ww w . r e u m a t o l o g i a . c o m . b r
REVISTA
BRASILEIRA
DE
REUMATOLOGIA
Case
report
Clinical
course
of
Behcet’s
disease
in
a
patient
with
delayed
diagnosis
and
radiological
follow-up
of
the
thrombi
with
computed
tomography
angiography:
a
five-year
follow-up
under
immunosuppressive
treatment
Evoluc¸ão
clínica
da
doenc¸a
de
Behc¸et
em
paciente
com
atraso
do
diagnóstico
e
seguimento
radiológico
dos
trombos
com
angiotomografia
computadorizada:
seguimento
por
5
anos
durante
tratamento
imunossupressor
Muhammet
Cinar
a,∗,
Sedat
Yilmaz
a,
Sinan
Akay
b,
Ugur
Bozlar
b,
Ayhan
Dinc
aaGulhaneMilitaryMedicalAcademySchoolofMedicine,DivisionofRheumatology,Ankara,Turkey
bGulhaneMilitaryMedicalAcademySchoolofMedicine,DepartmentofRadiology,Ankara,Turkey
a
r
t
i
c
l
e
i
n
f
o
Articlehistory:
Received23March2013
Accepted12August2013
Availableonline26November2014
Introduction
Behc¸et’s disease (BD) is achronic inflammatory disease of
unknownetiology.1Thediagnosisismadeonthebasisofthe
combinationofclinicalfindings;thereforedelayinthe
diag-nosisisnotrare.Sometimes,cardiovascularandpulmonary
involvementisseenbeforemakingdiagnosisofBD.Such
man-ifestationscanbelife-threateningandfailuretodiagnoseBD
insuchapatientmay beveryserious.2–4 Inthis paper, we
describeaBDpatientdiagnosedlatewithintracardiac,
supe-riorvenacava,andbilateralpulmonaryarterythrombi.We
usedcomputedtomographyangiography(CTA)tostudythe
∗ Correspondingauthor.
E-mail:muhcinar@hotmail.com(M.Cinar).
timecourseofthrombusdevelopmentfromthetimeof
ini-tial diagnosis throughouttreatment. Inthis aspect, this is
the firstreporttouse CTAtoexplorethelong-termcourse
ofintracardiac,superiorvenacava,andbilateralpulmonary
arterythrombi.
Case
report
Ourpatientisawomanwhowas27yearsatthetimeof
diag-nosis,andherfirstcomplaintwasfever,whichcommenced
in January 2005.Prior to that time, shehad suffered from
aphthouslesions,butdidnotseekmedicalattention.InApril
http://dx.doi.org/10.1016/j.rbre.2013.08.004
2255-5021/©2016ElsevierEditoraLtda.ThisisanopenaccessarticleundertheCCBY-NC-NDlicense(http://creativecommons.org/
2005,investigationsrevealed elevatedlevelsofacutephase
reactantsincludingtheerythrocytesedimentationrate(ESR)
andC-reactiveprotein(CRP)level;thesewere 38mm/hand
149mg/L,respectively.Shewasadmittedtohospitalatthat
time.Onphysicalexamination,multipleoralaphthousulcers
were detected. AlthoughBDwas considered in differential
diagnosis,shewasnotdiagnosedwiththediseasebecause
othersignsofBDwereabsent.Infact,shedidhaveagenital
ulcerbut,unfortunately,itwasnotmentionedtothe
physi-cian,andthegenitaliawerenotexamined.Exhaustivetests
seekingtheetiologyofthefeverwereconducted;allof
infec-tious,autoimmune, and malignetiologieswere considered.
Echocardiographyrevealedacardiacmass24mm×13mmin
dimensionsonthelateralwalloftherightventricularcavity.
This was confirmed by cardiac magnetic resonance
imag-ing (MRI); a soft tissue mass 25mm×40mm×40mm was
evident in the right ventricular cavity. The main features
of this soft tissue mass were its partially moving
charac-ter during systole and diastole, iso-hypointense according
to the myocardial tissue and without contrast
enhance-ment.Acardiacthrombuswasinitiallysuspected.Abiopsy
was performed, but it was non-diagnostic. Subsequently,
thepatientexperiencedherfirst episodesofpleuriticchest
painandhemoptysis.Lungventilation/perfusionscintigraphy
wasperformed;perfusionlossinmultiplesegmentsofboth
lungswasevident.Possiblefociofthrombosisandcausesof
thrombophiliaweresought.Shewasheterozygousforthe
pro-thrombinG-A20210mutation,butneithertheVLeidennor
theMTHFRgenewasmutated.Theactivatedpartial
thrombo-plastintime,andthelevelsoflupusanticoagulant,proteinC,
proteinS,anti-thrombinIII,anticardiolipinantibodies,
anti-beta2-glycoprotein1antibodies,andhomocysteinewereall
normal.
Onemonthlater,therightventricularmasswasbiopsied
oncemoreand foundtocontainonlynormalheartmuscle
fibersandadiposetissue.Hemoptysisre-occurredafterbiopsy
andpersistedforabout1week.PulmonaryCTAwasthen
per-formed, and ahypodense filling defect was evident inthe
rightventricleandrightpulmonaryartery(Fig.1A1andB1).
Therefore,anticoagulanttherapy(low-molecularweight
hep-arinfollowedbywarfarin)wascommenced.
InSeptember2005,whilestillonanticoagulanttherapy,the
patientwashospitalized withfever,cough,neckand facial
swelling,dyspnea,andpalpitations.Onphysicalexamination,
shehadfever(38.5◦C),bilateraljugularvenousdistention,face
and neck edema, osteofolliculitis, and erythema nodosum
onthe right pretibial region. Inaddition, two genital ulcer
scarsandoralaphthaewereobserved.Humanleukocyte
anti-gen B51 test was positive and pathergy test was negative,
sothediagnosisofBDwasmade.PulmonaryCTAwas
per-formedagain.Theintracardiacthrombus(ICT)notedearlier
remained,butnow,dilatationsof2cmoftheascendingand
2.5cm of the descending branches ofthe right pulmonary
arterywereevident,togetherwithadilatationof3cmofthe
descendingbranchoftheleftpulmonaryartery.Alldilatations
were associatedwiththe presenceofmuralthrombi. Also,
neithertherightbrachiocephalicveinnorthesuperiorvena
cavacouldbevisualizedbecauseofthrombosis.Theclinical
findingsthatdevelopedoverthe9-monthperiodpriorto
sub-sequenttreatmentareshowninchronologicalorder(Table1).
First, warfarin therapywasdiscontinuedbecause it was
possiblethatbothapulmonaryarterialaneurysmand
arteri-tiswerepresent.Methylprednisolone(1g/dayfor3days)was
administered,followedby1mg/kg/dayoforalprednisolone.
Acyclophosphamide(CYC)pulseof1gwasstartedand
con-tinuedmonthlythereafter.Prednisolonewastapered4weeks
later.Symptoms wererelieved,and boththeCRPlevel and
theESRfelltonormalranges.Hemoptysisgraduallydecreased
andthendisappeared.
In November2005, thepatient wasre-evaluatedby
pul-monaryCTA.Thrombipersistedintheintracardiacregion,the
superior venacava (Fig.1D2) and bothpulmonaryarteries.
Multiplecollateralintercostalveins,whichdraintheazygos
vein, were serving todrain theupper extremities.A filling
defectwasobservedinthedescendingbranchoftheleft
pul-monaryartery(Fig.1C2).Thiscreatedadilatationinthevessel
wall,whichwasassociatedwithminimalintraluminal
con-trastenhancement.However,thiswasnotconsideredtobe
ananeurysm.InSeptember2005,thereportofapulmonary
arteryaneurysmwasreviewedandre-classifiedaswall
dilata-tioncausedbyanintraluminalthrombus.
Elevenmonthslater,whilestillundergoingmonthlyCYC
treatment,feverwithchillsre-occurredassociatedwithan
ele-vatedESRandCRPlevel(37mm/hand51mg/L,respectively).
Therefore,interferon-alpha(5MUthreetimesperweek)was
addedtotherapyandthedoseofprednisolonewasincreased
to 1mg/kg/day. The patientreceived atotal of15g ofCYC
overan18-monthperiod.Interferontherapywascontinuedfor
approximately11months.Next,azathioprine150mg/dayand
acetylsalicylicacid100mg/daywerecommenced.Atthetime
ofwriting,thepatientremainsonthistreatment,andthesigns
andsymptomspreviouslyreportedhavenotre-appeared.
PulmonaryCTAwasusedtofollow-upthethrombiinthe
intracardiacregion,thepulmonaryarteries,andthesuperior
venacava.Thethrombusintherightventriclehaddecreased
insizeby2008(Fig.1A2).In2010,thus5yearsafterinitialCTA,
thesizeoftherightventricularthrombus(andthecalcificpart
thereof)hadbecomefurtherreduced(Fig.1A3).Thethrombus
inthepulmonaryarteryremainedvisibleontheCTAimagesin
2008and2010.Incomparisonwiththescanperformedin2005,
CTArevealedthatthethrombiintherightintermediatelobar
pulmonaryartery(Fig.1B1–B3)andintheleftinferiorlobar
pulmonaryartery(Fig.1C1–C3)decreasedinsizeovertime.In
theCTAscanscarriedoutin2008and2010,thrombosisinthe
superiorvenacavapersistedunchangedinthecranialsection
oftheazygosdrainage(Fig.1D2–D4). Nonewthrombiwere
notedonfollow-uppulmonaryCTA.Currently,noclinicalor
laboratoryevidenceindicatesthepresenceofactivedisease.
Discussion
WereportaBDpatientwithseriouscomplicationsincluding
cardiacandvascularinvolvement.Wedescribeclinical
find-ingspriortoclinicaldiagnosis(thusbeforetreatment)anduse
ofCTAtofollow-upthrombiover5yearsoftreatment.
TheclinicalcourseofBDisnotablymoresevereinmales.
Severecomplicationssuchasvascular,neurologicaland
pul-monaryinvolvementaswellasmortalityaremostlyrelated
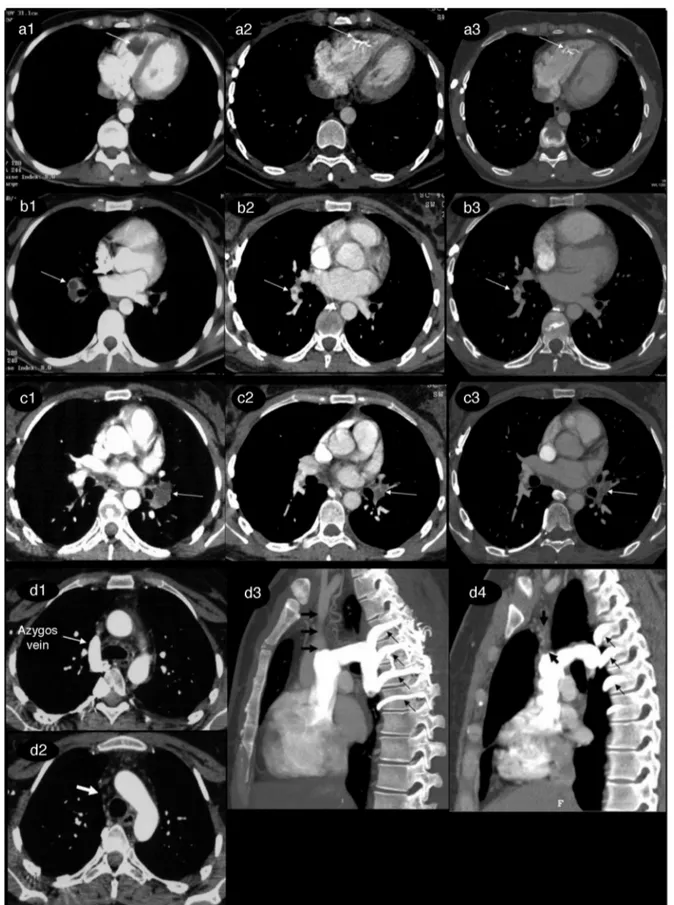
Fig.1–Five-yearcomputedtomographyangiography(CTA)follow-upofthrombiintheintracardiacregion,thesuperior venacava,andbothpulmonaryarteries.
In2005(A1),aCTAscanrevealedalargehypodensethrombusintherightventricle(arrow).In2008(A2),thethrombus decreasedinsizeandwaspartlycalcified,andsuchshrinkagecontinuedto2010(A3).
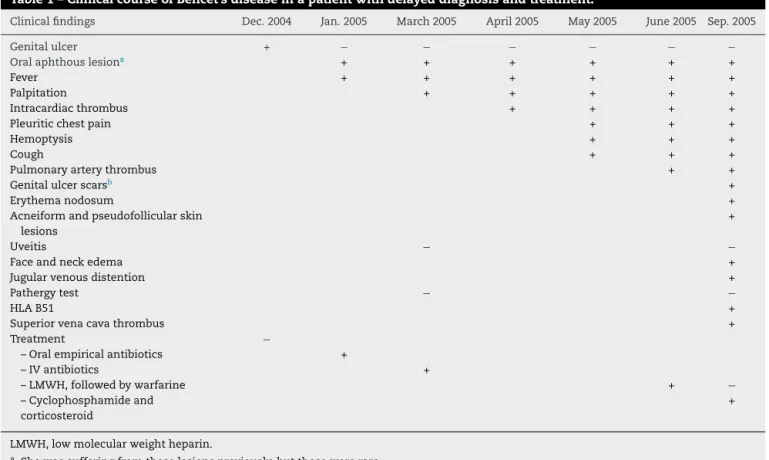
Table1–ClinicalcourseofBehcet’sdiseaseinapatientwithdelayeddiagnosisandtreatment.
Clinicalfindings Dec.2004 Jan.2005 March2005 April2005 May2005 June2005 Sep.2005
Genitalulcer + − − − − − −
Oralaphthouslesiona + + + + + +
Fever + + + + + +
Palpitation + + + + +
Intracardiacthrombus + + + +
Pleuriticchestpain + + +
Hemoptysis + + +
Cough + + +
Pulmonaryarterythrombus + +
Genitalulcerscarsb +
Erythemanodosum +
Acneiformandpseudofollicularskin lesions
+
Uveitis − −
Faceandneckedema +
Jugularvenousdistention +
Pathergytest − −
HLAB51 +
Superiorvenacavathrombus +
Treatment −
–Oralempiricalantibiotics +
–IVantibiotics +
–LMWH,followedbywarfarine + −
–Cyclophosphamideand corticosteroid
+
LMWH,lowmolecularweightheparin.
a Shewassufferingfromtheselesionspreviously,butthosewererare.
b Notexaminedbythephysicianpreviously.
developed during diagnostic evaluation were not fatal. It
remains poorlyknown why females withsevere
complica-tions suffer less mortality than males. As a mechanism,
estrogensmay suppress pro-inflammatory activities ofthe
vascularendotheliumandneutrophils.6Alternatively,
testos-teronemay augment neutrophil functionality,especially in
males.7
Thrombophlebitisandmajorvesselthrombosisare
com-monmanifestationsofvascularinvolvementinBDpatients,
whereasICTisextremelyrare.1Asinourcase,pulmonaryand
cardiaccomplicationsfrequentlyco-exist.1,8Fever,
hemopty-sis,dyspneaandcougharecommonpresentingsymptoms.8
The frequencies of such complications may be
underesti-matedbecausetheclinicalpresentationofICTisnonspecific
inmostpatients.
In differential diagnosis of BD with venous
thrombo-sis and pulmonary involvement, Hughes–Stovin Syndrome
(HSS) should be considered. The clinical, radiological, and
histopathologicalfindingsofHSSandBDoverlapsignificantly.
HSSisaveryraredisordercharacterizedbythrombophlebitis
andbythepresenceofmultiplepulmonaryand/orbronchial
aneurysms. HSS patients usuallypresent with cough,
dys-pnea,fever,chestpainandhemoptysis;thesesymptomsare
also evidentinBD patients. Specifically, the extentof
pul-monaryinvolvementisoftenidenticalinpatientswiththese
diseases.Indeed,HSShasbeenconsideredtobeavariantof
BDoranincompleteformofthedisease.However,findings
associatedspecificallywithBDincluderecurrentgenital
ulcer-ation,eyelesions,skinlesions,iritis,arthralgiaandapositive
pathergytest;thesehelptodistinguishBDfromHSS.9
ThrombophilicfactorsareexpressedinsomeBDpatients
and maycontributetothrombus formation.Inour patient,
heterozygousmutationofprothrombinG-A20210genewas
detected.Importantly,ICThasbeenreportedtobeassociated
withdeepveinthrombosisandthrombosisofthevenacava
in50%and22%ofBDcases,respectively.10Wefoundno
evi-denceofdeepveinthrombosisonDopplerultrasonography.
In patientswithICT associatedwithBD, thepresenceofa
pulmonaryembolismand/orthrombusshouldbeinvestigated
evenifvenousthrombosiscannotbedetected.
In2005(C1),hypodensefillingdefectswereevidentintheleftinferiorlobarpulmonaryartery.In2008(C2)and2010(C3),a thrombuswasevidentinthisregionbutbecameprogressivelysmallerinsize.
In2005(D1,D2),thrombosiswasevidentinthesuperiorvenacava(thickwhitearrow),andtheupperextremitiesdrainedto theVCSviaazygosvein(thinwhitearrow).In2008(D3),coronalCTAimagingrevealedthrombosisinthesuperiorvena
cava(thickblackarrow).TheupperextremitiesdrainedtotheVCSviathecollateralcirculationandtheintercostalveins
Associationofathromboticsuperiorvenacavasyndrome
withICTisnotcommon inBDpatients. However,the
inci-denceofpulmonaryembolismand/orthrombusishighinBD
patientswithICT.1,8 Thepresenceofall ofICT, thrombotic
superiorvenacavasyndrome,andapulmonaryartery
throm-bus/embolism,isextremelyrareinBDpatients;onlyfivecases
(includingthepresentcase)havebeendescribedinthe
litera-ture.Itissometimeshardtoechocardiographicallydistinguish
betweenICT,vegetationsandtumors.However,such
distinc-tionsare important,becausethe treatmentsand prognoses
differ.ComputedtomographyandMRImightbebetter
meth-odsforinvestigatingtheextensionoftheinvolvements,asin
ourcase.1,8 Also,althoughbiopsiesofthemassintheright
ventricularcavitywerenotdiagnosticforourpatient,these
didallowustoexcludemyxoma,endomyocardialfibrosis,and
endocarditis.11
Hemoptysisandfeverarethemostcommonsymptomsof
pulmonaryartery involvementinBD.12 Hemoptysiscan be
causedbypulmonaryaneurysmsand/orpulmonaryarteritis.
Inourcase,noaneurysmwasdetected,andwethusconsider
that the hemoptysis was caused by pulmonary arteritis.
Confirmationofthe causeofhemoptysis inaBDpatientis
essential to guide the choice of appropriate treatment.11
Hemoptysis caused us to discontinue anticoagulant
therapy.
RegardlessofthesiteoforganinvolvementinBD,theaimof
treatmentistopreventirreversibledamagethatoccurs
prin-cipallyatearlystagesofthedisease.Thus,earlydiagnosisis
important.11Inourcase,diagnosiswasmadeapproximately
9 months after symptom onset; this delayed initiation of
immunosuppressivetherapy.Noconsensushasyetemerged
onthemanagementofmajorvesseldisease(withthrombi)
and ICT in BD patients.13 Various treatment modalities
including surgery, immunosuppressiveand anticoagulation
medications,antiplatelettreatments,andthrombolytic
ther-apyhave been used.10 However,no randomized controlled
studyhasassessedtheefficacyofthevarioustherapeutic
regi-mens,andcurrentrecommendationsarebasedononlypartial
consensusorobservationalstudies.
Intravenousthrombolytictherapymightbeconsideredfor
BDpatientswithICTandwidespreadthrombibutwithout
pul-monaryarteryaneurysms.8Itisimportanttoemphasizethat
ifapulmonaryembolisminsuspectedinaBDpatient,neither
anticoagulantnorthrombolytictreatmentshouldcommence
before CTA scanning confirms that aneurysms are absent;
suchtreatmentwouldbeassociatedwithahighriskof
hem-orrhageifaneurysmswerepresent.Theformofpulmonary
artery occlusion seen in BD patients differs from classic
pulmonaryembolismsbecausethe BDocclusionsrepresent
principallyinsituthrombicomplicatingunderlyingvasculitis,
whichmayalsoresultininfarction,hemorrhage,hemoptysis,
andformationofpulmonaryarteryaneurysms.8,14As
hemop-tysiswasevident,andasitwaspossiblethatinsituthrombosis
waspresentinthepulmonaryarteries,weescheweduseof
thrombolytictherapy.
Aftersurgical removalof ICT, thrombus recursin some
BD patients despite prescription of heparin therapy. This
emphasizes the risk that BDcan be worsened bysurgery.
Therefore, to avoid surgery, immunosuppressive agents
shouldbegiven.10,13,15,16High-dosemethylprednisoloneand
CYC should be the treatment of choice. Interferon alpha
shouldbegivenifsymptomsdonotresolvequickly.11,15,17
Weinitiallyusedpulsemethylprednisoloneandcontinued
withmonthlyCYC(15ginall),and1mg/kg/dayprednisolone.
Elevenmonthslater,interferonalphawasaddedbecauseof
recurrence of fever and hemoptysis; this was given for 11
months.Wethencontinuedwithazathioprine.
Anotablefeatureofthiscasereportisthatcomplications
did not completely disappear despite immunosuppressive
therapy(Fig.1A–D).Corticosteroidsandimmunosuppressive
drugsmaynonethelessbeverybeneficial,particularlyifgiven
atanearlystageofdevelopmentofcomplications,thusbefore
irreversibledamagedevelops.10,13
In conclusion,use ofthe non-invasiveCTAtechniqueis
valuableindiagnosisandfollow-upofBDpatientswith
intrac-ardiacandmajorvascularthrombi.WesuggestthatBDshould
bekeptinmindupondifferentialdiagnosisofpatientswith
ICT andfever.Familiarity withthe radiologicaland clinical
characteristicsofBDisessentialtoensureaccurateearly
diag-nosisandprompttreatment.
Conflicts
of
interest
Theauthorsdeclarenoconflictsofinterest.
r
e
f
e
r
e
n
c
e
s
1.KajiyaT,AnanR,KamekoM,MizukamiN,MinagoeS,
HamasakiS,etal.Intracardiacthrombus,superiorvenacava
syndrome,andpulmonaryembolisminapatientwith
Behcet’sdisease:acasereportandliteraturereview.Heart
Vessels.2007;22:278–83.
2.CoccoG,GasparyanAY.Behcet’sdisease:aninsightfroma
cardiologist’spointofview.OpenCardiovascMedJ.
2010;4:63–70.
3.VivanteA,BujanoverY,JacobsonJ,PadehS,BerkunY.
Intracardiacthrombusandpulmonaryaneurysmsinan
adolescentwithBehcetdisease.RheumatolInt.2009;29:575–7.
4.ChaeEJ,DoKH,SeoJB,ParkSH,KangJW,JangYM,etal.
RadiologicandclinicalfindingsofBehcetdisease:
comprehensivereviewofmultisystemicinvolvement.
Radiographics.2008;28:e31.
5.YaziciH,FreskoI,YurdakulS.Behcet’ssyndrome:disease
manifestations,management,andadvancesintreatment.
NatClinPractRheumatol.2007;3:148–55.
6.MiyamotoN,MandaiM,SuzumaI,SuzumaK,KobayashiK,
HondaY.Estrogenprotectsagainstcellularinfiltrationby
reducingtheexpressionsofE-selectinandIL-6in
endotoxin-induceduveitis.JImmunol.1999;163:374–9.
7.YavuzS,OzilhanG,ElbirY,TolunayA,Eksioglu-DemiralpE,
DireskeneliH.Activationofneutrophilsbytestosteronein
Behcet’sdisease.ClinExpRheumatol.2007;25:S46–51.
8.MogulkocN,BurgessMI,BishopPW.Intracardiacthrombusin
Behcet’sdisease:asystematicreview.Chest.2000;118:479–87.
9.KhalidU,SaleemT.Hughes–Stovinsyndrome.OrphanetJ
RareDis.2011;13:6–15.
10.HoumanM,KsontiniI,BenGhorbelI,LamloumM,BrahamA,
MnifE,etal.Associationofrightheartthrombosis,
endomyocardialfibrosis,andpulmonaryarteryaneurysmin
11.CalamiaKT,KaklamanisPG.Behcet’sdisease:recent
advancesinearlydiagnosisandeffectivetreatment.Curr
RheumatolRep.2008;10:349–55.
12.UzunO,AkpolatT,ErkanL.Pulmonaryvasculitisinbehcet
disease:acumulativeanalysis.Chest.2005;127:2243–53.
13.HatemiG,SilmanA,BangD,BodaghiB,ChamberlainAM,Gul
A,etal.ManagementofBehcetdisease:asystematic
literaturereviewfortheEuropeanLeagueAgainst
Rheumatismevidence-basedrecommendationsforthe
managementofBehcetdisease.AnnRheumDis.
2009;68:1528–34.
14.PigaM,PuchadesF,MayoI,D’CruzD.Successfulthrombolytic
therapyforrecurrentrightventricularthrombosisinBehc¸et’s
disease.ClinExpRheumatol.2010;28:S76–8.
15.KanekoY,TanakaK,YoshizawaA,YasuokaH,SuwaA,Satoh
T,etal.Successfultreatmentofrecurrentintracardiac
thrombusinBehcet’sdiseasewithimmunosuppressive
therapy.ClinExpRheumatol.2005;23:885–7.
16.TürsenU,UlubasB,KayaTI,PekdemirtH,Ikizo ˘gluG.Cardiac
complicationsinBehcet’sdisease.ClinExpDermatol.
2002;27:651–3.
17.HamuryudanV,ErT,SeyahiE,AkmanC,TüzünH,FreskoI,
etal.PulmonaryarteryaneurysmsinBehcetsyndrome.AmJ