REVISTA
BRASILEIRA
DE
ANESTESIOLOGIA
OfficialPublicationoftheBrazilianSocietyofAnesthesiologywww.sba.com.br
SCIENTIFIC
ARTICLE
Comparison
of
the
i-gel
TM
and
the
Laryngeal
Mask
Airway
Classic
TM
in
terms
of
clinical
performance
Reyhan
Polat
∗,
Gözde
Bumin
Aydin,
Jülide
Ergil,
Murat
Sayin,
Tu˘
gba
Kokulu, ˙Ibrahim
Öztürk
DepartmentofAnesthesiology,DiskapiYildirimBeyazitResearchandTrainingHospitalDiskapi,Ankara,Turkey
Received18January2014;accepted5February2014 Availableonline6March2014
KEYWORDS
LaryngealMask
AirwayClassic;
i-gel;
Supraglotticairway
devices
Abstract
Purpose: Thei-gelTM isoneofthesecondgenerationsupraglotticairwaydevices.Our study wasdesignedtocomparethei-gelandtheLaryngealMaskAirwayClassicTMwithrespecttothe clinicalperformance.
Methods:Wecomparedtheperformanceofthei-gelwiththatoftheLaryngealMaskAirway Classic in 120patients undergoingurologic surgeryduringgeneral anesthesiawithout mus-clerelaxantwithrespecttothenumberofattemptsforsuccessfulinsertion,insertiontime, peak airway pressure,incidence ofregurgitation, fiberoptic glotticview andpostoperative complications.Secondgenerationsupraglotticairwaydeviceswereinsertedbythesame anes-thesiologist,experienced inuse ofbothdevices (>200uses andfirsttime failurerate<5%). Methylenebluemethodwasusedtodetectgastricregurgitation.
Results:There was no statisticaldifference between thetwo groups regarding thesuccess ofinsertionofsecondgeneration supraglotticairwaydevice(p=0.951).Thelaryngeal mask insertiontime forthei-gel groupwas significantlyshorterthanthatfor theLaryngealMask Airway Classic group(11.6±2.4sversus 13.1±1.8s[p=0.001]). Thefiberoptic glotticview scoresforthei-gelgroupwassignificantlybetterthanthatfortheonesfortheLaryngealMask AirwayClassicgroup(p=0.001).Onfiberopticview,therewasnosignofmethylenebluedye atanytimepoint ineithergroup.In addition,therewas nodifferencebetweenthegroups inpatient responseregardingthepresenceofasorethroatwhen questioned24hafterthe procedure(p=0.752).
Conclusion: Both devices had good performance with low postoperative complications and withoutoccurrenceofregurgitation.Thei-gelprovidedashorterinsertiontimeandabetter fiberopticviewthantheLaryngealMaskAirwayClassic.
© 2014SociedadeBrasileirade Anestesiologia.Publishedby ElsevierEditoraLtda.Allrights reserved.
∗Correspondingauthor.
E-mail:reyhanp9@gmail.com(R.Polat).
0104-0014/$–seefrontmatter©2014SociedadeBrasileiradeAnestesiologia.PublishedbyElsevierEditoraLtda.Allrightsreserved.
PALAVRAS-CHAVE
Máscaralaríngea
clássica; i-gel; Dispositivos supraglóticos
Comparac¸ãodamáscaralaríngeai-gel(i-gelTM)comamáscaralaríngeaclássica
(LMA-ClassicTM)emrelac¸ãoaodesempenhoclínico
Resumo
Justificativaeobjetivo:Ai-geléumdosdispositivossupraglóticosdesegundagerac¸ãoparao manejodasviasaéreas.Nossoestudofoiprojetadoparacompararai-gelTMeamáscaralaríngea clássica(LaryngealMaskAirwayClassicTM,LMA-C)emrelac¸ãoaodesempenhoclínico.
Métodos: Avaliamososdesempenhosdei-geleLMA-Cem120pacientessubmetidosàcirurgia urológicasobanestesiageralsemrelaxantemuscular.Comparamosonúmerodetentativasde inserc¸ãobem-sucedidas,otempodeinserc¸ão,apressãodepicodasviasaéreas,a incidên-ciaderegurgitac¸ão, avisibilidade daglotecomousode fibraópticaeascomplicac¸õesno pós-operatório.Osdispositivossupraglóticosdesegundagerac¸ãoforaminseridospelomesmo anestesiologistacomexperiência naaplicac¸ãodeambos os dispositivos(> 200aplicac¸ões e taxadefalhanaprimeiratentativa<5%).Ocoranteazuldemetilenofoiusadoparadetectar regurgitac¸ãogástrica.
Resultados: Nãohouvediferenc¸a estatísticaentreos doisgrupos em relac¸ãoao sucesso da inserc¸ão do dispositivo supraglótico de segunda gerac¸ão (p=0,951). O tempo de inserc¸ão da máscara laríngea no grupo i-gel foi significativamente menor do que no grupo LMA-C (11,6±2,4segundosvs.13,1±1,8segundos,p=0,001).Oescoredevisibilidade daglotevia fibraópticadogrupoi-gelfoisignificativamentemelhordoqueodogrupoLMA-C(p=0,001). Navisãoviafibraótica,sinaisdocoranteazuldemetilenonãoforamobservadosemqualquer momentoemambososgrupos.Alémdisso,não houvediferenc¸aentreasrespostasdos gru-posquandoperguntadossobreapresenc¸adedordegarganta24horasapósoprocedimento (p=0,752).
Conclusão:Ambososdispositivosapresentarambom desempenho,compoucascomplicac¸ões nopós-operatórioesemocorrênciaderegurgitac¸ão.Amáscaralaríngeai-gelproporcionouum tempodeinserc¸ãomaiscurtoeumavisãoviafibraópticamelhordoqueaLMA-C.
©2014SociedadeBrasileiradeAnestesiologia.PublicadoporElsevierEditoraLtda.Todosos direitosreservados.
Introduction
IntroductionofLaryngealMaskAirway(LMAClassicTM;
[LMA-C] Intavent Orthofix, UK), has changed the practice of
maintaining safe airway.1 Since then, supraglottic airway
devices(SGADs) havebeen usedsuccessfullyandsafely in
anestheticpracticewith variousmodels,and have
under-gonerapiddevelopment.2,3AlmostallSGADs,includingthe
LMA-C,useaninflatablecufftowedgeintotheupper esoph-agusandprovideaperilaryngealseal.4Accuratepositioning
andadequatepressureandvolumewithinthecuffare
fun-damentaltoachieve optimal function, and toreduce the
complications. A limiting factor for the use of SGAD is
thelackofairwayprotectionfromgastriccontents.5,6
Sev-eralSGADsarenowmarketedthatarespecificallydesigned
toreduce therisk of aspiration.The i-gelTM (Intersurgical
Ltd.,UK)is oneofthesecondgenerationSGADsproduced
forthispurpose. The cuffofthe i-gelisconstructed from
medical-grade thermoplastic elastomer (styrene ethylene
butadienestyrene)whichdoesnotrequireinflatingthecuff
or adjustingintra-cuff pressure.Its designenables a
mir-roredimpressionofthepharyngealandlaryngealstructures
andprovidesaperilaryngealsealwithoutcuffinflation.The potentialadvantagesofthei-gelareeasyandrapidinsertion
anda reductionin the risk of pharyngealtissue
compres-sionduetohigh cuffpressure.Moreover, ithasan inbuilt
drainage channel, which allows the insertion of a gastric
tube(maximum14Fgauge),tofacilitatetheefluxofgastric
fluidandgas.
This studycompares theclinical performance ofthe
i-gelwiththeLMA-Cintermsofinsertiontime,thenumber
ofattemptsforsuccessfulinsertion,peakairwaypressure,
fiberopticglotticview,incidenceofregurgitation,and
post-operative complicationswhich haveneverbeen compared
inarandomized-prospectivestudyinadultsinvivobefore.
Methods
ThisstudywasconductedbetweenJuneandSeptember2013
at DiskapiYildirim BeyazitResearchandTrainingHospital.
Thestudy(ref:06/27,date:12/17/2012)wasapprovedby
alocalresearchethicscommittee.Atotalof120patients,
whounderwenturologicsurgeryinlithotomypositionunder
general anesthesia with ASA physical status I---III (aged
18---70 years, weight 50---90kg), were assessed and
writ-teninformedconsentwastakenfromallpatientsenrolled
in the study. Patients with a history of gastroesophageal
reflux,hiatalhernia,previousgastricsurgeryorbodymass
index(BMI)>35kg/m2,andthosewhotakemedicationsfor
disorders of gastrointestinal motility were excluded from
the study.The patients were randomizedintotwogroups
(groupLMA-C,n=60,orgroupi-gel,n=60)bya
computer-generatedrandomnumbertable.TheinsertionofSGADswas
use of both devices(>200 uses andfirst timefailure rate <5%).
All patients’ demographic parameters (gender, age,
weight, height and body mass index), and the duration
of surgery were recorded. Patients were premedicated
with0.04mg/kgmidazolamivapproximately30minbefore
inductionofanesthesia.Agelatincapsulecontaining
methy-lene blue powder (25mg in lactose and 30mL of water)
wasingestedorallyinsittingpositionbythepatients10min beforeinductionofanesthesia.Thegelatincapsuledissolves
in wateror acidic pH 1---5solution within5min and turns
the gastric contents blue.7,8 Patient heart rate (HR) by a
three-channelECG,noninvasiveblood pressure,bispectral
index (BIS) (A-200 BIS monitoring system; Aspect Medical
systems,BISXP;Framingham,MA,USA),andpulseoximetry
weremonitored.Anestheticmanagementwasstandardized
according to the following protocol. Patients were
pre-oxygenated for 2min, and anesthesia was induced with
propofol(2---2.5mg/kg)andfentanyl(1.5---2g/kg).Inorder
toprovideconsistentconditions,insertionoftheSGADwas
madewhentheBISwasbelow60.BISvalueswerekept
sta-blebyinhalationalanesthesiathroughoutthestudyperiod.
Each devicewaslubricatedwithawater-based agentand
insertedaccordingtothemanufacturer’srecommendations.
Sizeselectionofthei-gelor LMA-Cdependedonpatient’s
weightinaccordancewiththeguidelines.TheLMA-Ccuffs
wereinflateduntiltheairleaksoundcomingfromthemouth
ceased (≤45cm3air). In orderto maintain adequate cuff
pressureforLMA-C,cuffpressurewasmaintainedinbyusing
ahandheldpressuregauge(VBMMedizintechnikGmbH,Sulz
a.N.,Germany).
Anesthesia wasmaintained with 1.5---2% sevoflurane in
50% oxygen---air mixture without using any neuromuscular
blockers,andremifentanilinfusionwasstartedatadoseof
0.2---0.3g/kg/min.Manualbagventilationwasmaintained
inallpatientsthroughacirclesystemuntilinsertionofSGAD
andvalidationofplacement.
InordertoinserttheSGAD,amaximumofthreeattempts
wasmadeforeachgroup.Ifitwasnotpossibletoventilate
the lungs, the following adjustments were allowed: neck
extensionorflexion,chin lift,jawthrustandgentle
push-ingor pullingof thedevice. Wheninsertion ofboth SGAD
modelsfailed,thesubjectwasexcludedfromthestudyand
theairwaywasmaintainedby an endotrachealtube.
Cor-rectinsertionwasassessedbyproperchestexpansion,the
presence of a curved CO2 wave on the capnography, the
absenceofaudibleleak,andlackofgastricinsufflation.The
presenceofgastric insufflationwasdeterminedby
epigas-tric auscultation.In both groups, insertionsuccess of the
SGAD(thenumberofairwaymanipulations),timerequired
to establish the airway (the total time from grasping of
the device toobserving asquare wave capnographtrace)
andcomplicationssuchaslaryngospasm,apnea,orhiccups
were recorded. After obtaining an effective airway, the
devicewasconnectedtoacirclebreathingsystem(Primus,
Drager,Lubek,Germany).Thelungswereventilatedwitha
tidalvolumeof 7mLkg−1,arespiratoryrateof12breaths
per minute, and I:E ratio of 1:2 and peak airway
pres-sure of approximately12---20cmH2O in volume controlled
mode. Peak airway pressure values were recorded. After
ensuringsatisfactoryventilation,theanatomicalpositionof
LMA-Candi-gelwasassessedusingafiberopticendoscope
(2.8mm;Olympus,Tokyo,Japan)viatheairwaytubeofthe
device.Thefiberscopewasalwayskeptstraight
(anatomi-calposition)tomaintaincontroloverthetip.Thetipofthe
fiberscopewaspositionedjustabovethebarsoftheLMA-C
ori-gel.Theviewviatheairwaychannelswasscoredas
fol-lows:Grade4,onlyvocalcordsareviewed;Grade3,vocal
cordsand posterior epiglottis areviewed; Grade 2, vocal
cordsandanteriorepiglottisareviewed;Grade1,cordsare
notviewedbutfunctioningadequately.9,10
To prevent false-positive regurgitation,the
oropharyn-gealcavity wasinspected for blue dye. Afterinsertion of
SGAD,thepresenceorabsenceofbluedyeinthebowlwas
assessedusingafiberscope.Additionally, beforeSGADwas
removed,fiberscopywasrepeatedagaintofindouttracesof methyleneblueinallthepatientsattheendofthe
surger-ies.AfterremovalofSGAD,thedevicesusedforfiberscopy
wereinspectedvisuallyfortraceofbluestainingandblood byoneoftheinvestigatorsandtheresultsofthese
inspec-tionswererecorded.
Once surgerywascompleted, sevofluraneand
remifen-tanilwerediscontinued.Whenthepatientwasabletoopen
hisorhermouthfollowingourcommand,theairwaydevice
wasremovedafterpharyngealsuctioningandliftingofthe
jaw.Then,thepatientwasgiven100%oxygenviafacemask
for10min.
The patients were interviewed in the post-anesthetic
careunitbynurseswhowereblindtostudy,withrespectto
thepresenceofsorethroatanddysphagia.Whenmodified
Aldretescoreswere10andabove,thepatientswere
trans-ferredtotheirrooms.Twenty-fourhoursaftersurgery,the
patientswereaskedonemoretimeiftheyhadsorethroat
anddysphagia.
Statisticalanalysis
Thesamplesizeof55pergroupwasdeterminedbypower
analysis;duetothepreliminarystudyresultsofdecreasein
insertiontimemeasurements,whendeltawasassumedtobe
1.25andSDas2.0,with90%powerand˛:0.05,thesample
size(n)wascalculatedtobeminimum55for eachgroup.
Consideringa10%drop-outrate,thenumberofsubjectswas
calculatedtobe60ineachgroup.
All statistical analyses were performed by using SPSS
15.0softwarepackage(SPSSInc.,Chicago,IL,USA).Ttest
forindependentsampleswasusedtocomparetwogroups
fordatawithnormaldistributionandMann---WhitneyUtest
wasusedforcomparingdatawithnon-normaldistribution.
Yates continuity correction test, Fisher’s exact test and
Fisher---Freeman---Haltontest were usedfor comparisonof
qualitativedata.
Alldatawere summarizedasmean±SDfor continuous
variables,numbers and percentages for categorical
varia-bles.Ap<0.05wasacceptedasstatisticallysignificant.
Results
Bothgroups were comparablewith respectto age,
male-to-femaleratio,height,weight,andbodymassindex.The
Table1 Baselinecharacteristicsofpatientswhounderwentanesthesiawiththei-gelorLaryngealMaskAirwayClassic(LMA-C). Dataareexpressedasmean±SD.
i-gel(n=59) LMA-C(n=59) p
Age(years) 48±15 50±17 0.619
Weight(kg) 77.9±10.5 75.9±14.1 0.384
Height(cm) 169.1±9.9 168.4±8.1 0.656
Bodymassindex(kg/m2) 27.3±3.5 26.7±4.4 0.436
Durationofsurgery(min) 48.6±16.1 47.5±23.5 0.753
Table2 Comparativedataforthei-gelandLaryngealMaskAirwayClassic(LMA-C).Dataareexpressedasnumber(proportion) ormean±SD.
i-gel(n=59) LMA-C(n=59) p
Insertiontime(s) 11.6±2.4 13.1±1.8 0.001
Peakairwaypressure(cmH2O) 12.4±2.2 12.6±2.4 0.753
Glotticviewa 0.001
4 19(32.2%) 1(1.7%)
3 16(27.1%) 10(16.9%)
2 14(23.7%) 19(32.2%)
1 10(16.9%) 29(49.2%)
aTheglotticviewviafiberopticexaminationwasscoredusing thefollowing:score 4,clearviewofthevocalcords;score3,only
arytenoidvisible;score2,onlyepiglottisvisible;score1,larynxnotvisible.
120 patients
LMA-C (n=60)
1st attempt 53/60(89.8%)
2nd attempt 1/60(1.69%)
3rd attempt 5/60(8.4%) 3rd attempt
3/60(5%) 2nd attempt
3/60(5%) 1st attempt 53/60(89.8%)
i-gel (n=60)
Failure 1/60 Failure 1/60
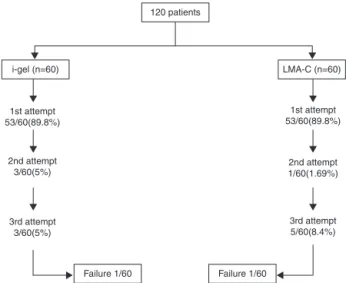
Figure1 Flowchartofthestudy,showingthesubdivisioninto groupscorrespondingtoeachsupraglotticairwaydevice.
Inthei-gelgroup,theSGADwassuccessfullyinsertedin
53patients (89.8%)at thefirstattempt, inthreepatients
(5.0%)atthesecondattempt,andinthreepatients(5.0%)
at the third attempt. In the LMA-C group, the SGAD was
successfully inserted in 53 patients (89.8%) at the first
attempt,inonepatient(1.69%)atthesecondattempt,and
infivepatients(8.4%)atthethirdattempt.Thereweretwo
patientsinwhomneitherthei-gelnortheLMA-Ccouldbe
inserted.Therewasnostatistical differencebetween two
groupsregardingtosuccessofinsertionofSGAD(p=0.951) (Fig.1).
Duration of laryngeal mask insertion time in the i-gel
group wassignificantly shorter than that in group LMA-C.
Themeanlaryngealmask insertiontimeswere11.6±2.4s
in i-gel and13.1±1.8s in LMA-C group (p=0.001). Three
patients in group LMA-C (5.0%) andfive patients in group
i-gel (8.4%) suffered from hiccups, which was the only
complication(p=0.717).Nolaryngospasmandapneawere
observedinanyofthepatients.
Peak airway pressure values measured by the
venti-lator were remarkably close for the two groups. The
mean peak airway pressures were 12.4±2.2cmH2O and
12.6±2.4cmH2Oin i-gelgroup andLMA-C group,
respec-tively (p=0.753). The fiberoptic viewscores for the i-gel groupweresignificantlybetterthanthatfortheLMA-Cgroup (p=0.001)(Table2).
Therewerenosignsofmethylenebluedyeinfiberoptic
viewatbeginning,afterinsertionofdevices,andjustbefore
removalofdevicesinbothgroups.Bluishdiscolorationwas
notseenafterremovalofanyofthedevices.
Bloodstainingwasencounteredrarelyafterremovalof
the devices in both groups; however, it was comparable
betweenthegroups(5ingroupi-gel[8.5%]and3ingroup
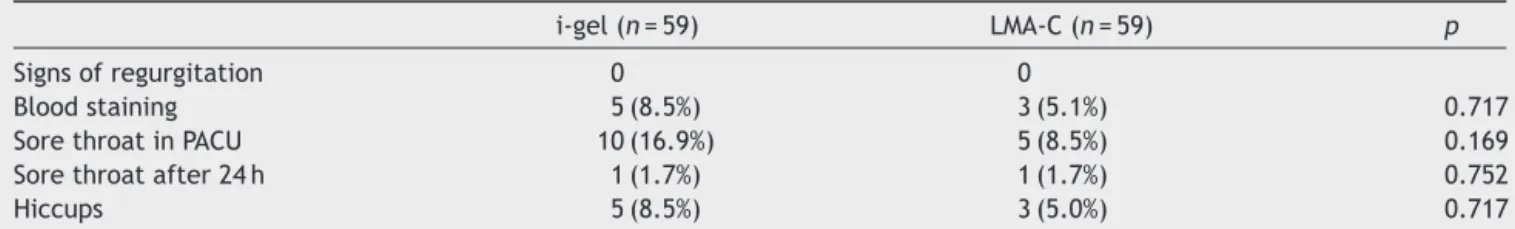
LMA-C[5.1%])(p=0.717).Postoperativeinterviewrevealed
a notable incidence of sore throat in both groups. Ten
patients of group i-gel (16.9%) and five patients of group
LMA-C(8.5%)reportedsorethroatatthepostanesthesiacare
unit(p=0.169).Also,therewasnodifferencebetweenthe
groupsregardingsorethroatat24hquestioning(p=0.752) (Table3).
Discussion
Ourresultsdemonstratethati-gelhasasimilarperformance
intermsofinsertionsuccess,peakairwaypressure,the
Table3 Sideeffectsobservedinstudygroups.
i-gel(n=59) LMA-C(n=59) p
Signsofregurgitation 0 0
Bloodstaining 5(8.5%) 3(5.1%) 0.717
SorethroatinPACU 10(16.9%) 5(8.5%) 0.169
Sorethroatafter24h 1(1.7%) 1(1.7%) 0.752
Hiccups 5(8.5%) 3(5.0%) 0.717
LMA-C,LaryngealMaskAirwayClassic.
thenumberofgastricregurgitationcomparedwiththe
LMA-C.However,i-gelhasadvantagesovertheLMA-Cintermsof
shorterinsertiontimesandimprovedfiberopticviewsofthe
glottis.
Our study showed high success rates of insertion with
both devices,which is inagreement withdataexistingin
the literature.In Gatward et al.11 study,they obtained a
86%successrateini-gelinsertionatthefirstattempt,and
theoverallinsertionsuccess ratewas100%,similartothe
LMA-CandtheprosealLMA(PLMA).Alietal.12hadasuccess
rateof77%forLMA-Cinsertionandasuccessrateof88.5%
forLMA-Supremeatthefirstattemptintheirstudy.Richez13
alsoshowedacomparablesuccessrateforplacementofthe
i-gel.Incontrasttothesestudies,inAminietal.’sstudy14
comparingi-gelandintersurgicalsolusLMA,theyfoundthat
i-gelgrouprequiredmoreinterventionsontheairwaythan
theintersurgicalsolusLMAgroup.Theythoughtitmightbe
becauseof lack of experienceof theanesthesiologists. In
ourstudy,i-gelhasasimilarperformanceintermsof
inser-tionsuccesscomparedwithLMA-C,andnointerventionwas
requiredduringmaintenanceofanesthesia.SGADswere
suc-cessfullyinsertedin89.8% ofpatientsat thefirstattempt
intheLMA-Candinthei-gelgroup.Thismaybeexplained
by thepresence ofexperienced instructorin placingboth
SGADs.
Ourresultsdemonstrate shorterinsertiontimesfor the
i-gelcomparedwiththetimesforLMA-C,probablybecause
ofthefactthatlessflexiblestemofthei-gelmakes inser-tioneasierandwithoutanyneedforcuffinflation.Insertion
success and shorter insertion times influence the
feasi-bility of SGADs, as determined by Uppal and Amini and
colleagues14,15;wefoundthattheinsertiontimewasshorter
inthei-gelgroupbutwedidnotfindanysignificantclinical differenceinthisregard.
Many investigators have demonstrated that there are
no significant differences in oropharyngeal leak pressure
between the i-gel and LMA-Supreme.16,17 Chen et al.’s18
meta-analyses revealed that there were similar
orop-haryngeal leak pressures during anesthesia between the
LMA-Supreme and the i-gel. In some studies, the LMA
Supremeisreportedtohavehigheroropharyngealleak
pres-surethantheLMA-C.12,17Althoughthei-geldoesnothavean
inflatablecuffandthusitishardertoadjusttheseal,given
Chenetal.’smeta-analysesoforopharyngealleakpressures
of i-geland LMA-Supremeand variousinvestigators’
com-parisons of oropharyngeal leak pressures of LMA Supreme
andLMA-C, itcanbededuced thati-gelmight have same
orhigheramountsoforopharyngealleakpressurethan
LMA-C.12,16---19 Further studies onthe most commonalternative
SGADs suggest thata meanpeakairway pressureof more
than20cmH2Oincreasestheriskofleakagewithresultant
insufficientventilationandincreasedriskofaspiration.20,21
In our study, the i-gel demonstrated similar peak airway
pressures(mean12cmH2O)with7mLkg−1tidalvolume,to
the LMA-C and was comparable with the LMA-C in other
studiesandlessthan20cmH2O.22
In ourstudy, we hadbetter glottic view in i-gelgroup
byfiberscopyandsimilarresultswerereportedinacohort
studyperformed by Beringeret al.23 as wellas anumber
ofadultstudies.17,18 Wethinkthatthereasonfor
fiberop-ticview of glottisnot being goodenough in LMA-C group
mightbeduetomalpositioncausedbycuffofLMA-C.The
fiberopticviewdependsonthehypopharyngealpositionof
theSGADandwhethertheepiglottisisfoldeddownduring
insertionornot.However,itwasshownthatthereisno
cor-relationbetweenfiberopticviewandSGAD’sfunction.The
fiberopticscoreconfirmsthattheSGADoccupiesafavorable
anatomicallocationtoensureunimpededventilation,with
lowerleakpressuresandlessgastricinsufflation.23
In manystudies that investigate SGADregurgitation,it
has been shown that the presence of SGAD results in a
reaction in the pharynx which causes a reflex relaxation
attheloweresophagealsphincteraswellasadecreasein
loweresophageal sphincterpressure.7,8,24 This mechanism
mightbemoreactiveduringsuperficialanesthesia.
Inade-quateanesthesialevelandinexperiencewiththeSGADuse
mayincreasetherisk ofregurgitation.Bapatetal.25
con-cludedthattheydidnotencounteranyregurgitationeven
inpatientswithhighriskintheirstudybecauseofan experi-encedSGADuser.Anotherstudywith280patientsusingi-gel
demonstratedthatthreepatientssufferedfrom
regurgita-tionandoneofthemresulted inaspiration.Thispatient’s
supraglotticdevice wasreplaced by a medicalstudent.26
Brimacombe22 has suggested two distinct learning curves
in the use of SGAD, and we believe that the high
inci-denceofregurgitationcitedintheearlierstudiesmighthave
occurred during the learning curve. We controlled depth
of anesthesia with BIS monitoring, and maintained it at
between50 and 60, withan experienced anesthesiologist
placingbothSGADs’.
The measurement of hypopharyngealpH is an another
methodtodetectgastricregurgitation,buthypopharyngeal
pH is measured at a single level and thus may not
accu-ratelyreflecttheactualincidenceofsilentregurgitation.27
Thevalidityofthemethylenebluemethodtodetect
regur-gitationisquestionable,becausedisintegrationofacapsule
in the esophagus may lead to a falsely high incidence of
regurgitation.8 Inour study,toreduce falsepositives, the
methylenebluecapsule wasingestedwith30mL waterin
patients 10min after theingestion of thedrug in case of falsepositivebluedye.
Severallimitationsexistinthisstudy.Firstly,unblinded
observerscollectedallthedata.Secondly,the
anesthesiol-ogistinsertingtheSGADshadconsiderablymoreexperience
in inserting the LMA-C and the i-gel and this may have
introduced bias in the results. Thirdly, the devices were
usedin non-obese patients andin those without
underly-inggastrointestinalsystemdisorders.Theresultscannotbe
extrapolatedtoothergroupsofpatients.
Inconclusion,ourstudydemonstratesthatbothdevices
hadgoodperformancewithlowpostoperativecomplications
andwithoutoccurrenceofregurgitation.Thei-gelprovided
ashorterinsertion timeandabetterfiberoptic viewthan
theLMA-C.
Conflicts
of
interest
Theauthorsdeclarenoconflictsofinterest.
References
1.BrainAl.Thelaryngealmask-anewconceptinairway manage-ment.BrJAnaesth.1983;55:801---5.
2.SmithI,JoshiG.Thelaryngealmaskairwayforoutpatient anes-thesia.JClinAnesth.1993;5:22---8.
3.MortensenCR,JenstrupMT,FruergardKO.Thelaryngealmask: anewalternativetothefacialmaskandtheendotrachealtube. UgeskrLaeger.1991;153:2542---4.
4.Miller DM. A proposed classification and scoring system for supraglottic sealing airways: a brief review. Anesth Analg. 2004;99:1553---9.
5.BrimacombeJR,BerryA.Theincidenceofaspirationassociated withthelaryngealmaskairway:ameta-analysisofpublished literature.JClinAnesth.1995;7:297---305.
6.KoehliN.Aspirationandthelaryngealmaskairway.Anaesthesia. 1991;46:419.
7.BarkerP,MurphyP,LongtanJA,etal.Regurgitatonofgastric contentsduringgeneralanaesthesiausinglaryngealmask air-way.BrJAnaesth.1992;69:314---5.
8.BarkerP,MurphyP,LongtanJA,etal.Regurgitatonofgastric contentsduringgeneralanaesthesiausinglaryngealmask air-way.BrJAnaesth.1991;67:660.
9.BrimacombeJ,BerryAA.Proposedfiber-opticscoringsystemto standardizetheassessmentoflaryngealmaskairwayposition. AnesthAnalg.1993;76:457.
10.Kapila A, Addy EV, VergheseC, et al. The intubating laryn-gealmaskairway:aninitialassessmentofperformance.Br J Anaesth.1997;79:710---3.
11.GatwardJJ,CookTM,SellerC,etal.Evaluationofthesize4 i-gelairwayinonehundrednon-paralyzedpatients.Anaesthesia. 2008;63:1124---30.
12.AliA,CanturkS,TurkmenA,etal. Comparisonofthe laryn-gealmaskairwaySupremeandlaryngealmaskairwayclassicin adults.EurJAnaesthesiol.2009;26:1010---4.
13.Richez B, Saltel L, Banchereau F, et al. A new single use supraglottic airway device with a noninflatable cuff and an esophagealvent:anobservational studyofthei-gel. Anesth Analg.2008;106:1137---9.
14.AminiS,KhoshfetratM.Comparisonoftheintersurgicalsolus laryngeal mask airway and the i-gel supralaryngeal device. Anaesthesia.2010;65:805---9.
15.UppalV,FletcherG,KinsellaJ.Comparisonofthei-gelwiththe cuffedtrachealtubeduringpressure-controlledventilation.Br JAnaesth.2009;102:264---8.
16.JagannathanN,SommersK,SohnLE,etal.Arandomized equiv-alence trial comparing the i-gel and laryngeal mask airway supremeinchildren.PaediatrAnaesth.2013;23:127---33.
17.Theiler LG,Kleine-Brueggeney M,Kaiser D,et al. Crossover comparison of the laryngeal mask supreme and the i-gel in simulated difficult airway scenario in anesthetized patients. Anesthesiology.2009;11:55---62.
18.ChenX,JiaoJ,CongX,etal.Acomparisonoftheperformance oftheI-gelTMvs.theLMA-STMduringanesthesia:ameta-analysis ofrandomizedcontrolledtrials.PLoSONE.2013;12:e71910.
19.Teoh WH, Lee KM, Suhitharan T, et al. Comparison of the LMAsupreme vs. the i-gel in paralysed patients undergoing gynaecologicallaparoscopicsurgerywithcontrolledventilation. Anaesthesia.2010;65:1173---9.
20.WenzelV,IdrisAH,DörgesV,etal.Therespiratorysystemduring resuscitation: a review of the history, risk of infection dur-ingassistedventilation,respiratorymechanics,andventilation strategiesforpatientswithanunprotectedairway. Resuscita-tion.2001;49:123---34.
21.BrainAI,BrimacombeJR,BerryAM,etal.Refluxduringpositive pressureventilationviathelaryngealmaskairway?BrJAnaesth. 1995;74:489---90.
22.Brimacombe J.Analyses of1500laryngeal maskusesbyone anaesthetistinadultsundergoingroutineanaesthesia. Anaes-thesia.1996;51:76---80.
23.BeringerRM,KellyF,CookTM,etal.Acohortevaluationofthe paediatrici-gelTM airway duringanaesthesiain 120children. Anaesthesia.2011;66:1121---6.
24.Rabey PG, Murphy PJ, Langton JA, et al. Effect of the laryngeal maskairway on lower oesophagealsphincter pres-sure in patients during general anaesthesia. Br J Anaesth. 1992;69:346---8.
25.BapatP,VergheseC.Laryngealmaskairwayandtheincidenceof regurtationduringgynecological laparascopies.AnesthAnalg. 1997;85:139---43.
26.GibbisonB,CookTM,SellerC.Caseseries:protectionfrom aspi-rationandfailureofprotectionfromaspirationwiththei-gel airway.BrJAnaesth.2008;100:415---7.