www.rpped.com.br
REVISTA
PAULISTA
DE
PEDIATRIA
ORIGINAL
ARTICLE
Clinical
evolution
and
nutritional
status
in
asthmatic
children
and
adolescents
enrolled
in
Primary
Health
Care
Rosinha
Yoko
Matsubayaci
Morishita
∗,
Maria
Wany
Louzada
Strufaldi,
Rosana
Fiorini
Puccini
DepartmentofPediatrics,EscolaPaulistadeMedicina,UniversidadeFederaldeSãoPaulo(Unifesp),SãoPaulo,SP,Brazil
Received22September2014;accepted8February2015 Availableonline1September2015
KEYWORDS
Asthma; Children;
Clinicalevolution; PrimaryHealthCare
Abstract
Objective: Toevaluatetheclinicalevolution andtheassociationbetweennutritionalstatus andseverityofasthmainchildrenandadolescentsenrolledinPrimaryHealthCare.
Methods: Aretrospectivecohortstudyof219asthmaticpatients(3---17yearsold)enrolledin PrimaryCareServices(PCSs)inEmbudasArtes(SP),from2007to2011.Secondarydata:gender, age,diagnosisofasthmaseverity,otheratopicdiseases,familyhistoryofatopy,andbodymass index.Toevaluatetheclinicaloutcomeofasthma,datawerecollectedonnumberofasthma exacerbations,numberofemergencyroomconsultationsanddosesofinhaledcorticosteroids atfollow-upvisitsinthe6thand12thmonths.Thestatisticalanalysisincludedchi-squareand Kappaagreementindex,with5%setasthesignificancelevel.
Results: 50.5%ofpatientsstartedwheezingbeforetheageof2years,99.5%hadallergicrhinitis and65.2%hadapositivefamilyhistoryofatopy.Regardingseverity,intermittentasthmawas more frequent (51.6%)and, in relationto nutritional status,65.8% ofpatients had normal weight.Therewas noassociationbetweennutritional statusandasthmaseverity(p=0.409). After1yearoffollow-up,25.2%ofpatientsshowedreductioninexacerbationsandemergency roomconsultations,and16.2%reducedtheamountofinhaledcorticosteroids.
Conclusions: ThemonitoringofasthmaticpatientsinPrimaryCareServicesshowed improve-ment in clinical outcome, with a decreased number of exacerbations, emergency room consultationsanddosesofinhaledcorticosteroids.Noassociationbetweennutritionalstatus andasthmaseveritywasobservedinthisstudy.
©2015SociedadedePediatriadeS˜aoPaulo.PublishedbyElsevierEditoraLtda.Thisisanopen accessarticleundertheCCBY-license(https://creativecommons.org/licenses/by/4.0/).
DOIoforiginalarticle:http://dx.doi.org/10.1016/j.rpped.2015.02.005
∗Correspondingauthor.
E-mail:rosinhamorishita@uol.com.br(R.Y.M.Morishita).
2359-3482/©2015SociedadedePediatriadeS˜aoPaulo.PublishedbyElsevierEditoraLtda.ThisisanopenaccessarticleundertheCC
PALAVRAS-CHAVE
Asma; Crianc¸as; Evoluc¸ãoclínica; Atenc¸ãobásicaà saúde
Evoluc¸ãoclínicaeestadonutricionaldecrianc¸aseadolescentesasmáticos acompanhadosemUnidadeBásicadeSaúde
Resumo
Objetivo: Avaliaraevoluc¸ãoclínicaeaassociac¸ãoentreoestadonutricionaleagravidadeda asmaemcrianc¸aseadolescentesmatriculadosemUnidadesBásicasdeSaúde(UBS).
Métodos: Estudodecoorteretrospectivacom219pacientesasmáticos(3---17anosdeidade), matriculadosemUBSdomunicípiodeEmbudasArtes(SP),de2007a2011.Dadossecundários: sexo,idade, diagnóstico de gravidade da asma, outrasatopias, antecedentes familiares de atopia,índice demassa corporal. Paraavaliar aevoluc¸ão da asmaforam coletadosnúmero decrisesdeasma,númerodeatendimentosdeurgênciaedosesdecorticoideinalatóriono6◦
e12◦mêsdeacompanhamento.Aanáliseestatísticaincluiutestesdequi-quadradoeíndicede concor-dânciaKappa,comníveldesignificânciade5%.
Resultados: Dospacientes,50,5% iniciaramasibilânciaantesdosdoisanosdeidade;99,5% apresentaramrinitealérgicaeem65,2%antecedentefamiliarparaatopiapositivo.Quantoà gravidade,aasmaintermitentefoimaisfrequente(51,6%),emrelac¸ãoaoestadonutricional, 65,8% dos pacienteseram eutróficos. Não houveassociac¸ãoentre o estadonutricional ea gravidadedaasma(p=0,409).Apósumanodeacompanhamento;25,2%dospacientesreduziram asexacerbac¸õeseosatendimentosnasurgênciase16,2%reduziramaquantidadedecorticóide inalatório.
Conclusões: O acompanhamento dos pacientes asmáticos em UBS demonstrou melhora da evoluc¸ãocomreduc¸ãodonúmerodeexacerbac¸ões,dosatendimentosnasurgênciasedasdoses decorticoideinalatório.Nãohouveassociac¸ãoentreoestadonutricionalegravidadedaasma. ©2015SociedadedePediatriadeS˜aoPaulo.PublicadoporElsevierEditoraLtda.Esteéumartigo OpenAccesssobalicençaCCBY(https://creativecommons.org/licenses/by/4.0/deed.pt).
Introduction
Asthma is a complexinflammatory disease,recognized as one of the most common chronic diseases of childhood. Itis characterizedby recurrentrespiratory symptomsand it significantly impairs the quality of life. In Brazil, epi-demiologicalstudiescarriedoutinrecentdecadesindicate a trend of increasing prevalence of asthma in children and adolescents.1---5 In this same period, an increase in
theprevalence of overweight and obesity inchildren and
adolescents has also been observed in several countries
and in Brazil, which constitutes a major public health
problem.6 Thisanalysisissupportedbythreenational
sur-veys that assessed nutritional status from 1974 to 2009,
showingan increasein overweightandobesity inchildren
and adolescents in all income groups and in all regions
ofBrazil.7 Obesityisacomplexandmultifactorialdisease
andit actively contributes tothe developmentof
cardio-vasculardiseases, arterial hypertension,diabetes mellitus
and metabolic syndrome, in addition to exacerbating
asthma.8---12
Epidemiological studies have suggested an association
between obesity and asthma, more consistent in adults,
revealing that obese asthmatic individuals have a higher
frequencyofexacerbationcrises,emergencyroom
consul-tationsandneedforhigherdosesofinhaledcorticosteroids,
aswellasgreaterdifficultyincontrollingthedisease.11,13,14
Theassociationbetweenobesityandasthmainchildrenand
adolescentsisstillcontroversial,andstudiesfrequentlyuse
differentmethodologies,whichexplains,inpart,thevarying
resultsobtained.11,15---21
In 1988, aspart of the activities of the Teaching-Care
IntegrationProgramdevelopedbyUniversidadeFederalde
SãoPaulointhetownofEmbudasArtes,inthe
metropoli-tan region of São Paulo, the Care Program for Children
with‘‘Wheezing’’wasimplementedinpartnershipwiththe
Departmentof Health.Thestructure ofthisprogram
con-sidered as its principle the role of primary care in the
management and monitoring of the most prevalent
mor-bidities.The program’spopulationconsistsofchildrenand
adolescentswithrecurrentwheezing,treatedbyateamof
pediatricians,undergraduatemedicalstudentsandmedical
residentsinPediatrics.Theactivitiesdevelopedbythe
pro-gramincludemedicalconsultations,educationalgroupsfor
family members and provision of medications for asthma
control.
Venturaetal.22evaluatedthisprograminthe1988---1993
period and observed that before its implantation, most
patientssoughttreatmentforthediseaseonlyinperiodsof
exacerbationsandatemergencyservices.Theauthors
veri-fiedthatafter1yearoffollow-up,childrenwhomaintained
higheradherencetotheprogramhadbenefited,despitethe
limitedsupplyofasthmamedicationsavailableinthe
pub-lic health system in that period, which was restricted to
the distribution of bronchodilators, theophylline and
sys-temiccorticosteroidsonly.Thissituationhaschangedsince
2009, with Portaria N◦ 2981 of the Ministry of Health,
whichprovidesfortheregularprovisionofmedicationsfor
asthmacontrolduringcrisesandforcontinuoususebythe
municipality.23
ConsideringthenutritionaltransitioninBrazil,withthe
in the prevalence of obesity,7 a phenomenon which was
alsoobservedinthemunicipality ofEmbudasArtes,24 and
consideringapossibleassociationbetweenobesityand
wors-eningofasthma,withmoreexacerbationcrisesandvisitsto
theemergencyroominpediatricpatients,15---21 thepresent
studyaimedtoevaluatetheclinicalevolutionandthe
asso-ciation between nutritional statusand disease severityin
childrenandadolescentswithasthma enrolledatand
fol-lowedinaPrimaryCareService(PCS)oftheBrazilianPublic
HealthSystem(SUS).
Method
Thisretrospectivecohortinvolvedchildrenaged3---17years, enrolledintheCareProgramforChildrenwith‘‘Wheezing’’ from1January2007to31December2011,intwoPCSsinthe municipality of Embu das Artes. Secondary data obtained from the first consultation were collected from patients’ records:age,gender,ageatfirstwheezingcrisisandother atopicdiseases (rhinitis,dermatitis), previous hospitaliza-tions forrespiratory diseases, birthweight,family history ofatopy(asthma,rhinitisanddermatitis),anddiagnosisof asthmaseverityusingtheclinical criteriaof theIV Brazil-ianGuidelinesforAsthmaManagement,2006(intermittent asthma, mild persistent, moderate persistent and severe persistent asthma).25 Regarding the clinical course of the
disease,thenumberofemergencyroomconsultationsand
asthmaattackswerecollected,inadditiontoinhaled
cor-ticosteroid doses according to the 2012 GINA Consensus
equipotential2inthe6thand12thmonthsoffollow-up.The
levelsof asthmacontrolwereclassifiedinthe12thmonth
offollow-upaccordingtothe2012GINAConsensus.2
Anthropometric data,such asweight(kg), height (cm)
andthecalculationofbodymassindex(BMI)(kg/m2)z-score
basedontheWHOcurvesof2006and2007,usingtheAnthro
andAnthroPlusprograms,26,27wereobtainedfromthe
medi-calrecordsofthe1stconsultation.Thecutoffpointsused
wereaccordingtoz-score:≥−3to<−2:thinness;≥−2to
<+1: normal weight; ≥+1 to <+2: risk of overweight (<5
years)andoverweight(≥5years);≥+2to<+3:overweight
(<5years)andobesity(≥5years);≥+3:obesity (<5years)
andsevereobesity(≥5years).26,27
Patients were considered as cases of loss of follow-up
afterfailingtocometoconsultationformorethan6months
sincethelastvisit anddischargewasdefinedfor casesof
asthma controlled without the use of inhaled
corticoste-roids.
Regarding the study procedure, a total of 439
chil-drenwereidentifiedwithafirstscheduledconsultationin
theperiod;after 92patients wereexcluded astheywere
youngerthan3yearsand/orhadotherpulmonarydiseases
andsyndromes,347patientswhomettheinclusioncriteria
remained.Ofthese,therewasalossof95individualswho
missedthefirstconsultation,32recordswerenotfound,and
therewasonedeath,thustotalling219patientsselectedfor
thestudyandwhoattendedthe1stconsultation.
After1yearoffollow-up,39patients(17.8%)abandoned
treatment. Four patients (1.8%)with intermittentasthma
weredischargedfromtheprogramduringthisperiod;one
patient with intermittent asthma moved to another city.
During this period, 88 patients (40%) missed at least one
consultation andthus, 131 patients came toall proposed
consultations,havingthecomplete datatobeusedinthe
analysisoftheclinicalcourseofthedisease.
Forthestatisticalanalyses,chi-squaretestswereusedto
comparecategoricalvariables,withthelevelofsignificance
beingsetat5%andtwo-tailedstatisticaltests.TheKappa
indexwasusedtoassessthenumberof crises,emergency
roomconsultationsanddosesofmedicationsusedbetween
thefirstandsecondsemesteroftheprogramfollow-up,with
lack of agreement being considered when the value was
zero(=0)andperfectagreementwithKappaindex=1.The
standarderroroftheKappaindexof5%allowedthe
estima-tionofthe statistical significanceand the95% confidence
interval.
ThisstudywasapprovedbytheInstitutionalReviewBoard
oftheDepartmentofHealthofEmbudasArtesandwasalso
approvedbytheInstitutional Review Boardof UNIFESP,n.
1821/11.
Results
The 219 patients who attended the 1st consultation had a mean age of 6.65 years ±4.89 SD (3---17 years), with most being male (58.4%); 9.3% had low birth weight and 50.5%ofpatients startedwheezing before2 yearsofage; 91.7%hadotheratopicconditions,almostallofthemwith allergicrhinitis (99.5%),and 46% reportedprevious hospi-talizationatthestartoffollow-up.Familyhistoryofatopy waspositive in65.2% of patients. As for disease severity, intermittentasthma was themost frequent type(51.6%), andinrelationtonutritionalstatus,normalweight predom-inated (65.8%) amongpatients. The calculatedBMI had a mean±SDof17.22±3.34(11.98---36.22kg/m2),andz-score
of0.48±5.20(−2.72to5.20).
Patient distribution according to the nutritional sta-tus and the severity of asthma in the 1st consultation is describedinTable1.Itshouldbenotedthatsevereasthma
wasdiagnosed only in patients withoverweight and
obe-sity.After statistical analysis, it wasobserved that there
wasnosignificantassociationbetweennutritionalstatusand
asthmaseverity(p=0.409).
In relation to asthma attacks, approximately 20% of
patientshadnoexacerbationsinthe1stand2ndsemesters.
Therewasnoagreementbetweenthetwomomentsdueto
theknownheterogeneousdiseaseprogression(=0.060and
p=0.375);however,25.2%ofthepatientsimproved
exacer-bations,and 19.1% started having more crises in the 2nd
semester (Table 2). It is noteworthy that these patients
started theprogram follow-up in differentmonths of the
year, thus minimizing the influence of seasonality on the
frequencyofexacerbations.
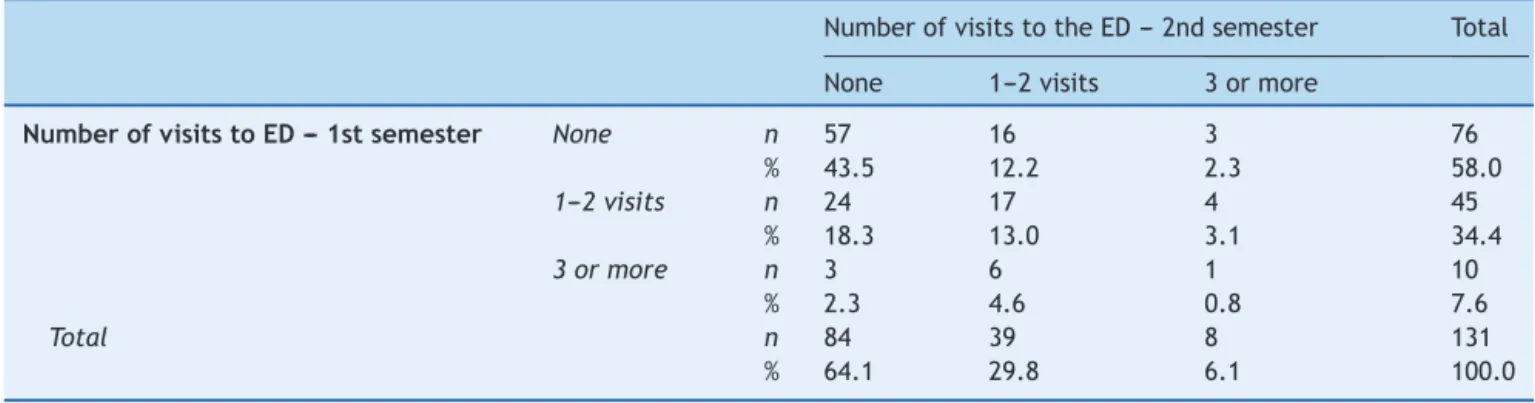
Table3showsthenumberofemergencyroom
consulta-tions due toasthma attacksper patient between the 1st
and2ndsemesters.TheKappaindexshowedanagreement
between the two periods (p=0.013), but with a value of
=0.180, i.e., a poor agreement. When analyzing all the
answers,57.3%ofpatientshadthesamenumberof
emer-gencyroomconsultationsinboth moments;25.2%showed
improvementand 17.6% showed worsening of the clinical
picture,withmoreemergencyroomconsultations,withthis
Table1 Nutritionalstatusandasthmaseverityinthe1stconsultationattheCareProgramfor Childrenwith‘‘Wheezing’’, EmbudasArtes.
Nutritionalstatus Asthmaseverity
Exercise Intermittent Mild Moderate Severe
n=3(%) n=113(%) n=54(%) n=46(%) n=3 %
Thinness 0(0.0) 1(20.0) 2(40.0) 2(40.0) 0 0.0
Normalweight 2(1.4) 81(56.3) 34(23.6) 27(18.8) 0 0.0
Overweightrisk 0(0.0) 8(40.0) 6(30.0) 6(30.0) 0 0.0
Overweight 1(2.9) 16(47.1) 8(23.5) 7(20.6) 2 5.9
Obesity 0(0.0) 7(43.8) 4(25.0) 4(25.0) 1 6.2
p-value=0.409.
Table2 Numberofasthmacrisesinthe1stand2ndsemestersoffollow-upofpatientsenrolledintheCareProgramforChildren with‘‘Wheezing’’,EmbudasArtes.
Numberofcrises---2ndsemester Total
None 1---5 ≥6crises
Numberofcrises---1stsemester None n 9 16 1 26
% 6.9 12.2 0.8 19.8
1---5 n 17 63 8 88
% 13.0 48.1 6.1 67.2
≥6crises n 2 14 1 17
% 1.5 10.7 0.8 13.0
Total n 28 93 10 131
% 21.4 71.0 7.6 100.0
=0.060;p-value=0.375.
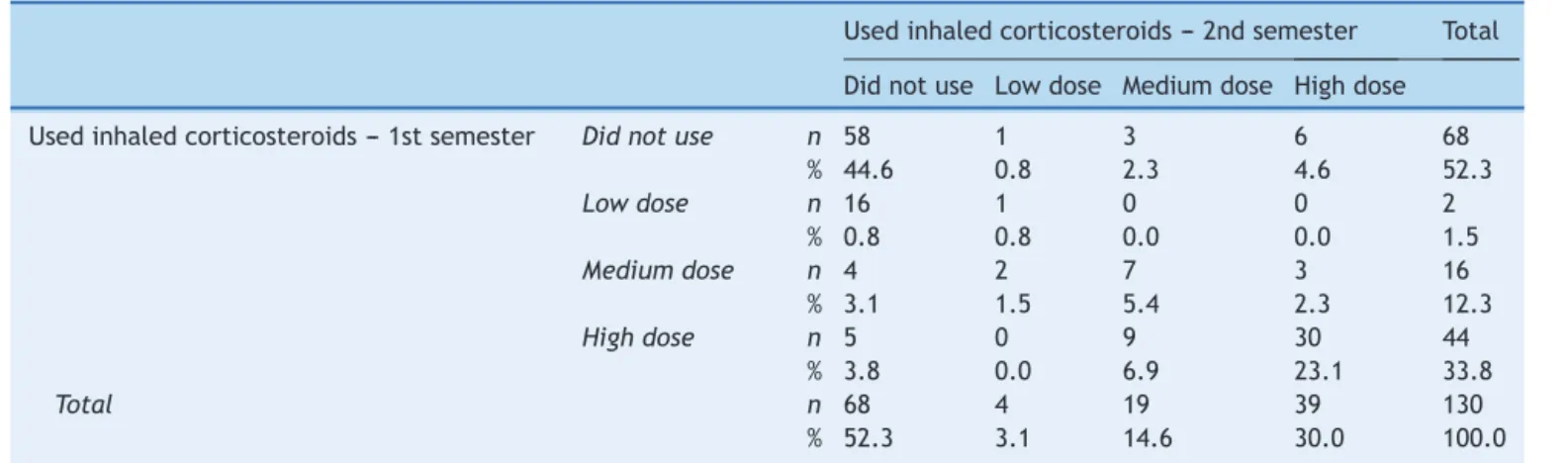
Table 4 describes the doses of inhaled corticosteroids
used by asthma patients in the 1st and 2nd semesters.
The observed results showed that there was an
agree-ment between the twomoments in time (p=0.001), with
avalueof=0.569,indicatingmoderateagreement.Itcan
beobservedthat73.8%ofpatientsremainedwiththesame
doseofcorticosteroids inthe1stand2ndsemesters,
indi-cating a high correlation between the results in the two
moments;10.0% ofpatients showed worseningandit was
necessary tostartusinginhaled corticosteroidsin the2nd
semester, with 2.3% using medium and 4.6%, high doses.
Ofthe 16.2%of patientswhoimproved,8.4% reducedthe
amount and 7.7% stopped using medication in the 2nd
semester of follow-up. A patient using the association of
inhaled corticosteroids/long-acting bronchodilator in the
2nd semester was excluded from this table to allow
sta-tistical analysis. Additionally, it was observed that 11.3%
of patients in the 1st semester showed irregular use of
Table3 Numberofpatients’visitstotheemergencydepartment(ED)inthe1stand2ndsemestersoffollow-upattheCare ProgramforChildrenwith‘‘Wheezing’’,EmbudasArtes.
NumberofvisitstotheED---2ndsemester Total
None 1---2visits 3ormore
NumberofvisitstoED---1stsemester None n 57 16 3 76
% 43.5 12.2 2.3 58.0
1---2visits n 24 17 4 45
% 18.3 13.0 3.1 34.4
3ormore n 3 6 1 10
% 2.3 4.6 0.8 7.6
Total n 84 39 8 131
% 64.1 29.8 6.1 100.0
Table4 Inhaledcorticosteroiddosesusedbypatientsinthe1stand2ndsemesterfollowedattheCareProgramforChildren with‘‘Wheezing’’,EmbudasArtes.
Usedinhaledcorticosteroids---2ndsemester Total
Didnotuse Lowdose Mediumdose Highdose
Usedinhaledcorticosteroids---1stsemester Didnotuse n 58 1 3 6 68
% 44.6 0.8 2.3 4.6 52.3
Lowdose n 16 1 0 0 2
% 0.8 0.8 0.0 0.0 1.5
Mediumdose n 4 2 7 3 16
% 3.1 1.5 5.4 2.3 12.3
Highdose n 5 0 9 30 44
% 3.8 0.0 6.9 23.1 33.8
Total n 68 4 19 39 130
% 52.3 3.1 14.6 30.0 100.0
=0.569;p-value<0.001.
inhaled corticosteroids, and 8% in the 2nd semester of follow-up.
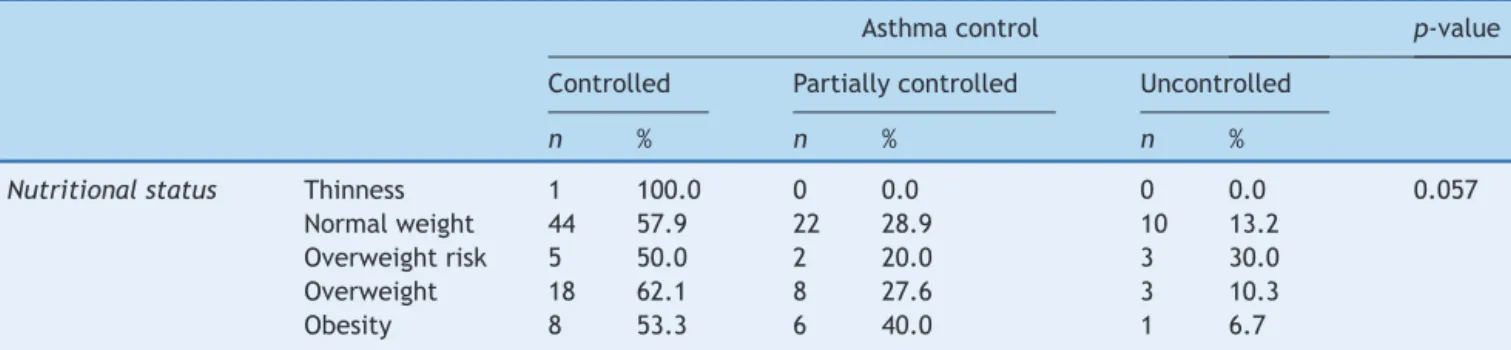
Table 5 shows the levels of asthma control and
nutri-tional status at 12 months of follow-up of 131 patients.
Obese patients showed more controlled asthma (53.3%),
followed by partially controlled (40.0%) and uncontrolled
(6.7%).Accordingtotheanalysis,itwasobservedthatthere
wasnosignificantassociationbetweennutritionalstatusand
asthmacontrollevels(p=0.057).
Discussion
Given the increasing prevalence of asthma2---5 and of
obesity6,7 in childhood, this study sought to establish an
association between the two, the impacton disease
evo-lution andthe effects of therapeutic intervention after a
1-year follow-upof patients enrolledinthe CareProgram
forChildrenwith‘‘Wheezing’’.
When analyzing the nutritional status of asthmatic
patientsinthisstudy,itisobservedthattheresultscontrast
withthe findingsof Venturaet al.28 in the sameprogram
ofthemunicipality,althoughthenutritionalstatus
classifi-cationcriteriaaredifferentinthetwoassessedmoments,
including regarding the use of the term ‘‘malnutrition’’
and not thinness, as currently recommended by the
WHO26,27; the authors did not report any patients with
excess weight, and 38% were malnourished according to
that assessment, which reinforces the observation of the
nutritionaltransition amongthe patients in this program,
as reported in the national Household Budget Survey of
2008---2009.7
In thisstudy,when assessingthe nutritionalstatus and
asthmaseverityin1stconsultation,thesevereformofthe
diseasewasobservedonlyin patientswithexcessweight,
while Ventura et al. observed the highest prevalence of
malnutrition inthe moderate/severe asthma group in the
1988---1993periodinthesamemunicipality,despitethe
dif-ferences in nutritional classification criteria used at the
time.28
Regardingtheclinicaldiagnosisofdiseaseseverityinthe
1stconsultation,thehighestfrequencywasofintermittent
asthma(51.5%),while severeasthmawasobservedinonly
1.4%,asimilarratetothatreportedintheIVBrazilian
Guide-linesfor Asthma Management, 2006.25 Simões et al.,29 in
the municipality of Salvador, state of Bahia, described a
higherprevalenceofmild(40%)andsevere(10.8%)asthma
andlowerprevalence ofintermittent(36%) andmoderate
(12.8%)asthma.
Inthepresent study,we assessedtheinfluenceof high
BMIandasthmaseverity,aswellasdiseasecontrolaftera
yearoffollow-upofpatientsenrolledintheprogram.The
analysesshowednoassociationsbetweennutritionalstatus
andasthma severity,aswell asbetweennutritionalstatus
anddiseasecontrol.
Studiesontheassociationbetween asthmaandobesity
show heterogeneous results due to the use of
differ-entmethods for asthma severityclassification,withsome
reporting symptoms of wheezing, while others use
medi-caldiagnosisorobjectivemeasurementssuchasspirometry,
thereforeshowingvariedresults.FarahandSalome,11 ina
reviewarticle, pointedout thecontroversies onthe
asso-ciationbetweenobesityandworseasthmaseverity.Cassol
et al.16 carried out a population-based study with
ado-lescents in a city in southern Brazil and did not find an
association between increased BMI and asthma symptom
worsening.IntheUSA,Rossetal.17didnotfindany
differ-encesinpulmonaryfunctionbetweenobeseandnonobese
childrenandadolescentswithasthma.On theotherhand,
otherstudieshaveshownan associationbetweenhighBMI
andhigherasthmaseverity.18,19
Regardingasthmacontrol,theassociationbetween
obe-sityandworsedisease controlisnotwell establishedyet.
Quintoetal.21 observedthatchildrenandadolescentswith
overweight and obesity had worse asthma control, with
moreexacerbationsandmorefrequentuseofrescue
med-ications.Kattan etal.20 described anassociation between
worseasthmacontrolandobesityinthefemalegenderina
studyofadolescentswithasthma. Otherauthorsfound no
differencesinlevelsofasthmacontrolbetweenobeseand
nonobesepatients.17,30
The present study assessed the evolution of asthma
considering patients who attended all proposed
Table5 Nutritionalstatusanddiseasecontrollevelsinthe2ndsemesteroffollow-up.
Asthmacontrol p-value
Controlled Partiallycontrolled Uncontrolled
n % n % n %
Nutritionalstatus Thinness 1 100.0 0 0.0 0 0.0 0.057
Normalweight 44 57.9 22 28.9 10 13.2
Overweightrisk 5 50.0 2 20.0 3 30.0
Overweight 18 62.1 8 27.6 3 10.3
Obesity 8 53.3 6 40.0 1 6.7
maybedifferentfromthosewholefttheprogramandthe oneswhomissedtheconsultations,whichmayhavelimited theanalysesofdiseaseevolution.Thequantificationofthe numberofcrisesmayhavebeen influencedbyrecallbias, especiallywhenexacerbationsoccurredseveraltimesduring onesemester;theemergencyroomconsultationsare impor-tanteventsinapatient’slife,makingrecordsmorereliable. Ontheotherhand,patientsstartedtheProgramfollow-up indifferent monthsof theyear, thus reducingthe biasof asthmaexacerbationsduetoseasonality.
During1yearoffollow-up,25.2%ofpatientsreducedthe numberofcrisesandemergencyroomconsultations.Ofthe patientswhoshowedworsening,only19.1%hadmorecrises, and17.6%requiredmoreemergencyroomconsultationsin thatperiod.Itwasobservedthattheproportionof asthmat-icswhoshowedimprovementwashigherthantheoneswho showedworsening,demonstratingthebenefitsofmonitoring inthosepatientswhojoinedtheprogram.
Ventura et al.22 verified that patients with moderate
andsevere asthma had a smaller number of crises,when
analyzingtheperiodbeforeandafter1yearoffollow-up,
in thesame PCSs, from 1988 to1993. These authors also
observedthattimeoffollow-upinfluencedtheevolutionof
moderateasthma,showingclinicalimprovementwithtime
longerthan1year.Moreover,thetimeoffollow-upshorter
or longer than 1 year showed no difference in the
evo-lutionof severe asthmatics.22 The observed results arein
agreementwiththeretrospectivecohortstudycarriedout
by Fontes et al.,31 who evaluated the follow-up of
asth-maticchildrenandadolescentsinaPulmonologyServicein
thecityofBeloHorizonte,StateofMinasGerais,observing
asignificantreductioninthefrequencyofhospitalizations
and emergency room visits for asthma during a 1-year
period.
Accordingtothisstudy,mostpatientsshowedtreatment
adherence. An important part of these results should be
attributedto the provision of asthma medications by the
Public Health System PCSs, including the municipality of
Embudas Artes, since2009,withthe PortariaN◦
2981 of
the Ministry of Health.23 Progresshas been made in
Pub-licHealthPolicieswithhealthmanagers’acknowledgment
thatasthmaisoneofthemostcommonchronicdiseases,by
makingavailableinhaledmedicationssuchascorticosteroids
withorwithoutacombinationwithlong-acting
bronchodila-tors,rescuemedicationssuchasshort-acting-agonistsand
oralcorticoidstopatientswithasthma.
Improved adherence to the program by patients and
familymemberswasdemonstratedbythedecreaseinthe
abandonmentrate,from53.2%22sinceitsimplementationin
bothPCSstocurrently17.8%.Thisfindingwasalsodescribed
byDalcinetal.inasthmaticpatientsrecruitedfroman
out-patientclinicofahospitalinthecityofPortoAlegre,stateof
RioGrandedoSul,alsoobservingthataccesstomedication
andadequateuseofinhaledcorticosteroidswereassociated
withasthmacontrol.30
However,despitetheconsistentimprovementinprogram
adherence andfollow-up,thisstudy hassome limitations,
suchasobtaining somesecondary data(medical records),
andthelossofinformationonpatientsthatmissed
appoint-ments or abandoned the program, while study data was
being collected. In spite of these limitations, we can
conclude that the study showed noassociations between
nutritionalstatusandasthma severityandcontrol.
Adher-encetotreatmentresultedinadecreasednumberofasthma
crises, emergency room consultations during the
follow-up period,in addition todecreasing the dosesof inhaled
corticosteroids.Thisstudyemphasizestheimportanceand
feasibilityofasthmaticpatientsfollow-upinPCSs.Moreover,
the implementationof public policiesthat facilitated the
introductionofspecificmedicationsforasthmatreatment,
themostcommonchronicdiseaseinchildhood,inPrimary
Health Carecontributedtothe favorableoutcome of this
evolution.
Funding
Fundac¸ão de Amparo à Pesquisa do Estado de São Paulo (FAPESP),SãoPauloCity,StateofSãoPaulo,Brazil.Process N◦2011/51.634-3.
Conflicts
of
interest
Theauthorsdeclarenoconflictsofinterest.
Acknowledgements
TheauthorswouldliketothanktheDepartmentofHealthof EmbudasArtesandtheDivisionofGeneralandCommunity PediatricsoftheDepartmentofPediatricsofEPM/UNIFESP.
References
con-trolledasthmaanduncontrolledasthmaticpatients.BrazJMed BiolRes.2007;40:943---8.
2.GINA. Global Initiative for Asthma. Global strategy asthma managementand preventionupdate 2012 [homepageon the Internet]. NIH publication [2012 December]; 2012 [accessed 20.03.14].Availablefrom:http://www.ginasthma.org
3.SBPT.SociedadeBrasileira dePneumologiaeTisiologia. Dire-trizesdaSociedadeBrasileiradePneumologiaeTisiologiapara oManejodeAsma---2012.JPneumol.2012;38(supl1):S51---546.
4.WehrmeisterFC,MenezesAMB,CascaesAM,Martínez-MesaJ, BarrosAJD.Tendênciatemporaldeasmaemcrianc¸ase adoles-centesnoBrasilnoperíodode1998a2008.RevSaúdePública. 2012;46:242---9.
5.SoléD,Camelo-NunesIC,WandalsenGF,MalloziMC.Aasmana crianc¸a eno adolescentebrasileiro:contribuic¸ãodo Interna-tionalStudyofAsthmaandAllergiesinChildhood(ISAAC).Rev PaulPediatr.2014;32:114---25.
6.WHO. World Health Organization [homepage on the
Inter-net]. Population-based Prevention Strategies for Childhood
Obesity-Report of a WHO Forum and Technical
Meet-ing. 2009 [accessed 20.03.14]. Available from: http://www.
who.int/mediacentre/factsheetes/fs311/en/
7.Brasil Ministério do Planejamento, Orc¸amento e Gestão.
Instituto Brasileiro de Geografia e Estatística --- IBGE
[homepage on the Internet]. Pesquisa de Orc¸amentos
Familiares 2008---2009. Antropometria e análise do estado
nutricional de crianc¸as, adolescentes e adultos no Brasil.
Rio de Janeiro; 2010 [accessed 20.03.14]. Available from:
http://www.ibge.gov.br/home/estatistica/populacao/ condicaodevida/pof/20082009encaa/default.shtm
8.NogueiraPCK, Costa RF, CunhaJSN, SilvestriniL, Fisberg M. PressãoarterialelevadaemescolaresdeSantos:relac¸ãocom obesidade.RevAssocMedBras.2007;53:426---32.
9.SBP.SociedadeBrasileiradePediatria.Departamentocientífico denutrologia.Obesidadenainfânciaeadolescência:Manualde orientac¸ão.SãoPaulo:SBP;2008.p.116.
10.Dowd JB, Zajacova A, Aiello AE. Predictors of inflammation inU.S. childrenaged 3---16 years. Am JPrev Med. 2010;39: 314---20.
11.FarahCS,SalomeCH.Asthmaandobesity.Aknownassociation butunknownmechanism.Respirology.2012;17:412---21.
12.GraversenL,SorensenTIA,PetersenL,etal.Preschoolweight andbodymassindexinrelationtocentralobesityandmetabolic syndromeinadulthood.PlosOne.2014;9:e89986.
13.BeutherDA,SutherlandER.Overweight,obesity,andincident asthma:ameta-analysisofprospectiveepidemiologicstudies. AmJRespirCritCareMed.2007;175:661---6.
14.RodrigoGJ,PlazaV.Bodymassindexandresponseto emer-gency department treatment in adults with severe asthma exacerbations: prospective cohort study. Chest. 2007;132: 1513---9.
15.FlatermanV,RutherfordGW.Ameta-analysisoftheeffectof highweightonasthma.ArchDisChild.2006;91:334---9.
16.CassolVE,RizzatoTM,TecheSP,etal.Prevalênciaegravidade daasmaentreadolescentesesuarelac¸ãocomÍndicedeMassa Corporal.JPediatr(RioJ).2005;81:305---9.
17.RossKR, Hart MA, Stofer-Isser A, et al. Obesity and obesity relatedco-morbiditiesinareferralpopulationofchildrenwith asthma.PediatrPulmonol.2009;44:877---84.
18.CamiloDF,RibeiroJD,ToroADC,BaracatECE,BarrosFilhoAA. Obesidadeeasma:associac¸ãooucoincidência?JPediatr(Rio J).2010;86:6---14.
19.BlackMH,SmithN,PorterA,JacobsenSJ,KoebnickC.Higher prevalence ofobesity among childrenwithasthma. Obesity. 2012;20:1041---7.
20.KattanM,KumarR,BloomerbergGR,etal.Asthmacontrol, adi-posity,andadipokinesamonginner-cityadolescents.JAllergy ClinImmunol.2010;125:583---92.
21.QuintoKB,ZurawBL,PoonKY,ChenW,SchatzM,Christiansen SC.Theassociationofobesityandasthmaseverityandcontrol inchildren.JAllergyClinImmunol.2011;128:964---9.
22.VenturaRN,NaspitzC,PucciniRF,DaSilvaEMK.Avaliac¸ãodo programadeatenc¸ãoacrianc¸asasmáticasacompanhadasnas UnidadesdesaúdedoMunicípiodeEmbu,SãoPaulo,noperíodo de1988a1993.CadSaúdePublica.1998;14:117---28.
23.Brasil. Ministério da Saúde. Portaria N◦ 2.981/GM, 26 de
novembro de 2009. Regulamentac¸ão do componente
espe-cializado da Assistência Farmacêutica no âmbito de SUS
[homepage on the Internet] [accessed 20.03.14]. Available
from:http://www.saude.gov.br.
24.StrufaldiMWL,DaSilvaEMK,PucciniRF.Sobrepesoeobesidade emescolarespré-púberes:associac¸ãocombaixopesoaonascer eantecedentesfamiliaresparadoenc¸acardiovascular.Embu ---RegiãometropolitanadeSãoPaulo,2006.CiêncSaúdeColet. 2011;16:4465---72.
25.IVDiretrizesBrasileirasparaoManejodaAsma.JBrasPneumol. 2006;32:S447---74.
26.WHO. World Health Organization. The WHO child growth
standards: length/height-for-age, weight-for-age and body
massindex-for-age.Methodsanddevelopment.Geneva:World
Health Organization; 2006 [homepage on the Internet. Acta
PaediatrSuppl2006;450:1---101][accessed20.03.14].Available
from:http://www.who.int/childgrowth/en/
27.WHO. World Health Organization. Development of a WHO
growth reference for school-aged children and adolescents
[homepage on the Internet], vol. 85. World Health
Organi-zation; 2007. p. 660---7 [accessed 20.03.14]. Available from:
http://www.who.int/growthref/en/
28.VenturaRN,PucciniRF,DaSilvaEMK.Avaliac¸ãonutricionalde crianc¸asportadorasdeChiadonoPeitoatendidasnasUnidades BásicasdeSaúdedoJardimSantoEduardoedoJardimSanta Emília,MunicípiodoEmbu,noperíododemaio/88ajulho/93. RevPaulPediatr.1998;16:201---7.
29.Simões SM, DaCunha SS, Barreto ML, Cruz AA. Distribuic¸ão da gravidade da asma na infância. J Pediatr (Rio J). 2010;86:417---23.
30.DalcinPTR,MenegotoDM,ZanonatoA,etal.Factorsassociated withuncontrolledasthmainPortoAlegre,Brazil.BrazJMedBiol Res.2009;42:1097---103.