Sao Paulo Med J. 2010; 128(5):268-71
268
Original article
Evolution of blood magnesium and phosphorus ion levels
following thyroidectomy and correlation with total calcium values
Evolução dos níveis dos íons fósforo e magnésio séricos e sua correlação com valores de cálcio
total após tireoidectomia
Alexandre de Andrade Sousa
I, José Maria Porcaro Salles
II, João Marcos Arantes Soares
III, Gustavo Meyer de Moraes
I,
Jomar Rezende Carvalho
I, Paulo Roberto Savassi-Rocha
IVInstituto Alfa de Gastroenterologia (IAG), Hospital das Clínicas, Universidade Federal de Minas Gerais (UFMG), Belo Horizonte, Minas Gerais, Brazil
IMD. Surgeon in the Head and Neck Group and member of the Instituto Alfa de Gastroenterologia (IAG), Hospital das Clínicas, Universidade Federal de Minas Gerais (UFMG), Belo Horizonte, Minas Gerais, Brazil.
IIMD. Professor of Head and Neck Surgery and Head of the Head and Neck Group of the Instituto Alfa de Gastroenterologia (IAG), Hospital das Clínicas, Universidade Federal de Minas Gerais (UFMG), Belo Horizonte, Minas Gerais, Brazil. IIIMD, PhD. Surgeon in the Head and Neck Group and member of the Instituto Alfa de Gastroenterologia (IAG), Hospital das Clínicas, Universidade Federal de Minas Gerais (UFMG), Belo Horizonte, Minas Gerais, Brazil. IVMD, PhD. Professor of Surgery and Head of the Instituto Alfa de Gastroenterologia (IAG), Hospital das Clínicas, Universidade Federal de Minas Gerais (UFMG), Belo Horizonte, Minas Gerais, Brazil.
ABSTRACT
CONTEXT AND OBJECTIVE: Magnesium ion concentration is directly related and phosphorus ion concentration is inversely related to calcemia. The aim of this study was to evaluate the evolution of magnesium and phosphorus ion levels in patients undergoing thyroidectomy and correlate these
with changes to calcium concentration.
DESIGN AND SETTING: Prospective study at the Alpha Institute of Gastroenterology, Hospital das Clínicas, Universidade Federal de Minas Gerais.
METHODS: The study included 333 patients, of both genders and mean age 45 ± 15 years, who underwent thyroidectomy between 2000 and 2005. Total calcium, phosphorus and magnesium were measured in the blood preoperatively and 24 and 48 hours postoperatively. Ionic changes were
evaluated according to the presence or absence of postoperative hypocalcemia.
RESULTS: There were statistically signiicant drops in blood phosphorus levels 24 and 48 hours after thyroidectomy, compared with preoperative values, in the patients without hypocalcemia. In the patients who developed hypocalcemia, there was a signiicant drop in plasma phosphorus on the irst postoperative day and an increase (also statistically signiicant) on the second day, in relation to preoperative phosphorus levels. A signiicant
drop in postoperative magnesium was also observed on the irst and second days after thyroidectomy in the patients with hypocalcemia, in relation to preoperative levels. In the patients without hypocalcemia, the drop in magnesium was signiicant on the irst day, but there was no difference on
the second day.
CONCLUSION: Despite the postoperative changes, neither magnesium nor phosphorus ion levels had any role in post-thyroidectomy calcemia.
RESUMO
CONTEXTO E OBJETIVO: A concentração do íon magnésio está diretamente e a do íon fósforo inversamente relacionada à calcemia. O objetivo foi avaliar a evolução das concentrações dos íons magnésio e fósforo nos pacientes submetidos a tireoidectomia, e relacioná-los com as alterações da concentração do cálcio.
TIPO DE ESTUDO E LOCAL: Estudo prospectivo realizado no Instituto Alfa de Gastroenterologia, Hospital das Clínicas, Universidade Federal de Minas Gerais.
MÉTODOS: O estudo incluiu 333 pacientes de ambos os sexos, com média de idade de 45 ± 15 anos, submetidos a tireoidectomia no período de 2000 a 2005. Cálcio total, fósforo e magnésio foram dosados no pré-operatório e com 24 e 48 horas de pós-operatório. As alterações dos íons
foram avaliadas de acordo com a presença ou ausência de hipocalcemia pós-operatória.
RESULTADOS: Houve queda estatisticamente signiicativa dos níveis sanguíneos de fósforo 24 horas e 48 horas após a tireoidectomia em relação ao pré-operatório nos pacientes que não tiveram hipocalcemia. Quanto aos pacientes que evoluíram com hipocalcemia, houve queda signiicativa do fósforo plasmático no primeiro dia de pós-operatório e elevação, também estatisticamente signiicativa, no segundo dia em relação ao fósforo
pré-operatório. Foi também observada queda signiicativa do magnésio pós-operatório em relação ao pré-operatório no primeiro e no segundo dia após a tireoidectomia nos pacientes com hipocalcemia. Naqueles sem hipocalcemia, a queda do magnésio foi signiicativa no primeiro dia, mas
não houve diferença no segundo dia.
CONCLUSÃO: Embora alterados no operatório, as concentrações dos íons magnésio e fósforo não apresentaram papel na calcemia pós-tireoidectomia.
KEY WORDS: Magnesium. Phosphorus.
Calcium. Thyroidectomy.
Complications.
PALAVRAS CHAVES: Magnésio. Fósforo.
Cálcio. Tireoidectomia.
Evolution of blood magnesium and phosphorus ion levels following thyroidectomy and correlation with total calcium values
Sao Paulo Med J. 2010; 128(5):268-71
269
INTRODUCTION
hyroidectomy is a clean surgical procedure with a small exposed area, minimal blood and luid loss and no involvement of the diges-tive tract. Dietary intake can be resumed a few hours after the opera-tion, in most cases. he endocrine and metabolic response is slight and short-lived. Consequently, both luid volumes and ion concentrations promptly return to their baseline preoperative states.1-3
Although the incidence of postoperative complications is accept-able, they may be extremely uncomfortable and incapacitating. he most common metabolic complications are disorders of calcium ion concentrations.4
Homeostasis of magnesium ions is directly related to calcium levels. An abrupt fall in calcium concentration leads to reduction of the pro-duction and release of parathormone (PTH) and exacerbates the sec-ondary clinical manifestations, because of hypocalcemia. Phosphorus concentration is inversely related to calcium and is regulated by calcium, PTH and vitamin D.2
OBJECTIVE
he aim of this study was to evaluate the changes in magnesium and phosphorus ion concentrations in patients undergoing thyroidectomy, and to correlate these changes with changes to total calcium.
METHODS
Patients were evaluated prospectively and were included in the study after signing a free and informed consent statement that was in accordance with the World Health Organization guidelines for research on human beings.5
All the patients who underwent thyroidectomy performed by the Head and Neck Surgery Group in the Alpha Institute of Gastroenterolo-gy, Hospital das Clínicas, Universidade Federal de Minas Gerais (UFMG), between September 2000 and December 2005, were eligible for inclusion in the study. All the patients included in this study had a formal surgical indication for thyroidectomy, independently of the extent of the surgery.
Patients who chose not to participate in the study, those with an incomplete preoperative assessment, those who did not return for their follow-up appointments and those who presented preoperative hypo or hyper magnesemia/phosphatemia or preoperative hyperparathyroidism (as shown through calcium ion and PTH measurements) were excluded from this study.
In addition to the routine examinations that are performed prior to any thyroidectomy, the preoperative assessment for these patients in-cluded measurement of total calcium, phosphorus and magnesium ion levels in the blood. he postoperative assessment included measurement of total calcium, phosphorus and magnesium ion levels in the blood, 24 hours and 48 hours after the operation. All the blood samples were taken at 6:00 a.m.
Patients who presented postoperative clinical manifestations of hy-pocalcemia, as conirmed through laboratory tests, received oral
calci-um carbonate. he initial dose was 2.0 grams every six hours, and this was adjusted in accordance with the clinical and laboratory follow-up. In treatment-resistant cases (high doses of oral calcium carbonate with no clinical improvement), oral vitamin D was also administered. Se-verely symptomatic patients received intravenous calcium gluconate, as well as oral calcium carbonate, until the clinical manifestations had dis-appeared.
Patients were evaluated according to the presence or absence of postoperative hypocalcemia. his variable was correlated with preop-erative phosphorus (P) and magnesium (Mg) measurements and serum concentrations of postoperative magnesium and phosphorus ions, in samples taken on the irst and second day after thyroidectomy;
Concentrations that were below the reference values for the ions evaluated were considered to be cases of hypocalcemia, hypophos-phatemia and hypomagnesemia. he laboratory tests were performed at the Clinical Pathology Laboratory of Hospital das Clínicas, UFMG, and included the following:
• Total calcium – reference value: 8.4 mg/dl to 10.2 mg/dl. • Phosphorus – reference value: 2.5 mg/dl to 4.5 mg/dl. • Magnesium – reference value: 1.6 mg/dl to 2.3 mg/dl.
he data were analyzed using the Statistical Package for the Social Sci-ences (SPSS), version 13.0. he signiicance level was taken to be 5%.
RESULTS
he study included 359 patients, of both genders and all age groups, who underwent thyroidectomy performed by the Head and Neck Sur-gery Group in the Alpha Institute of Gastroenterology of the University Hospital of UFMG, between September 2000 and December 2005.
he complete outpatient follow-up in accordance with the pro-posed method was performed in the cases of 333 patients. he other 26 patients were excluded.
Among these 333 patients, 29 (8.7%) were male and 304 were fe-male (91.3%). heir age ranged from 8 to 88 years, with a mean of 45 ± 15 years and a median of 46 years.
he mean values for total calcium, phosphorus and magnesium be-fore the operation and on the irst and second postoperative days are shown in Table 1.
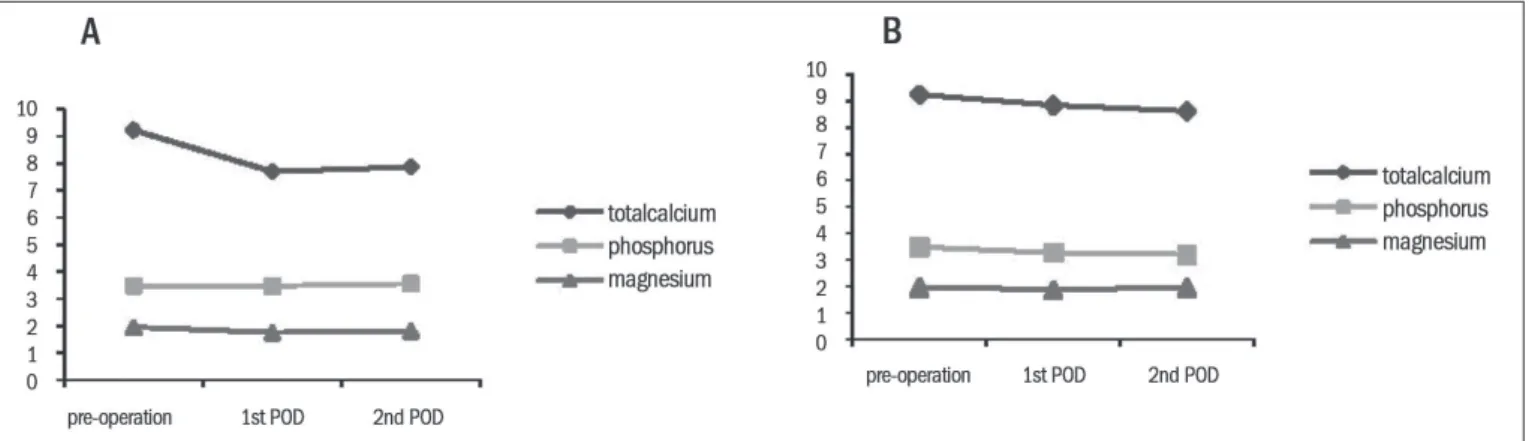
Among the hypocalcemic patients, the mean values for total calcium, phosphorus and magnesium on the irst postoperative day were, respec-tively, 7.69 ± 0.74 mg/dl, 3.47 ± 0.77 mg/dl and 1.75 ± 0.46 mg/dl. On the second postoperative day, the values were 7.87 ± 0.85 mg/dl, 3.56 ±
0.93 mg/dl and 1.81 ± 0.46 mg/dl (Figure 1A).
Among the patients without hypocalcemia, the mean values on the irst postoperative day were, respectively, 8.83 ± 0.52 mg/dl, 3.27 ±
0.68 mg/dl and 1.88 ± 0.39 mg/dl. On the second postoperative day, the values were 8.62 ± 0.55 mg/dl, 3.21 ± 0.65 mg/dl and 1.95 ± 0.34 mg/dl
(Figure 1B).
Sao Paulo Med J. 2010; 128(5):268-71
Sousa AA, Salles JMP, Soares JMA, Moraes GM, Carvalho JR, Savassi-Rocha PR
270
postoperative hypocalcemia (n = 136), the drop in the levels was signii-cant on both days following surgery (P = 0.000) (Table 2).
here was a statistically signiicant drop in blood phosphorus levels on these two days following thyroidectomy, compared with preoperative levels, among the patients without hypocalcemia (P = 0.000). Among the patients who developed hypocalcemia, there was a signiicant drop in plasma phosphorus on the irst postoperative day (P = 0.006) and an increase (which was also signiicant) on the second day (P = 0.012), in relation to preoperative phosphorus levels (Table 3).
A signiicant drop in postoperative magnesium levels was also ob-served on both the irst and second postoperative days following thyroi-dectomy, among the patients who developed hypocalcemia (P = 0.000). Among the patients without hypocalcemia, the drop in magnesium lev-els was signiicant on the irst day (P = 0.017), but no signiicant difer-ence was noted on the second day (P = 0.876) (Table 4).
DISCUSSION
Phosphorus and magnesium ions have a direct relationship with calcium metabolism. Plasma calcium concentrations frequently present disorders following thyroidectomy.
he adult human body contains approximately 600 g of phospho-rus (1.0% of total body weight), of which 85.0% is in the skeleton, while the remaining 15.0% can be found in extracellular luids, in the form of inorganic phosphate, and in soft tissue, in the form of phos-phate esters.1
Intestinal and renal absorption and excretion of phosphorus are re-lated to PTH concentration. PTH increases vitamin D concentration, which is responsible for stimulating active absorption of this phospho-rus in the intestines. In the kidneys, PTH acts directly on proximal tu-bules, thereby reducing phosphorus reabsorption and increasing phos-phaturia.6
he drop in serum concentration of phosphorus in response to PTH stimulation occurs more promptly than does the increase in cal-cium. herefore, monitoring of phosphorus in hypocalcemic patients who require calcium supplementation may provide an early indication of regulation of parathyroid gland function.7
Figure 1. Mean total calcium, phosphorus and magnesium levels before the operation and on the irst and second postoperative days (POD), among patients with hypocalcemia (A) and without hypocalcemia (B) after the surgery.
Table 1. Mean total calcium, phosphorus and magnesium levels before the operation and on the irst and second postoperative days (POD)
Total calcium (mg/dl) Phosphorus (mg/dl) Magnesium (mg/dl)
Before operation 9.23 ± 0.54 3.48 ± 0.58 1.96 ± 0.26 First POD 8.36 ± 0.40 3.36 ± 0.72 1.83 ± 0.42 Second POD 8.31 ± 0.78 3.36 ± 0.79 1.89 ± 0.40
Reference values: total calcium, 8.4 to 10.2 mg/dl; phosphorus, 2.5 to 4.5 mg/dl; magnesium, 1.6 mg/dl to 2.3 mg/dl.
Table 2. Comparison of mean total serum calcium levels (mg/dl) before the operation (pre) and on the irst and second postoperative days (POD), among 333 patients, with or without hypocalcemia
Group Variables
Difference between means (mg/dl)
P
Without hypocalcemia TotCa pre vs. TotCa 1
st POD 0.41 0.265
TotCa pre vs. TotCa 2nd POD 0.62 0.000
With hypocalcemia TotCa pre vs. TotCa 1
st POD 1.51 0.000
TotCa pre vs. TotCa 2nd POD 1.34 0.000
TotCa = total calcium; vs. = versus. Statistical method = Student’s t test.
Table 3. Comparison between mean serum phosphorus levels (mg/dl) before the operation (pre) and on the irst and second postoperative days (POD), among 333 patients, with or without hypocalcemia
Group Variables
Difference between means (mg/dl)
P
Without hypocalcemia P pre vs. P 1
st POD 0.18 0.000
P pre vs. P 2nd POD 0.26 0.000
With hypocalcemia P pre vs. P 1
st POD 0.05 0.006
P pre vs. P 2nd POD -0.04 0.012
P = phosphorus; vs. = versus. Statistical method = Student’s t test.
Table 4. Comparison between mean serum magnesium levels (mg/dl) before the operation (pre) and on the irst and second postoperative days (POD), among 333 patients, with or without hypocalcemia
Group Variables
Difference between means (mg/dl)
P
Without hypocalcemia Mg pre vs. Mg 1
st POD 0.43 0.017
Mg pre vs. Mg 2nd POD 0.01 0.876
With hypocalcemia Mg pre vs. Mg 1
st POD 0.22 0.000
Mg pre vs. Mg 2nd POD 0.15 0.000
Evolution of blood magnesium and phosphorus ion levels following thyroidectomy and correlation with total calcium values
Sao Paulo Med J. 2010; 128(5):268-71
271
Magnesium deiciency reduces the PTH efect in the kidneys and bones and increases its degradation in the liver and kidneys. herefore, hypocalcemic patients with magnesium deiciency will present relative hypoparathyroidism.8
Magnesium is also involved in the metabolism and activity of vita-min D. Patients with hypocalcemia and hypomagnesemia are resistant to large doses of vitamin D, because of reductions in PTH secretion and renal resistance to this hormone. Furthermore, oral administration of vitamin D does not increase blood calcium levels.9
Hypomagnesemia and hypocalcemia occurring together in-crease the symptoms in patients. Plasma calcium correction with-out concurrent normalization of magnesium may prolong the clinical manifestations.7,10
Temporary hypoparathyroidism leads to a reduction in renal reab-sorption of magnesium, and expansion of the extracellular volume in-creases magnesium excretion.10 According to Wilson et al.,10 10.0% of
patients who undergo total thyroidectomy develop hypomagnesemia and hypocalcemia.
Our results showed that the mean total calcium level in patients who underwent thyroidectomy decreased. his conirms the results published by other authors, thus underscoring the inluence of hemodi-lution on total calcium concentration during and following surgery. Measurements on ion concentrations on the irst two days following the operation showed recuperation, albeit partial at times, of luid vol-ume and plasma ion concentrations. Aside from hemodilution, signii-cant and prolonged reduction of calcemia may be caused by temporary disorders of the parathyroid glands, and consequently, by hypoparathy-roidism. Although routine measurement of PTH following thyroidecto-my is not available at our service, hypoparathyroidism can be suspected when there is a drop in calcium levels, especially when patients require oral supplementation.
here was a signiicant drop in plasma phosphorus levels in patients without hypocalcemia, on the irst two days following surgery in rela-tion to preoperative levels, which suggests that hemodilurela-tion may have an important role. Among the patients with hypocalcemia, a signii-cant drop in phosphorus levels was observed on the irst postoperative day. However, possibly because of lack of PTH stimulation caused by parathyroid gland disorders, there was a reduction in renal excretion of phosphorus and a progressive increase in blood levels of this ion, in con-trast to the reduction in calcium. herefore, plasma phosphorus levels rose to signiicantly higher levels on the second postoperative day.
he patients who presented hypocalcemia presented signiicantly lower magnesium levels on the irst two days following the operation, in comparison with preoperative levels. Patients without hypocalcemia had a signiicant drop in magnesium levels on the irst postoperative day, with a return to baseline levels on the second postoperative day, which might indicate volume reestablishment. However, both in the pa-tients with and in those without hypocalcemia, the serum magnesium levels remained within the reference values, thus making it diicult to evaluate their role in postoperative hypocalcemia. Even in patients with symptoms of hypocalcemia and signiicant reductions in calcium levels, the blood magnesium levels remained within their reference values and
probably did not inluence the reduction in calcium levels and hypocal-cemia symptoms.
CONCLUSIONS
In conclusion, despite the postoperative changes, neither the magne-sium nor the phosphorus levels had any role in post-thyroidectomy calce-mia. he magnesium concentration varied according to total calcium lev-els, while the phosphorus concentration was inversely proportional.
REFERENCES
1. Arioli EL. Hipocalcemia [Hypocalcemia]. Arq Bras Endocrinol Metab. 1999;43(6):467-71. 2. Falk SA, Birken EA, Baran DT. Temporary postthyroidectomy hypocalcemia. Arch Otolaryngol
Head Neck Surg. 1988;114(2):168-74.
3. Lemaire FX, Debruyne F, Delaere P, Vander Poorten V. Parathyroid function in the early posto-perative period after thyroidectomy. Acta Otorhinolaryngol Belg. 2001;55(2):187-98. 4. Salles JMP, Soares JMA, Sousa AA, Salles PV. Prevenção e tratamento das complicações da
tireoidectomia. In: Carvalho MB, editor. Tratado de tireóide e paratireóide. Rio de Janeiro: Rubio; 2007. p. 651-62.
5. International Ethical Guidelines for Biomedical Research Involving Human Subjects. Gene-va: Council for International Organizations of Medical Sciences (CIOMS) in collaboration with the World Health Organization (WHO); 2002. Available from: http://www.fhi.org/trai-ning/fr/retc/pdf_iles/cioms.pdf. Accessed in 2010 (Sep 16).
6. Schaefer SD, Fee WE Jr. Thyroid surgery: surgical and metabolic causes of hypocalcemia. Arch Otolaryngol. 1978;104(5):263-6.
7. Fahmy FF, Gillett D, Lolen Y, Shotton JC. Management of serum calcium levels in post-thyroi-dectomy patients. Clin Otolaryngol Allied Sci. 2004;29(6):735-9.
8. Freitag JJ, Martin KJ, Conrades MB, et al. Evidence for skeletal resistance to parathyroid hormone in magnesium deiciency. Studies in isolated perfused bone. J Clin Invest. 1979;64(5):1238-44.
9. Mori S, Harada S, Okazaki R, et al. Hypomagnesemia with increased metabolism of pa-rathyroid hormone and reduced responsiveness to calcitropic hormones. Intern Med. 1992;31(6):820-4.
10. Wilson RB, Erskine C, Crowe PJ. Hypomagnesemia and hypocalcemia after thyroidectomy: prospective study. World J Surg. 2000;24(6):722-6.
Sources of funding: Not declared
Conlict of interest: Not declared
Date of irst submission: June 26, 2009
Last received: September 15, 2010
Accepted: September 16, 2010
Address for correspondence: Alexandre de Andrade Sousa Av. do Contorno, 5.351 — sala 1206 Cruzeiro — Belo Horizonte (MG) CEP 30110-035