REVISTA
BRASILEIRA
DE
ANESTESIOLOGIA
PublicaçãoOficialdaSociedadeBrasileiradeAnestesiologiawww.sba.com.br
SCIENTIFIC
ARTICLE
Faster
onset
time
of
supraclavicular
brachial
plexus
block
using
local
anesthetic
diluted
with
dextrose
夽
Hong
Jin
Lim
a,
Mohd
Shahnaz
Hasan
a,∗,
Karuthan
Chinna
baDepartmentofAnesthesiology,FacultyofMedicine,UniversityofMalaya,50603KualaLumpur,Malaysia
bJuliusCentreUniversityMalaya,DepartmentofSocialandPreventiveMedicine,FacultyofMedicine,UniversityofMalaya,
50603KualaLumpur,Malaysia
Received21September2014;accepted11November2014
Availableonline27October2015
KEYWORDS
Ultrasound; Supraclavicular; Brachialplexus; Block;
Saline; Dextrose
Abstract
Backgroundandobjectives: A highsodiumconcentration isknowntoantagonizelocal anes-theticswheninfiltratedaroundneuraltissue.Thus,wehypothesizedthattheonsettimefor sensoryandmotorblockade,insupraclavicularbrachialplexusblockusingropivacainediluted withdextrosewouldbeshorterthanwithsaline.
Methods:Patientsscheduled forupper limbsurgerywererandomizedtoreceiveultrasound guidedsupraclavicularbrachialplexusblockwith0.5%ropivacaine.Evaluationofsensoryand motorblockadewasperformedevery5minfor60min.Patientswerefollowed-upon postop-erativeday1,andbetweendays7and10forthepresenceofanycomplications.Twenty-five patientsineachgroupwereanalyzed.
Results:Meantimeforonsetofanalgesiaforthedextrosegroupwas37.6±12.9minwhilethe meantimeforthesalinegroupwas45.2±13.9minwithap-valueof0.05.Theeffectsizewas 0.567,whichwasmoderatetolarge.Nomajorcomplicationswereobserved.
Conclusion: Weconcludethattherewasadecreaseinonsettimeofanalgesiawhendextrose wasusedasadiluentinsteadofsalineforultrasoundguidedsupraclavicularblock.
©2015SociedadeBrasileiradeAnestesiologia.Publishedby ElsevierEditoraLtda.Thisisan openaccessarticleundertheCCBY-NC-NDlicense( http://creativecommons.org/licenses/by-nc-nd/4.0/).
夽 Workattributedto:DepartmentofAnesthesiology,FacultyofMedicine,UniversityofMalaya,50603KualaLumpur,Malaysia.
∗Correspondingauthor.
E-mail:shahnaz@ummc.edu.my(M.S.Hasan). http://dx.doi.org/10.1016/j.bjane.2014.11.012
PALAVRAS-CHAVE
Ultrassom; Supraclavicular; Plexobraquial; Bloqueio; Soluc¸ãosalina; Dextrose
Tempomaisrápidodeiníciodobloqueiodoplexobraquialsupraclavicularusando anestésicolocaldiluídocomdextrose
Resumo
Justificativaeobjetivos: Aaltaconcentrac¸ãodesódioéconhecidaporantagonizar anestési-cos locaisquandoinfiltrado emtornode tecidoneural.Portanto, anossahipótese foiade que otempo de início para osbloqueios sensorial emotor, em bloqueio do plexobraquial supraclavicular usando ropivacaínadiluída com dextrose,seria menor do que com soluc¸ão salina.
Métodos: Ospacientesagendadosparacirurgiaemmembrosuperiorforamrandomizadospara receberbloqueiodoplexobraquialsupraclavicularcomropivacaínaa0,5%gguiadopor ultra-ssom.Aavaliac¸ãodosbloqueiossensorialemotorfoirealizadaacada5minutosdurante60 minutos.Ospacientesforamacompanhadosnopós-operatórionoprimeirodiae,entreosdias 7-10parapresenc¸adequalquercomplicac¸ão.Foramanalisados25pacientesemcadagrupo. Resultados: Amédiadotempoparaoiníciodaanalgesianogrupodextrosefoide37,6±12,9 minutos,enquantoquenogruposoluc¸ãosalinaamédiafoide45,2±13,9minutos,comum valor-pde0,05.Otamanhodoefeitofoi0,567,oquefoidemoderadoagrande.Complicac¸ões maioresnãoforamobservadas.
Conclusão:Concluimosquehouveumareduc¸ãodotempodeiníciodaanalgesiaquandodextrose em vezde soluc¸ão salinafoiusada como diluente para bloqueiosupraclavicularguiado por ultrassom.
©2015SociedadeBrasileiradeAnestesiologia.PublicadoporElsevierEditoraLtda.Este ´eum artigoOpen Accesssobumalicenc¸aCCBY-NC-ND( http://creativecommons.org/licenses/by-nc-nd/4.0/).
Introduction
Regional anesthesiawith local anesthetics blocks specific nervestoenablepainfreesurgery,orforintra-and postop-erativepainrelief.Dilutionoflocalanestheticswithnormal saline is a common practice to enable administration of larger volumes of local anesthetics particularly in cases whereby multiple nerve blocksare needed. This will also minimizetheriskofsystemictoxicity.
Localanestheticsblockthefunctionofsodiumchannels locatedinneuraltissue,inhibitingdepolarizationandthus thetransmissionofnerveimpulses.1Ahighsodium concen-trationisknowntoantagonizetheanalgesiceffectoflocal anesthetics.2 On the other hand, dextrose when injected aroundnervoustissuedoesnotcauseanypainoninjection anddoesnotcauseanylongtermneurologicaldeficitin ani-malsorhumans.3---5Dilutionwithdextrosewouldreducethe concentrationofsodiumionsandhencereduceits antago-nisticeffect.Intheliterature,onlyonestudyusingdextrose asdiluenttoproduce0.5%ropivacaineforaxillarybrachial plexusblockshowedareductionintheonsettimefor sen-soryblockadewhencomparedwithdilutionwithsaline.6Our hypothesis wasthat dilution ofthe local anesthetics with dextrosewouldshortentheonsettimecomparedtosaline forasupraclavicularbrachialplexusblock.
In the present randomized and blinded clinical study, 0.75%ropivacainewasdilutedwithdextroseorsalineto pro-duce0.5%ropivacaine,forultrasoundguidedsupraclavicular brachialplexusblock.Theprimaryaimwastocomparethe onsettimefor complete analgesia and motorblockade in both groups. Analysis withregardsto the durationof the neuralblockadewasalsocarriedout.
Methods
This clinical study was registered at clinicaltrials.gov (ID no.NCT01815944).Afterobtainingapprovalfromthe Medi-cal Ethics Committee, University Malaya Medical Centre (Ethicscommittee/IRBreferenceno.883.11dated19 Octo-ber2011),patientsagedbetween18and85yearswhowere ASA I toIII, scheduled for elective or emergency surgery of thehand, forearmand elbowwereevaluatedfor eligi-bility tobe enrolledin the study.Patientswereexcluded if they had a history of diabetes mellitus, any neurolog-ical deficit, contraindications to supraclavicular brachial plexusblockade,wereunabletogiveconsent,orrefusedto participate.
Uponobtainingwritteninformedconsent,patientswere randomly assigned to either the dextrose (D5%) or nor-malsaline(NS)group.Randomizationwasperformedusing a computer-generated random table and patients were blindedastotheirgroupallocation.Groupallocationswere concealed in a sealedopaque envelopeand were opened byanindependentanesthesiologistjustbeforethe perfor-mance of the block. The same anesthesiologist prepared 20mL 0.5% ropivacaine bydiluting 13.3mL of 0.75% ropi-vacaine with 6.7mL of either dextrose or normal saline, dependingonthepatient’sgroupallocation.
An anesthesiologist familiar with the technique, who wasblindedtogroupallocation,performedall ultrasound-guidedsupraclavicularblocks.Priortotheblock,allpatients were placed supine on a trolley and were equipped with routine monitoring, i.e. ECG, SpO2, NIBP, and a
torelieveanxietybut nottothepoint ofbeingunableto respondclearly.
AfterthebrachialplexuswasidentifiedusingaSonosite M-Turbo ultrasoundmachine and a 13---6MHz linear probe (Sonosite®, Bothell,WA, USA),theadjacent skinareawas
cleaned with povidone iodine and draped. Under asep-tic technique, a sterile 22G, 50mm short bevel needle (Stimuplex®,BBraun,Melsungen,Germany)wasguided
in-plane withthe ultrasound beamtoward the plexus. Once at theappropriatelocation,localanestheticwas adminis-teredincrementally,eachtimeafteranegativeaspiration, ensuringexpansionandadequatespreadaroundthebrachial plexus.Atotalof19mLoflocalanestheticwasgiveneach time;1mL fromthe initial 20mL prepared being usedto primethecatheterfortheneedle.
Evaluationofsensoryandmotorblockadewasthen car-ried out. The same anesthesiologist who performed the blocksandwasblindedtogroupallocationdidevery eval-uation. Sensory and motor blockade were tested, after injection of the local anesthetic, every 5min until total analgesia was obtained in all four nerve distributions, or up till 60min, whichever was earlier. Sensory loss was testedinthemedian,radial,ulnar,andmusculocutaneous nervedistributionsandevaluatedusingathreepointscore: two=normal, one=analgesia, i.e. loss of pinprick sensa-tion,orzero=anesthesia,i.e.totalsensoryloss.Theextent of motor blockade was tested in the distribution of the radial(thumbabduction,fingerandwristextension),ulnar (thumbadduction),musculocutaneous(flexionoftheelbow in supination and pronation), and median nerves (thumb opposition)andevaluatedusingathree-pointscalewhere two=normalmovement,one=paresiswithsomemovement possible,andzero=totalparalysis.
Blocksuccesswasdefinedaslossofsensationtopinprick (sensory score one) in each of the radial, ulnar, median, andmusculocutaneousnervedistributions,measureduptill 60minaftertheendoflocalanestheticinjection.Patients inwhomblocksuccesswasnotachievedafter60minwere excludedfromdataanalysis.Theyweresubsequentlygiven appropriateindividualnerveblocksat theaxillaorelbow, or weregivengeneralanesthesiaprior toproceedingwith surgery.
Low-dose midazolam (1---3mg) and/or propofol at con-scioussedationdoses(25---75g/kg/min)weregivenduring surgeryaccordingtotheusualstandardofcareatour cen-ter.In theeventof inadequateanalgesia intraoperatively, boluses of fentanyl (1---2g/kg) were given, followed by conversiontogeneralanesthesiaifnecessary.Anyadverse eventswerenotedduringandaftertheblockperformance. The onsettimefor sensoryblockadewastakenastime from completion of injection of local anesthetic to time of complete analgesia in all four nerves. Time for motor blockade was taken as time from complete injection of localanesthetictotimeoftotalmotorblockofthenerves assessed.
During the postoperative recovery periodbefore being discharged tothe ward, pain (verbal response score four or patientrequest for analgesic) wastreated withIV tra-madol25---50mgslowboluswithorwithout fentanyl25g bolusesevery5minasneeded.Onceinthewardandwhen oral intake wasallowed, patients receivedoral paraceta-mol 1gwithoral diclofenac50mg or celecoxib200mg,if
notcontraindicated,whentheyfelttheslightestpainfrom theoperative site andrequested oral analgesics. Patients weretoldtonotethetimetofirstrequest foranalgesics. The block duration wassubsequently taken as time from completeanalgesiatothetimewhenthepatientfirstfeels theslightestpainfromtheoperativesiteandrequestsoral analgesics.
Patientswerefollowed uptwice; onpostoperativeday (POD)1 andonce between POD7---10. They were seen in thewardorwerecontactedviatelephoneandaskedforthe presenceofanypain,weakness,numbness,tingling,orany abnormalsensationintheoperativeextremity.Ifindicated, theywere then told to return tothe hospital for further evaluationandmanagementasnecessary.
The primary outcome measure for this study was the onsettimeofsensoryblockade definedasthetime inter-valbetweentheendoflocalanestheticinfiltrationandloss ofsensationtopinprick.Dhiretal.reportedamean differ-enceof4.2minintheonsettimebetweenthetwocompared groups. The pooledstandard deviation was6.25. Calcula-tionsbasedonthisstudyshowedthat25patientspergroup wereneededtodetectastatisticallysignificantdifference betweenthegroupswith˛=0.05andapowerof80%.
For patient demographics, descriptive statistics were used. For the onset time of sensory blockade, the independent-ttestwasused.Individualnerveblocktimes, totaldurationofblock,totalproceduretime,andonsettime fortotalparesiswerealsoanalyzedusingtheindependent t-test. Dataanalysiswasdone usingSPSSversion16(SPSS Inc.,Chicago,Illinois,USA).
We alsocalculatedthe effectsizevaluesin this study. Effect sizevalues aretypicallycomputed tocompare the effectsof differenttreatments.7It providesameasure to assessthemagnitudeofdifferencebetweengroupsthat can-notbeobtainedsolelybyfocusingonp-values.p-Valuesare dependent onboth the magnitudeof differencebetween groups andthe sample size. Therefore withother factors heldconstant,increasingthesamplesizeincreasesthe prob-ability of finding a statistically significant difference.8 In this study, effectsize values were calculated in addition top-values,toassessthemagnitudeandtostrengthenthe validityofourresults.Theeffectsizereportedinthisstudy wascalculatedasthe‘standardized’meandifference,i.e. astheratioofmeanchangetothestandarddeviationofthe change.8 Effect sizevaluesbetween0.2---0.5, 0.5---0.8and >0.8weretakentodenote‘small’, ‘moderate’and‘large’ changesinoutcomesrespectively.8
Anindependentmedicalstatistician carriedoutall sta-tisticalanalyses.
Results
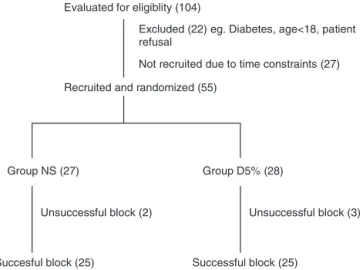
Evaluated for eligiblity (104)
Recruited and randomized (55)
Succesful block (25) Successful block (25) Group D5% (28) Group NS (27)
Excluded (22) eg. Diabetes, age<18, patient refusal
Not recruited due to time constraints (27)
Unsuccessful block (3) Unsuccessful block (2)
Figure1 Consort diagram.NS-normalsaline,D5%---dextrose 5%.
Table1 Patientdemographics.Valuesforage,sex,weight, heightandASAclass.
GroupNS(n=25) GroupD5%(n=25)
Age,years 32(16) 34(13)
Sex,M:F 19:6 22:3
Weight,kg 65(14) 68(15)
Height,cm 159(30) 167(6)
ASAclass,I/II/III 23/2/0 22/3/0
Continuousdataarepresentedasmean(SD).
theblock,alsohadtopreparethelocalanestheticsolution.
Therewashoweveralargernumberofmalesineachgroup.
Mean timefor onsetofanalgesia forthe NSgroup was
45.2±13.9min while mean time for the D5% group was
37.6±12.9min. The p-value of the test was 0.05, which
is significant at the 5% level. The effect size was 0.567,
whichdepicts amoderate change in outcome. Mean time
foronsetofanalgesiafor individualnervesshowedno dif-ferencebetweentheNSandD5%groups(Table2).
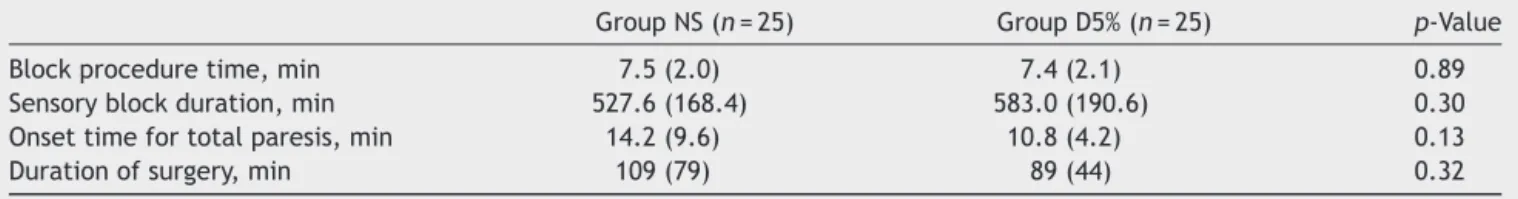
Themeantimeforonsetofmotorblock(totalparalysis) couldnotbeanalyzed,as90%ofpatientsdidnothave com-pleteparalysisattheendpointoftotallossofsensationto pinprick.Themeantimeforonsetoftotalparesiswasnot statisticallysignificantbetweentheNSandD5%groups.
Block procedure timeand sensoryblock durationwere alsonotdifferentbetweenthetwogroups(Table3).
Overallblocksuccesswas89%fortheD5%groupand92% fortheNSgroup,whichwerenotdifferent.
Nopatientneededrescueanalgesiaintra-operatively. Postinjectionoflocalanesthetics,2patients,onefrom eachgroup,developedHorner’ssyndrome,whichtheywere unaware of, and this resolved spontaneously after 24h observation.
Onepatient from the D5% group complainedof weak-ness and shooting pains in the operative arm on POD 7. Howeveruponfurtherquestioningandexamination,itwas discovered that the patient already had those symptoms bilaterally,priortotheoperationandthatthosesymptoms wereactuallyworseonthecontralateralarm.Howeveras the symptoms had marginally worsened, the patient was referredfor anMRI ofthecervicalspine. Thepatientwas thenreferredforanerveconductionstudyoftheoperative arm, whichconfirmed pathologyatthe levelofthe spinal cord.
Discussion
In this study, the mean time for onset of analgesia was 45.2min and37.6min for the normal saline and dextrose groups, respectively. The p-value of 0.05, together with a moderateeffectsize of0.567,8 makesusconclude that thereisclinicalevidencethatdilutionwithdextroseresults inafasteronsettimeofanalgesiacomparedtodilutionwith normalsaline.Inthisstudy,effectsizevalueswere calcu-latedinadditiontop-values,toassessthemagnitudeand tostrengthen the validityof ourresults.8 Thus,we could alsoreasonablyinferthatthis translatestoa fasteronset timeforanesthesia.Thisfindingissimilartoanotherstudy by Dhiretal.6 Ourslightly longermeantime foronset of analgesiaascomparedtosomestudiescouldbeattributed totheconsistentdepositionoflocalanestheticaroundthe brachialplexussheath(periplexus).6,9---11Thisapproachmay avoid needle-to-nerve contactand thus reduce the possi-bilityofnerveinjury.However,onestudyfoundthatupto 40minwasneededforcompleteanalgesiaandupto50min fortotallossofsensation.11
Meantimeforonsetofmotorblockcouldnotbe calcu-lated,asalargenumberofpatientsdidnothavecomplete motor paralysis at the point of total loss of sensation to pinprick. This was unusual, as the concentration of 0.5% ropivacaineusedshouldhaveproducedtotalmotorblockade aswell asanesthesia.However,ropivacaineis alsoknown tohavelessmotorblockadethan sensoryblockade.12 This mighthaveaccountedforthisunusualfinding.Itcouldalso
Table2 Onsettimesforanalgesiaandindividualnerves.
GroupNS(n=25) GroupD5%(n=25) p-Value
Onsetofanalgesia,min 45.2(13.9) 37.6(12.9) 0.05
Individualnerves
Radial,min 17.7(8.9) 17.0(10.0) 0.82
Median,min 37.4(16.6) 31.0(14.6) 0.15
Ulnar,min 40.8(17.9) 33.9(15.9) 0.16
Musculocutaneous,min 13.2(7.7) 16.2(8.6) 0.20
Table3 Onsettimesforotherendpoints.
GroupNS(n=25) GroupD5%(n=25) p-Value
Blockproceduretime,min 7.5(2.0) 7.4(2.1) 0.89
Sensoryblockduration,min 527.6(168.4) 583.0(190.6) 0.30
Onsettimefortotalparesis,min 14.2(9.6) 10.8(4.2) 0.13
Durationofsurgery,min 109(79) 89(44) 0.32
Valuesaremean(SD).
beduetodepositionoflocalanestheticoutsidethebrachial plexussheath(periplexus).
Mean block procedure time of about 7.5min for each
groupwasnotexpectedtobedifferentasasingle
opera-torperformedallblocks.Thistimewasalsocomparableto arecentstudythatreportedtimesof7.3---7.6min.6
Sensory block durationaveraged more than 520min or 8.5h for both groups. However,the methodof evaluating thisdurationofeffectwasbysubjectivepatientfeedback ofthetimetheyfirstfeltpain.Offsetofsensoryandmotor blockade wasnot assessed individually until full recovery whenthe patienthadreturnedtothe ward.Patientsalso received oral analgesia prior toblock resolution toavoid reboundpainafterreturnofsensation.
Despitetheslightlylongermeantimeforonsetof anal-gesia in this study,block success of 89% and 92% for the two groups were similar to the success rates for ultra-soundguidedsupraclavicularbrachialplexusblocksquoted inotherstudies,whichrangedfrom85to95%.9---11
Horner’s syndromeoccurred in2(3.6%) ofthepatients in this study. This is slightly higher than 1% cited in one study,but wasmuchlower than 37.5%cited inanother.13 Hence, there is evidence of wide variations in incidence and some studies donot actually report the incidenceof Horner’ssyndrome.Ratherthanacomplicationperse,ithas beendescribedasanunpleasantsideeffectwithnoclinical sequelae.Indeed,thetwopatientswithHorner’ssyndrome inourstudydidnotknowtheydevelopedituntiltold.
Thedominanceofmalesineachgroupcanbeattributed to the fact that many of these patients were coming for plating of the radius or ulnar due to motor vehicle accidents, which have been shown to have a higher inci-dence in males.14 There are notable limitations in this study.Theanesthesiologistevaluatingtheblockwasblinded till halfwaythroughthe study.Duetounforeseen circum-stances,thepreparationofthelocalanesthetichadtobe carriedoutbyhiminthelatterhalf.Thisinherently intro-ducesoperatorbiastothestudy.However,blockevaluation usedaveryclearandobjectiveendpointoflossofsensation topinprick,whichwouldhavedecreasedthesubjectivityof theevaluationbytheassessor.
Summary
Afasteronsettimeofanalgesiatoprovideconditions suit-ableforsurgeryiswhatisdesiredinthedailyrunningofthe operatingtheater listandin optimizing efficientusageof theatertime.Ourstudysuggestsadecreaseinonsettime ofanalgesiawhendextrosewasusedasadiluentinsteadof normalsalineforultrasoundguidedsupraclavicularbrachial
plexusblock.Furtherstudiesarerequiredtoascertainifthe resultsaresimilarfordifferentconcentrationsofotherlocal anesthetics,andforotherultrasoundguidednerveblocks.
Conflicts
of
interest
Theauthorsdeclarenoconflictsofinterest.
References
1.Heavner JE. Local anesthetics. Curr Opin Anesthesiol. 2007;20:336---42.
2.KanaiA,HokaS.Acomparisonofepiduralblockadeproduced byplain1%lidocaineand1%lidocainepreparedbydilutionof 2% lidocaine withthesamevolume ofsaline. AnesthAnalg. 2006;102:1851---5.
3.TsuiBCH,KropelinB.Theelectrophysiologicaleffectsof dex-trose5%inwateronsingleshotperipheralnervestimulation. AnesthAnalg.2005;100:1837---9.
4.HashimotoK,SakuraS,BollenAW,etal.Comparativetoxicity ofglucoseandlidocaineadministeredintrathecallyintherat. RegAnesthPainMed.1998;23:444---50.
5.Tsui BCH, Kropelin B, Ganapathy S, et al. Dextrose 5% in water:fluidmediumformaintainingelectricalstimulationof peripheralnervesduringstimulatingcatheterplacement.Acta AnaesthesiolScand.2005;49:1562---5.
6.DhirS,TureanuL,BouzariA,etal.Reductioninsodiumcontent of local anesthetics for peripheral nerve blocks: a compar-ative evaluation of saline with 5% dextrose. Anesth Analg. 2012;114:1359---64.
7.DurlakJA.Howtoselect,calculate,andinterpreteffectsizes. JPediatrPsychol.2009;34:917---28.
8.Chinna K, Krishnan K. Biostatistics for the health sciences. McGrawHill;2009.
9.PerlasA,LoboG,LoN,etal.Ultrasound-guidedsupraclavicular block:outcomeof510consecutivecases.RegAnesthPainMed. 2009;34:171---6.
10.WilliamsSR,ChouinardP,ArcandG,etal.Ultrasoundguidance speedsexecutionand improvesthequalityofsupraclavicular block.AnesthAnalg.2003;97:1518---23.
11.KapralS,KrafftP,EibenbergerK,etal.Ultrasound-guided sup-raclavicularapproach for regional anesthesia ofthebrachial plexus.AnesthAnalg.1994;78:507---13.
12.Markham A, Faulds D, Ropivacaine. A review of its phar-macology and therapeutic use inregional anesthesia.Drugs. 1996;52:429---49.
13.TrandeQH,RussoG,Mu˜nozL,etal.Aprospective,randomized comparisonbetweenultrasound-guidedsupraclavicular, infra-clavicular,andaxillarybrachialplexusblocks.RegAnesthPain Med.2009;34:366---71.