w w w . r b o . o r g . b r
Original
Article
Alignment
of
the
tibial
component
in
total
knee
arthroplasty
procedures
using
an
intramedullary
or
extramedullary
guide:
double-blind
randomized
prospective
study
夽
Bruno
da
Rocha
Moreira
Rezende
∗,
Thiago
Fuchs,
Rodrigo
Nishimoto
Nishi,
Munif
Ahmad
Hatem,
Luciana
Mendes
Ferreira
da
Silva,
Rogério
Fuchs,
Paulo
Gilberto
Cimbalista
de
Alencar
HospitaldeClínicas,UniversidadeFederaldoParaná,Curitiba,PR,Brazil
a
r
t
i
c
l
e
i
n
f
o
Articlehistory:
Received19January2014 Accepted20March2014 Availableonline12March2015
Keywords: Arthroplasty Knee
Instrumentation Kneeosteoarthritis
a
b
s
t
r
a
c
t
Objectives:To evaluate the results obtained through using an intramedullary or extramedullaryguideforsectioningthetibiaintotalkneearthroplastyprocedures,with aviewtoidentifyingtheaccuracyoftheseguidesandwhetheronemightbesuperiortothe other.
Methods:Thiswasarandomizeddouble-blindprospectivestudyon41totalknee arthro-plastyproceduresperformedbetweenAugust2011andMarch2012.Theanglebetweenthe baseofthetibialcomponentandthemechanicalaxisofthetibiawasmeasuredduringthe immediatepostoperativeperiodbymeansofradiographyinanteroposteriorviewonthe tibiathatencompassedthekneeandankle.
Results:Therewasnodemographicdifferencebetweenthetwogroupsevaluated.Themean alignmentofthetibialcomponentinthepatientsofgroupA(intramedullary)was90.3◦
(range:84–97◦).IngroupB(extramedullary),itwas88.5◦(range:83–94◦).
Conclusion:Inourstudy,wedidnotfindanydifferenceregardingtheprecisionoraccuracyof eitheroftheguides.Somepatientspresentanabsoluteorrelativecontraindicationagainst usingoneorotheroftheguides.However,fortheothercases,neitheroftheguideswas superiortotheotherone.
©2015SociedadeBrasileiradeOrtopediaeTraumatologia.PublishedbyElsevierEditora Ltda.Allrightsreserved.
夽
WorkdevelopedintheHipandKneeSurgeryGroupofHospitaldeClínicas,UniversidadeFederaldoParaná,Curitiba,PR,Brazil.
∗ Correspondingauthor.
E-mails:brezende77@gmail.com,brezende@icloud.com(B.R.M.Rezende).
http://dx.doi.org/10.1016/j.rboe.2015.02.013
Alinhamento
do
componente
tibial
em
artroplastia
total
do
joelho
com
o
uso
de
guia
intramedular
ou
extramedular:
um
estudo
prospectivo,
randomizado,
duplo
cego
Palavras-chave: Artroplastia Joelho
Instrumentac¸ão Osteoartritedojoelho
r
e
s
u
m
o
Objetivos: Avaliarosresultadosobtidoscomousodeguiaintramedularouextramedular paraocortetibialemartroplastiastotaisdojoelho,comvistasaidentificarsuaacuráciae asuperioridadedeumemrelac¸ãoaooutro.
Métodos: Estudoprospectivo,randomizado,duplocegode41artroplastiastotaisdejoelho feitasentreagostode2011emarc¸ode2012.Foimedidooânguloentreabasedocomponente tibialeoeixomecânicodatíbianoperíodopós-operatórioimediatopormeioderadiografia emincidênciaanteroposteriordatíbiaqueengloboujoelhoetornozelo.
Resultados:Nãohouvediferenc¸ademográficaentreosdoisgruposavaliados.Oalinhamento médiodocomponentetibialnospacientesdogrupoA(intramedular)foide90,3◦(84◦-97◦).
NogrupoB(extramedular),foide88,5◦(83◦-94◦).
Conclusão: Nãoencontramos,emnossoestudo,diferenc¸aquantoàprecisãoouacuráciade qualquerumdosguias.Algunspacientesapresentamcontraindicac¸ão,absolutaourelativa, paraousodeumououtroguia.Todavia,paraosdemaiscasos,nãohásuperioridadede algumdeles.
©2015SociedadeBrasileiradeOrtopediaeTraumatologia.PublicadoporElsevier EditoraLtda.Todososdireitosreservados.
Introduction
Currently,thenumberoftotalkneearthroplasty(TKA) pro-cedures performed is increasinggreatly, influenced by the agingofthepopulation,increasingnumbersofindicationsand largernumbersofproceduresperformedonyoungpatients.1–3
Thus,thesearchforbetterclinicalresultsandlongersurvival ofimplantshasbecomethesubjectofmanystudiesonthis topic.
Thelong-termresultsfromTKAareinfluencedbyseveral factors,suchaspatientselection,implantcharacteristicsand surgicaltechnique.4Regardingthetechnique,onefactorthat
isbelievedtohaveanimportantroleisthealignmentofthe lowerlimb,withregardtorestorationofthemechanicalaxis, andespecially,anadequateangleforthetibialcomponent4–8
(Fig.1).Severalauthorshavecorrelatedanangleof88–92◦in
thecoronalplane,betweenthetibialplateauandthe mechan-icalaxisofthetibia,withbetterresultsandgreatersurvivalof theimplant.5,7,9
Technological advances and the evolution of surgical instrumentsandcomponentshaveenabledgreater intraop-erative precision and, through this, greater possibilities of achieving positioning and alignment closer towhat would beconsideredideal.In thisregard,the guidesusedforthe femoralandtibialcuts,whichmaybeintraorextramedullary, are ofgreatimportance. For the femur, thestandard is an intramedullaryorientation inmostcases. However,forthe tibia,thereisnoconsensusregardingthebestreferencepoint touse.5–8
Weconducted the present study with the aim of com-paring the alignments of tibial components obtained by means of intra and extramedullary guides, in cases of TKA.
Materials
and
methods
Thepresent study wasapprovedbyourinstitution’s ethics committeeforresearchonhumanbeings.Forthisstudy,we selected patients withan indication for TKA who fulfilled the followinginclusioncriteria: primaryoperation; without deformitiesofthetibiainthesagittalorcoronalplane; with-out presenceofosteosynthesismaterialthatwouldimpede thepassageoftheintramedullaryguide;andwithoutsevere
obesity or increased soft-tissue volume that would cause difficultyinpalpatingthebonestructurestolocatethe refer-encepointsfortheextramedullaryguide.Otherpatientswere excluded,aswerethosewhodidnotagreetosignthefreeand informedconsentstatement.
Forty-threepatients fulfilledthe criteria and underwent operations between August 2011 and March 2012. Two of these patients were subsequently excluded because their radiographiccontrolexaminationswereofpoorquality,thus makingitimpossibletoadequatelymeasurethealignmentof thetibialcomponent. Thus,41patientsremainedandwere evaluatedinthepresentstudy.
At the time when anesthesia was induced, these 41
patientswererandomizedbymeansofadrawthatconsisted ofusingsealedenvelopesthateachcontainedagroup allo-cation.Inthefirstgroup(A),thetibialcutwasmadeusing an intramedullary guide; and in the second group (B), an extramedullaryguidewasused.Allthepatientshad under-gonepreoperativeradiographytoproducethefollowingviews: anteroposteriorviewofthekneewhilestandingononefoot; lateralview;axialviewofthepatella;andpanoramicviewof thelowerlimbs.Thesewereusedfordiagnosticpurposesand forpreoperativeplanning.
Thesurgicalprocedureswereperformedbysurgeonswith different levels of experience, including some who were undergoingtrainingatourservice. Thesamesurgical tech-nique was used in all the cases, consisting of using a pneumatic tourniquet on the root of the thigh; a medial longitudinalcutaneousaccesstotheknee;medial parapatel-lararthrotomy; and lateral dislocationofthe patella. After debridementandresectionofosteophytes,menisciandthe anterior cruciate ligament (ACL), a femoralcut withmade usingtheintramedullaryguide,atavalgusangleof5◦ or6◦
andatanexternalrotationof3◦.Followingthis,atibialcut
wasmade,withsacrificingoftheposteriorcruciateligament (PCL)anduseofanintramedullaryguideamongthepatients ingroupA,orandextramedullaryguideingroupB.Thiswas followedbycomponenttestingandligamentbalancing.Lastly, thedefinitivecomponentswerecementedin.Inallcases,the Advance®MedialPivotprosthesiswasused(WrightMedical, Arlington,TN,USA).
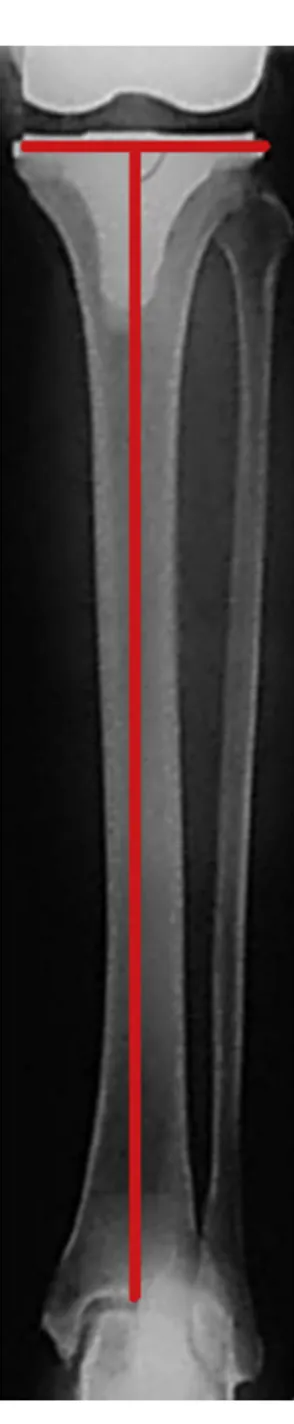
Thealignmentofthetibialcomponentwasevaluatedby means of radiographs ofthe tibia in anteroposterior view, encompassingthekneeandankle,withthepatellaabsentas areferenceforneutralrotationofthelowerlimb(Fig.1).These were producedduringthe immediatepostoperativeperiod. Theangleofthetibialcomponent,formedbetweenthetibial baseandthemechanicalaxisofthetibia(Fig.2),wasmeasured usingagoniometerwithaprecisionof1◦. Valuesof88–92◦
wereconsiderednormal;those greaterthan92◦ werevarus
angles;andthoselowerthan88◦ werevalgusangles(Fig.3).
Theradiographswereevaluatedbyanexaminerwithout pre-viousknowledgeofthegrouptowhicheachpatientbelonged (Fig.4).Varusangles(over90◦)wereconsideredtobepositive,
andvalgusangleswereconsideredtobenegative(Fig.3). The statistical analysis was performed using the Bio-Calc application (Enet Inc., Columbus, OH, USA). The null hypothesis was rejected at the significance level of 0.05 and the parametric T test was used to compare unpaired samples.
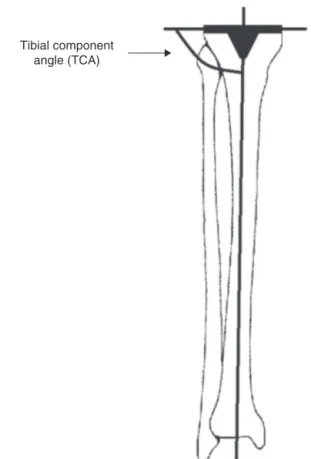
Tibial component angle (TCA)
Fig.2–Tibialcomponentangle(TCA)andlateralviewof theleg,encompassingthekneeandankle.Postoperative situation.
Results
Out of the 41 patients, 22 were allocated to group A (intramedullary guide). These comprised 16 women and six men, with a mean age of 61.4 years (range: 39–78), with a preoperative diagnosis of primary gonarthrosis in 16 cases, rheumatoid arthritis in five cases and juvenile rheumatoidarthritisinonecase.IngroupB(extramedullary guide), there were 19 patients, of whom 13 were women and six were men, with a mean age of 62.4 years (range: 26–79) and with adiagnosis ofprimary gonarthrosis in 13 cases, rheumatoidarthritisin fourcases, juvenile rheuma-toid arthritisin onecaseand osteonecrosis ofthefemoral condyle inonecase. Therewas no differencebetween the groups with regard to age, sex or preoperative diagnosis
(Table1).
Themeanalignmentofthetibialcomponentamongthe patientsingroupA(intramedullary)was90.3◦(range:84–97◦).
In13ofthe22cases(59.1%),thealignmentwasconsidered to be adequate, while four cases presentedvalgus (18.2%) andfivepresentedvarus(22.7%).IngroupB(extramedullary), the mean alignment was 88.5◦ (range: 83–94◦). Itwas
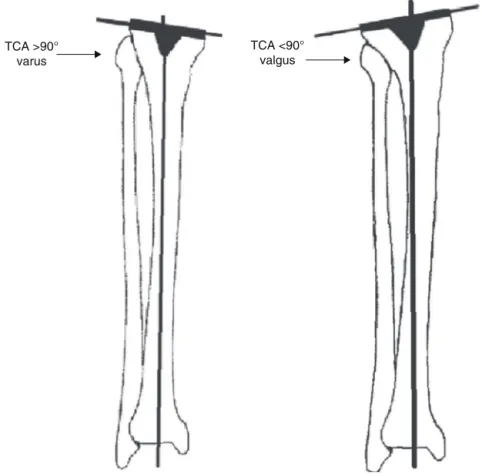
TCA >90° varus
TCA <90° valgus
Fig.3–Tibialcomponentangle(TCA)>90◦:varus.Tibialcomponentangle(TCA)<90◦:valgus.
Table1–Demographicdata.
Variables GroupA GroupB p-Value
Patients 22 19 NS
Age 61.4±9.3a 62.4±11.8a NS Gender(male/female) 16/6 13/6 NS
Diagnosis
Primary 16 13 NS
RA 5 4
JRA 1 1
ON 1
RA,rheumatoidarthritis;JRA,juvenilerheumatoidarthritis;ON, osteonecrosis;NS,notsignificant.
a Mean±standarddeviation.
Table2–Tibialcomponentangle(TCA).
GroupA GroupB p-Value
Patients 22 19 NS
TCA(degrees) 90±3.2◦a 88.5±3.1◦a NS TCAadequate 13/22 10/19 NS
(59.1%) (52.6%)
TCAinadequate 9/22 9/19 NS
Varus 5 2
Valgus 4 7
TCA,tibialcomponentangle;NS,notsignificant. a Mean±standarddeviation.
Discussion
Several factors have been correlated with success in TKA procedures.Therearecharacteristicsrelatingtothepatient, such asage, sex and body massindex.1–3 Others relateto
thesurgicaltechnique:restorationofthelimbalignment, cor-rectpositioningofthecomponentsandsatisfactoryligament balance.4–8 Itwasobservedthatthere hasbeen major
evo-lutionininstrumentdesign,whichnow allowssurgeonsto performpreciseoperations.Thisseemstohaveinfluencedthe resultsmoresignificantlythantheprosthesismodelhas.
Althoughnotthemainobjectiveofourstudy,weobserved considerablevarianceinthevaluesfortheangleofthetibial component.Nonetheless,themeanobtainedwassatisfactory. Webelievethatthereareotherfactorsjustasimportantfor thesuccessofaTKAprocedureastheangleofthetibial com-ponent, particularlywithregardtotheligament balanceof theknee.Hence,theexactnessofthetibialcomponentangle of90◦perhapsisnotfundamental.However,sincethe
objec-tiveinusingtheguides(bothintraandextramedullary)wasto obtainatibialcomponentangleof90◦,theresultwas
Fig.4–Tibialcomponentangle(TCA)measuredona postoperativeradiograph.
Table3–AccuracyoftheTCAafterTKA.
Reference N Accuracy(%)a
Jefferyetal.13 115 68
Reedetal.8 135 85(intra)–65(extra) Ishiietal.6 100 88
Dennisetal.5 120 88(intra)–72(extra) Maestroetal.4 116 90.1(intra)–87.2(extra) Ourstudy 41 59.1(intra)–52.6(extra)
a Tibialcomponentangle(TCA)neutral±2◦.
notseparatedaccordingtosurgeon,althoughthismighthave clarifiedtheextenttowhichpersonalexperienceplaysarole inobtainingthe expectedresults. Inany event,we believe thatthereisroomfordiscussionontheuseofnavigation sys-temsinTKAprocedures.Giventhatprecisecutsandadequate
finalalignmentaresought,navigationmayreducethe varia-tionresultingfromindividualjudgmentandproduceresults thataremorehomogenous.1,10 Therearecertaindifficulties
in undertakinggeneralintroduction ofnavigation systems, suchasthecost,theincreasedduration ofsurgeryandthe needforspecificsoftwareforeachimplant.11 Thereisalso
thepossibilityofcomplications,suchasfracturesatthe fix-ationpointsforthefemoralandtibialguides,becauseofthe pinsthatfirmlyholdthepositionsensorsforthenavigation. Nonetheless,webelievethattechnologicaltoolsthatimprove thegeneralresultsandmakethemlessdivergentshouldbe studiedandpossiblyused,sothatthefinalresultsfromTKA mightbecomemorepredictable.
Regarding the surgical technique, restoration of the mechanicalaxisofthelowerlimbisusuallysoughtthrougha jointlinethatisparalleltotheground,andthefinal anatom-icalaxisisatavalgusanglerangingfrom 5◦ to7◦ inmost
cases.5AccordingtoIshiietal.,6theoverloadonthemedial
compartmentreachesapproximately75%oftheload trans-mittedtotheknee,eveninpatientswithaneutralmechanical axis.6 Anotherimportantfactoristheinclinationofthe
tib-ialcomponent, whichaccordingtosomeauthorsshouldbe
90±2◦.5,7,9
Consideringthatoneofthesurgeon’sobjectivesduringthe procedureistoachieveadequatecuts,withaviewtoobtaining satisfactory finalalignment,theexistenceofpreciseguides is fundamental. In this regard, intra and extramedullary guides havebeen developed to performfemoral and tibial cuts. Regarding the femur, it seems that aconsensus that intramedullary guides should be used has been reached, consideringthatthelocalsoft-tissueenvelopemakesit dif-ficulttocorrectlyidentifythebone.6Ontheotherhand,for
thetibialcut,uncertaintiesregardingthebestorientationstill exist.5,6,8
Both the intramedullary and the extramedullary guide
present advantages and disadvantages. Regarding the
intramedullaryguide, notonlyisthereanincreasedriskof fatty embolism,12 butalsotherearegreatlimitationsonits
use,orevenimpossibility,incasesofbonedeformity, seque-lae of trauma or presence of osteosynthesis material that obliteratesthemedullarycanal.Regardingtheextramedullary guide, it becomes moredifficulttouse it in casesofgreat obesityorincreasedsoft-tissuevolumearoundthetibia.
Weconductedthepresentstudywiththeaimof identify-ingtheprecisionofthesetwooptionsforguidesforthetibial cut,andalsowhetheroneofthemmightbesuperiortothe other.Thus,twodemographically,radiologicallyandclinically comparablegroupswererandomizedsuchthatoneofthetwo guidesavailablewouldbeusedineachcase.However,inour study,wedidnotfindany differenceregardingprecisionor superiorityofoneguideovertheother.
Asmentionedearlier,somepatientspresentabsoluteor relativecontraindications againstusingoneor otherofthe guides.However,fortheothercases,neitheroftheguideswas superiortotheother.Ontheotherhand,webelievethatproper preoperativeplanningandmeticulousimplementationofthe planthathasbeenestablishedaremoreimportant, irrespec-tiveofwhichguideisusedforthetibialcut.
procedures,2–9,11,13 other factors may be asdeterminant as
thealignment,ormoreso,forthelong-termresults.Parratte etal.9followedup398kneesthatunderwentTKA,overa
15-year periodand analyzed the long-termresults. According totheseauthors,therewere nostatisticallysignificant dif-ferencesinrelationtothesurvivaloftheimplants,between thegroupsthatpresentedpostoperativemechanicalaxesat anglesof0±3◦,lessthan−3◦andgreaterthan3◦.Therefore,
itseemsthatthereareother factorsasdeterminantasthe alignment,orevenmoreimportantthanthis,forthesuccess ofTKAprocedures.
Conflicts
of
interest
Theauthorsdeclarenoconflictsofinterest.
r
e
f
e
r
e
n
c
e
s
1. MasonJB,FehringTK,EstokR,BanelD,FahrbachK.
Meta-analysisofalignmentoutcomesincomputer-assisted
totalkneearthroplastysurgery.JArthroplasty.
2007;22(8):1097–106.
2. WindsorRE,ScuderiGR,MoranMC,InsallJN.Mechanismsof
failureofthefemoralandtibialcomponentsintotalknee
arthroplasty.ClinOrthopRelatRes.1989;(248):15–9.
3. RandJA,TrousdaleRT,IlstrupDM,HarmsenWS.Factors
affectingthedurabilityofprimarytotalkneeprostheses.J
BoneJointSurgAm.2003;85(2):259–65.
4. MaestroA,HarwinSF,SandovalMG,VaqueroDH,MurciaA.
Influenceofintramedullaryversusextramedullaryalignment
guidesonfinaltotalkneearthroplastycomponentposition:a
radiographicanalysis.JArthroplasty.1998;13(5):552–8.
5.DennisDA,ChannerM,SusmanMH,StringerEA.
Intramedullaryversusextramedullarytibialalignment
systemsintotalkneearthroplasty.JArthroplasty.
1993;8(1):43–7.
6.IshiiY,OhmoriG,BechtoldJE,GustiloRB.Extramedullary
versusintramedullaryalignmentguidesintotalknee
arthroplasty.ClinOrthopRelatRes.1995;(318):167–75.
7.RitterMA,FarisPM,KeatingEM,MedingJB.Postoperative
alignmentoftotalkneereplacement:itseffectonsurvival.
ClinOrthopRelatRes.1994;(299):153–6.
8.ReedMR,BlissW,SherJL,EmmersonKP,JonesSM,Partington
PF.Extramedullaryorintramedullarytibialalignmentguides:
arandomised,prospectivetrialofradiologicalalignment.J
BoneJointSurgBr.2002;84(6):858–60.
9.ParratteS,PagnanoMW,TrousdaleRT,BerryDJ.Effectof
postoperativemechanicalaxisalignmentonthefifteen-year
survivalofmodern,cementedtotalkneereplacements.J
BoneJointSurgAm.2010;92(12):2143–9.
10.EnsiniA,CataniF,LeardiniA,RomagnoliM,GianniniS.
Alignmentsandclinicalresultsinconventionaland
navigatedtotalkneearthroplasty.ClinOrthopRelatRes.
2007;(457):156–62.
11.GarvinKL,BarreraA,MahoneyCR,HartmanCW,HaiderH.
Totalkneearthroplastywithacomputer-navigatedsaw:a
pilotstudy.ClinOrthopRelatRes.2013;471(1):155–61.
12.FahmyNR,ChandlerHP,DanylchukK,MattaEB,SunderN,
SiliskiJM.Blood-gasandcirculatorychangesduringtotal
kneereplacement.Roleoftheintramedullaryalignmentrod.J
BoneJointSurgAm.1990;72(1):19–26.
13.JefferyRS,MorrisRW,DenhamRA.Coronalalignmentafter