REVISTA
BRASILEIRA
DE
ANESTESIOLOGIA
OfficialPublicationoftheBrazilianSocietyofAnesthesiologywww.sba.com.br
SCIENTIFIC
ARTICLE
Lidocaine
alleviates
propofol
related
pain
much
better
than
metoprolol
and
nitroglycerin
Asutay
Goktug
a,
Handan
Gulec
b,∗,
Suna
Akin
Takmaz
a,
Esra
Turkyilmaz
c,
Hulya
Basar
aaDepartmentofAnaesthesiology,AnkaraEducationandResearchHospital,Ankara,Turkey bDepartmentofAnaesthesiology,KeciorenEducationandResearchHospital,Ankara,Turkey cDepartmentofAnaesthesiology,ZekaiTahirBurakEducationandResearchHospital,Ankara,Turkey
Received25November2013;accepted2January2014 Availableonline13February2014
KEYWORDS
Propofolpain; Lidocaine; Nitroglycerin; Metoprolol
Abstract
Backgroundandobjectives: Injectionpain afterpropofoladministrationiscommonandmay disturbpatients’comfort.Theaimofthisstudywastocompareeffectivenessofintravenous (iv)nitroglycerin,lidocaineandmetoprololappliedthroughtheveinsonthedorsumofhandor antecubitalveinoneliminatingpropofolinjectionpain.
Method: Therewere147patientsandtheyweregroupedaccordingtotheanalgesic adminis-tered.Metoprolol(n=31,GroupM),lidocaine(n=32,GroupL)andnitroglycerin(n=29,Group N)wereappliedthroughivcatheteratdorsumhandveinorantecubitalvein.Painwas evalu-atedby4pointscale(0---nopain,1---lightpain,2---mildpain,3---severepain)in5,10,15 and20thseconds.ASA,BMI,patientdemographics,educationlevelandtheeffectofpathways forinjectionandlocationofoperationswereanalyzedfortheireffectontotalpainscore.
Results:Therewerenodifferencesbetweenthegroupsintermsoftotalpainscore(p=0.981). Therewere nodifferences intermsoftotalpain scoredepending onASA,education level, locationofoperation.However,lidocainewasmoreeffectivewhencomparedwithmetoprolol (p=0.015)andnitroglycerin(p=0.001)amonggroups.Althoughneitherlidocainenor metopro-lolhadanydifferenceonpainmanagementwhenappliedfromantecubitalordorsalhandvein (p>0.05),nitroglycerininjectionfromantecubitalveinhaddemonstratedstatisticallylower painscores(p=0.001).
Conclusion:We found lidocaine to be the most effective analgesic in decreasing propofol relatedpain.Wethereforesuggestivlidocaineforalleviatingpropofolrelatedpainat opera-tions.
©2014SociedadeBrasileiradeAnestesiologia.PublishedbyElsevier EditoraLtda.Allrights reserved.
∗Correspondingauthor.
E-mail:handandrhandan@yahoo.com.tr(H.Gulec).
0104-0014/$–seefrontmatter©2014SociedadeBrasileiradeAnestesiologia.PublishedbyElsevierEditoraLtda.Allrightsreserved.
PALAVRAS-CHAVE
Dornolocalda injec¸ãodepropofol; Lidocaína;
Nitroglicerina; Metoprolol
Lidocaínaémaiseficazdoquemetoprololenitroglicerinaparaoalíviodador relacionadaàinjec¸ãodepropofol
Resumo
Justificativaeobjetivos: Adornolocaldainjec¸ãoapósaadministrac¸ãodepropofolécomum epodecausardesconfortonospacientes.Oobjetivodesteestudofoicompararaeficáciade nitroglicerina,lidocaínaemetoprolol,aplicadosintravenosamenteatravésdeveiasdodorso dasmãosouantecubitais,paraeliminaradorcausadapelainjec¸ãodepropofol.
Métodos: Foramalocadosemgrupos147pacientesdeacordocomoanalgésicoadministrado: metoprolol(n=31,GrupoM),lidocaína(n=32,GrupoL)enitroglicerina(n=29,GrupoN).Os analgésicosforamaplicadosviacateterintravenosoemveiadodorsodamãoouantecubital.A dorfoiavaliadacomumaescaladequatropontos(0=semdor,1=dorleve,2=dormoderada, 3=dorintensa)nossegundoscinco,10,15e20.Osdadosdemográficosdospacientes,estado físicoASA,IMC,níveldeescolaridade,efeitodasviasdeinjec¸ãoelocaldascirurgiasforam analisadosquantoaseusefeitosnoescoretotaldedor.
Resultados: Nãohouvediferenc¸aentreosgruposemrelac¸ãoaoescoretotaldedor(p=0,981). Nãohouvediferenc¸anoescoretotaldedoremrelac¸ãoaoestadofísicoASA,escolaridadeelocal dacirurgia.Noentanto,lidocaínafoimaiseficazemcomparac¸ãocommetoprolol(p=0,015)e nitroglicerina(p=0,001),nacomparac¸ãoentreosgrupos.Emboralidocaínaemetoprololnão tenhamapresentadodiferenc¸anotratamentodadorquandoaplicadosemveiaantecubitalou dodorsodamão(p>0,05),ainjec¸ãodenitroglicerinaemveiaantecubitalapresentouescores dedorestatisticamentemenores(p=0,001).
Conclusão:Lidocaínamostrou-secomoanalgésicomaiseficazparadiminuiradorrelacionadaà injec¸ãodepropofol.Sugerimos,portanto,lidocaínaIVparaaliviaradorrelacionadaàinjec¸ão depropofolemoperac¸ões.
©2014SociedadeBrasileira deAnestesiologia.PublicadoporElsevierEditoraLtda.Todosos direitosreservados.
Introduction
Propofol is an intravenous agent which is often preferred forsamedaysurgeryandhasshortperiodeffects.Injection painisthemostcommonpainandoneoftheadverseeffects disturbingpatients’comfort.Injectionpainincidencerateis 28---90%foradultsinthecourseofinduction.1,2Various
meth-odsanddrugsaretestedandsuggestedinordertoeliminate
injectionpaincaused by Propofol.Forthis purpose,some
studiesabout injectionspeed ofpropofol,temperatureof
propofol and the vein immensity have been carried
out-fordecreasingpain.Beforepropofolinjection,somedrugs
suchasalfentanyl,tramadol,ketamine,fentanyl,morphine,
meperidine,metoprololandlidocainehave beenusedand
the effectiveness of these drugs on eliminating injection
painhasbeentested.3---10
Althoughtherearemanyresearchesonanalgesiceffects
oftransdermalnitroglycerin,researchesabouteffectiveness
ofnitroglycerin oneliminating propofolinjectionpainare
limited.2Theaimofthisstudywastocompareeffectiveness
ofintravenous (iv)nitroglycerin,lidocaineandmetoprolol
appliedthroughtheveinsonthedorsumofhandon
elimi-natingpropofolinjectionpainandthemainpurposeofthis
studywastoensuresatisfactionofpatients.
Methods
Aftertheapprovalofpatientsandhospitalethics
commit-tee,92patientsattheagesbetween19and70yearshave
been involved intherandomizeddoubleblind methodfor
theresearchplannedinelective conditionsat HM(Health
Ministry) Ankara Training and Research Hospital in
accor-dancewithclassificationgroupIandIIofAmericanSocietyof
Anesthesiologist.Hypertensivepatients,diabeticpatientsor
patientswithanotherneuropathy,patientswhosebodymass
indexis 35kgm−2 orabove,patientswithallergytothese
drugsand withParkinson’sdisease,withthrombophlebitis
storyhavebeenexcludedfromthisresearch.
Routine monitorization including ECG, pulse oximeter
and non-invasive blood pressure have been applied to
patients who have undergone intramuscular (im)
preme-dicationwith50mg meperidine and0.5mg atropineafter
intravenousline(iv) hasbeen openedat thedorsumhand
veinwith20G catheter.Drugs that hadtobeusedin the
researchhavebeenpreparedas2mlintotalandnumbered
byaresearcherindependentfromapplicator.Aftervenous
discharge,tourniquetwereappliedtoarmmanuallyfor45s
and2mgmetoprololto31patientsinGroupM,20mg
lido-caineto32patientsinGroupL,0.25mgnitroglycerinto29
patients in Group N were applied through iv catheter at
dorsumhand vein. Aftertourniquet was loosened up, for
anesthesiainduction2mg/kg propofolwasinjectedwitha
flowof2mlin4s.Theadministrationpathwayswereused
forcomparisonofdifferentanalgesics.
Painduringinjectionwasevaluatedinthe4pointscale
(0---nopain,1---lightpain,2---mildpain,3---severepain)at
5,10,15and20thseconds.Patientsweregroupedaccording
to their education levels as: 1 --- illiterate, 2 --- primary
school,3---secondaryschool,4---highschool,5---university
scorewasdone.ASAclassificationandBMIwerecompared
withtotalpainscoreusingtheabovementionedscale.Inthe
pre-operativeperiod,after propofolinduction andshortly
afterintubation 5minlater,heartrateandbloodpressure
wererecorded.Thefifteenthsecondwasdeterminedasthe
maintimebecausepainfrequencywasobservedinthistime
atmost.Inthatcase,totalpainscoreinsteadofpainscore
measured after injection is more effective in reflecting
satisfactionofpatientsandtotallifequalityscore.Location
ofoperationwasrecordedanditwascomparedwithtotal
painscore.The locationwasnumberedas0--- head---neck
(n=65), 1 ---thorax (n=1),2 --- upperabdomen (n=23),3
--- lower abdomen and pelvis (n=57), 4 --- extremity and
paraspinal area(n=31). The operation at thorax wasnot
included into the evaluation because therewas only one
patient.
ANOVA variance analysis has been used for statistical
analysisoftheresultsanddemographicdataand2testhas
beenusedforcomparisonofgroupsintermsofpain.Because
thedistributionofgroupswasnormal,pulseoximetry,
arte-rial blood pressure and heart rate measurements among
groups were evaluatedaccording to thevariance analysis
andBonferronitest.Ap<0.05wasconsideredsignificant.
Results
The mean age of the patients was 40 years (range,
19---70 years) and the mean BMI (body mass index) was
25.34±3.94kgm−2. There were 81 female and 66 male
patients.Nodifferencewasfoundamongthegroupsinterms
ofdemographicaldatasuchasage,gender,andbodymass
index (p>0.05). Also there were no differences in terms
oftotalpainscoredependingoneducationlevel(p>0.05).
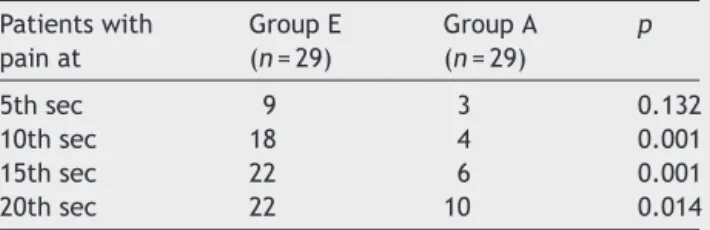
Number of patients withpain according to timeintervals
whileadministrationofanalgesicfromantecubitalareaand
dorsumofhandareshown inTables1 and2.Alsonumber
of patients withpain when lidocaine (n=60), metoprolol
Table1 Numberofpatients withpainaccordingtotime intervals while administration of analgesic from back of hand.
Patientswith painat
GroupL (n=32)
GroupM (n=31)
GroupN (n=29)
p
5thsec 1 5 9 0.052
10thsec 6 9 18 0.023
15thsec 6 11 22 0.001
20thsec 3 14 22 0.001
L,Lidocaine;M,Metoprolol;N,Nitroglycerin.
Table2 Numberofpatients withpainaccordingtotime intervalswhileadministrationofanalgesicfromantecubital area.
Patientswith painat
GroupL (n=29)
GroupM (n=27)
GroupN (n=29)
p
5thsec 0 3 3 0.095
10thsec 0 5 4 0.261
15thsec 2 6 6 0.589
20thsec 0 4 10 0.011
L,Lidocaine;M,Metoprolol;N,Nitroglycerin.
Table 3 Number of patients with pain when Lidocaine (n=60)wasinjectedfromdifferentpathways.
Patientswith painat
GroupE (n=31)
GroupA (n=29)
p
5thsec 1 1 1.0
10thsec 6 6 0.101
15thsec 6 2 0.317
20thsec 3 3 0.228
A,antecubitalarea;E,backofhand.
Table 4 Numberof patients with pain when Metoprolol (n=59)wasinjectedfromdifferentpathways.
Patientswith painat
GroupE (n=32)
GroupA (n=27)
p
5thsec 5 1 0.108
10thsec 3 2 0.463
15thsec 11 6 0.712
20thsec 14 4 0.071
A,antecubitalarea;E,backofhand.
(n=59) and nitroglycerin (n=58) were injected from dif-ferentpathwaysareshowninTables3---5.Althoughneither
lidocainenormetoprololhad anydifferenceonpain
man-agementwhenappliedfromantecubitalordorsalhandvein
(p>0.05),nitroglycerininjectionfromantecubitalveinhad
demonstratedstatisticallylowerpainscores(p=0.001).
Totalpainscoreinwomenwas1.63±2.89andtotalpain
score in men was1.62±2.44. There were no differences
betweenthegroupsintermsoftotalpainscore(p=0.981).
WhenASAIandIIdifferencesaretakenintoconsideration,
therewerenosignificantdifferencesthatexistedamongthe
groupsintermsoftotalpainscore(ASAI=134,ASAII=42)
(p=0.661).ThemeanpainscoresatASA-IandASA-IIpatients
were1.63±2.58and1.42±2.82,respectively.
The total pain score in patients who have undergone
extremityandspinaloperationshasbeenmeasuredhasthe
lowest rate when compared with other locations. There
were no differences among other areas in terms of pain
score.Lidocainewasmore effective whencomparedwith
metoprolol(p=0.015)andnitroglycerin(p=0.001).
Further-more,metoprololwasleasteffectivewhencomparedwith
nitroglycerinintermsoftotalpainscore(p=0.002).Intotal
painscoreevaluation,injectionsinantecubitalareaswere
determinedtobemoreadvantageous(p=0.001).Totalpain
scoreforthegroupincludingpatientswithBMIlowerthan
30,withnormalBMIandhighBMIwas1.40±2.48kgm−2.For
Table5 NumberofpatientswithpainwhenNitroglycerin (n=58)wasinjectedfromdifferentpathways.
Patientswith painat
GroupE (n=29)
GroupA (n=29)
p
5thsec 9 3 0.132
10thsec 18 4 0.001
15thsec 22 6 0.001
20thsec 22 10 0.014
theobesegroup(n=30),thescorewas2.70±3.38kgm−2. The total pain score for obese patients was statistically higher(p=0.016).
Discussion
Because propofol injection causes negative experiences about anesthesiaand restricts comfort of patients, some studieshavebeen carriedouttofindvariousmethods and tools.Thepropofol,whichisaphenol,causesirritationat skin,mucous membranesandintimaoftheveins.11 Direct
endotelial irritation of nerve endings caused by propofol
causessecretionofbradykininbystimulatingkallikrein-kinin
cascadesystem.Thisstatebringsoutinjectionpainby
caus-ing increase in contact of free nerve endings and liquid
phaseofpropofolaswellasvenousdilatationandincrease
ofpermeability.Everydruggivenbeforepropofolinjection
alleviates pain by diluting liquid phaseof propofolwhich
hasanendotheliumirritanteffect.Itisthoughtthatpainis
relatedtoconcentrationofliquidphasealthoughthereisno
certaininformationaboutitsmechanism.12
Paincaused bypropofolinjectionemergesat earlyand
lateperiods.Painatearlyperiodisrelatedtodirecteffectof
propofolandpainatlateperiodisrelatedtolocalsecretion
ofkininogens.Atthepresentday,themostcommonagent
usedfor alleviating propofolinjection pain is lidocaine.10
Scott et al. stated that lidocaine alleviates pain by
sta-bilizing kinincascadewhile Erikssonstated thatthis agent
alleviatespainbydecreasingpHandconcentration.13,14
Propofol,byanindirectactionontheendothelium,
acti-vates the kallikrein-kinin system and releases bradykinin,
therebyproducingvenousdilationandhyperpermeability,
which increases the contact between the aqueous phase
of propofol and free nerve endings, resulting in pain on
injection.15Propofol,whendrawnupinadisposablesyringe,
mayleadtoformationofirritantsandpropofolpain.Ithas
been confirmed that propofol stripsthe siliconelubricant
from the inside barrel of plastic syringes. A reduction in
propofolpainbycoolingitto4◦Candminimizingpropofol
injectionpainis animportantclinicalgoalbecauseitmay
influencethepatient’sperceptionofqualityand
acceptabil-ityofanesthesia.Inconclusion,pretreatmentwithlidocaine
40mg, thiopental 0.25mg/kg, and thiopentone 0.5mg/kg
after manual venous occlusion attenuates propofol pain.
However, pretreatment with thiopental 0.5mg/kg after
manualvenous occlusionwasthemost effective in
atten-uatingpropofol-inducedpain.Wethereforesuggestroutine
pretreatmentwiththiopental0.5mg/kgalongwithmanual
venousocclusionfor1minforpreventionofpainassociated
withpropofolinjection.
Nitroglycerinisacommonlyusedagentintreatmentof
ischemic heart disease.16 Nitroglycerin,a strong
vasodila-tor,ismetabolizedasnitricoxide(NO)incells.NOcauses
intracellular concentration of cylicguanosine
monophos-phate(cGMP)whichleadstopainmodulationincentraland
peripheral nervous system.17 NO,applied topically, shows
anti-inflammatoryandanalgesic effectby blocking
neuro-geniccomponentofinflammatoryedemaandhyperallergy
and inhibits adhesion of neutrophils to endothelium
sur-face. The fact that transdermal nitroglycerin is effective
in paintreatment hasbeen provenwithvariousstudies.18
Transdermal nitroglycerin shows vasodilation effect and
analgesic effectby increasing diffusion of local
anesthet-icsandarrivaltonervetrunk.19Nitroglycerinpomadeshows
analgesiceffectandvasodilatoreffectinveinsizes.20
Nitroglycerinis metabolizedtonitric oxide(NO)inthe
cell.17,21 NO causes increase in the intracellular
concen-trationof, whichproduces painmodulationin thecentral
andperipheralnervoussystem.NOgeneratorsalsoinduce
anti-inflammatoryeffectsandanalgesiabyblocking
hyper-algesia and the neurogenic component of inflammatory
edema by topical application.22 Another possible
mech-anism includes an analgesic effect through the direct
stimulation of peripheral fibers mimicking the actions
of locally appliedacetylcholine.23 Mechanisms mentioned
above, or their combinations, might contribute to the
analgesic effects of nitroglycerin added to lidocaine in
intravenous regional anesthesia. The clinical efficacy of
transdermal nitroglycerin for acute pain relief has been
documentedin several studies.23 Nitroglycerin was found
to be useful for the treatment of shoulder pain and
thrombophlebitis and for enhancing the effect of spinal
sufentanilorneostigmine.22Laurettietal.alsoshowedthat
deliveryofNOdonors(transdermalnitroglycerin)together
with.24
Opioidsmaybeofsignificantbenefitincancerpain
man-agement,delayingmorphinetolerance anddecreasingthe
frequencyofadverseeffectsrelatedtolargedosesofopioid.
Ithasbeenconcludedthat0.25nitroglycerinislesseffective
inalleviatingpropofolinjectionpaincomparedtolidocaine
andmetroprolol.Wehaveconcludedthathigherpainrates
inobesepatientsstemsfromstandardamountof
premedi-cation.Inotherwords,amountofdrugsperkiloislowerin
obesepatients
Nitroglycerinis metabolizedtonitric oxide(NO)inthe
cell.17,21NOcausesanincreaseintheintracellular
concen-trationofcyclicguanosinemonophosphate,whichproduces
pain modulation in the central and peripheral nervous
system.24,17 NO generators also induce anti-inflammatory
effects and analgesia by blocking hyperalgesia and the
neurogenic component of inflammatory edema by
top-ical application.22 Another possible mechanism includes
an analgesic effect through the direct stimulation of
peripheral fibers mimicking the actions of locally applied
acetylcholine.17,23As¸ıketal.havestatedthatpre-treatment
with(iv)metoprololisaseffectiveaslidocaineinalleviating
propofolinjectionpain.10
In conclusion, we found Lidocaine to be the most
effective analgesic in decreasing propofol related pain.
Wetherefore suggest iv Lidocaine for alleviatingpropofol
relatedpainatoperations.However,nitroglycerininjection
intoantecubitalveinshasyieldedlowerlevelsofpropofol
relatedpain. Also we have confirmed that injection pain
isnotrelatedtogenderandeducationlevel.Furthermore,
wefoundthatinjectionpainisrelatedtoobesityandtotal
pain score in obese patients was statistically higher. For
evaluation of total pain score, antecubital area is more
advantageousthanthedorsumofthehand.
Conflict
of
interest
Acknowledgements
The authors thank Ismail Demirkale, MD, for hisvaluable
guidanceandsupportoncompletionofthisarticle.
References
1.LyonsB,LohanD,FlynnC,etal.Modificationofpainon injec-tion of propofol.A comparison of pethidine and lignocaine. Anaesthesia.1996;5:394---5.
2.MangarD,HolakEJ.Tourniquetat50mmHgfollowedby intra-venouslidocainediminisheshandpainassociatedwithpropofol injection.AnesthAnalg.1992;74:250---2.
3.Shimizu T, Inomata S, Kihara S, et al. Rapid injection reducespain oninjectionwithpropofol.EurJ Anaesthesiol. 2005;22:394---6.
4.GrauersA,Liljeroth E,AkesonJ.Propofolinfusionrate does not affect localpain on injection. Acta Anaesthesiol Scand. 2002;46:361---3.
5.Seki S, Sekine R, Aketa K, et al. Induction of anesthesia with propofol injected through a central catheter. Masui. 1999;48:62---6.
6.NathansonMH,GajrajNM,RussellJA.Preventionofinjection ofpropofol:acomparisonoflidocainewithalfentanil.Anesth Analg.1996;82:469---71.
7.WongWH, CheongKF. Roleof tramadol in reducing painon propofolinjection.SingaporeMedJ.2001;42:193---5.
8.BatraYK,AlQattanAR,MarzoukHM,etal.Ketamine pretreat-mentwithvenousocclusionattenuatespainoninjectionwith propofol.EurJAnaesthesiol.2005;22:69---70.
9.PangWW,MokMS,HuangS,etal.Theanalgesiceffectof fen-tanyl,morphine,meperidine,and lidocaineintheperipheral veins:acomparativestudy.AnesthAnalg.1998;86:382---6.
10.As¸ıkI,Yörüko˘gluD,GülayI,etal.Painoninjectionofpropofol; comparisonofmetoprololwithlidocaine.EurJAnaesthesiol. 2003;20:487---9.
11.AmbeshSP,DubeyPK,SinhaPK.Ondansetronpretreatmentto alleviatepainonpropofolinjection:arandomized,controlled, double-blindedstudy.AnesthAnalg.1999;89:197---9.
12.Klement W, Arndt JO. Pain on injection of propofol: effectsofconcentrationand diluent. BrJAnaesth.1991;67: 281---4.
13.ScottRPF, SaundersDA, Norman J. Propofol:clinical strate-giesfor preventing pain on injection. Anaesthesia.1988;43: 492---4.
14.ErikssonM.Prilocainereducesinjectionpaincausedby propo-fol.ActaAnaesthScan.1995;39:210---3.
15.SimJY,LeeSH,ParkDY,etal.Painoninjectionwith microemul-sionpropofol.BrJClinPharmacol.2009;67:316---25.
16.ThomasG,RamwellPW.Nitricoxide,donors,and inhibitors. In:KatzungBG,editor.Basicandclinicalpharmacology.7thed. AppletonandLange:Stamford;1998.p.319---24.
17.LaurettiGR,OliveiraR,ReisMP,etal.Transdermalnitroglycerin enhancesspinal sufentanil postoperative analgesia following orthopedicsurgery.Anesthesiology.1999;90:734---9.
18.Glantz L, Godovic G, Lekar M, et al. Efficacy of transder-malnitroglycerin combinedwith etodolac for thetreatment ofchronic post-thoracotomypain: anopen-label prospective clinicaltrial.JPainSymptomManage.2004;27:277---81.
19.TuranA,WhitePF,KoyuncuO,etal.Transdermalnicotinepatch failed to improve postoperative pain management. Anesth Analg.2008;107:1011---7.
20.KhanlariB,LinderL,HaefeliWE.Localeffectoftransdermal isosorbidedinitrateointmentonhandveindiameter.EurJClin Pharmacol.2001;57:701---4.
21.HashimotoS,KobayashiA.Clinicalpharmacokineticsand phar-macodynamics ofglyceryltrinitrate and its metabolites. Clin Pharmacokinet.2003;42:205---21.
22.Ferreira SH, Lorenzetti BB, Faccioli LH. Blockade of hyper-algesia and neurogenic edema by topical application of nitroglycerin.EurJPharmacol.1992;217:207---9.
23.Duarte IDC,Lorenzetti BB, Ferreira SH. Peripheralanalgesia and activationof thenitricoxide-cyclicGMP pathway.EurJ Pharmacol.1990;186:289---93.