Prospective Comparative Study between Retroperitoneoscopic
and Hand-Assisted Laparoscopic Approach for Radical
Nephrectomy
Marcos Tobias-Machado, Pedro I. Ravizzini, Leonardo O. Pertusier, Eduardo Pedroso, Eric R.
Wroclawski
Division of Urologic Oncology and Laparoscopy (MTM, PIR, LOP, EP, ERW), ABC Medical School,
Santo Andre, Sao Paulo, Research and Educational Institute of Albert Einstein Jewish Hospital (MTM,
ERW) Sao Paulo, and Brazilian Institute for Cancer Control (MTM, ERW), Sao Paulo, SP, Brazil
ABSTRACT
Objective: No consensus has yet been established regarding the best minimally invasive access for radical ablation of renal tumors. Our objective was to prospectively compare the surgical results and oncologic management of two currently used endoscopic techniques.
Materials and Methods: Over a four-year period, 50 patients with renal tumors and clinical stage T1b-T2, smaller than 12 cm, underwent a radical nephrectomy at two reference institutions, 25 underwent retroperitoneoscopic radical nephrec-tomy (RRN) and 25 a hand-assisted laparoscopic radical nephrecnephrec-tomy (HALRN). Mean follow-up of both cohorts was 50 months. Operative parameters and oncological management were compared.
Results: The mean operative time was 180 min in RRN and 108 min in HALRN (p < 0.001). The time required to access the renal pedicle in RRN was 30 min. and in HALRN 40 min., Learning curve was shorter in HALRN than RRN. Mean blood loss was 100 mL in RRN and 242 mL in HALRN. Mean incision size for specimen retrieval in RRN was 6.5 cm and in HALRN 7.5 cm. One patient with intra operative occurrence of ascites and subsequent pathological stage pT2N0M0 grade 3 operated via HALRN, had neoplasic implants in the Hand-port incision 3 months after surgery followed by death 4 months after recurrence. One patient, with pathological stage pT3N0M0 grade 3 in RRN had metastasis after 36 months.
Conclusion: Both, RRN and HALRN techniques are accepted minimally invasive options for endoscopic radical nephrec-tomy with equivalent long term oncological outcome in the treatment of renal tumors.
Key words: kidney neoplasms; surgery; nephrectomy; laparoscopy
Int Braz J Urol. 2009; 35: 284-92
INTRODUCTION
Laparoscopic radical nephrectomy has been accepted as a treatment of choice for renal tumors with stage T1-T2 smaller than 8 cm when radical surgery is indicated (1-4).
There are three different minimally invasive approaches described for endoscopic ablation of the
The retroperitoneoscopic technique has won increasing world acceptance. Through this access, there is no intra-peritoneal manipulation, therefore reducing the chance of iatrogenic abdominal lesions (3).
The hand-assisted laparoscopic radical ne-phrectomy (HALRN), initially described in 1994 had not gained popularity until the introduction of hand-port devices for maintenance of the pneumoperi-toneum. The potential advantages of this technique are the adjunct of tactile sensation of the laparoscopic procedure, increased orientation, manual dissection access and retraction of anatomic structures. It is particularly useful when an incision is necessary to remove an intact surgical specimen or when a large size tumor has to be resected (5,6).
The aim of this study was to prospectively compare operative and oncologic outcomes of both techniques as different options for radical surgical treatment of renal cell carcinomas (RCC).
MATERIAL AND METHODS
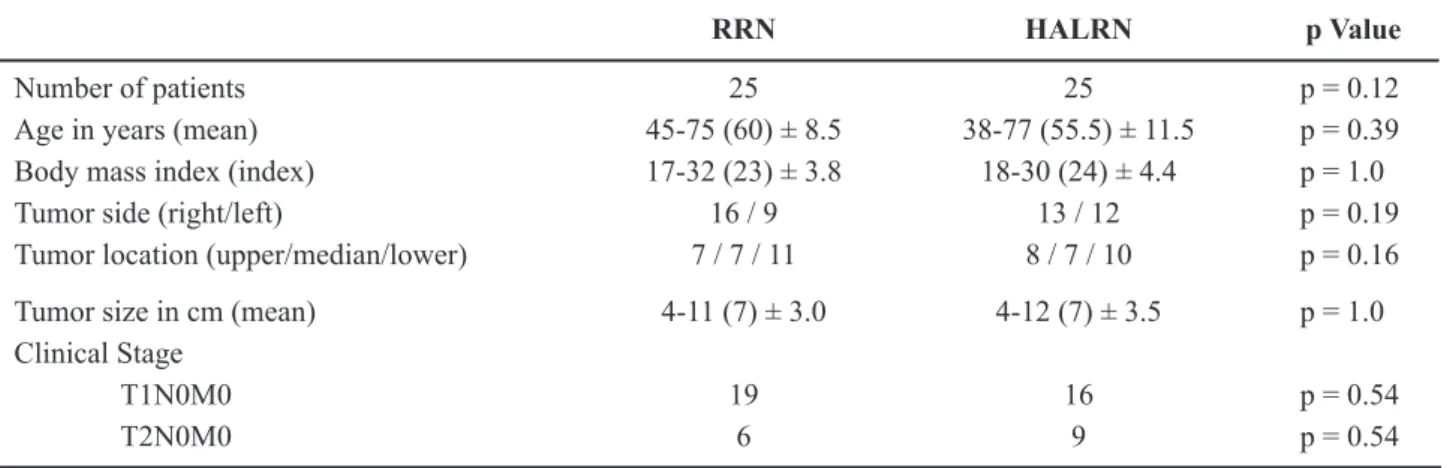
In a period from February 1999 to February 2003, 25 retroperitoneoscopic radical nephrectomies (RRN) and 25 HALRN were performed in the two institutions. Both groups were comparable regarding demographic data (Table-1). The patients presented good performance status (ASA score I or II) and no formal contraindications to the laparoscopic ap-proach. Fifty patients with the diagnosis of a solid renal mass, larger than 4 cm and smaller or equal to 12 cm, with clinical stage T1b-T2N0M0 RCC deter-mined by abdominal CT scan and chest X-ray, were prospectively included. Surgical procedures including cases of learning curve were performed at 2 regional referral teaching hospitals, by a single surgeon in each institution with experience in laparoscopic procedures. The two techniques were performed in accordance with the techniques previously described in literature (1,3). In the RRN group, there were 10 male and 15 female patients, with a mean age of 60 years (range 45 to 75), and a mean body mass index (BMI) of 24 (range 17 to 32). The mean size of the tumors in the pre-operative tomographic study was 7 cm (range 4 to 11) (Table-1). Nineteen (76%) of the patients had a clinical stage T1N0M0, and 6 (24%), T2N0M0. In
the HALRN group, there were 11 male and 14 female patients, with a mean age of 55.5 years (range 38 to 77) and mean BMI of 23 (range 18 to 30). Mean tumor size in tomographic study was of 7 cm (range 4 to 12) (Table-1). Sixteen (64%) of the patients presented clinical stage T1N0M0, and 9 (36%) T2N0M0. The two groups were compared according to operative time, learning curve (analyzing the irst 15 cases, and remaining 10 separately), time of access to renal pedicle, estimated blood loss, need for painkillers post-operatively, size of incision for specimen retrieval, complications, need for blood transfusion, specimen histopathologic analysis and oncologic management during a mean follow-up time of 30 months.
Statistical analysis used was Student-t-test and Chi-square test. The difference was considered signiicant at p < 0.05.
RESULTS
Intra-operative Data
Mean operative time was 180 min. (range 120 to 240) in the RRN group, and 108 min (range 80 to 140) in the HALRN (p < 0.001).
In the RRN group, the mean operative time for the irst 15 procedures was 220 min. (range 100 to 140), and for the remaining 15, 96 min. (range 80 to 120). The time of access to the renal pedicle after installing the portals was on average 30 min. (20 to 60) for the RRN, and 40 min. (30 to 75) for the HALRN group.
Adrenalectomy was executed in 18 patients (72%) of the 8 RRN group, and 12 (48%) of the HALRN group. Mean estimated blood loss was of 100 mL (range 30 to 200) in the RRN group, and 242 mL (range 160 to 320) in the HALRN group. Blood intra-operative transfusions were not required in any of the procedures in either group. Mean incision size for specimen retrieval of the RRN group was 6.5 cm (5 to 9), and for the HALRN group 7.5 cm (Table-2).
Intra-operative Complications
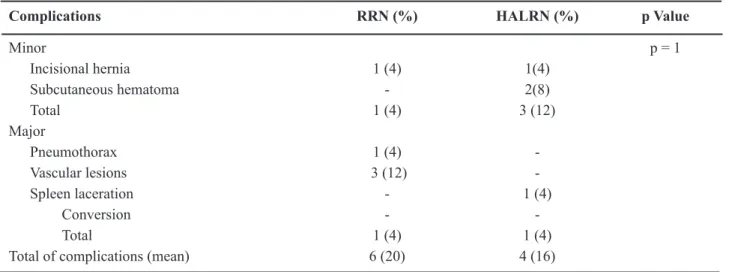
hernia at the site of the incision for specimen retrieval. Four patients (16%) had a major complication: one pneumothorax (treated by thoracic tube drainage), three vascular intra-operative lesions that were all controlled endoscopically.
In the HALRN group we observed complica-tions in 4 (16%) patients. Three (12%) presented mi-nor complications: two (8%) anterior abdominal wall hematomas (one patient, needed a second post-opera-tive day blood transfusion) and one (4%) incisional hernia at one of the 10 mm port sites. One (4%) of the patients presented an intra-operative splenic laceration and underwent a hand-assisted laparoscopic splenec-tomy. There were no conversions to open surgery in any of the groups (Table-3).
Postoperative Data
Mean time for first deambulation was 6 hours in RRN and 8 hours in HALRN group. Mean postoperative diet reintroduction time was 1.5 and 1.7 days in the RRN and HALRN group respectively. Mean hospital stay was 2.5 (1 to 4) days in the RRN group, and 2.2 (2 to 3) days in the HALRN group. The mean morphine equivalent intake requirement in the RRN group was 45 mg (range 17 to 120) and 55 mg (range 20 to 120) in the HALRN group. None of the patients needed I.V. analgesics after the second day hospital stay. Fourteen patients (56%) in the RRN group and 20 (75%) in the HALRN group continued taking paracetamol tablets for more than 2 Table 1 – Demographic data comparing retroperitoneoscopic radical nephrectomy (RRN) and hand-assisted laparoscopic radical nephrectomy (HALRN).
RRN HALRN p Value
Number of patients 25 25 p = 0.12
Age in years (mean) 45-75 (60) ± 8.5 38-77 (55.5) ± 11.5 p = 0.39 Body mass index (index) 17-32 (23) ± 3.8 18-30 (24) ± 4.4 p = 1.0
Tumor side (right/left) 16 / 9 13 / 12 p = 0.19
Tumor location (upper/median/lower) 7 / 7 / 11 8 / 7 / 10 p = 0.16
Tumor size in cm (mean) 4-11 (7) ± 3.0 4-12 (7) ± 3.5 p = 1.0 Clinical Stage
T1N0M0 19 16 p = 0.54
T2N0M0 6 9 p = 0.54
Table 2 – Intra-operative data comparing retroperitoneoscopic radical nephrectomy (RRN) and hand-assisted laparoscopic radical nephrectomy (HALRN).
RRN HALRN p Value
Operative time in min (mean) 120-240 (180) ± 42 80-140 (108) ± 42 p < 0.001 First 15 patients (mean) 200-240 (220) 100-140 (120)
Last 10 patients (mean) 120-160 (140) 80-120 (96) Time for renal pedicle access in min (mean) 20-60 (30) 30-75 (40)
Average blood loss in mL (mean) 30-200 (100) ± 382 160-320 (242) ± 204 p = 0.10
Need for intra-operative transfusion 0 0
Number of adrenalectomies 18 12
days. Mean time for convalescence was 3 weeks in the Retroperitoneoscopic group and 4 weeks in the Hand-assisted group (Table-4).
Histopathologic Data
In all patients a complete and intact re-moval of the surgical specimen was achieved. The diagnosis of renal cell carcinoma was conirmed in all patients in the RRN group. In the HALRN group, 23 specimens corresponded to renal cell car-cinomas, one presented as an oncocytoma, and the other as a renal adenoma. Pathologic stages in the Retroperitoneoscopic group was a T1N0M0 in 18
(72%), T2N0M0 in 4 (16%), T3N0M0 in 2 (8%) and T3N1M0 in 1 (4%) of the patients. In the Hand-as-sisted group, pathologic stages were T1N0M0 in 15 (60%), T2N0M0 in 6 (24%) and T3N1M0 in 2 (8%). The mean surgical specimen weight was 310g (95 to 410g) in the Retroperitoneoscopic group and 482g (130 to 800g) in the Hand-assisted group (Table-5).
Negative surgical margins were obtained in all surgical specimens. The RRN group specimens had a larger mean diameter size, 12.2 cm (8 to 20), and mean tumor size, 6.9 cm (3.5 to 11 cm) compared to the specimens of the HALRN group, which had an average size of 10.3 cm (9 to 22 cm) and mean tumors size of 6.4 cm (4 to 12 cm).
Table 3 – Surgical complications comparing retroperitoneoscopic radical nephrectomy (RRN) and hand-assisted laparo-scopic radical nephrectomy (HALRN).
Complications RRN (%) HALRN (%) p Value
Minor p = 1
Incisional hernia 1 (4) 1(4)
Subcutaneous hematoma - 2(8)
Total 1 (4) 3 (12)
Major
Pneumothorax 1 (4)
-Vascular lesions 3 (12)
-Spleen laceration - 1 (4)
Conversion -
-Total 1 (4) 1 (4)
Total of complications (mean) 6 (20) 4 (16)
Table 4 – Postoperative data comparing retroperitoneoscopic radical nephrectomy (RRN) and hand-assisted laparoscopic radical nephrectomy (HALRN).
RRN HALRN p Value
Mean time for irst deambulation 6 h ± 0.6 8 h ± 2.3 p < 0.001
Mean time for reintroduction of postoperative diet
1.5 days ± 0.35 1.7 days ± 0.3 p < 0.05
Hospital stay (mean) 1-4 days (2.5) ± 1.1 2-3 days (2.2) ± 2.3 p = 0.56 Analgesic intake (mean) 17-120 mg (45) ± 19.9 20-120 mg (55) ± 4.9 p = 0.018
Oncologic Follow-up
Mean follow-up time for the RRN and HALRN groups were respectively 48 months (36 to 58 mo) and 52 months (30 to 66 mo) respectively.
In the RRN group, one patient presenting with pT3N1M0 grade 3 stage developed local recurrence, adrenal and retroperitoneal metastasis, 36 months after surgical resection. At the moment the patient is under-going interferon therapy, and is still alive 40 months after surgery. There were no deaths in this group.
In the HALRN group, there was one death not-related to the neoplasia. Also, one patient with pT3N1M0 grade 3 stage, presented 4 months after surgery with subcutaneous tumors at one of the 10 mm laparoscopic ports and Hand-port incision sites. The patient also was found to have another implant site on the anterior abdominal wall, with no relation to surgical incisions. The patient died 4 months after surgery. This patient was diagnosed intra-operatively with ascites and signs of the peritoneal carcinomatosis at the time of HALRN. There were no other cases of disease recurrence in this group.
COMMENTS
Radical nephrectomy is considered the es-tablished treatment for renal cell carcinoma. Several
published data suggests that laparoscopic radical nephrectomy for stage T1-2 tumors, smaller than 8 cm, present relative advantages, reducing morbidity compared to the open technique, with better post-op-erative recovery and shorter return to normal activities (4,7).
The ideal minimally invasive method is not yet widely deined. Radical laparoscopic pure ne -phrectomy can be performed via a trans-peritoneal and a retro-peritoneal approach. Retroperitoneoscopic radical nephrectomy is currently gaining increasing world acceptance for the treatment of renal tumors (3,8,9).
Hand-assisted laparoscopic radical nephrec-tomy has been presented as another technical option and, according to some authors, is considered best indicated in selected cases (10,11). Some reports sug-gest that the choice between endoscopic techniques for renal ablation depends on the experience and preference of the surgeon, as well as the advantages, and disadvantages offered by each technique.
Regarding the indications, the retroperito-neoscopic access has been recommended for patients with previous abdominal surgery. Some authors avoid RRN when the tumor has a large volume, due to its smaller working space. On the other hand, Gill et al. (3) performed retroperitoneoscopic renal surgery in tumors with sizes of up to 12 cm. In our series, we also performed this technique, independently from Table 5 – Hystopathologic data comparing retroperitoneoscopic radical nephrectomy (RRN) and hand-assisted laparo-scopic radical nephrectomy (HALRN).
RRN HALRN p Value
Renal cell carcinoma 25 23
Specimen weight (mean) 95-410g (310) 130-800 (482) Specimen size (mean) 8-20 cm (12.2) 9-22 (10.3)
Tumor size (mean) 3.5-11 cm (6.9) ± 1.3 4-12 (6.4) ± 2.9 p = 0.44
Pathologic stage p = 0.50
T1N0M0 18 14
T2N0M0 4 7
T3N0M0 2
-T3N1M0 1 1
the size of the tumor, as long as the renal pedicle was apparently free of tumor on the CT scan images. For some authors, HALRN constitutes a selective indica-tion for larger tumors. HALRN could also be a more appropriate option for patients with co-morbidities where a shorter operative time would be advised.
Each of the techniques has some limitations and demands some kind of adaptation by surgeon. In the retroperitoneal access, as there is a less signiicant working space, small CO2 losses may make it dificult to perform surgery (12,13). Moreover, to avoid this problem, the surgeon should develop an adequate expansion of the retroperitoneal space, use rigorously sealed ports, perform optimized laparoscopic aspira-tion and increase CO2 replacement speed.
In HALRN the biggest limitation may be a smaller working space for hand insertion in the small abdominal cavities (12).
The main advantages of the retroperitoneo-scopic technique are the absence of intra abdominal manipulation, therefore reducing the chance of iatro-genic lesions of the intra-peritoneal organs (3,4,8,9), and the direct access to the renal pedicle allowing early control of the renal artery and vein (3,9). In our series we obtained faster access to the renal pedicle with RRN than with HALRN.
The main advantages for HALRN are a shorter operative time and facilitating the approach to masses of greater volume, especially in large sized kidney tumors. It also facilities, to some extent, vas-cular control in the case of a major vasvas-cular lesion and specimen retrieval at the end of the procedure.
Considering the learning curves for both tech-niques, HALRN has signiicantly shorter operative time for the initial cases than any pure laparoscopic technique, but there is less reduction in operating time when the technique is mastered (12). With RRN we observed a deinite impact on the learning curve, with signiicant reduction of operating time, when more experience is acquired. These results explain the larger acceptance of the Hand-assisted technique by surgeons with less experience in laparoscopic surgery. Our irst 15 cases, include as learning curve in a sample of 25 patients in each group however, this may be a limitation in our study.
Blood loss in the RRN group was smaller. Reported data are conlicting as we evaluated blood
loss on different endoscopic accesses for radical nephrectomy. A possible explanation for our results is that in the HALRN group, blunt dissection was employed throughout the procedure as a means of re-ducing operating time. In fact, in our data, the HALRN technique showed a signiicantly shorter operating time, which does not agree with the other author’s results. Again, blunt dissection may have had played an important role in reducing operating time but the difference obtained could be partially explained by the largest percentage of adrenalectomies performed in the RRN group.
When the requirement for analgesia and hospital stay was considered, there was no signiicant difference between both groups. Although it seems logical that the retroperitoneoscopic technique would require a smaller dosage of analgesics than Hand-as-sisted techniques, some comparative studies failed to demonstrate this advantage (10,11,13,14).
Complications rates in our study were similar for both techniques. The RRN group presented a high-er index of vascular lesions than the HALRN group. However, all lesions were controlled laparoscopically and no blood transfusions were necessary in any of the cases. These data are not in agreement with the series reported by other authors where major complications were more frequent for the Hand-assisted method (10,14-16). Minor complications represented by incisional hernia and parietal hematoma, were more frequent in the HALRN group. Parietal hematoma was caused by a partial epigastric arterial lesion at the 10 mm port site, detected post-operatively. An extensive abdominal wall hematoma was formed and blood transfusion was required in the second post-operative day.
The transverse incision for specimen extrac-tion in the retroperitoneoscopic technique is smaller, and may be applied to the lank, therefore in order to achieve a more aesthetic result. The incision for the Hand-port placement is generally longitudinal or oblique, larger in comparison, and is applied to the anterior abdominal wall, therefore producing a less aesthetic result.
in this study, surgeons opted for an intact specimen removal. Laparoscopic port site tumoral seeding was not observed in any cases from the RRN group over a period of 30 months. In our series, we had a patient, in each group, who presented metastases related to a high histologic grade with lymph node involvement. However, a longer follow-up period would be neces-sary to evaluate the oncological results related to each technique.
Our results suggest that in general, both techniques are equivalent and feasible in the treat-ment of renal malignant tumors. The knowledge of both surgical techniques is important for an adequate selection of the optimal minimally invasive access to be used in each case. The hand assisted technique in none of the referral centers was considered use-ful to introduce the practice of minimally invasive procedures.
CONCLUSION
Hand-assisted technique showed a relative reduction in operating time, which may be especially useful in more debilitated patients, and a good option for the treatment of large size renal tumors.
Retroperitoneoscopic technique provides early access to vascular control, permitting minimal blood loss. In addition, the removal of the specimen was possible by using a more aesthetic incision.
The comparison of long term oncological data seems to be similar using either one of these two techniques.
CONFLICT OF INTEREST
None declared.
REFERENCES
1. Gill IS: Laparoscopic radical nephrectomy for cancer. Urol Clin North Am. 2000; 27: 707-19.
2. Ono Y, Kinukawa T, Hattori R, Yamada S, Nishiyama N, Mizutani K, et al.: Laparoscopic radical
nephrec-tomy for renal cell carcinoma: a ive-year experience.
Urology. 1999; 53: 280-6.
3. Gill IS, Schweizer D, Hobart MG, Sung GT, Klein EA, Novick AC: Retroperitoneal laparoscopic radical nephrectomy: the Cleveland clinic experience. J Urol. 2000; 163: 1665-70.
4. Allan JD, Tolley DA, Kaouk JH, Novick AC, Gill IS: Laparoscopic radical nephrectomy. Eur Urol. 2001; 40: 17-23.
5. Tierney JP, Oliver SR, Kuminsky RE, Tiley EH, Lu-cente FC, Boland JP: Laparoscopic radical nephrec-tomy with intra-abdominal manipulation. Minimal Invas. Ther. 1994; 3: 303-5.
6. Kusminsky RE, Tiley EH, Lucente FC, Boland JP: Laparoscopic staging laparotomy with intra-abdominal manipulation. Surg Laparosc Endosc. 1994; 4: 103-5.
7. Gill IS: Retroperitoneal laparoscopic nephrectomy. Urol Clin North Am. 1998; 25: 343-60.
8. Dunn MD, Portis AJ, Shalhav AL, Elbahnasy AM, Heidorn C, McDougall EM, et al.: Laparoscopic versus open radical nephrectomy: a 9-year experience. J Urol. 2000; 164: 1153-9.
9. Abbou CC, Cicco A, Gasman D, Hoznek A, Antiphon P, Chopin DK, et al.: Retroperitoneal laparoscopic versus open radical nephrectomy. J Urol. 1999; 161: 1776-80.
10. Nelson CP, Wolf JS Jr: Comparison of hand assisted versus standard laparoscopic radical nephrectomy for suspected renal cell carcinoma. J Urol. 2002; 167: 1989-94.
11. Busby E, Das S, Rao Tunuguntla HS, Evans CP:
Hand-assisted laparoscopic vs the open (lank incision)
approach to radical nephrectomy. BJU Int. 2003; 91: 341-4.
12. Wolf JS Jr: Hand-assisted laparoscopy: pro. Urology. 2001; 58: 310-2.
13. Pareek G, Hedican SP, Gee JR, Bruskewitz RC, Nakada SY: Meta-analysis of the complications of laparoscopic renal surgery: comparison of procedures and techniques. J Urol. 2006; 175: 1208-13.
14. Matin SF, Dhanani N, Acosta M, Wood CG: Conven-tional and hand-assisted laparoscopic radical nephrec-tomy: Comparative analysis of 271 cases. J Endourol. 2006; 20: 891-4.
15. Venkatesh R, Belani JS, Chen C, Sundaram CP, Bhay-ani SB, Figenshau RS, et al.: Prospective random-ized comparison of laparoscopic and hand-assisted laparoscopic radical nephrectomy. Urology. 2007; 70: 873-7.
util-EDITORIAL COMMENT
This is an interesting prospective study comparing two laparoscopic approaches for radi-cal nephrectomy: a retroperitoneoscopic (RRN) and hand-assisted (HALRN) approach, which attempts to deine the best minimal access to this surgery. A shorter operative time and learning curve were in fa-vor of HALRN versus a minor blood loss and small-er incision for organ retrieval in favor of RRN. No differences in the complication rate were observed. After a mean follow-up of 50 months, no difference in oncological control was found.
Although the study was conducted prospec-tively, a randomized trial would have been a better way, even if more dificult to perform, to compare different surgical techniques.
An important issue that should be investi-gated in any comparative surgical technique study is the health-related quality of life (HRQoL). In the literature, there is little reported data regarding long-term HRQoL after RRN and HALRN performed for renal cancer. Patel et al. (1) using the SF-36 ques-tionnaire, showed no difference in terms of HRQoL between the two techniques with a mean follow-up ity of a 3-month minifellowship. J Laparoendosc Adv Surg Tech A. 2007; 17: 435-9.
17. Bandi G, Christian MW, Hedican SP, Moon TD, Nakada SY: Oncological outcomes of hand-assisted laparoscopic radical nephrectomy for clinically local-ized renal cell carcinoma: a single-institution study
with >or=3 years of follow-up. BJU Int. 2008; 101: 459-62.
18. Chung SD, Huang KH, Lai MK, Huang CY, Pu YS, Yu HJ, Chueh SC: Long-term follow-up of hand-assisted
laparoscopic radical nephrectomy for organ-conined
renal cell carcinoma. Urology. 2007; 69: 652-5.
Accepted after revision: February 16, 2009
Correspondence address:
Dr. Marcos Tobias-Machado Rua Grauna, 104 / 131
São Paulo, SP, 04514-000, Brazil Fax: + 55 11 4437-3118
E-mail: tobias-machado@uol.com.br
of 6 months, but studies with a larger patient popula-tion and a longer follow-up are required.
We agree with the authors’ statement that in general, both techniques are feasible for treatment of renal malignant tumors and the knowledge of both techniques should be theoretically familiar to the ex-perienced surgeon.
However, our impression is that both tech-niques, as stated, are not equivalent. A difference of one hour in surgical time is the most striking differ-ence described in this study and it should be con-sidered an extremely important factor today in view of budget cuts for hospital costs, also considering that additional costs of laparoscopic hand-assisted devices could be avoided (2). In addition, longer anesthesia is associated with an increase in the inci-dence of perioperative complications and mortality (3).
In search of the “Holy Grail” (i.e. the ideal minimally invasive method), this paper adds more information to the body of literature on laparoscopic radical nephrectomy. However, still today, the most important factor that guides the choice of a laparo-scopic technique depends on the surgeon’s experi-ence and personal preferexperi-ence.
REFERENCES
1. Patel A, Wilson L, Blick C, Gurajala R, Rané A: Health-related quality of life after
retroperitoneo-scopic and hand-assisted laparoretroperitoneo-scopic nephrectomy. J Endourol. 2005; 19: 849-52.
2. Ditonno P, Lucarelli G, Bettocchi C, Palazzo S, Palel-la GV, Battaglia M, et al.: “Deviceless” hand-assisted laparoscopic donor nephrectomy. Transplant Proc. 2008; 40: 1829-30.
3. Routh JC, Bacon DR, Leibovich BC, Zincke H, Blute ML, Frank I: How long is too long? The effect of the duration of anaesthesia on the incidence of non-uro-logical complications after surgery. BJU Int. 2008; 102: 301-4.