RevBrasAnestesiol.2016;66(1):82---85
REVISTA
BRASILEIRA
DE
ANESTESIOLOGIA
OfficialPublicationoftheBrazilianSocietyofAnesthesiologywww.sba.com.br
CLINICAL
INFORMATION
Continuous
spinal
anaesthesia
with
minimally
invasive
haemodynamic
monitoring
for
surgical
hip
repair
in
two
patients
with
severe
aortic
stenosis
夽
María
Mercedes
López
a,
Emilia
Guasch
a,
Renato
Schiraldi
a,
Genaro
Maggi
a,∗,
Eduardo
Alonso
a,
Fernando
Gilsanz
a,baHospitalUniversitarioLaPaz,Madrid,Spain
bSociedadEspa˜noladeAnestesiologia,ReanimacionyTerapeuticadelDolor,Madrid,Spain
Received5December2012;accepted20March2013
Availableonline11October2013
KEYWORDS
Anaesthetic techniques ---subdural; Measurement techniques---cardiac output
Abstract
Backgroundandobjectives: Aortic stenosisincreases perioperative morbidity andmortality, perioperativeinvasivemonitoringisadvisedforpatientswithanaorticvalvearea<1.0cm2ora
meanaorticvalvegradient>30mmHganditisimportanttoavoidhypotensionandarrhythmias. Wereporttheanaestheticmanagementwithcontinuousspinalanaesthesiaandminimally inva-sivehaemodynamicmonitoringoftwopatientswithsevereaorticstenosisundergoingsurgical hiprepair.
Casereport: Twowomenwithsevere aorticstenosiswerescheduledfor hipfracture repair. Continuousspinalanaesthesiawithminimallyinvasivehaemodynamicmonitoringwasusedfor anaestheticmanagementofboth.Surgery wasperformedsuccessfully aftertwoconsecutive dosesof2mgofisobaricbupivacaine0.5%inoneofthemandfourconsecutivedosesinthe other.Haemodynamicconditionsremainedstablethroughouttheintervention.Vitalsignsand haemodynamicparametersremainedstablethroughoutthetwointerventions.
Conclusion:Ourreportillustratestheuseofcontinuousspinalanaesthesiawithminimally inva-sivehaemodynamicmonitoringasavalidalternativetogeneralorepiduralanaesthesiaintwo patientswithsevereaorticstenosiswhoareundergoinglowerlimbsurgery.However,controlled clinicaltrialswouldberequiredtoestablishthatthistechniqueissafeandeffectiveinthese typeorpatients.
©2013SociedadeBrasileiradeAnestesiologia.PublishedbyElsevier EditoraLtda.Allrights reserved.
夽 ThisstudywascarriedoutatLaPazUniversityHospitalinMadrid,Spain. ∗Correspondingauthor.
E-mails:genaromaggi@hotmail.com,genaromaggi@gmail.com(G.Maggi).
Continuosspinalanaesthesiaforaorticstenosis 83
PALAVRAS-CHAVE
Técnicasanestésicas ---subdural;
Técnicasde
mensurac¸ão---débito cardíaco
Raquianestesiacontínuacommonitorac¸ãohemodinâmicaminimamenteinvasivapara
cirurgiadereparac¸ãodoquadrilemdoispacientescomestenoseaórticagrave
Resumo
Justificativaeobjetivos: Aestenoseaórticaaumentaamorbidadeemortalidadenoperíodo perioperatório.Amonitorac¸ãoinvasivanoperioperatórioérecomendadaparapacientescom áreavalvar<1,0cm2ougradientemédio>30mmHg,alémdeserimportanteevitarahipotensão
earritmias.Relatamosomanejoanestésicocomousoderaquianestesiacontínuaemonitorac¸ão hemodinâmicaminimamenteinvasivaemduaspacientescomestenoseaórticagrave, submeti-dasàcirurgiadereparac¸ãodoquadril.
Relatodecaso: Duaspacientescomestenoseaórticagraveforamprogramadasparacirurgia dereparac¸ãodefraturadequadril.Raquianestesiacontínuacommonitorac¸ãohemodinâmica minimamenteinvasivafoiusadaparaomanejoanestésicodeambasaspacientes.Acirurgia foi realizada comsucesso apósduasdoses consecutivasde 2mg debupivacaínaisobárica a 0,5%emumadaspacientesequatrodosesconsecutivasnaoutra.Ascondic¸õeshemodinâmicas permaneceram estáveisduranteaintervenc¸ão.Ossinaisvitaiseparâmetroshemodinâmicos permaneceramestáveisduranteasduasintervenc¸ões.
Conclusão:Nossorelatodescreveousodaraquianestesiacontínuacommonitorac¸ão hemod-inâmicaminimamenteinvasivacomoumaalternativaválidaparaaanestesiageralouperidural emduaspacientescomestenoseaórticagrave,submetidasàcirurgiademembroinferior. Con-tudo,ensaiosclínicoscontroladossãonecessáriosparaestabelecerqueatécnicaésegurae eficaznessetipodepacientes.
©2013SociedadeBrasileira deAnestesiologia.PublicadoporElsevierEditoraLtda.Todosos direitosreservados.
Introduction
Severe aortic stenosis is defined as an aortic valve area lessthan0.8cm2andatransvalvularpeakgradientgreater than 80mmHg.1 Patients often presented with dyspnoea, angina and syncope on exertion. We can find patients withuncorrectedsevere aorticstenosis submittedto non-cardiacsurgery.Inthesecases,anaestheticconsiderations involve maintenance of sinus rhythm, normal heart rate and intravascular volume, and avoidance of hypotension. Severe hypotension can lead to coronary hypoperfusion and ventricular failure. Central blocks have been tradi-tionally contraindicated in these patients.1 Nevertheless, continuous spinal anaesthesia (CSA) may be of particu-lar interest in patients with severe aortic stenosis, since it allows individualized titration of local anaesthetic and can provide greater haemodynamic stability than single-injection spinal anaesthesia.2---4 CSA has been successfully employed in patients in whom haemodynamic stability is mandatory,asinpatientswithcardiacpathologyundergoing lowerlimbsurgery,5---7orobstetricprocedures.8---9
We report the anaesthetic management with CSA and minimally invasive haemodynamic monitoring of two patientswithsevereaorticstenosisundergoingsurgicalhip repair.
Case
report
Case1
A 92-year-old woman was scheduled for left hip frac-ture repairaftera leftpertrochantericfemurfracture. In
her past medical history we found hypertension, severe aorticstenosisandmoderatemitralregurgitation.Her pre-operative treatment consisted in Eplerenone, Aspirin and Furosemide.Shehadnoknowndrugallergy.
Weperformedanechocardiogrambeforesurgery,which revealedanaorticvalveareaof0.6cm2 andapeakaortic
transvalvulargradientof85.4mmHg,addedtoanejection fractionof63%andadoublemitralimpairment,with mod-eratemitralstenosis andseveremitralregurgitation.ECG showednormalsinusrhythm.
Once in theatre, we monitored the patient with ECG, non-invasiveblood pressure (NIBP) and peripheral oxygen saturation (SO2). Basal values were: NIBP 150/78mmHg;
heart rate (HR) 89bpm, SO2 100%. We inserted an
arte-rial catheter in the left radial artery with the patient awake and slightly sedated using midazolam 0.05mgkg−1
IV and 50g IV fentanyl; we connected the catheter to a Flotrac-VigileoR (Edwards LifeSciences), and measured
continuouslyStroke VolumeIndex(SVI),Cardiac Index(CI) and Stroke Volume Variation (SVV). Basal values were SVI 24mLm2, CI 2Lmin−1m2−1, SVV 8%. After recording
measurements, we positionedthe patient in right lateral decubitus. For the CSA, we used a Micro-Spinolong set (PolymedicR, Temena, France), in which the catheter is
84 M.M.Lópezetal.
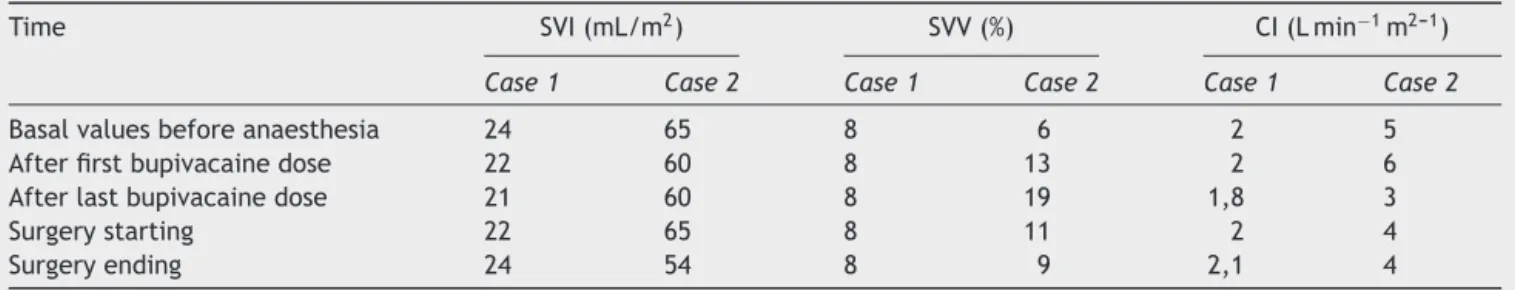
Table1 Minimallyinvasivehaemodynamicparameters.
Time SVI(mL/m2) SVV(%) CI(Lmin−1m2---1)
Case1 Case2 Case1 Case2 Case1 Case2
Basalvaluesbeforeanaesthesia 24 65 8 6 2 5
Afterfirstbupivacainedose 22 60 8 13 2 6
Afterlastbupivacainedose 21 60 8 19 1,8 3
Surgerystarting 22 65 8 11 2 4
Surgeryending 24 54 8 9 2,1 4
SVI,StrokeVolumeIndex;SVV,StrokeVolumeVariation;CI,CardiacIndex.
of thecatheter, we injected 2mg of isobaricbupivacaine 0.5%. Haemodynamic parameters maintained stable and the pin-prick test revealed a sensory block at T10 level. Weinjected afurther2mg-dose 5min later.After achiev-inga T8-sensorylevel of anaesthesia,andpersisting good haemodynamic conditions, we positioned the patient for surgery.
The total procedure lasted 35min. Vital signs and haemodynamicparametersremainedstablethroughoutthe intervention (Table 1). There was no need of additional doses of bupivacaine. We gave the patient a total fluid volume of 500mL of lactated Ringer’s solution, guided by haemodynamic parameters. Estimated blood loss was 300mL.
Aftersurgery,weremovedthespinalcatheter,and trans-ferredthe patienttotherecovery roomawake,alertand comfortable. Postoperative pain was well managed with patient-controlledanalgesiausingmorphine,followinglocal protocols. We discharged the patient from the recovery room 4h later. There was no report of cardiovascular complicationorpost-duralpunctureheadacheduring post-operativestay.
Case2
A 66-year-old woman wasscheduled for lefthip fracture repairafterarightpertrochantericfemurfracture.Shewas asmoker,andapparentlyhadnoothermedicalhistory.She hadnoknowndrugallergy.
In the preoperative physical examination we found a systolic murmur and cardiomegaly on chest X-ray. We decidedtoperformapreoperative cardiacevaluationand anechocardiogram.Thisrevealedasevereaorticstenosis, withanaorticvalveareaof0.45cm2andapeakaortic
gradi-entof95mmHg,addedtoanejectionfractionof73.1%and moderate mitral regurgitation. ECG showed normal sinus rhythm.Thepatientrefusedprevioussymptomsrelatedto aorticstenosis.
Once in theatre, we monitored the patient with ECG, NIBP andperipheral oxygen saturation(SO2). Basal values
were:NIBP168/58mmHg;HR72bpm,SO298%.Weinserted
anarterialcatheterintheleftradialarterywiththepatient awake and slightly sedated using midazolam 0.05mgkg−1
IVand50g IVfentanyl;we connectedthe cathetertoa Flotrac-VigileoR(EdwardsLifeSciences),andmeasured
con-tinuouslySVI,CIandSVV.Basalvalueswere:SVI65mLm2,
CI 5Lmin−1m2---1, SVV 6%. After recording measurements,
wepositionedthepatientinleftlateraldecubitus.Forthe CSA,we useda Micro-Spinolongset (PolymedicR,Temena,
France).Weinsertedthe27Gpencilpointspinalneedleat theL3---L4vertebralinterspaceintothesubarachnoidspace. We removed the needle and advanced the 26G cannula; throughit,weinsertedthe27Gcatheter4cmintode sub-arachnoidspace,andsecuredittoskin.
Werepositionedthepatientsupineand,afteraspiration ofcerebrospinalfluidtoconfirmthecorrectplacementof thecatheter,weinjected2mgofisobaricbupivacaine0.5%. Haemodynamicparametersmaintainedstableandthe pin-pricktestrevealedasensoryblockatL1level.Weinjected threemore2mg-doseevery5minuntilweachieveda T8-sensorylevelofanaesthesia,persistinggoodhaemodynamic conditions.Afterthat,wepositionedthepatientforsurgery. The total procedure lasted 70min. Vital signs and haemodynamicparametersremainedstablethroughoutthe intervention(Table1).Therewasnoneedofadditionaldoses oflocalanaesthetic.Thetotalfluidvolumewasof750mLof lactatedRinger’ssolution,guidedbyhaemodynamic param-eters.Estimatedbloodlosswas400mL.
Spinalcatheterwasremoved aftersurgery.Thepatient was transferred to the recovery room awake, alert and comfortable. Postoperative pain was well managed with patient-controlledanalgesiausingmorphine,followinglocal protocols. The patient was discharged from the recov-ery room4h later. Therewasno reportof cardiovascular complicationorpost-duralpunctureheadacheduring post-operativestay.
Discussion
Thesearethefirstreportedcasesofsevereaorticstenosis with hipfracture, which use CSA with minimally invasive haemodynamicmonitoring.
In patients with severe aortic stenosis, an abrupt decrease in systemic vascular resistance (SVR) could be fatal.Forthisreason,generalanaesthesiaisgenerally rec-ommended,orinanycase,epiduralblockwithprogressive titrationoflocalanaestheticcanbeemployed,toavoid a suddendropinSVR.
Continuosspinalanaesthesiaforaorticstenosis 85
Moreover,haemodynamic alterationsderivedfrom gen-eral anaesthesia’s induction and maintenance and from intubationareavoidedwiththeCSA.
TheuseofCSAinpatientswithaorticstenosis undergo-inglowerlimbsurgeryislimitedinthebibliographytothe reportofclinicalcases,whileitsusewithminimallyinvasive haemodynamic monitoring has not been documentedyet. Fuzierandcolleagues,5andCollardandcolleagues,6showed thatCSAinelderlypatientspresentingsevereaorticstenosis isasafeandeffectivetechniqueforhipsurgery.Fuzierand colleaguesreportedtwocasesoftheuseofCSAforhip frac-turerepair.Theyusedonlystandardmonitoring,andshowed haemodynamicstabilityinbothpatients,usingaperfusionof lowerdoseofphenylephrineinoneofthem.Phenylephrine can restore peripheral resistance rapidly without any  -adrenergicsideeffectsortachycardia,whichcouldbefatal inthesecases.Weconsideredaphenylephrineinfusionafter spinalblockade,butitwasnotnecessaryduetothe main-tainedhaemodynamicconditionsofthepatients.
Collard and colleagues, in two cases of hip surgery as well, used radialand pulmonary arterial catheters for monitoring,andshowedhaemodynamicstabilityduringthe procedure,withoutusingvasoactivedrugs.Nowadays, min-imallyinvasivemonitoringofcardiacoutputcanrepresenta validalternativetoinvasiveprocedureaspulmonaryartery catheterization. Uncalibrated, pressure waveform-based monitors,asFlotrac-VigileoR, have been well validatedin
literature10andtheycanguideintraoperativemanagement needingonlyaradialarterycatheterization.
In literature, there is a disparity in terms of dose of localanaestheticandofintervalsbetweenthem.3---6Inmost studies,dosesranged 2.5---5mgof bupivacaine,witha 15-min interval. We choose a smaller dose (2mg of isobaric bupivacaine)andatitration’sintervalof5min:we consid-eredthat5minwasanadequatetimetoassessthesensory blockade.Moreover,haemodynamicmonitoring allowedus toavoidcardiovascularimpairmentduetoanexcessive sym-patheticblockade.Afterconfirminghaemodynamicstability and sensory level, we repeated the dose, until achieving goodsurgical conditions while maintaininghaemodynamic stability.Furtherstudiesarerequiredtodeterminethebest dosingcriteriaandintervals.Furthermore,CSA withlower dosesoflocalanaesthetic4---5maybeachoiceinothertypes ofpatientinwhichasuddenfallinbloodpressureshouldbe avoided,forexampleparturient,especiallywhenpresenting cardiovasculardiseases.8---9
However,theuseofCSAhaspotentialrisksthatshould not be forgotten. Major bleeding, in addition to the
vasodilatationproducedbytheblockade,couldbefatal.In theseconditionsitcouldleadtoafatalcycleof hypotension-inducedischaemia,ventriculardysfunction,andworsening hypotension.
OurreportillustratestheuseofCSAwithminimally inva-sive haemodynamic monitoring as a valid alternative to generalorepiduralanaesthesiainapatientwithsevere aor-ticstenosiswhoisundergoinglowerlimbsurgery.However, controlledclinicaltrialswouldberequiredtoestablishthat thistechniqueissafeandeffectiveinthesetypeorpatients.
Conflicts
of
interest
Theauthorsdeclarenoconflictsofinterest.
References
1.HerreraA.AorticStenosis.In:HinesRL,MarschallKE,editors. Stoelting’sanesthesiaandco-existingdisease.6thed. Philadel-phia:ElsevierSaunders;2012.p.40---2.
2.Moore JM. Continuous spinal anesthesia. Am J Ther. 2009;16:289---94.
3.Imbelloni LE, Gouveia MA, Cordeiro JA. Continuous spinal anesthesia versus combined spinal epidural block for major orthopedicsurgery:prospectiverandomizedstudy.SaoPaulMed J.2009;127:7---11.
4.Minville V, Fourcade O, GroussetD, et al. Spinal anesthesia usingsingleinjectionsmall-dosebupivacaineversuscontinuous catheterinjectiontechniquesforsurgicalrepairofhipfracture inelderlypatients.AnesthAnalg.2006;102:1559---63.
5.FuzierR,MuratO,GilbertML,etal. Continuousspinal anes-thesiaforfemoralfractureintwopatientswithsevereaortic stenosis.AnnFrAnesthReanim.2006;25:528---31.
6.CollardCD,EappenS,LynchEP,etal.Continuousspinal anaes-thesiawithinvasivehemodynamicmonitoringforsurgicalrepair ofthehipintwopatientswithsevereaorticstenosis.Anesth Analg.1995;81:195---8.
7.TurcJ,LamblinA,KlackF,etal.Pulmonaryhypertensionand femoralneckfracture:interestofcontinuousspinalanesthesia. AnnFrAnesthReanim.2012;31:557---9.
8.Velickovic IA, Leicht CH. Continuous spinal anesthesia for cesarean section in a parturient with severe recurrent peripartum cardiomyopathy. Int J Obstet Anesth. 2004;13: 40---3.
9.Van deVelde M, BudtsW, VandermeerschE, et al. Continu-ousspinalanalgesiaforlaborpaininaparturientwithaortic stenosis.IntJObstetAnesth.2003;12:51---4.