REVISTA
BRASILEIRA
DE
ANESTESIOLOGIA
PublicaçãoOficialdaSociedadeBrasileiradeAnestesiologiawww.sba.com.br
SCIENTIFIC
ARTICLE
Functional
respiratory
imaging
after
neostigmine-
or
sugammadex-enhanced
recovery
from
neuromuscular
blockade
in
the
anesthetised
rat:
a
randomised
controlled
pilot
study
夽
Tom
Schepens
a,
Guy
Cammu
b,∗,
Sabine
Maes
a,
Benny
Desmedt
c,
Wim
Vos
d,
Kristof
Deseure
eaAntwerpUniversityHospital,DepartmentofAnesthesiology,Edegem,Belgium
bOnze-Lieve-VrouwZiekenhuis,AnaesthesiologyandCriticalCareMedicine,Aalst,Belgium cResearchCentre,Aalst,Belgium
dFLUIDDA,Kontich,Belgium
eUniversityofAntwerp,DepartmentofAlgology,Wilrijk,Belgium
Received24July2015;accepted23November2015
Availableonline20April2016
KEYWORDS
Diaphragm; Neostigmine; Neuromuscular blockade; Rocuronium; Sugammadex
Abstract
Objectives: Reductionsindiaphragmactivityareassociatedwiththepostoperative develop-ment of atelectasis.Neostigmine reversalis also associated withincreased atelectasis.We assessedtheeffectsofneostigmine,sugammadex,andspontaneousreversalonregionallung ventilationandairwayflow.
Methods:SixSprague---Dawleyratswereparalysedwithrocuroniumandmechanicallyventilated untilrecoveryofthetrain-of-fourratioto0.5.Weadministeredneostigmine(0.06mg.kg−1),
sugammadex (15mg.kg−1), or saline (n=2 per group). Computed tomography scans were
obtainedduringthebreathingcycle.Three-dimensionalmodelsoflunglobesweregenerated usingfunctionalrespiratoryimagingtechnology,andlobarvolumeswerecalculatedduringthe breathingcycle.The diaphragmaticsurfacewassegmentedfor theend-expiratoryand end-inspiratoryscans.Thetotalchangeinvolumewasreportedbythelungvolumechangefrom theend-expiratoryscantotheend-inspiratoryscan.Chestwallmovementwasdefinedasthe lungvolumechangeminusthevolumechangethatresultedfromdiaphragmexcursion.
Results:Thetwo ratsthatreceivedneostigmineexhibitedasmallerrelativecontributionof diaphragm movementto thetotal changein lungvolume compared withthe tworats that receivedsugammadexorsaline(chestwallcontribution(%):26.69and25.55forneostigmine; −2.77and15.98forsugammadex;18.82and10.30forsaline).
夽 TheexperimentswereconductedattheBrukerfacilities(Kontich,Belgium).
∗Correspondingauthor.
E-mail:guy.cammu@olvz-aalst.be(G.Cammu). http://dx.doi.org/10.1016/j.bjane.2015.11.004
Conclusion:Thispilotstudyinratsdemonstratedanincreasedrelativecontributionofchest wallexpansionafterneostigminecomparedwithsugammadexorsaline.Thissmallerrelative contributionofdiaphragmmovementmaybeexplainedbyaneostigmine-induceddecreasein phrenicnerveactivityorbyremainingoccupiedacetylcholinereceptorsafterneostigmine. ©2016SociedadeBrasileiradeAnestesiologia.PublishedbyElsevierEditoraLtda.Thisisan openaccessarticleundertheCCBY-NC-NDlicense( http://creativecommons.org/licenses/by-nc-nd/4.0/).
PALAVRAS-CHAVE
Diafragma; Neostigmina; Bloqueio neuromuscular; Rocurônio; Sugamadex
Imagemfuncionaldarespirac¸ãoapósacelerac¸ãodarecuperac¸ãodobloqueio neuromuscularcomneostigminaousugamadexemratosanestesiados:estudopiloto controladoerandomizado
Resumo
Objetivos: Asreduc¸ões da atividadedo diafragma estão associadas ao desenvolvimento de atelectasiano período pós-operatório. A reversãocom neostigminatambémestá associada ao aumentode atelectasia. Avaliamos osefeitos de neostigmina,sugamadex edareversão espontâneasobreaventilac¸ãopulmonarregionalefluxoaéreo.
Métodos: SeisratosSprague-Dawleyforamparalisadoscomrocurônioemecanicamente venti-ladosatéarecuperac¸ãodasequênciadequatroestímulosatingirrelac¸ão0,5.Administramos neostigmina(0,06mg.kg−1), sugamadex (15mg.kg−1)ousoluc¸ãosalina (n=2 porgrupo). As
tomografiasforamrealizadas duranteociclorespiratório.Modelostridimensionaisdoslobos pulmonaresforamgeradosusandoatecnologiadeimagemfuncionalrespiratóriaeosvolumes lobaresforamcalculadosduranteociclorespiratório.Asuperfíciediafragmáticafoisegmentada paraasvarredurasexpiratóriafinaleinspiratóriafinal.Aalterac¸ãototalnovolumefoirelatada pelaalterac¸ãodovolumepulmonardavarreduraexpiratóriafinalparaavarredurainspiratória final.Omovimentodaparedetorácicafoidefinidocomoavariac¸ãodovolumepulmonarmenos aalterac¸ãonovolumeresultantedaexcursãododiafragma.
Resultados: Osdoisratosquereceberamneostigminaapresentaramumacontribuic¸ãorelativa menordomovimentododiafragmaparaaalterac¸ãototaldovolumepulmonaremcomparac¸ão comosdoisratosquereceberamsugamadexousoluc¸ãosalina(contribuic¸ãodaparedetorácica (%):26,69e25,55paraneostigmina;-2,77e15.98parasugamadex;18,82e10,30parasoluc¸ão salina).
Conclusão:Esteestudopilotocomratosdemonstrouumacontribuic¸ãorelativaaumentadade expansãoda paredetorácica apósneostigmine em comparac¸ãocom sugamadexou soluc¸ão salina.Essacontribuic¸ãorelativamenordemovimentododiafragmapodeserexplicadapor uma reduc¸ão induzida porneostigminanaatividade donervo frênico ouporreceptores de acetilcolinapermaneceremocupadosapósaadministrac¸ãodeneostigmina.
©2016SociedadeBrasileiradeAnestesiologia.PublicadoporElsevierEditoraLtda.Este ´eum artigoOpen Accesssobumalicenc¸aCCBY-NC-ND( http://creativecommons.org/licenses/by-nc-nd/4.0/).
Introduction
TheuseofNeuromuscularBlockingAgents(NMBAs)is associ-atedwithpostoperativepulmonarycomplicationsattheend of surgery.1 Respiratory complications after surgery(e.g., desaturationandatelectasis)arepotentiallyrelatedtothe lackofdiaphragmactivity,whichcannotbedetectedusing peripheralAcceleromyography(AMG)monitoring.2,3
A previous trial by our study group associated the use of a Selective Relaxant-Binding Agent (SRBA) for the reversal of neuromuscular blockade, sugammadex, to an increase in diaphragm Electromyographic activity (EMGdi) comparedwithreversal withneostigmine.4 More nicotinic acetylcholine receptors may be free from rocuronium in diaphragmatic neuromuscular junctions after SRBA
studies ofregional flow andallowsstructural simulations. Differentairwaysectionsareassociatedwithcorresponding lungtissuetorenderafullanatomicalpicture.Acomparison ofmorphological scansat differentbreathinglevels(e.g., end-inspiratory and end-expiratory) allows the modelling ofregionalairwayandalveolarrecruitment.
Methods
This study was a randomised, controlled, parallel-group double-blindedtrialinrats.Wecomparedspontaneous(no drug)reversalwithneostigmine-orsugammadex-enhanced reversalofarocuronium-inducedneuromuscularblockade. Animalprotocolsstrictlyadheredtotheinstitutional guide-linesforanimalcareanduseforresearchpurposes.Approval oftheCommitteeforMedicalEthicsandtheUseof Exper-imental Animals at the University of Antwerp, Belgium was obtained (Ref. 2014-63, Chairperson Prof. Dr. P. De Deyn)onNovember17,2014.The studywasregisteredas NCT02284412.Everyeffortwasmadetominimisethe num-berof ratsused.The experimentswere conductedat the Brukerfacilities(Kontich,Belgium),andqualifiedpersonnel performedallexperimentalanimalprocedures.
Experimentalanimalpreparation
SixadultmaleSprague---Dawleyrats(LAnumber:1100155) weighing 377---451g were fed a standard pellet diet and water ad libitum. Room temperature and humidity were monitored dailyand kept constant.Twelve-hour light and dark cycles were provided. The 6 animals were ran-domised to one of the following three groups in a 1:1:1 ratio according to a computer-generated randomisation list: 0.06mg.kg−1 neostigmine, 15mg.kg−1 sugammadex7 or saline. All drugs were obtained from clinical supplies. Anesthesia wasinduced in an inductionchamber using5% isoflurane, and anesthesia was maintained with 1.5---2.5% isofluranein air-oxygen. Atail veinand thetrachea were cannulatedafteranesthesiainduction.Theratswereplaced in a supine position with the head in a neutral position and connectedto a breathingcircuit (Harvard model 683 SmallAnimalVentilator,Holliston,MA,USA).Body temper-ature was measured using a rectalprobe and maintained at>36◦Cusingathermostaticallycontrolledheatingplate.
Heartrate,breathingfrequencyandpawskincolourwere maintainedwithinnormalranges.
The right leg was shaved, and the femoral nerve was stimulatedsupramaximallyusingsubcutaneousneedle elec-trodes (B. BraunMelsungen AG,Melsungen, Germany)for assessments of neuromuscular transmission. The evoked response of the femoral muscle was measured using accelerometrywiththeTOF-WatchSX(MIPMMammendorfer InstitutfürPhysikundMedizinGmbH,Munich,Germany),as describedpreviously.7Thetransducerwasfixedtotheskin ventromediallyattheproximalendofthethigh(Fig.1).The supramaximalstimulationcurrentwasdetermined,andthe femoralnervewascontinuouslystimulatedat1Hz(8---10mA) untilthetwitchheightreachedastableplateau.The stimu-lationpatternwaschangedthereaftertotrain-of-four(TOF) stimulation(2Hz) appliedfor aminimum of3min to cali-bratetheTOF-WatchSXmonitor(calibrationmode1).TOF
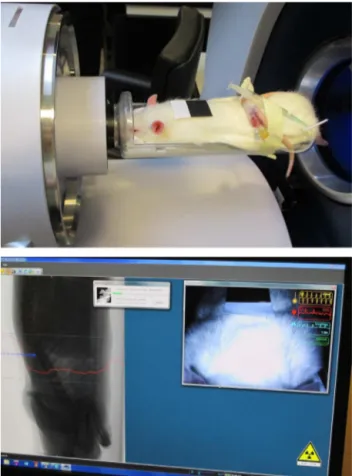
Figure 1 Assessment of neuromuscular transmission using
accelerometry with the TOF Watch SX, subcutaneous needle
electrodesforfemoralnervestimulationandtransducer
place-mentontheratthighformuscleresponsemeasurements.
stimulationwascontinuedforatleast2minbeforeinjection oftheNMBA.Rocuronium(3.5mg.kg−1,2timestheeffective
dose(ED)90)wasinjected,andthelungswereventilated using a 2.5mL tidal volume, 90 breaths per minute ven-tilation scheme. TOF stimulation with a 15s interval was continuedthroughouttheremainderoftheprocedure.
We administered0.06mg.kg−1 neostigmine, 15mg.kg−1
sugammadex or saline at a TOF=0.5. Neostigmine was dosed as 0.06mg.kg−1, and glycopyrrolate was used at
0.012mg.kg−1(commerciallyavailable5:1co-formulation).
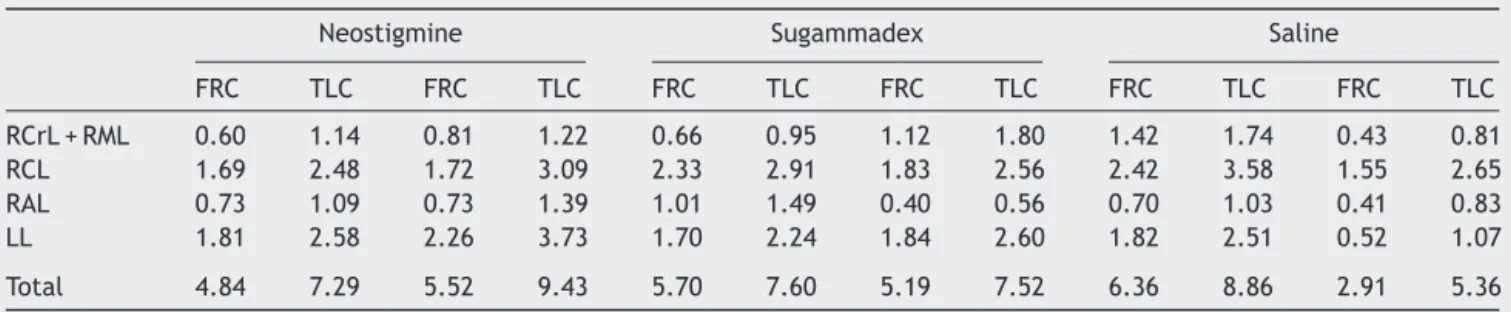
Figure2 Top:PositionoftheratintheCTtube.Bottom:The
physiologicalmonitoringsystem includedvideomonitoringof
theratwithreal-timebreathingdetection.Thesoftware
analy-sesthevideostreamfromthepointwherebreathingmovement
isvisible. These movements areconverted into amovement
waveformto providebreathingtime marksfor time-resolved
micro-CTreconstruction.Topandbottom:Theanesthetic
deliv-eryfacemaskontheanimalisconnectedtoaflowsensorfor
directbreathingdetection.Multipleprojectionimagesobtained
ateach angular position are sorted post-scaninto breathing
timebinsusingrecordedphysiologicalmonitoringtimemarks.
usedtherespiratoryfrequencyasparametersfor anesthe-siadepthmaintenanceduringtheCTscanningperiodwhen theratswereinaccessible.Allrecordswerekeptandstored. Allanimalswereeuthanisedattheendoftheprocedure.
Imaging
WeusedtheSkyScan1278invivomicro-CTscanner(Bruker microCT, Kontich, Belgium). This system has integrated physiological monitoring, including breathing movement, andfour-dimensional(4D)time-resolved microtomography capabilities. Dynamicscanning techniques, asusedin the present 4D free-breathing CT scan protocol, exhibit the intrinsicproblem of motion artefacts. We usedthe respi-ratorygatingtechnique toreduce theseartefacts. Motion oftheanimal’sthoraxwasregistered, andtheir breathing patterns were monitored to apply this gating. The gat-ing thresholds were set on these recordings. Scans were obtainedusingasourcevoltageof70kVandasourcecurrent of140A.Theresolutionwassetto100m.Thescannerhad
an8cmwidefieldofview,whichspannedtheentirethorax. Theretrospectivelysynchronised‘‘listmode’’scanwas per-formedwithanexposuretimeof40ms,ascanrotationof 360◦ andstepof 0.75◦.Twenty-five imageswereacquired
perstepforsubsequentsortingintobreathingcyclephases. The timeofallvideo-recorded breathinginhalation move-mentmaximaandthetimeofacquisitionofallprojection imageswererecordedduringthescanintextfileswitha pre-cisionof±1mstofacilitatelistmodesorting.End-expiratory andend-inspiratorygated andbinnedimagesaroundtidal breathing were further processed. The respiratory wave-train wasdisplayedin real-time, anddata were exported at the end of thescanning processfor furtherreference. Theentirescanningproceduretookbetween18and24min. CTimageswerepost-processedtoassesssegmentationand regionalflowpatternsandvisualiseandquantifythe follow-ingparametersof themicro-CT images:(1)lung andlobe volumesatinspirationandexpiration;(2)airwayvolumesat inspirationandexpiration;(3)diaphragmshapeand defor-mationwithresultinglungvolumechangefrominspiration toexpiration; and(4)skeletal movement frominspiration toexpiration.Theseparameterswereusedtoassess differ-encesbetweentreatmentgroups.
Thepresentstudycomparedtheeffectofsugammadex, neostigmine/glycopyrrolate and spontaneous reversal on regionallung ventilation.Allcomparisonswereperformed withanexploratoryintent,andnostatisticalanalyseswere performed.Dataareexpressedasabsolutevalues(%).
Results
Thetimefromrocuroniumadministrationtorecoveryofthe TOF ratio to 0.5 was 14min and 14min in the rats that received neostigmine, 15min and 21min in the rats that receivedsugammadex, and 14min and16min inrats that receivedsaline.Thetimefromthestartofneostigmineor sugammadexorsalineadministrationtorecoveryoftheTOF ratioto0.9was120and90s,45and90s,and120and360s, respectively.
LunglobesweresegmentedanddividedforFRIbasedon visiblelobarfissuresontheCTscan.Therearefivelunglobes intherat:oneLeftLobe(LL)andfourlobesontheright (cra-nial(RCrL),middle(RML),caudal(RCL)andaccessory(RAL) lobes).Theaccessorylobecontactsthediaphragmandapex oftheheartanditisnotchedtoaccommodatethecaudal cavalvein.8Fig.3presentsanexampleofthe3D reconstruc-tionofthelung lobesfor onerat.The fissuredividingthe rightcraniallobeandtherightmiddlelobewasnotvisibleon mostofthescans,andtherightcraniallobeoftenappeared collapsed.Therefore,theselobes werenotseparatedand consideredasinglelobeforallsubsequentanalyses.
Lobar volumes were reconstructed for all rats, and total lung volumes were calculated using these models. The relative lobar growth from the end-expiratory scan level (hereafter referred to as FRC) to the end-inspiratory scan level (hereafter referred to as TLC),
VTLClobe−VFRClobe/VTLClungs−VFRClungs,wasconsidereda
mea-sure for the internal distribution of inhaled air. Table 1
Table1 Lobarandtotallungvolumes(inmL)attheend-expiratoryscan(FRC)andend-inspiratoryscan(TLC).
Neostigmine Sugammadex Saline
FRC TLC FRC TLC FRC TLC FRC TLC FRC TLC FRC TLC
RCrL+RML 0.60 1.14 0.81 1.22 0.66 0.95 1.12 1.80 1.42 1.74 0.43 0.81
RCL 1.69 2.48 1.72 3.09 2.33 2.91 1.83 2.56 2.42 3.58 1.55 2.65
RAL 0.73 1.09 0.73 1.39 1.01 1.49 0.40 0.56 0.70 1.03 0.41 0.83
LL 1.81 2.58 2.26 3.73 1.70 2.24 1.84 2.60 1.82 2.51 0.52 1.07
Total 4.84 7.29 5.52 9.43 5.70 7.60 5.19 7.52 6.36 8.86 2.91 5.36
RCrL,rightcraniallobe;RML,rightmiddlelobe;RCL,rightcaudallobe;RAL,rightaccessorylobe;LL,leftlobe.
Table2 Internalairflowdistribution(%)fromtheend-expiratoryscan(FRC)totheend-inspiratoryscan(TLC).
Neostigmine Sugammadex Saline
RCrL+RML 21.77 10.31 15.29 29.14 13.07 15.49
RCL 32.24 35.27 30.72 31.31 46.42 45.06
RAL 14.69 16.74 25.55 6.84 13.28 16.82
LL 31.30 37.68 28.44 32.70 27.22 22.63
RCrL,rightcraniallobe;RML,rightmiddlelobe;RCL,rightcaudallobe;RAL,rightaccessorylobe;LL,leftlobe.
eachratusingthesevalues,andtheresultsarepresented inTable2.
Three-dimensionalmodelsofthediaphragmaticsurface weregeneratedforFRCandTLCaftertheidentificationof the FRC and TLC scans based on the total lung volumes, as exemplified in Fig. 4 (same rat as Fig. 3). Diaphragm movementwasassessedbymeasuringthevolumecontained between the twosurfaces. The total change in volumeis indicated by the lung volume change from FRC to TLC.
Figure3 Three-dimensionalreconstructionofthelunglobes
attheend-inspiratoryscanforoneofthestudyrats.Right
cra-niallobe(RCrL)---red;rightmiddlelobe(RML)---yellow;right
caudallobe(RCL)---orange;rightaccessorylobe(RAL)---green;
leftlobe(LL)---blue.
Therefore,thechestwallmovementwasdefinedasthetotal lungvolumechangeminusthelungvolumechangeresulting fromdiaphragmaticmovement.
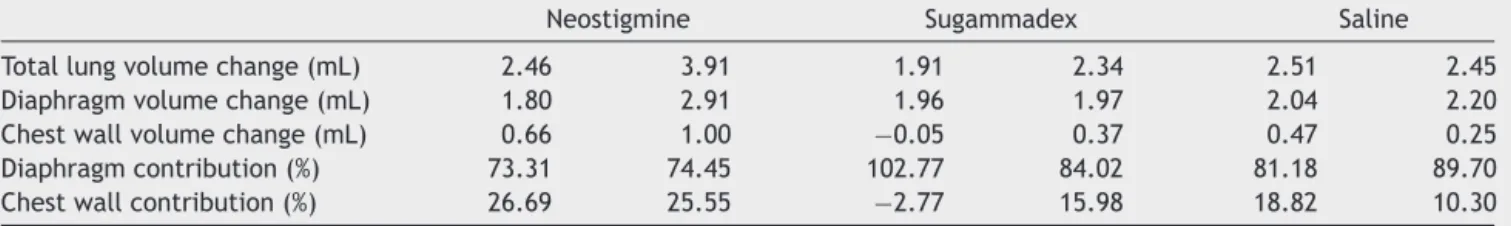
Table3summarisesthecalculationsthatwereperformed toobtaintherelativecontributionsofthechestwall expan-sionanddiaphragm movementtothetotalchange oflung volume.The relativecontribution ofchest wallexpansion wasincreasedin neostigmine-treated rats compared with sugammadex-orsaline-treatedrats(chestwallcontribution (%):26.69and25.55forneostigmine;−2.77and15.98for sugammadex;18.82and10.30forsaline).
Discussion
This pilot study compared the effects of sugammadex, neostigmine/glycopyrrolate and spontaneous reversal on regionallungventilationinratsparalysedwithrocuronium andreversed(ornot)ataTOFratioof0.5.CTscanswere obtained after recovery of the TOF ratio >0.9 during the spontaneous breathing cycle, and 3D models of the lung lobes were generated using FRI technology to calculate lobarvolumes.Therelativecontributionsofthechestwall
Figure 4 3D reconstruction of the diaphragm at the
end-inspiratory scan (TLC)--- yellow and the end-expiratory scan
Table3 Totallung,diaphragmandchestwallvolumechangesfromtheend-expiratoryscan(FRC)totheend-inspiratoryscan (TLC)andtherelativecontributionofthechestwallexpansionanddiaphragmmovementtothetotalvolumechange.
Neostigmine Sugammadex Saline
Totallungvolumechange(mL) 2.46 3.91 1.91 2.34 2.51 2.45
Diaphragmvolumechange(mL) 1.80 2.91 1.96 1.97 2.04 2.20
Chestwallvolumechange(mL) 0.66 1.00 −0.05 0.37 0.47 0.25
Diaphragmcontribution(%) 73.31 74.45 102.77 84.02 81.18 89.70
Chestwallcontribution(%) 26.69 25.55 −2.77 15.98 18.82 10.30
expansion and diaphragm movement to the total change oflungvolumewereobtained.The tworatsthatreceived neostigmineas a reversal agent displayed a smaller rela-tivecontributionofdiaphragmmovementtototalchangein lungvolumecomparedwithratsthatreceivedsugammadex orsaline. Consequently,therelativecontribution ofchest wallexpansionwasincreasedinneostigmineratscompared withratsthatreceivedsugammadexorsaline.
Theexacteffectofneuromuscularblockadeand rever-sal agents on the diaphragm in a perioperative setting is not well studied. Mechanical ventilation and rocuro-niumplayindependentrolesindiaphragmaticdysfunction.9 Mechanicalventilation exertsrelatively short-termeffects ontheratdiaphragm,includingareductioninbloodflow, which impairs oxygen uptake.10 However, good diaphrag-maticfunctionisessentialinpatientsattheendofsurgery whenspontaneousbreathingisresumed.The diaphragmis the most important inspiratorymuscle, and reductions in diaphragmactivityareassociatedwiththedevelopmentof atelectasispostoperatively.2
A previous study compared the effects of neostig-mine/glycopyrrolate and sugammadexon EMGdi.4 EMGdi, tidal volume and PaO2 following tracheal extubation at
a TOF ratio >0.9 decreased after neostigmine compared with sugammadex, which reflects a reduced diaphragm-driven inspiration after neostigmine. Eikermann et al.11 demonstratedthatneostigminealone(withoutprior treat-mentwithaNMBA)decreaseddiaphragmaticEMGactivity. Neostigminereversalwasrecentlyassociatedwithincreased atelectasis and longer postoperative hospital stays. The unwarranteduse of neostigmine (neostigmine administra-tion without appropriate guidance from neuromuscular transmission monitoring) is associated with an increased incidenceofpulmonaryoedemaandreintubation.12 These studyresultsareconsistentwiththefindingsfromaprevious epidemiological study that revealed an absence of bene-ficialeffects ofneostigmineonpostoperativeoxygenation andreintubation.1,13
Ourpilot studyin rats demonstratedthatunwarranted neostigmine use was not an issue because reversal was notadministered earlier thana TOF ratioof 0.5, and FRI occurred after recovery of the TOF ratio >0.9. However, thetworatsthatreceivedneostigmineasareversalagent exhibited a smaller relative contribution of diaphragm movement to the total change in lung volume compared withratsthatreceived sugammadexorsaline. This result may be explained by an effect on neuromuscular trans-mission because the remaining occupied acetylcholine receptors after neostigmine administration may decrease
theefficiencyofneuromuscularcouplingatthediaphragm in contrasttosugammadex. Alternatively, we hypothesise that the increased relative contribution of rat chest wall expansion after neostigmine compared with sugammadex or salinemayalso beexplainedbyaneostigmine-induced decrease in phrenic nerve activity. Neostigmine reduced efferent phrenic nerve activity before neuromuscular blockadeatthegastrocnemicmuscleincats.5
Summary
Ratsinthispilotstudyexhibiteda smallerrelative contri-butionofdiaphragmmovementtothetotalchangeinlung volume after a neostigmine-enhanced recovery to a TOF ratioofatleast0.9comparedwithsugammadexorsaline, whichconsequentlyrecruitedsecondaryrespiratorymuscles asprimarybreathingmuscle.Limitationsofourpilotstudy include theuse of an animal model,the smallnumber of subjects,andthepossibleimprecisionassociatedwiththe results. The relevance tohuman biology requires further investigation.
Conflicts
of
interest
TSreceivedresearchgrantsfromMSD.GCreceivedresearch grantsandlecturefeesfromMSDandpreviouslyperformed funded researchonsugammadex. SM, BDand KDhave no competinginterestsrelatedtothisarticle.TS,GC,SM,BD andKDhavenofinancialrelationshipswithanyorganisation orcompanythatmayhaveaninterestinthesubmittedwork. WVisChiefTechnologyOfficeratFLUIDDA.
Acknowledgments
ThisworkwassponsoredbyMSDBelgiumBVBA/SPRL,1200 Brussels,Belgium(Investigator-InitiatedStudy52169).The authors designed, conducted and analysed the investiga-tion.Responsibility for interpretation of thedataand the contentandconclusionofthispaperlieswiththeauthors. The authorsthankJanGielisandAnnemieVanDenBroeck fortheirindispensablehelpandadvice.
References
2.KarayiannakisAJ,MakriGG,MantziokaA,etal.Postoperative pulmonaryfunctionafterlaparoscopicandopen cholecystec-tomy.BrJAnaesth.1996;77:448---52.
3.EikermannM,GerwigM,HasselmannC,etal.Impaired neuro-musculartransmissionafterrecoveryofthetrain-of-fourratio. ActaAnaesthesiolScand.2007;51:226---34.
4.Schepens T, Cammu G, Saldien V, et al. Electromyo-graphic activity of the diaphragm during neostigmine or sugammadex-enhancedrecoveryafterneuromuscularblockade withrocuronium.EurJAnaesthesiol.2015;32:49---57.
5.Fleming NW, Henderson TR, Dretchen KL. Mechanisms of respiratoryfailureproducedbyneostigmineanddiisopropyl flu-orophosphates.EurJPharmacol.1991;195:85---91.
6.DeBackerJW,VosWG,BurnellP,etal.Studyofthevariability inupperandlowerairwaymorphologyinSprague-Dawleyrats usingmodernmicro-CTscan-basedsegmentation techniques. AnatRec(Hoboken).2009;292:720---7.
7.EikermannM,ZarembaS,MalhotraA,etal.Neostigminebut notsugammadeximpairsupperairwaydilatormuscleactivity andbreathing.BrJAnaesth.2008;101:344---9.
8.Baker HJ, J, Lindsey JR, Weisbroth SH. The laboratory rat: biologyand diseases.Waltham,MA:ElsevierAcademicPress; 2013.
9.TestelmansD,MaesK,WoutersP,etal.Rocuroniumexacerbates mechanicalventilation-induceddiaphragmdysfunctioninrats. CritCareMed.2006;34:3018---23.
10.DavisRT,BruellsCS,StableyJN,etal.Mechanicalventilation reducesratdiaphragmbloodflowandimpairsoxygendelivery anduptake.CritCareMed.2012;40:2858---66.
11.Eikermann M, FassbenderP, MalhotraA, et al. Unwarranted administration of acetylcholinesterase inhibitors can impair genioglossusand diaphragm muscle function.Anesthesiology. 2007;107:621---9.
12.SasakiN,MeyerMJ,MalviyaSA,etal.Effectsofneostigmine reversalofnondepolarizingneuromuscularblockingagentson postoperativerespiratoryoutcomes:aprospectivestudy. Anes-thesiology.2014;121:959---68.