REVISTA
BRASILEIRA
DE
ANESTESIOLOGIA
Publicação Oficial da Sociedade Brasileira de Anestesiologiawww.sba.com.br
SCIENTIFIC
ARTICLE
Paravertebral
block
for
management
of
acute
postoperative
pain
and
intercostobrachial
neuralgia
in
major
breast
surgery
Mercedes
Fernández
Gacio
a,∗,
Ana
Maria
Agrelo
Lousame
a,
Susana
Pereira
b,
Clara
Castro
c,
Juliana
Santos
daDepartamentodeAnestesiologia,InstitutoPortuguêsdeOncologiaFranciscoGentil(EPE),Porto,Portugal bServic¸odeNeurologia,InstitutoPortuguêsdeOncologiaFranciscoGentil(EPE),Porto,Portugal
cRegistoOncológicoRegionaldoNorte(Roreno),InstitutoPortuguêsdeOncologiaFranciscoGentil(EPE),Porto,Portugal dUnidadedeDiagnósticoeTratamentodaDor,InstitutoPortuguêsdeOncologiaFranciscoGentil(EPE),Porto,Portugal
Received16October2014;accepted23February2015 Availableonline14July2016
KEYWORDS Paravertebralblock; Majorbreastsurgery; Acutepain;
DN4;
Neuropathicpain; Intercostalnerve
Abstract
Background: Severallocoregionaltechniqueshavebeendescribedforthemanagementofacute andchronicpainafterbreastsurgery.Theoptimaltechniqueshouldbeeasytoperform, repro-ducible, withlittle discomforttothepatient,little complications,allowing goodcontrolof acutepainandadecreasedincidenceofchronicpain,namelyintercostobrachialneuralgiafor beingthemostfrequententity.
Objectives: Theaimofthisstudywastoevaluatetheparavertebralblockwithpreoperative singleneedleprick formajorbreastsurgeryandassessinitiallythecontrolofpostoperative nausea andvomiting (PONV)andacutepain inthe first 24h andsecondlythe incidenceof neuropathicpainintheintercostobrachialnerveregionsixmonthsaftersurgery.
Methods:Thestudyincluded80femalepatients,ASAI-II,aged18---70years,undergoingmajor breastsurgery,undergeneralanesthesia,stratifiedinto2groups:generalanesthesia(inhalation anesthesiawithopioids,accordingtohemodynamicresponse)andparavertebral(paravertebral blockwithsingleneedleprickinT4with0.5%ropivacaine+adrenaline3gmL−1withavolume
of0.3mLkg−1preoperativelyandsubsequentinductionandmaintenancewithgeneral
inhala-tionalanesthesia).In theearlypostoperativeperiod,patient-controlledanalgesia(PCA)was placedwithmorphinesetforbolusondemandfor24h.Intraoperativefentanyl,postoperative morphineconsumption,technique-relatedcomplications, painatrestandduringmovement
∗Correspondingauthor.
E-mail:acidade21@hotmail.com(M.F.Gacio).
http://dx.doi.org/10.1016/j.bjane.2015.02.007
wererecordedat0h,1h,6hand24h,aswellasepisodesofPONV.Allvariablesidentified asfactorscontributingtopainchronicityage,typeofsurgery,anxietyaccordingtothe Hos-pitalAnxietyandDepressionScale(HADS),preoperativepain,monitoringathome;bodymass index(BMI)andadjuvantchemotherapy/radiationtherapywereanalyzed,checkingthe homo-geneity ofthesamples. Sixmonths after surgery, theincidenceofneuropathic pain inthe intercostobrachialnervewasassessedusingtheDN4scale.
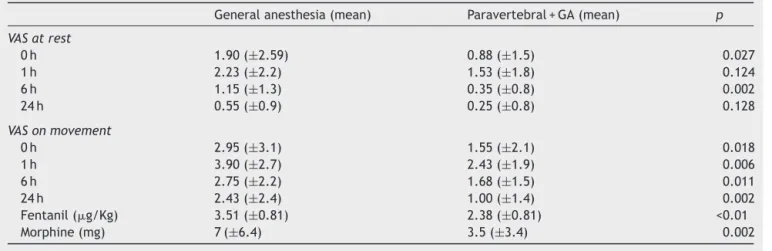
Results:TheVisualAnalogScale(VAS)valuesofparavertebralgroupatrestwerelower through-outthe24hofstudy0h1.90(±2.59)versus0.88(±1.5)1h2.23(±2.2)versus1.53(±1.8)6h 1.15(±1.3)versus0.35(±0.8);24h0.55(±0.9)versus0.25(±0.8)withstatisticalsignificance at0hand6h.Regardingmovement,paravertebralgrouphadVASvalueslowerandstatistically significantinallfourtimepoints:0h2.95(±3.1)versus1.55(±2.1);1h3.90(±2.7)versus2.43 (±1.9)6h2.75(±2.2)versus1.68(±1.5);24h2.43(±2.4)versus1.00(±1.4).Theparavertebral groupconsumedlesspostoperativefentanyl(2.38±0.81gkg−1versus3.51±0.81gkg−1)and
morphine(3.5mg±3.4versus7mg±6.4)withstatisticallysignificantdifference.Chronicpain evaluationofat6monthsofparavertebralgroupfoundfewercasesofneuropathicpaininthe intercostobrachialnerveregion(3casesversus7cases),althoughnotstatisticallysignificant. Conclusions:Single-injectionparavertebralblockallowspropercontrolofacutepainwithless intraoperativeandpostoperativeconsumptionofopioidsbutapparentlyitcannotpreventpain chronicity.Furtherstudiesareneededtoclarifytheroleofparavertebralblockinpainchronicity inmajorbreastsurgery.
©2015SociedadeBrasileiradeAnestesiologia.PublishedbyElsevierEditoraLtda.Thisisan openaccessarticleundertheCCBY-NC-NDlicense( http://creativecommons.org/licenses/by-nc-nd/4.0/).
PALAVRAS-CHAVE Bloqueio
paravertebral; Cirurgiademama; Doraguda; DN4;
Dorneuropática; Nervo
intercostobraquial
Bloqueioparavertebralnocontroledadoragudapós-operatóriaedorneuropática donervointercostobraquialemcirurgiamamáriadegrandeporte
Resumo
Justificativa:Estãodescritasváriastécnicaslocorregionaisparaaabordagemdadoragudae dorcrônicaapóscirurgiademama.Oidealseriaumatécnicafácildefazer,reprodutível,com poucodesconfortoparaasdoentes,compoucascomplicac¸õesequepermitiráumbomcontrole dadoragudaeumadiminuic¸ãodaincidênciadedorcrônica,notadamentedorneuropáticado intercostobraquial,porseraentidademaisfrequente.
Objetivos: Estudaraaplicac¸ãodebloqueioparavertebralcompicadaúnicanopré-operatório de cirurgia mamáriade grande porte. Avaliarnuma primeira fase o controlede doraguda enáuseas-vômitos nopós-operatório (NVPO)nasprimeiras 24horase numasegunda fasea incidênciadedorneuropáticanaregiãodonervointercostobraquialseismesesapósacirurgia. Métodos: Foramincluídas80doentesdosexofeminino,ASAI-II,entre18e70anos,submetidas acirurgiamamáriadegrandeportesobanestesiageral,estratificadasemdoisgrupos:anestesia geral(anestesiageralinalatóriacomopioidessegundorespostahemodinâmica)eparavertebral (bloqueioparavertebralcompicada únicaemT4comropivacaína0,5%+adrenalina3g/mL
comum volume de0,3mL/kg pré-operatoriamente eposterior induc¸ão emanutenc¸ãocom anestesiageralinalatória).Nopós-operatórioimediato foicolocadaPCA (Patient-controlled analgesia)demorfinaprogramadacombolusademandadurante24horas.Foramregistados fentanilintraoperatório,consumodemorfinapós-operatória,complicac¸õesrelacionadascomas técnicas,doremrepousoeaomovimentoa0,1h,6he24h,assimcomoosepisódiosdeNVPO. Foramanalisadastodasasvariáveisidentificadascomo fatoresdecronificac¸ãodadoridade, tipodecirurgia,ansiedadesegundoescaladeHADS(HospitalAnxietyandDepressionscale), dorpré-operatória;acompanhamentonodomicílio;índicedemassacorporal(IMC),tratamentos adjuvantesdequimioterapia/radioterapiaefoiverificadaahomogeneidadedasamostras.Aos seismesesdacirurgiafoiavaliada,segundoescalaDN4,aincidênciadedorneuropáticanaárea donervointercostobraquial.
(2,38±0,81g/Kgversus3,51±0,81g/Kg)emenosmorfinanopós-operatório(3,5mg±3,4
versus 7 mg±6,4), com diferenc¸a estatisticamente significativa. Na avaliac¸ão de dor crônica aos seis meses no grupo paravertebral houve menos casos de dor neuropática na região do nervo intercostobraquial (trêsversus sete)embora sem significânciaestatística. Conclusões: Obloqueioparavertebralcompicadaúnicapermiteumadequadocontrolrdador agudacommenorconsumodeopioidesintraopreatóriosepós-operatórios,masaparentemente nãoconsegueevitaracronificac¸ãodador.Maisestudossãonecessáriosparaesclareceropapel dobloqueioparavertebralnacronificac¸ãodadoremcirurgiamamáriadegrandeporte. ©2015SociedadeBrasileiradeAnestesiologia.PublicadoporElsevierEditoraLtda.Este ´eum artigo OpenAccesssobuma licenc¸aCCBY-NC-ND( http://creativecommons.org/licenses/by-nc-nd/4.0/).
Introduction
Inrecentyearsbreastcancerthemost frequentcancerin women1hasdecreaseditsmortality,butunfortunatelyoften
associatedwithincreasedmorbidityduetosequelaeofthe treatmentused.2
Breast cancer surgery has many risk factors for post-operative nausea and vomiting (PONV), reaching up to 70% in some series. In 0.2% of cases, it corresponds to uncontrollablecasesthatdelay hospitaldischarge,require unexpectedadmissions,lowerratesofpatientsatisfaction, andincreasedhospitalcosts.3,4
Chronically, half of patients undergoing breast surgery had some kind of surgery-related pain,5,6 either
nocicep-tive or neuropathic. Pain in the intercostobrachial nerve area is the most common neuropathic pain.7 Among the
factors thatmay influence chronic pain,the most readily modifiablearepostoperativepainandopioidconsumption, so that the greater the intensity of postoperative pain andanalgesic consumption, the higherthe risk ofchronic pain.8
Paravertebralblockseemstoproduceaneffectiveblock ofthepainfulpathways,characterizedbyunilateralregional blockade of several dermatomes. It also allows a sympa-thetic block that could have some benefit in oncology.9
Currently, there are ongoing studies aimed at identifying if thereis a relationship between theloco-regional tech-nique and tumor recurrence, particularly in the breast area.10
The usefulness of this technique for effective postop-erative pain management has already been evaluated in differentstudies,11,12 although therearestillsomedoubts
abouttheparavertebralspaceapproach,moreeffectiveand with fewerside effects. There arereports of single- and multiple-injection techniques with or without a catheter placementaredescribed.13,14
This studywasdesignedintwostagesinorderto com-paretwodifferentapproachesinbreastsurgeryanesthesia: aparavertebralblockwithsingle-injectionassociatedwith general anesthesia versus general anesthesia alone. At the first stage we intended to evaluate the acute pain management in the immediate postoperative period and occurrence of PONVin patients undergoingmajor surgery for breast cancer. At the second stage we evaluated the
presence of neuropathic pain in the intercostobrachial regioninthesame groupof patientssix monthsafterthe surgery.
Material
and
methods
Aprospective,stratifiedobservationalstudywasdesigned.It wasassumedadifferenceof2.64intheaverageassessment oftheVisualAnalogScale(VAS)at24hbetweenthepatients whounderwentparavertebralblockandgeneralanesthesia andpatientswhounderwentgeneralanesthesiaalone,with 80%studypower,5%significancelevel,andsample stratifica-tionaccordingtotheanxiety,agegroup,andtypeofsurgery variables,andweestimatedtheinclusionof80patients ---40ineachgroup.Thesample stratificationvariableswere chosenforbeingthemostoftencitedfactorsasindependent variablesforthedevelopmentofacutepainand/orchronic pain.
Anxiety was assessed using the Hospital Anxiety and Depression scale (HADS). HADS is a hospital tool widely usedfor screeningsituations of anxiety anddepression in hospitalizedcancer patients.15 It consists of 14 questions
(odd-numberedquestionsassessanxietytheeven-numbered assessdepression)withresponsesscoredonascaleof0---3. Totalscoreisobtainedbysummingthevaluesofeach sub-scale. In both cases the higher the score, the higher the levelofanxietyordepression.Thisscalewascompletedby patientsinthepre-anestheticvisitbeforesurgery.Forthis studyweusedacut-off>8points.
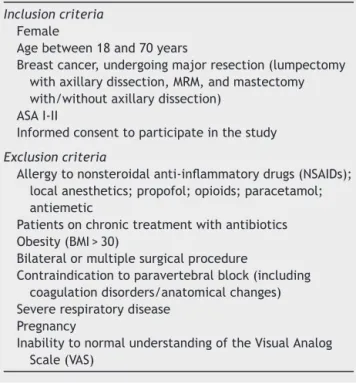
InclusionandexclusioncriteriaareshowninTable1.The study was performed between January 2012 and January 2013.ItwasapprovedbytheEthicsCommitteeofthe insti-tutionandallpatientsgavetheirwritteninformedconsent toparticipateinthestudy.
First
phase
of
the
study
Preoperatively, all patients were stratified into two groups according to the type of surgery, HADS score, and age: paravertebral group (general anesthesia com-bined with paravertebral block) and general anesthesia group.
Table1 Inclusionandexclusioncriteriaofthestudy.
Inclusioncriteria Female
Agebetween18and70years
Breastcancer,undergoingmajorresection(lumpectomy withaxillarydissection,MRM,andmastectomy with/withoutaxillarydissection)
ASAI-II
Informedconsenttoparticipateinthestudy
Exclusioncriteria
Allergytononsteroidalanti-inflammatorydrugs(NSAIDs); localanesthetics;propofol;opioids;paracetamol; antiemetic
Patientsonchronictreatmentwithantibiotics Obesity(BMI>30)
Bilateralormultiplesurgicalprocedure
Contraindicationtoparavertebralblock(including coagulationdisorders/anatomicalchanges) Severerespiratorydisease
Pregnancy
InabilitytonormalunderstandingoftheVisualAnalog Scale(VAS)
monitored according to ASA standards and bispectral index(BIS)anestheticdepth.
Paravertebralgroup
Paravertebral block was performed with single-injection, according to the classic technique,16 at the T4 level
withTuohyneedle18G, with0.5%ropivacaine+adrenaline 3gmL−1,withavolumeof0.3mLkg−1(maximumtotal
vol-umeof30mL).Subsequently,anesthesiawasinduced with propofol(1.5mgkg−1h−1)andfentanyl(2
gkg−1)and
laryn-gealmaskairway(LMA)wasinserted.
Generalanesthesiagroup
Anesthesiawasinducedwithpropofol(1.5mgkg−1h−1)and
fentanyl(2gkg−1)andLMAwasinserted.Themaintenance
of anesthesia was performed in both groups with desflu-rane to maintain BIS values at 45---60 with a mixture of O2/air.
Bothgroupsreceivedparecoxib40mgIVbeforethestart ofsurgery.Duringmaintenance,fentanyl(1.5gkg−1)was
administered if there wasan increase of 20% from base-linevaluesofmeanarterialpressure(MAP)andheartrate (HR).
For maintenance of hemodynamic stability, ephedrine or atropine was administered, at the anesthesiologist’s discretion, if verified a decreased in MAP>20% or HR<50beats/minofbaselinevalues.
Inallpatients,theinstitutionalprotocolforthe preven-tionofnauseaandvomitingwasadministered,accordingto thepredictive model by Apfeland colleagues,with three antiemeticinterventionlines(Table2).
Table2 PreventiveprotocolofPONVusedinthestudy.
Institutionalpreventiveprotocolofpostoperativenausea andvomiting
2riskfactorsorahistoryofPONV:prophylaxiswithone drug(Droperidol);
3riskfactorsorhistoryofNVPO+1riskfactor: prophylaxiswith2drugs(Droperidol+Ondansetrom); PrevioushistoryofPONVmorethanonce+anotherrisk factor:Prophylaxiswith3drugs(Dexamethasone, Droperidol,Ondansetron).
Attheendofsurgery,patient-controlledanalgesia(PCA) with morphine was initiated, programmed with bolus of 2mg ondemand and5min lock-out anda maximum dose of6mgh−1duringthefirst24hpostoperatively.
Inthedifferentphasesofthestudy(preoperative, intra-operative,postoperative),werecordeddifferentvariables thatwereconsideredrelevantinthedevelopmentofacute and/orchronic painor thatcouldinterferewiththestudy results.ThesevariablesareshowninTable3.
We assessed pain at rest according to the VAS score (0---10),aswellaspainwithmobilizationoftheipsilateral arminterpretedas90◦armabductionatfourdifferenttimes
aftersurgery:0h;1h;6hand24haftersurgery.
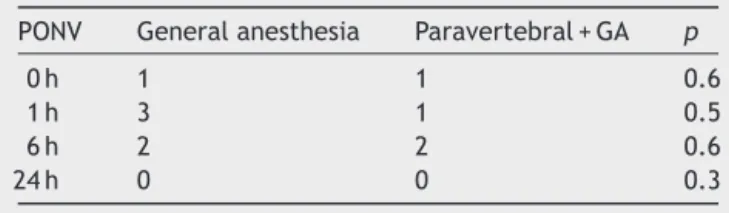
We evaluated the occurrence of PONV using a cate-gorical scale of the institution (0=no nausea; 1=motion sickness; 2=nausea at rest; 3=vomiting; 4=vomiting despite antiemetics) and the need for antiemetic rescue medication,inthefirst24h.
Statisticalanalysis
A descriptive analysis of all variables wasperformed and giventheabsoluteandrelativefrequenciesforcategorical variablesandmeanandstandard deviationor medianand interquartile range for continuous variables, according to theadequacyforeachvariable.
Continuous variables were compared using the inde-pendentsample t-test andcategorical variables usingthe chi-squaretest.Iftherewerenostatisticalassumptionsfor their application, we used the optional statistical tests: Mann---Whitney and Fisher, respectively. The analysis was performedwithasignificancelevelof0.05.
Firstphaseresults
Wecheckedthehomogeneityofthetwogroupsandthere werenostatisticallysignificantdifferencesinvariables,such asage,typeofsurgery,andHADS.Thegroupsprovedtobe homogeneousin the analysisof other variablesthat char-acterize thesample, suchasthe durationof surgery;and variablesrelatedtotheonsetofchronicpain,suchasthe presence of breast pain before surgery, body mass index body(BMI),andfamilysupport(Table4).
During surgery, the average consumption of fentanyl wassignificantlylower(p<0.01)intheparavertebralgroup (2.38±0.81gkg−1)comparedwiththegeneralanesthesia
Table3 Parametersrecordedinthepreoperative,intraoperative,andpostoperativeperiods.
Preoperative Intraoperative Postoperative Sixmonthsaftersurgery
HADS Fentanyl
Age Ephedrine -VASatrest
(0h---1h---6h---24h)
Presenceofneuropathicpain intheintercostobrachial nerveregion
Typeofsurgery Atropine
BMI Complications: -VASonmovement
(0h---1h---6h---24h) Familysupport -Hypotension:>20%
baseline
-DN4 -PONV(0h-1h-6h-24h)
Presenceofbreastpain -Bradycardia<50bpm; Pleuralpuncture;
-EORTC-QLQC30 -Morphine -EORTC-QLQ-BR23 -Pneumothorax
-Localhematoma; -Localbleeding; -Convulsions; -Allergicreaction.
Table4 Variablesrelatedtoacuteandchronicpaininthestudyfirstphase.
Variable Paravertebralgroup(n=40) Generalanesthesiagroup(n=40) p
Age 55.10(±9.8) 52.68(±8.9) 0.2
HADS(%) 0.82
HADS≤8 51.3 48.7
HADS>8 46.7 52.3
Typeofsurgery(%) 0.85
TA+lymphadenectomy 54.5 45.5
Simplemastectomy 50 50
MRM 46.4 53.6
BMI(%) 25.6(±3.4) 25.21(±3.5) 0.6
Durationofsurgery(min) 86.9(±26.9) 84.75(±28.6) 0.7
Preoperativepain(%) 33.3 66.7 0.31
Familysupport(%) 53.6 46.4 0.056
Table5 VASscoreatrestandonmovement;fentanylandmorphineconsumption.
Generalanesthesia(mean) Paravertebral+GA(mean) p
VASatrest
0h 1.90(±2.59) 0.88(±1.5) 0.027
1h 2.23(±2.2) 1.53(±1.8) 0.124
6h 1.15(±1.3) 0.35(±0.8) 0.002
24h 0.55(±0.9) 0.25(±0.8) 0.128
VASonmovement
0h 2.95(±3.1) 1.55(±2.1) 0.018
1h 3.90(±2.7) 2.43(±1.9) 0.006
6h 2.75(±2.2) 1.68(±1.5) 0.011
24h 2.43(±2.4) 1.00(±1.4) 0.002
Fentanil(g/Kg) 3.51(±0.81) 2.38(±0.81) <0.01
Table6 Postoperativeepisodesofnauseaandvomiting.
PONV Generalanesthesia Paravertebral+GA p
0h 1 1 0.6
1h 3 1 0.5
6h 2 2 0.6
24h 0 0 0.3
When the mean values of VAS at rest were compared betweenthe anesthesiagroups at the severaltimes mea-sured, it appears to be always higher in the general anesthesiagroup.Onlyattimes0hand6h,thedifferences inmeanVASweresignificant.So,onecansaythatmeanVAS atrest at 0h and 6h issignificantly higherin thegeneral anesthesiagroup(Table5).
Regarding VAS evaluated during movement, which involvesa90◦abductionofthelimbipsilateraltosurgery,at
alltime-points,thegeneralanesthesiagrouphadmean val-ueshigherthanthoserecordedfortheparavertebralgroup withstatisticalsignificance(Table5).
The group general anesthesia had a higher num-ber of patients (14; 35%) with severe pain (VAS at rest≥7) over 24h compared with the paravertebral group (6; 6%). However, this difference is not significant (p=0.069).
Comparedtopostoperativemorphineconsumption,there wasahigherproportionofpatientsinthegeneralanesthesia group:80%ofpatientsincontrastto67.5%ofthe paraver-tebralgroup,althoughtherewasnostatisticallysignificant differences(p=0.3).
Of the patients who consumed morphine, the general anesthesiagroupconsumed morethan twice the paraver-tebral group, with an average of 7mg (±6.4) in general anesthesiagroupand3.5mg(±3.4)inparavertebralgroup, adifferencestatisticallysignificant(p=0.002).
Regarding nauseaand vomiting there were few events in each subtype according to the institution’s scale, so the results are presented as the sum of any episode of nausea and/or vomiting 24h after surgery. We found that the general anesthesia group had more episodes of NVPO, with six cases (15%), compared to four cases (10.3%)recordedfor theparavertebral group.Therewere no statistically significant differences between groups (Table6).
There were no serious complications related to the techniquethroughoutthestudy.Therewasagreater num-ber of intraoperative hypotension in the paravertebral group (9versus 3 cases),with statistically significant dif-ference(p=0.007) andneed for ephedrine administration in 22.5% of patients in paravertebral group and 2.5% in the general anesthesia group; five cases had bradycar-dia (HR<50) in both groups, with 12.5% of patients in paravertebral group and 7.5% in the general anesthesia group requiring atropine administration. There was one caseofpleuralpunctureintheparavertebralgroupwithout pneumothoraxsignspostoperatively.Therewereno occur-rencesoflocalhematoma,bleeding,convulsionsandallergic reactions.
Second
phase
of
the
study
Six months after the surgery all patients were contacted to start the second phase of the study, which aimed to determinethepresenceofchronicpain,particularly inter-costobrachial neuralgia, and the quality of life of these patients.
Fromtheinitial sampleof80 patientswhohad partici-patedinthefirstphase,therewasalossof14patientswho werenotincludedinthesecondphasefordifferentreasons: follow-upvisitsandadjuvanttreatmentsmadeinother hos-pitalsthatdidnotallowcomingtotheconsultation(four); refusal toparticipate in the second phase (three); death (one); patients undergoingnew breast surgery during the sixmonths(six).
Thesampleforthesecondphaseconsistedof66patients: 34inthegeneralanesthesiagroupand32inthe paraverte-bralgroup. The chemotherapy (CT)andradiation therapy (RT)receivedbythepatientswererecorded.
The66patientsincludedinthesecondstagewereinvited toaconsultationinwhichaclinicalinterviewwasperformed toassessthepresenceofpainintheareaoftheoperated breastand/oripsilateralarm.Todetermineifthepainhad neuropathic characteristics,the DN4scale wasappliedby trainedpersonnel.17DN4isascreeningscaleforneuropathic
pain,translatedandvalidatedforthePortugueselanguage andculture, whichhas aspecificity andsensitivityof 90% and 83%, respectively. It is a simple questionnaire, easily applicable,consistingof fourquestions,tworesponded by thepatientandtwoobjectivelyrespondedbytheclinician. Atotalscoregreaterthanfourclassifiespainasneuropathic (Fig.1).
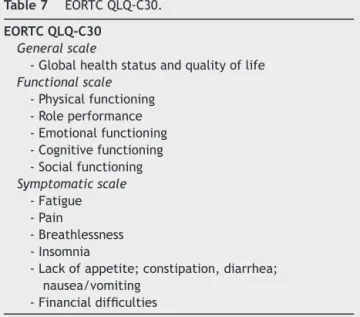
To assess these patients’ quality of life, the European OrganizationforResearchandTreatmentofCancer(EORTC) scalewasused.18Itincorporatesfivefunctionalscales,three
toassesssymptomsandoneeachtoassessqualityoflifeand overallhealth.Thescorerangesfrom0to100(0=theworst health statusand100=thebesthealthstatus),exceptfor thesymptomscalesinwhichhigherscoresrepresentmore symptomsandworsequalityoflife.TheEORTCQLQ-C30uses modules withanucleus ofthe generic questionnaire, fol-lowedbyacombinationofmodulesforspecificdiseases.The EORTC QLQ-C30 is followedby the BreastSpecific Module (BR-23), whichevaluates specificaspectsofbreast cancer (Tables7and8).
Second
phase
results
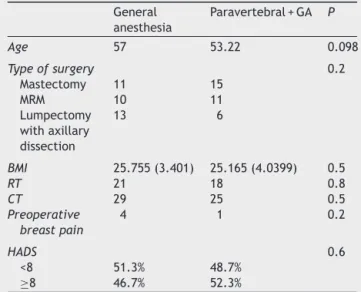
Regarding bothgroups comparisonin thesecond phase,it can besaidthatdemographiccharacteristics, suchasage andBMI, arerelativelyhomogeneousand thattherewere nosignificantdifferencesbetweenthetwogroupsregarding thesevariables.
Questionnaire for neuropathic pain diagnosis: DN4,
Interview of the patient
Examination of the patient
Score
Question 1: Does the pain have one or more of the following characteristics?
Question 2: Is the pain associated with one of more of the following symptoms in the same area?
Question 3: Is the pain located in an area where the physical examination may reveal one or more of the following characteristics?
Question 4: In the painful area, can the pain be caused or increased by: 1- Burning
Yes
Yes
No
No
No 2- Painful cold
3- Electric shocks
4- Tingling 5- Pins and needles 6- Numbness 7- Itching
8- Hypoesthesia to touch
10- Brushing
0 – For each negative response 1 – For each positive response
Neuropathic pain: Total score from 4/10.
( ) Nociceptive pain ( ) Neuropathic pain Yes
No Yes
9- Hypoesthesia to prick
Please complete this questionnaire by ticking one answer for each number:
Figure1 Questionnaireforneuropathicpaindiagnosis:DN4,validatedforPortuguese.
Table7 EORTCQLQ-C30.
EORTCQLQ-C30
Generalscale
-Globalhealthstatusandqualityoflife Functionalscale
-Physicalfunctioning -Roleperformance -Emotionalfunctioning -Cognitivefunctioning -Socialfunctioning Symptomaticscale
-Fatigue -Pain
-Breathlessness -Insomnia
-Lackofappetite;constipation,diarrhea; nausea/vomiting
-Financialdifficulties
Of the 66 evaluated patients, 10 were diagnosed with pain characteristic of intercostobrachial neuralgia (seven inthegeneral anesthesiagroupandthreein the paraver-tebral group),although the differencewasnot significant (p=0.3).
Regarding the EORTC-QLQ C30 score, we found that patientsintheparavertebralgrouphadthehighestscores in both overall quality of life and in the five functional scales,althoughitwasstatisticallysignificantonlyforsocial function.Intheevaluationofsymptoms,theparavertebral group had lower values compared to the general anes-thesia group, although it was not statistically significant (Table10).
Table8 EORTCQLQ-BR23.
QLQ-BR23
Functionalscale -Bodyimage -Sexualfunctioning -Sexualpleasure -Perspectives Symptomaticscale
-Chemotherapyeffects -Breastsymptoms -Armsymptoms -Concernwithhairloss
Table9 Variablesrelated topainchronicityinthestudy secondphase.
General anesthesia
Paravertebral+GA P
Age 57 53.22 0.098
Typeofsurgery 0.2
Mastectomy 11 15
MRM 10 11
Lumpectomy withaxillary dissection
13 6
BMI 25.755(3.401) 25.165(4.0399) 0.5
RT 21 18 0.8
CT 29 25 0.5
Preoperative breastpain
4 1 0.2
HADS 0.6
<8 51.3% 48.7%
≥8 46.7% 52.3%
Discussion
This study intended to know if with an easy to perform technique,suchasparavertebralblock,andwithlittle dis-comforttothepatient,suchasthesingle-injection,agood managementofacutepaincouldbeachievedandifitwould helptoachievealowerincidenceofpaininthe intercosto-brachialnerveareainthelongrun.
Inthefirstphase ofourstudy itwasseen adecreased VASscoreintheparavertebralgroupforpainatrestandon movement.Thedurationoftheanestheticblockatrestwith significantscoresonlyattimes0---6showsshortertimes com-paredtootherpublishedstudies.Thiscouldberelatedtothe lower concentrations of adrenaline used,which decrease thetime-effectofthelocalanesthetic.Althoughforpainon movement,theparavertebralgrouphadsignificantlylower VASscoreover24h.
The decreased consumption of opioidsboth intraoper-atively (fentanyl) and postoperatively (morphine) in the paravertebralgroupdemonstratestheeffectivenessofthe single-injection paravertebral technique for postoperative acute pain management without serious complications and improves comfort and hospital discharge of patients.
Thecases ofPONV seen inboth groups throughout the studywerelessthanexpectbasedonthetypeofsurgeryand patients’characteristics.Thisdemonstratesthattheuseof a preventive protocol allowsreducing the onset of these eventswiththeconsequentcomfortforpatients.
Thesecondphaseofthestudyintendedtoevaluatethe incidence of intercostobrachial neuralgia. The evaluation wasperformedsix monthsafter surgerybecauseradiation canworsenthepainfulsymptomsfromthatmoment.
The diagnosis was based on clinical assessment of patientsphysicallypresent,withtheDN4scale application
Table10 ResultsofEORTCQLQ-C30.
Generalanesthesia(%) Paravertebral(%) p
Qualityoflife 60±18.4 63±20 0.52
Physicalfunction 80.1±16.7 84.3±13.5 0.36
Roleperformance 77±26.2 81.2±22.6 0.55
Emotionalfunction 69.3±25.4 73.2±19.7 0.63
CognitiveFunction 82.3±20.5 83.8±16.6 0.99
Socialrole 82.3±22.8 92.2±14 0.043
Tiredness 30±23.14 20±18 0.12
Pain 21±24.3 13.5±20.5 0.2
Insomnia 30.4±28.8 18.7±23.8 0.8
Table11 ResultsofEORTCQLQ-BR23.
Generalanesthesia(%) Paravertebral+GA(%) p
Bodyimage 74±23.3 78.6±23.4 0.4
Perspectives 42.1±36 39.5±36.3 0.8
Treatmentsideeffects 25.6±17.1 19.7±17.7 0.15
Breastsymptoms 14.9±16.2 12±12.1 0.55
tocharacterizethetypeofpain.Weareawarethatthis trav-elingtoanewconsultationcausedthelossofsomepatients forthesecondphase.
Inthisstudy,weachievedhomogenization ofthe inter-costobrachialneuralgia conditioning characteristics in the sample.ThestudiesbyTasmuthetal.19reportadecreasein
painwhentheintercostobrachialnerveispreserved.Other studies20 didnot achieve thesame result,so theinternal
policyofoursurgicalteamremainsthenon-preservationof theintercostobrachialnerve.
Inthefirstphaseofourstudy,therewasless consump-tionof opioidsin theGA andPVBgroups, this is thebest indicatorofbetteranalgesiccontroland,accordingtothe meta-analysisperformedbyOngetal.,itisthebest indica-toroftheanalgesiapreventiveeffects.
However, the resultof our study shows that thereare statistically significant differences in the developmentof intercostobrachialneuralgiabetweengroups.The intercos-tobrachialnerveis athoracicnerveoriginatinginT2.The technique used in this study wasa single-injection at T4 level.Weknowthatthespreadofsolutionwiththe single-injection technique is erratic, a reasonwhy groups, such asGreengrassetal.,advocatethemultiple-injection tech-nique in surgical anesthesia. For this reason, we believe thatthesingle-injectionparavertebralblocktechniquehasa patchyandpoorlyreproducibledistributionandconditions thelocalanestheticarrival, ornot,at T2at asufficiently long time toavoid a centralsensitization that favors the onsetofpostoperativechronicpain,specifically intercosto-brachialneuralgia.
Becausethesamplewascalculatedbasedonthe evalua-tionof acute painin the immediatepostoperative period and there were a loss of patients for the second phase, inadditiontoalowerthan expectedincidenceofchronic pain,morestudiestoassesschronicintercostobrachial neu-ralgiaaftermajorbreastsurgeryareneededtoevaluatethe possiblebenefitsofthistechnique.
Summary
A prospective observational study with a sample of 80 patientsstratifiedintotwogroupsof40patientseach.The groupswerehomogeneous,withnostatisticallysignificant differencesinage,typeofsurgery,HADS,BMI,presenceof breastpainbeforesurgery,andfamilysupportvariables.All thesearefactorsfrequentlyreportedasindependent varia-blesforthedevelopmentofacuteand/orchronicpain.The study aim wastocompare two differentanesthetic tech-niquesfor breastsurgery: asingle-injection paravertebral blocktechniqueassociated withgeneralanesthesiaversus general anesthesia technique alone. The study was per-formedover24hintheimmediatepostoperativeperiodand a second evaluation six monthsafter surgery. The single-injection paravertebral block allows adequate control of acutepainwithlessintraoperativeandpostoperative con-sumptionofopioidsinthefirst24h,butapparentlyitcannot preventpainchronicity,particularlyintercostobrachial neu-ralgia.Morestudiesareneededtoestablishthebeneficial effects of paravertebral block in painchronicity in major breastsurgery.
Conflicts
of
interest
Theauthorsdeclarenoconflictsofinterest.
Acknowledgement
To theAssociac¸ãoPara o Estudo daMedicina deCuidados IntensivosdeOncologia(APEMCIO).
References
1.Ferlay J, Autier P, Boniol M, et al. Estimates of the can-cer incidence and mortality in Europe in 2006. Ann Oncol. 2007;18:581---92.
2.KwanW,JacksonJ,WeirLM,etal.Chronicarmmorbidityafter curativebreastcancertreatment:prevalenceand impacton qualityoflife.JClinOncol.2002;20:4242---8.
3.ApfelCC,GreimCA,HaubitzI,etal.Ariskscoretopredictthe probabilityofpostoperativevomitinginadults.Acta Anaesthe-siolScand.1998;42:495---501.
4.JaffeSM,CampbellP,BellmanM,etal.Postoperativenausea andvomitinginwomenfollowingbreastsurgery:anaudit.Eur JAnaesthesiol.2000;17:261---4.
5.MacraeWA.Chronicpainaftersurgery.BrJAnaesth.2001;87: 88---98.
6.IglehartDJ,KalinCM.Diseasesofthebreast.In:TownsendCM, editor.Sabistontextbookofsurgery.16thed.Philadelphia:WB Saunders;1992.p.136---8.
7.BethFJ,GretchenMA,OaklandercAL,etal.Neuropathicpain following breast cancer surgery: proposed classification and researchupdate.Pain.2003;104:1---13.
8.TasmuthT,KatajaM,BlomqvistC,etal.Treatmentrelated fac-torspredisposingtochronicpaininpatientswithbreastcancer: amultivariateapproach.ActaOncol.1997;36:625---30. 9.Sessler DI, Ben-Eliyahu S, Mascha EJ, et al. Can regional
analgesiareduce theriskof recurrence afterbreastcancer? Methodologyofamulticenterrandomizedtrial.ContempClin Trials.2008;29:517---26.
10.ExadaktylosAK,BuggyDJ,MoriartyDC,etal.Cananesthetic techniqueforprimarybreastcancersurgeryaffectrecurrence ormetastasis?Anesthesiology.2006;105:660---4.
11.Moller JF, Nikolajsen L, Rodt SA, et al. Thoracic paraverte-bralblockforbreastcancersurgery:arandomizeddouble-blind study.AnesthAnalg.2007;105:1848---51.
12.Schnabel A, Reichl SU, Kranke P, et al. Efficacy and safety of paravertebral blocks in breast surgery: a meta-analysis of randomized controlled trials. Br J Anaesth. 2010;105: 842---52.
13.Kairaluoma PM, Bachmann MS, Korpinen AK, et al. Single-injection paravertebral block before general anesthesia enhancesanalgesiaafterbreastcancersurgerywithand with-out associated lymph node biopsy. Anesth Anal. 2004;99: 1837---43.
14.KleinSM, Bergh A, SteeleSM,et al.Paravertebral blockfor breastsurgery.AnesthAnalg.2000;90:1402---5.
15.Pais-RibeiroJ,SilvaI,FerreiraT,etal.Validationstudyofa Por-tugueseversionoftheHospitalAnxietyandDepressionScale. PsycholHealthMed.2007;12:225---37.
16.EasonMJ,WyattR.Paravertebralthoracicblock---areappraisal. Anaesthesia.1979;34:638---42.
17.Santos JG, Brito JO, de Andrade DC, et al. Translation to PortugueseandvalidationoftheDouleurNeuropathique4 ques-tionnaire.JPain.2010;11:484---90.
quality-of-lifeinstrumentforuseininternationalclinicaltrials inoncology.JNatlCancerInst.1993;85:365---76.
19.TasmuthT,KatajaM,BlomqvistC,etal.Treatment-related fac-torspredisposingtochronicpaininpatientswithbreastcancer ---amultivariateapproach.ActaOncol.1997;36:625---30.