliceventsinbothgroupsofpatients.
A study assessing the efficacy and safetyof increasing
doses of intravenous tranexamic acid (1000mg; 2000mg;
and3000mg)inpatientsundergoingtotalkneereplacement
showednothromboemboliceventsinstudiedgroups.24
Several studies have failed to show an association
betweentheuseoftranexamicacidandtheoccurrenceof
thromboembolicevents.9,13Thelikelyexplanationforthese
findingsliesinthefacttranexamicaciddoesnotaffect
fib-rinolyticactivityonthewallsoftheveinsandpromoteno
prothromboticactivityinthestudiedgroups.13
In this study, we conclude that the use of tranexamic
acidreducespostoperativebleedinginprimarytotalknee
replacement,withtheabsenceofthromboembolicevents.
However,additionalstudiesareneededtoassessitsimpact
ontheneedfortransfusionofbloodandbloodproducts.
Conflicts
of
interest
Theauthorsdeclarenoconflictsofinterest.
Acknowledgements
TheauthorsthankthePharmacyService HospitalPompeia
forthepreparationandrandomizationofthedrugsusedin
thiswork.
References
1.MichelJWP,Schlüter-BrustKU,EyselP.Theepidemiology, eti-ology,diagnosis,and treatmentofosteoarthritisoftheknee. DtschArzteblInt.2010;107:152---62.
2.CarlsonJL,DuffA,BerlinJA,etal.Perioperativeblood trans-fusionandpostoperativemortality.JAMA.1998;279:199---205.
3.BaronDM,HochrieserH,PoschM,etal.Preoperativeanaemia isassociatedwithpoorclinicaloutcomeinnon-cardiacsurgery patients.BrJAnaesth.2014;113:416---23.
4.Hynes M, Calder P,Scott G. The useof tranexamic acid to reduce bloodloss during totalknee arthroplasty. The Knee. 2003;10:375---7.
5.KotzéA,CarterLA,ScallyAJ.Effectofpatientblood manage-mentprogrammeonpreoperativeanaemia,transfusion rate, andoutcomeafterprimaryhipandkneearthroplasty:aquality improvementcycle.BrJAnaesth.2012;108:943---52.
6.Snyder GL,Grinberg S. Effect of anaesthetic technique and otherperioperativefactorsoncancerrecurrence.BrJAnaesth. 2010;105:106---15.
7.WheatleyT,VeitchPS.Effectofbloodtransfusionon postop-erativeimmunocompetence.BrJAnaesth.1997;78:489---92.
8.Garneti N, Field J. Bone bleeding during total hip arthro-plasty after administration of tranexamic acid. J Arth. 2004;19:488---92.
9.JansenJ,AndreicaS,ClaeysM,etal.Useoftranexamicacid for aneffectivebloodconservationstrategyaftertotalknee arthroplasty.BrJAnaesth.1999;83:596---601.
10.MacGillivrayRG,TarabichiSB.Tranexamicacidtoreduceblood lossafterbilateraltotalkneearthroplasty---aprospective, ran-domizeddoubleblindstudy.JArth.2011;26:24---8.
12.OrpenNM,LittleC,WalkerG,etal.Tranexamicacidreduces earlypost-operativebloodlossaftertotalkneearthroplasty: aprospectiverandomisedcontrolledtrialof29patients.The Knee.2006;13:106---10.
13.BenoniG,LethagenS,FredinH.Theeffectoftranexamicacid onlocalandplasmafibrinolysisduringtotalkneearthroplasty. ThrombRes.1997;85:195---206.
14.Tarwala R, DorrLD,GilbertPK,et al.Tourniquet useduring cementationonlyduringtotalkneearthroplasty:arandomized trial.ClinOrthopRelatRes.2014;472:169---74.
15.Charoencholvanich K, Siriwattanasakul P. Tranexamic acid reducesbloodlossandbloodtransfusionafterTKA:a prospec-tive randomized controlled trial. Clin Orthop Relat Res. 2011;469:2874---80.
16.ManiarRN,KumarG,SinghiT,etal.Mosteffectiveregimenof tranexamic acidinkneearthroplasty:aprospective random-ized controlledstudyin240patients.ClinOrthopRelatRes. 2012;470:2605---12.
17.Gandhi R, Evans HMK,Mahomed SR, et al. Tranexamic acid andreductionofbloodlossintotalkneeandhiparthroplasty: ameta-analysis.BMCResNotes.2013;6:184,doi:http://www. biomedcentral.com/1756-0500/6/184.
18.ZuffereyPJ,MiquetM,QuenetS,etal.Tranexamicacidinhip fracturesurgery:arandomizedcontrolledtrial.BrJAnaesth. 2010;104:23---30.
19.Camarasa MA, Ollé G, Serra-Prat M, et al. Efficacy of aminocaproic,tranexamicacidinthecontrolofbleeding dur-ingtotalkneereplacement: arandomizedclinicaltrial. BrJ Anaesth.2006;96:576---82.
20.KagomaYK,CrowtherMA,DouketisJ,etal.Useof antifibri-nolytic therapy toreduce transfusion inpatients undergoing orthopedicsurgery:asystematicreviewofrandomizedtrials. ThrombRes.2009;123:687---96.
21.MannucciPM,LeviM.Preventionandtreatmentofmajorblood loss.NEnglJMed.2007;356:2301---11.
22.Ballantyne A, Walmstey P, Brenkel I. Reduction of blood transfusionratesin unilateraltotalkneearthroplastybythe introductionofasimplebloodtransfusionprotocol.TheKnee. 2003;10:379---84.
23.Zadzilka JD, Stulberg BN. Blood conservation in total knee arthroplasty: hedging your bets. Semin Arthro. 2011;22: 150---2.
24.Poeran J, Rasul R, Suzuki S, et al. Tranexamic acid use and postoperative outcomes in patients undergoing total hip or knee arthroplasty in United States: retrospective analysis of effectiveness and safety. BMJ. 2014;349:g4829,