w w w . r b o . o r g . b r
Original
Article
Supra-acetabular
fixation
and
sacroiliac
screws
for
treating
unstable
pelvic
ring
injuries:
preliminary
results
from
20
patients
夽
Rodrigo
Pereira
Guimarães
∗,
Arthur
de
Góes
Ribeiro,
Oliver
Ulson,
Ricardo
Bertozzi
de
Ávila,
Nelson
Keiske
Ono,
Giancarlo
Cavalli
Polesello
FaculdadedeCiênciasMédicasdaSantaCasadeSãoPaulo(FCMSCSP),SãoPaulo,SP,Brazil
a
r
t
i
c
l
e
i
n
f
o
Articlehistory:
Received30September2014 Accepted6April2015 Availableonline2March2016
Keywords:
Surgicalprocedures,minimally invasive
Externalfixators Fracturefixation,internal Retrospectivestudies
a
b
s
t
r
a
c
t
Objective:Toanalyzethetreatmentresultsfrom20patientswhounderwentanalternative osteosynthesismethodasdefinitivetreatmentforpelvicringfractures.
Methods:Aretrospectiveanalysiswasconductedonaseriesof20patientswithpelvicring fractures(TiletypeC)andahighriskofpostoperativeinfection,whoweretreatedatSanta CasadeMisericórdiadeSãoPaulobetweenAugust2004andDecember2012.Thepatients underwentpercutaneoussupra-acetabularexternalfixationinassociationwithcannulated 7.0mmiliosacralscrews.
Results:Thepatients’meanagewas40years(range22–77years)andthemeanlengthof follow-upwas18.5months(range3–69months).Attheendofthetreatment,tenpatients (50%)wereclassifiedashavinggoodresults,ninepatients(45%)hadfairresultsandone patient(5%)didnothave anyimprovement.Sixpatientspresentedcomplications,and paresthesiaofthelateralfemoralcutaneousnervewasthemostfrequentofthese(two patients).
Conclusion:Supra-acetabularexternalfixationinassociationwithiliosacralpercutaneous osteosynthesisisagooddefinitivetreatmentmethodforpatientswithahighriskof post-operativeinfection.
©2016SociedadeBrasileiradeOrtopediaeTraumatologia.PublishedbyElsevierEditora Ltda.Allrightsreserved.
夽
WorkperformedintheHipGroup,DepartmentofOrthopedicsandTraumatology,FaculdadedeCiênciasMédicasdaSantaCasade SãoPaulo(FCMSCSP),IrmandadedeSantaCasadeMisericórdiadeSãoPaulo(ISCMSP),SãoPaulo,SP,Brazil.
∗ Correspondingauthor.
E-mail:clinicaguimaraes@gmail.com(R.P.Guimarães). http://dx.doi.org/10.1016/j.rboe.2016.02.010
Tratamento
das
lesões
instáveis
do
anel
pélvico
com
fixador
supra-acetabular
e
parafusos
sacroilíacos:
resultados
preliminares
em
20
pacientes
Palavras-chave:
Procedimentoscirúrgicos minimamenteinvasivos Fixadoresexternos Fixac¸ãointernadefraturas Estudosretrospectivos
r
e
s
u
m
o
Objetivo:Avaliarosresultadosdotratamentode20pacientesqueusaramcomotratamento definitivoummétododeosteossínteseopcionalparafraturasdoanelpélvico.
Métodos: Foifeitaumaanáliseretrospectivadasériede20casosdepacientescomfratura doanelpélvicotipoCdeTile,portadoresdealtoriscodeinfecc¸ãopós-operatória,tratados
naSantaCasadeMisericórdiadeSãoPauloentreagostode2004edezembrode2012, sub-metidosafixac¸ãoexternasupra-acetabularpercutâneaassociadacomparafusoscanulados iliossacraisde70mm.
Resultados: Amédiadeidadedospacientesfoide40anos(mínimode22;máximode77) eotempomédiodeseguimentofoide18,5meses(mínimodetrês;máximode69).Apóso términodotratamentodezpacientes(50%)foramclassificadoscombonsresultados,nove (45%)tiveramdesfechoregulareum(5%)nãoapresentoumelhoriaalguma.Seis apresen-taramcomplicac¸ões.Aparestesiadonervocutâneofemorallateralfoiamaisfrequente (doispacientes).
Conclusão: Afixac¸ãoexternasupra-acetabularassociadaaosteossíntesepercutânea ilios-sacral éum bommétodo detratamentodefinitivoparaospacientescomaltorisco de infecc¸ãopós-operatória.
©2016SociedadeBrasileiradeOrtopediaeTraumatologia.PublicadoporElsevier EditoraLtda.Todososdireitosreservados.
Introduction
Pelvicringfracturesformpartoftheroutinewithin trauma-tology.Occurrencesofhigher-energytraumaandinvolvement ofyoungadultsintheseaccidentsaremattersofconcern.1 Theassociatedtraumaticinjuriesoftenrequireneurosurgery,
abdominalsurgery, colostomy, drains and lengthy stays in
intensivecarecenters2–4andadddifficultytoorthopedic treat-ments.
Given that osteosynthesis in critical patients needs to beeffectiveandminimally invasive,oneoptionfortreating pelvicfracturesinthesepatientsmightbesupra-acetabular externalfixationinassociationwithsacroiliacpercutaneous fixation.
Theobjective of this study was to evaluate the results fromtreating20patientswithunstablefracturesofthepelvic ringwho underwentsurgeryconsistingofsupra-acetabular externalfixationinassociationwithsacroiliacpercutaneous fixation,betweenAugust2004andDecember2012.
Methodology
Aretrospectiveanalysiswasconductedonthemedicalfiles of20 patients with pelvicring fractures who were treated
between August 2004 and December 2012. These patients
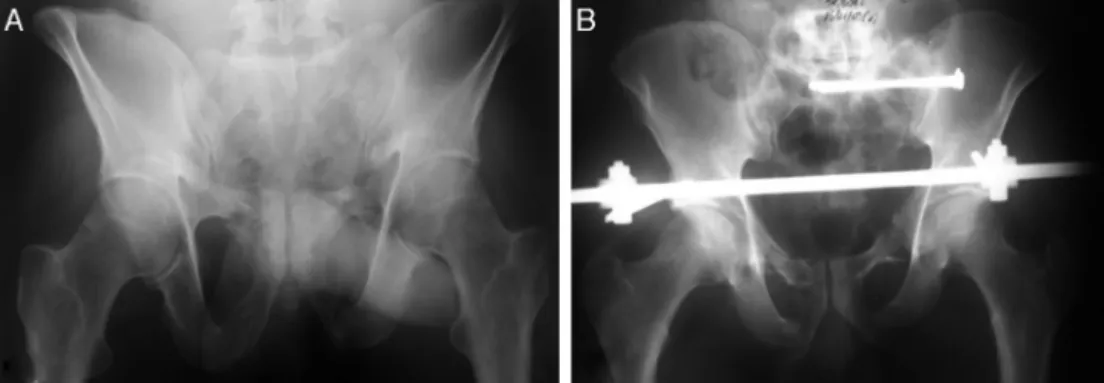
underwentfixationoftheanteriorregionofthepelvicring bymeansofsupra-acetabular pins andalsosacroiliac pins usingapercutaneoustechniquewithcannulated7mmscrews (Fig.1AandB).Thesurgicalfixationswereperformedduring thesameoperation.
The inclusion criteria were that the patients had to be adults, aged 18–80 years, with fractures classified as Tile typeC,5whopresentedariskofpostoperativecomplications withinternalosteosynthesis.Prolongedhospitalstay, decom-pensated clinical diseases, concomitant surgical diagnoses
(abdominal and/or pelvicsurgery)and presenceofostomy,
drainsandprobeswereconsideredtoberiskfactorsleadingto theneedforopenreductionandinternalfixationwithplates. Theexclusioncriteriawerepoorlyfilledoutmedicalrecords, patientsundertheageof18years,patientswithinjuries clas-sifiedasTiletypesAandB,patientstreatedwithoutsurgery, patientstreatedbymeansofosteosynthesiswithplatesand casesofdeathduringthepreoperativeperiod.
Theepidemiologicaldatadescribedweresex,age,trauma mechanism,associatedinjuriesandtheresultfromthe treat-mentswiththesurgicaltechniqueused.Theinjuriestothe pelvicring weredescribed asfracturesinthe rami(R), dis-junctionofthesymphysis(S)orbothofthesetogether(S+R), orasinjuriesofthesacroiliaccomplex(SI).Weconsideredthat casespresentedbilateralinjurywhenfractureswerepresent onbothsidesofthepelvicring.
Thefractureswereevaluatedusingradiographicand
tomo-graphic images, before and after the surgical treatment,
always bythree orthopedists.After the surgery,the reduc-tions werestratifiedasanatomical,displacedby1–5mmor
displacedmorethan5mm.
Theexternalfixatorswereremoved16weeksafterthe sur-gicaltreatment,exceptinonecaseinwhichthisdatehadto bebroughtforward.Noiliosacralscrewwasremovedduring thestudy.
Fig.1–(A)Imageofthepelvisinoutletview,showingfracturingofthepubicramiandthesacrumontheleft.(B) PostoperativecoronalimageofthepelviswithtwosacroiliacscrewsintheS1bodyandsupra-acetabularexternalfixator.
fair(returntoactivitieswithcomplaints)orpoor(noreturn toprevious activitiesand/orunsatisfactoryreturn).Wealso comparedtheseresultswiththepostoperativeradiographs.
Results
Twentypatientswerefollowedupforperiodsrangingfrom3 to69months.Themeanlengthoffollow-upwas18.5months (standarddeviation,SD,of19.99months).
Thepatients’meanagewas40years(minimumof22and maximumof77;SD:14.7).Elevenpatients(55%)weremale. Themaincausefoundwasbeingrunover(ten;50%),followed byfallingfromaheight(five;25%),carcrashes(three;15%)and accidentswithmotorcycles(two;10%).
Allofthe20caseswereTiletypeC.In18cases(90%),there wasfracturingofthepubicrami,whiledisjunctionofthe sym-physisoccurredinfivepatients(25%).Wefound15casesof R+SI(75%);threecasesofS+R+SI (15%);andtwocasesof S+SI(10%).
Theinjurywasbilateralintencases(50%).Twocases(10%) occurredsolelyontherightsideandeightcases(40%)onthe leftside.
Fourteenpatients (70%)presentedsome formof
associ-ated traumatic injury: one (5%) suffered severe traumatic
braininjuryalone;one(5%)sufferedtraumaticbraininjury and fracturesofthe extremities; one(5%)presentedinjury
to the urethra; one (5%) had an abdominal injury that
requiredlaparotomyand embolization;one(5%)underwent
cystostomy;three(15%)presentedabdominalandpelvic lac-erationsandhemorrhage,withlongstaysintheintensivecare unit;andsix(30%)presentedotherassociatedfracturesalone (Fig.2).Theothers(30%)haddiagnosesofpelvicfracturealone, butpresentedcontraindicationsforinternalosteosynthesis: three(15%)withpreviouslaparotomy;one(5%)with abdom-inalsurgeryandinfectionoftheurinarytract;one(5%)with underlyingcoagulopathy;andone(5%)withdeepinfectionon theskeletaltractionpins.
Anatomicalreductionwasachievedin14cases(70%).Two
cases(10%)continued topresent displacements of1–5mm
afterthereductionand,inthreecases(15%),thebestreduction obtainedstillpresentedadisplacementofmorethan5mm.
Complicationsoccurredinsixcases(30%):two(10%) pre-sentedneuropraxia ofthelateral femoralcutaneousnerve;
30 30
5 5
10
5
15
Severe traumatic brain injury
Traumatic brain injury with fractures of the extremities
Genitourinary injury
Abdominal injury
Multiple lacerations
Fractures of the extremities
Without associated traumatic injuries
Associated injuries
Fig.2–Presenceanddistributionofassociatedinjuriesat timeofpatients’admissiontohospital.
one(5%) presentedskewedconsolidationandevolvedwith
lumbosacral andsacroiliacpain; andone(5%)continuedto presentoccasionalsacroiliacpainalone.Therewasonecase (5%)ofpseudarthrosisofthepubicramiinassociationwith postoperativeinfection.Thispatientwastreatedwith intra-venousantibioticsandremovalofthesynthesismaterials,and evolvedwithlossofreduction.Onepatient(5%)continuedto presentleg-lengthdiscrepancy.Therewerenodeathsafterthe surgeryandtheremainingpatients(14;70%)didnotpresent anycomplications.
Overthe courseofthe clinicaloutpatientfollow-up, ten patients(50%)returnedtotheiractivitiesanddidnotreport anycomplaintsorlimitations.Thesepatientswereclassified aspresentinggoodresults.Nine(45%)continuedtohave occa-sionalcomplaints,characterizedmainlybydiffusepaininthe posterior region, and were classified ashavingfair results.
One patient(5%) saidthat therehad not beenany typeof
improvement, withcontinuinglumbalgia,muscle pain and
limbshortening,andwasclassifiedasapoorresult.
Discussion
highermortality,9 andsurvivorshaveahighchanceof hav-ingtolivewithsomeformofpermanentsequela.4Surgical treatmentoftheseinjuriesduringtheacutephaseprovides thebestresults1–3,10andenablesrehabilitationwithareturn tocommunitylife.
Pelvic fixation can be done using plates or external
fixators.11 Fractures classified asTile type Bor C are pref-erentiallytreatedby means ofrigidinternalfixation,12 but directreductiongivesrisetogreateroperativetrauma,blood lossandriskofinfection,13 andforthisreasonneedstobe consideredon acase-by-casebasis.11,12 Thus,patients ina moresevereconditionand/orpresentingcolonizationby resis-tantmicroorganismsofintensivecareunitsmaybebenefited throughminimallyinvasiveorthopedictreatment.
Use of external fixators for the pelvis dates from the
1950s.14 Several studies have now attempted to
estab-lish a more versatile, safer and more resistant means of
construction,14–16 but there is still no consensus in this regard.17 Anterosuperior assemblies (above the iliac crest) andanteroinferiorassemblies(supra-acetabular)aretheones mostusedused.14
Thesupra-acetabular methodismorestableand longer
lasting,and it needsfew incisions.Thetechniquerequires theaidofradioscopy.EachSchanzpinispositionedcranially tothe hopjoint and slightly laterally tothe anteroinferior iliac spine,oriented toward the greater sciatic notch.3 The stabilization is completed anteriorly by one or two bars. Careisneeded,soasnottoinjurethelateralfemoral cuta-neousnerve,nottopositionthepinwithinthejointandnot to invade the greater sciatic notch. A safety zone for pla-cingthepinshasbeendescribed bysomeauthors.14–16 The small cutsin the skin and the lesser degree of
manipula-tion ofthefracture makethis anadvantageous method in
comparisonwith the traditional access routes for internal fixation.
Sacroiliacosteosynthesisisessentialincasesclassifiedas TiletypeC,12and severaltypesofimplant formpartofthe therapeuticarsenal.18,19
Percutaneousfixationissimpleand effective,andisthe preferredmethodinthemajorityofthe cases.20,21 Asingle 7.0mmcannulatedscrewisusuallysufficient,buttwoscrews maybeusedwhenthereisgreaterinstability.18,20Inthe opera-tivetechnique,correctimplantpositioningwiththethreaded endinsidetheS1bodyisfundamental.18Somestudieshave shown that intraoperativedifficulties exist in situations of anatomicalvariationsofthesacrumandinadequate fluoro-scopicimages.22,23
Themeanageof40yearsfoundinourresultswassimilarto thedataintheliterature,1,8aswasalsothefrequencyof occur-rencesaccordingtosex(55%male).Inoursample,accidents withvehiclesaccountedfor75%ofthecasesthatweretreated usingthemethoddescribedhere,butmotorcycleaccidentsdid notaccountforthemajorityofthesecases.
Although sacroiliac dislocation, sacral fractures and
growthfracturesaredifferentinjuries,theywereconsidered togetherinthesamegroup(SI),soastohaveabetter group-ing forstatistical comprehension. There would not beany advantageinseparatingthemaccordingtotheirnature,given thatallofthemareverticallyunstablefracturesthatrequire osteosynthesisoftheposteriorregion.
Wefoundthatupto50%ofthepatientspresentedother associatedinjurieswhentheyarrivedatthehospital,which reflectstheseverityofthesecasesandcorroboratestheneed fordifferentiatedattendance.Thisproportionisinlinewith data established inthe literature.1,3,8 However, despite the severityofthesepatients’condition,noneofthem deterio-ratedtodeathaftertheorthopedicsurgery.
Insixcases(30%),thereductionobtainedwasnot anatom-ical.Thisnumberwasexpected,sincetheseweresevereand unstable fractures,whichcontributedtowardthe incongru-ence.However, this resultwas amatter ofconcern forus, becausechronicpainisusuallyaprobleminthesepatients. Inastudyon102patientswhounderwentfixationbymeans of a sacroiliac screw, 88% presented reductions that were
anatomical or close toanatomical, 12% presented residual
incongruence of1cm or moreand, over the courseof the
follow-up,eightpatientspresenteddisplacementofthe reduc-tionthathadbeenobtained.21McLarenetal.24showedthat twothirdsoftheirpatientspresentedpainincaseswithfinal incongruencegreaterthan1cm,while88%hadminimalpain
whentheincongruenceremainedlessthan1cm.Thus,they
demonstratedthatseekingtoachieveanatomicalreductionis anecessity.
In ourstudy,the functional resultsobtained were simi-lartothose from techniquesthat are acceptedasthe gold standard,8,12,17 with 50% of the results classified as good. Ninepatients(45%)presentedfairresultsdespite consolida-tion ofthe fractures and returningto work activities.Only onepatient(5%)hadapoorresult,inwhichaleg-length
dis-crepancyof5cmremainedandtherewasnoimprovementin
thesymptoms.Thispatientwastreatedthroughtheuseof
insolesandfootwearwithacompensatoryheel.Today,this
patient continues tocomplain ofpain, but is managingto
work.Clinicalandradiologicalcomparisonsshowedthatthere was a directcorrelation between the quality ofthe
reduc-tion and the presence ofsymptoms during the outpatient
follow-up.
The injury complication rate through the method
pre-sented here reached 30% (six cases). The most frequent
complicationswere paresthesiaofthelateral femoral cuta-neousnerve(twopatients)andsacroiliacpain(two).Thetwo
patientswithparesthesiapresentedcompleteimprovement
of the condition. Apraxia may occur during the dissection
or introduction oftheSchanz pins andit incidenceduring externalfixationis2%.25Noneofourpatientspresented neu-ropraxiaoftherootofL5.Theneurovascularinjuryrateduring positioning oftheiliosacral screwranges from2to 15%in the literature.26 Rysav ´y et al.21 reported occurrences of L5 injury in 6%, with complete remission ofthe deficit in all the cases.Moed andWhiting19 didnotreportanycasesof neurologicalinjuriesintheirstudyontencases,after oper-ative treatmentonposteriorinjuriesofthepelvicring.Gao etal.27didnotfindanycasesofneurological,vascularor uro-logicalinjuriesamong17patientswhounderwentsacroiliac osteosynthesis.
The patients with traumatic brain injury evolved well, withoutneurologicaldeficits,andwereabletoreturntothe activitiesthattheydidbeforetheaccident.
The patient who presented urethral injury
dilatation and periodic follow-up with a urologist. The
patient who underwent cystostomy evolved satisfactorily
during the follow-up and did not have any
complica-tions.
Onepatientpresenteddeepinfectionthatrequiredremoval ofthefixatorandcurettageoftheorifices,whichwasdone
in a sterile environment, under anesthesia. He presented
displacementofthepelvicfracture.Noneoftheother19 fixa-torsthatremainedinplacethroughoutthe16weeksevolved withany deepinfection.Thismakesit clearthatlocalcare isfundamental.Livingwithanexternalfixatorinthehome environmentisburdensome,becauseactivitiesofdailyliving becomeimpairedandthepatientrequiresconstantassistance fromotherpeople.
Thisstudy presents some limitations:it was retrospec-tive;thedataweregatheredfrommedicalfiles;andalthough
the inclusion criteria were very clear, the number of 20
patientsmayhavebeeninsufficienttoportraythereality.The
assessmentsonthe patients were subjectiveand were not
characterizedthroughscores.Nonetheless,thepatients’ com-plaintsand degreeofsatisfaction,and whetherornotthey returnedtotheirworkactivities,areevidentinthemedical records.Thisstudylacksstatisticaldataofgreaterrobustness, butthisdoesnotinvalidateitsimportance,giventhatit high-lightsanother possibilityfordefinitivetreatment forpelvic fractures.
Thepositivepointsfromthisstudyarethatitreportson aseries of20casesthat were definitivelytreatedusing an optionalmethodthat isinexpensive, rapidlyimplemented, efficientandavailableinmosthospitals.Thisstudy demon-stratedclinicalandradiographicresultssimilartotheopen techniquesforinternalfixationandcouldbeeasilyreproduced inotherhospitalservices.
Conclusion
Supra-acetabularexternalfixationinassociationwith percu-taneoussacroiliac osteosynthesisusing 7.0mmcannulated screwsforfracturesclassifiedasTiletypeCisagoodoption foruseasadefinitivetreatmentforpatientswithahighrisk ofpostoperativeinfection.
Multicenter randomized prospective studies with larger numbersofpatientsareneededforbettercomprehensionand treatmentofthesepatients.
Conflicts
of
interest
Theauthorsdeclarenoconflictsofinterest.
Acknowledgements
WearedeeplygratefultoProf.Drs.EmersonKiyoshiHonda, WalterRicioliJúniorand MarceloCavalheiro deQueirozfor theirsupport,encouragementandgreatdedicationduringthe study.
r
e
f
e
r
e
n
c
e
s
1.AmericanCollegeofSurgeons.CommitteeonTrauma.In: Advancedtraumalifesupport(ATLS).8thed.Chicago,IL: AmericanCollegeofSurgeons;2008.
2.TileM.Introductionandnaturalhistoryofthepelvicring.In: TileM,HelfetDL,KellanJF,editors.Fracturesofthepelvisand acetabulum.3rded.Philadelphia:LippincottWilliam& Wilkins;2003.p.3–11.
3.StoverMD,MayoKA,KellamJF.Pelvicringdisruptions.In: BrownerBD,JupiterJB,LevineAM,TraftonPG,KrettekC, editors.Skeletaltrauma:basicscience,management,and reconstruction.4thed.Philadelphia:SaundersElsevier;2009. p.1107–69.
4.GruborP,MilicevicS,BiscevicM,TanjgaR.Selectionof treatmentmethodforpelvicringfractures.MedArch. 2011;65(5):278–82.
5.PennalGF,TileM,WaddellJP,GarsideH.Pelvicdisruption: assessmentandclassification.ClinOrthopRelatRes. 1980;(151):12–21.
6.PerryJFJr.Pelvicopenfractures.ClinOrthopRelatRes. 1980;(151):41–5.
7.HolsteinJH,CulemannU,PohlemannT.Whatarepredictors ofmortalityinpatientswithpelvicfractures?ClinOrthop RelatRes.2012;470(8):2090–7.
8.GiannoudisPV,GrotzMR,TzioupisC,DinopoulosH,WellsGE, BouamraO,etal.Prevalenceofpelvicfractures,associated injuries,andmortality:theUnitedKingdomperspective.J Trauma.2007;63:875–83.
9.CohenMT,GuimarãesJM,MottaFilhoGR,CohenJC,Goldsztjn F,GuimarãesFM.Fixac¸ãopercutâneacomparafusoiliossacral nalesãotraumáticadoanelpélvico.RevBrasOrtop.
2005;40(1/2):32–41.
10.PapakostidisC,KanakarisNK,KontakisG,GiannoudisPV. Pelvicringdisruptions:treatmentmodalitiesandanalysisof outcomes.IntOrthop.2009;33(2):329–38.
11.GorczycaJ,HearnT,TileM.Biomechanicsandmethodsof pelvicfixation.In:TileM,HelfetDL,KellanJF,editors. Fracturesofthepelvisandacetabulum.3rded. Philadelphia:LippincottWilliam&Wilkins;2003. p.116–29.
12.TileM,RubensteinJ.Definingtheinjury:assessmentofpelvic fractures.In:TileM,HelfetDL,KellanJF,editors.Fracturesof thepelvisandacetabulum.3rded.Philadelphia:Lippincott William&Wilkins;2003.p.102–15.
13.MoedBR,KellamJF,McLrenA,TileM.Internalfixation fortheinjuriedpelvicring.In:TileM,HelfetDL,KellanJF, editors.Fracturesofthepelvisandacetabulum.3rded. Philadelphia:LippincottWilliam&Wilkins;2003. p.217–93.
14.KimWY,HearnTC,SeleemO,MahalingamE,StephenD,Tile M.Effectofpinlocationonstabilityofpelvicexternal fixation.ClinOrthopRelatRes.1999;(361):237–44. 15.TileM.Describingtheinjury:classificationofpelvicring
injuries.In:TileM,HelfetDL,KellanJF,editors.Fracturesof thepelvisandacetabulum.3rded.Philadelphia:Lippincott William&Wilkins;2003.p.135–49.
16.SolomonLB,PohlAP,SukthankarA,ChehadeMJ.JOrthop Trauma.2009;23(5):365–9.
17.WolinskyP,StephenD.Femur,shaft(incl.subtrochanteric fractures).In:RüediTP,MurphyWM,editors.AOprinciplesof fracturemanagement.2nded.Stuttgart:ThiemePublishing Group;2007.p.778–99.
19.MoedBR,WhitingDR.Lockedtranssacralscrewfixationof bilateralinjuriesoftheposteriorpelvicring:initialclinical series.JOrthopTrauma.2010;24(10):616–21.
20.vanZwienenCM,vandenBoschEW,SnijdersCJ,Kleinrensink GJ,vanVugtAB.Biomechanicalcomparisonofsacroiliac screwtechniquesforunstablepelvicringfractures.JOrthop Trauma.2004;18(9):589–95.
21.Rysav ´yM,PavelkaT,KhayarinM,DzupaV.Iliosacralscrew fixationoftheunstablepelvicringinjuries.ActaChirOrthop TraumatolCech.2010;77(3):209–14.
22.MillerAN,RouttMLJr.Variationsinsacralmorphologyand implicationsforiliosacralscrewfixation.JAmAcadOrthop Surg.2012;20(1):8–16.
23.GravesML,RouttMLJr.Iliosacralscrewplacement:are uniplanarchangesrealisticbasedonstandardfluoroscopic imaging?JTrauma.2011;71(1):204–8.
24.McLarenAC,RorabeckCH,HalpennyJ.Long-termpain anddisabilityinrelationtoresidualdeformityafter displacedpelvicringfractures.CanJSurg.1990;33(6): 492–4.
25.RiemerBL,ButterfieldSL,DiamondDL,YoungJC,RavesJJ, CottingtonE,etal.Acutemortalityassociatedwithinjuriesto thepelvicring:theroleofearlypatientmobilizationand externalfixation.JTrauma.1993;35(5):671–5.
26.HinscheAF,GiannoudisPV,SmithRM.Fluoroscopy-based multiplanarimageguidanceforinsertionofsacroiliacscrews. ClinOrthopRelatRes.2002;(395):135–44.