RevBrasAnestesiol.2016;66(2):200---203
REVISTA
BRASILEIRA
DE
ANESTESIOLOGIA
OfficialPublicationoftheBrazilianSocietyofAnesthesiologywww.sba.com.br
CLINICAL
INFORMATION
Neurogenic
pulmonary
edema
due
to
ventriculo-atrial
shunt
dysfunction:
a
case
report
Ana
Sofia
Cruz
a,∗,
Sónia
Menezes
b,
Maria
Silva
aaAnesthesiologyDepartment,CentroHospitalSãoJoão,Porto,Portugal
bAnesthesiologyDepartment,HospitalDistritaldeSantarém,Santarém,Portugal
Received2September2013;accepted31October2013 Availableonline12December2013
KEYWORDS
Neurogenic pulmonaryedema; Hydrocephalus; Neuroanesthesia
Abstract
Backgroundandobjectives: Pulmonaryedemaiscausedbytheaccumulationoffluidwithinthe airspacesandtheinterstitiumofthelung.Neurogenicpulmonaryedemaisaclinicalsyndrome characterizedbytheacuteonsetofpulmonaryedemafollowingasignificantcentralnervous systeminsult.Itmaybealess-recognizedconsequenceofraisedintracranialpressuredueto obstructivehydrocephalusbyblockedventricularshunts.Itusuallyappearswithinminutesto hoursaftertheinjuryandhasahighmortalityrateifnotrecognizedandtreatedappropriately.
Casereport: Wereportapatientwithacuteobstructivehydrocephalusduetoventriculo-atrial shuntdysfunction,proposedtourgentsurgeryforplacementofexternalventriculardrainage, whopresentedwithneurogenicpulmonaryedemapreoperatively. Shewasanesthetizedand supportivetreatmentwasinstituted.Attheendoftheprocedurethepatientshowedno clin-icalsignsofrespiratorydistress,aspromptreductioninintracranialpressurefacilitatedthe regressionofthepulmonaryedema.
Conclusions:This report addresses the importance ofrecognition ofneurogenic pulmonary edemaasapossibleperioperativecomplicationresultingfromanincreaseinintracranial pres-sure.Ifnotrecognizedandtreatedappropriately,neurogenicpulmonaryedemacanleadto acutecardiopulmonaryfailurewithglobalhypoperfusionandhypoxia.Therefore,awarenessof andknowledgeabouttheoccurrence,clinicalpresentationandtreatmentareessential. ©2013SociedadeBrasileiradeAnestesiologia.PublishedbyElsevier EditoraLtda.Allrights reserved.
PALAVRAS-CHAVE
Edemapulmonar neurogênico; Hidrocefalia; Neuroanestesia
Edemapulmonarneurogênicodevidoàdisfunc¸ãodaderivac¸ãoventrículo-atrial: relatodecaso
Resumo
Justificativaeobjetivos: Oedemapulmonarécausadopeloacúmulodelíquidonosalvéolos enointerstíciopulmonar.Edemapulmonarneurogênicoéumasíndromeclínicacaracterizada
∗Correspondingauthor.
E-mail:fyzzita@gmail.com(A.S.Cruz).
Neurogenicpulmonaryedemaduetoventriculo-atrialshuntdysfunction 201
poredemapulmonardeinícioagudoapósumacometimentosúbitodosistemanervosocentral. Podeserumaconsequênciamenosreconhecidadepressãointracranianaaumentadaporcausa dahidrocefaliaobstrutiva porderivac¸õesventricularesbloqueadas.Geralmenteaparece em minutosouhorasapósoinsultoetemumaaltataxademortalidade,casonãosejaidentificado etratadoadequadamente.
Relatodecaso: Relatamosocasodepacientecomhidrocefaliaobstrutivaagudaporcausada disfunc¸ãodaderivac¸ãoventrículo-atrial,programadoparacirurgiaemcaráterdeurgênciapara acolocac¸ãodederivac¸ãoventricularexterna,queapresentouedemapulmonarneurogênicono pré-operatório.Apaciente foianestesiadaeotratamentodemanutenc¸ãoinstituído. Nofim doprocedimento,apacientenãoapresentouquaisquersinaisdedistúrbiorespiratório,poisa reduc¸ãorápidadapressãointracranianafacilitouaregressãodoedemapulmonar.
Conclusões: Esterelatoaborda aimportânciadaidentificac¸ão deum edemapulmonar neu-rogênicocomoumapossívelcomplicac¸ãonoperíodoperioperatórioresultantedeumaumento dapressãointracraniana.Quandonão identificado etratadoadequadamente, oedema pul-monar neurogênicopode levarà insuficiência cardiorrespiratória aguda, com hipoperfusão globalehipóxia.Portanto,aconscientizac¸ãoeoconhecimentodesuaocorrência,apresentac¸ão clínicaeseutratamentosãoessenciais.
©2013SociedadeBrasileira deAnestesiologia.PublicadoporElsevierEditoraLtda.Todosos direitosreservados.
Introduction
Pulmonary edema is caused by the accumulation of fluid within the air spaces and the interstitium of the lung. It may form due to intrinsic lung pathology or systemic dysfunction,1leadingtoimpaired gasexchangeand
respi-ratoryfailure.
Neurogenicpulmonaryedema(NPE)isaclinicalsyndrome characterizedbytheacuteonsetofpulmonaryedema fol-lowing a significant central nervous system (CNS) insult.2
Itusuallyappearswithinminutestohoursaftertheinjury andhasahighmortalityrateifnotrecognizedandtreated appropriately.3Ahighindexofsuspicionisrequiredforits
diagnosis,which isbasedontheoccurrenceoftheedema afteraneurologicinsultandtheexclusionofotherpossible causes.4
The most common causes of NPE are subarachnoid hemorrhages, followedbyhead trauma,seizures, embolic stroke, neurologicendovascular proceduresand increased intracranialpressure(ICP)ofanyetiology.1,5NPEmaybea
less-recognizedconsequence ofraisedICP dueto obstruc-tive hydrocephalusby blocked ventricularshunts.6 In this
setting,amechanicalshuntmalfunctionshouldbetreated urgentlytopreventtheneurologicsequelsofICP,7 butthe
presence of preoperative NPE presents a dilemma to the neuroanesthesistduetothedivergentgoalsofmanagement ofaraisedintracranialpressureandpulmonaryedema.6
Wereportapatientwithacuteobstructivehydrocephalus due toventriculo-atrial shunt dysfunction who presented withNPE.
Case
report
A 15-year-old female patient, with history of obe-sity, asthma, epilepsy, myelomeningocele sequelae and ventriculo-atrialshunt,wasproposedtourgentsurgeryfor placementof external ventriculardrainage (EVD)totreat obstructivehydrocephalusduetoshuntobstruction.
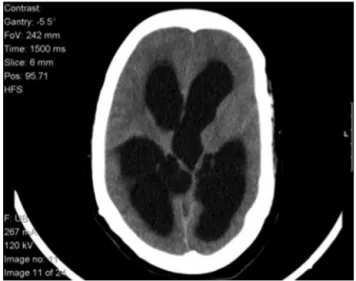
On admission, in the emergency department, she pre-sented with vomit, headache and somnolence (Glasgow ComaScale(GCS)of14)andherCTscanshoweda triven-tricularhydrocephalus(Fig.1).
Shewasadmittedtotheemergencyoperatingroom(EOR) prostrate,showingprogressivesignsofrespiratorydistress (whilewithoxygensupportbyfacemaskwithaFiO2of80%)
and with bilateral thick scattered crackles on pulmonary auscultation.Shehadaheartrateof100beatsperminute, arterial pressure of 140/85mmHg, respiratory rate of 25 ventilations per minute and SatO2 of 96%. Her chest
X-rayshowedbilateralhazinesssuggestingpulmonaryedema (Fig.2).Thearterialbloodgasparameters(ABG)werethe following:pH7.44;pCO229mmHg;pO286mmHg;Oxygen
Saturation97%; Lactates: 2.68mmolL−1.All other clinical
andbiochemicalinvestigationswerenormal.
Duringpre-oxygenation,andwiththesupineposition,the presenceofpinkfoamysecretionswasnoticed.
202 A.S.Cruzetal.
Figure2 AdmissionX-rayshowingbilateralhaziness.
As there was no other cause for the respiratory dys-functionorprevious respiratoryillness,adiagnosis ofNPE wasconsidered.Furosemidewasimmediatelyadministered and repeated later (in a total of 160mg), and a rapid sequenceinductionofanesthesiawasperformedwith propo-fol 2mg/kg and succinilcoline 1mg/kg. The patient was intubated and mechanically ventilated. An arterial line for invasive arterial pressure monitoring and blood sam-plecollectionwasputinplace.SalbutamolandIpratropium bromidewereadministeredthroughthetrachealtube. Anes-thesia was maintainedwith a mixture of air and oxygen, adjustingthe FiO2 tomaintain an arterial oxygen
satura-tion>90%,and 2.2%of sevofluranealong withrocuronium (0.6mg/kg) and fentanyl (0.002mg/kg). Low physiologic PEEP was applied. Duringsurgery, and after the cerebral spinalfluid(CSF)drainage,itwaspossibletoprogressively reduceFiO2to40%.
Thepatientremainedhemodynamicallystableduringthe entireprocedure.Intheendofthesurgery,theABGshowed: pH7.44;pCO229mmHg;pO286mmHg;OxygenSaturation
97%;Lactates2.6mmolL−1.Attheendoftheprocedurethe
neuromuscularblockadewasreversed,sevofluranewas sus-pended,andthe patientwasawake,responding toverbal command,breathingspontaneouslyandwithnoevidenceof respiratoryfailure.Thepatientwasdeemedstablefor extu-bation,andwastransportedtothePostAnesthesiaCareUnit (PACU)ona100%non-rebreathermask.
InthepostoperativeperiodthepatienthadtwonewNPE episodesduetoEVDobstruction.Thelastoneneeded tra-chealintubationtomanagehypoxia.Onthetenthdayafter admissionshe wassuccessfully submittedtoher ventricle shunt revision and extubated a few hours after surgery. Shewasdischargedonthe14thdayafter admission,with SpO2100%inair,noclinicalsignsofrespiratorydistressand
regressionof the hydrocephalus, visible in the controlCT scan.
Discussion
The exact cascade leading to the development of NPE remains unclear. There are thought to be two interac-tingprocesses:acentrallymediatedexcessivesympathetic
discharge, leading to loss of vasomotor homeostasis and intense pulmonary vasoconstriction; and an inflammatory mediator-relatedincreaseinvascularpermeability.1
The CNS discharge increases sympathetic nervous sys-temtoneandcirculatingcatecholaminerelease.Thisresults in a dramatic increase in pulmonary and systemic vascu-lar resistance, cardiac contractility and tachycardia. The increasedpulmonaryvascularpressurealterstheStarling’s forcesandshiftsthebalancetowardextravasationoffluid intothelunginterstitium.1Thereisconcomitantmechanical
stress injury to the pulmonary capillary basement mem-brane whichoccursatpressures aslowas24mmHg.8This
exacerbates the flow of fluid out of the capillary as the endotheliumisprogressivelydamaged.Fluidisfollowedby plasma proteins, red blood cells and inflammatory cells.1
The acute onset of cerebral hypertension and chemical irritation may be important underlying factors. Also, the velocityofincreaseinintracranialhypertensionaloneseems toberesponsibleforNPE.9Thisfactmayexplainthe
appear-anceofNPE afterhydrocephalusthatwasobservedinthis case.
The second proposed component in the development of NPE is increased vascular permeability mediated by inflammatory cytokines.The injury tothebrain results in theexpression andrelease ofpro-inflammatorymolecules within the brain. These move tothe systemic circulation bydisruptionoftheblood---brainbarrierandinitiate physio-logical changes in lung endothelial cells which drives the recruitment and extravasation of inflammatory cells and permits the translocationof fluid. The lung increases the expression and release of cytokines in response to the mechanical insult caused by increased pulmonary capil-lary pressure which is exacerbated by the barotrauma of mechanicalventilation.1
NPEshows abroad clinical spectrum,ranging fromthe asymptomaticpatienttotherapiddevelopmentof respira-tory failure. It typically presentswithin minutes tohours fromasevereCNSinsult.TheclinicalsymptomsforNPEare nonspecific and often includedyspnea, tachypnea, tachy-cardia,cyanosis,pinkfrothysputum,cracklesandraleson clinical examination. The chest radiograph usually shows bilateralinfiltrates,increasedvascularshadowingand nor-malcardiacindex.1,3,10
Inmanycases,NPEisaretrospective diagnosis,largely based upon the occurrence of pulmonary edema in the appropriatesettingandin theabsenceof anotherobvious cause.9
Themaindifferentialdiagnosesincludeaspiration pneu-monia,communityacquired pneumonia,negativepressure edema,leftventricularfailureandpulmonarycontusions.1
Neurogenicpulmonaryedemaduetoventriculo-atrialshuntdysfunction 203
Duetotheconcomitantdevelopmentofanacute hydro-cephalusandICP,adirectandcausalrelationbetweenthese twoconditionswashypothesized.Thereappearanceofthe respiratorydysfunctionwiththefurtherobstructionofthe EDV furthercorroboratedthiscausalrelation,settling the diagnosisofNPE.AspirationpneumoniadiffersfromNPEby thepresenceofclinicalclues(vomiting,gastriccontentsin theoropharynx,witnessedaspiration)andthedistribution of alveolar diseasein dependent portions of thelungs. In contrast,NPEischaracterizedbyfrothy,oftenblood-tinged sputumandmorecentrallydistributed alveolardiseaseon chestX-ray.
The initial stepinmanagementof NPE isidentification and definitive treatment of the precipitating cause. The strategy for treatment is the rapid control of the trigg-ering central neurologic insult (and prompt reduction in intracranial pressure), while supporting organfunction.1,3
Theearlysurgicaltreatmentoftheprimaryinjuryisstrongly recommended becauseit facilitates the regression of the pulmonaryedema.11
Themainconcernsinhandlinganesthesiainthese situa-tionsarepreventionofhypoxiaandmaintenanceofcerebral perfusion pressure in a patientwith concomitant ICP and impairedgasexchangeatthealveolar---capillarymembrane. Therisksofdecreasedcerebralperfusionmustbeweighed againstthebenefitsofdecreasedsystolicbloodpressureand pulmonaryedema.5
The patient’sneurologicalstatusshouldbetheprimary determinantofwhethertrachealintubationis required.If intubationandmechanicalventilationis needed,itshould beperformedusingatechniquewhichwillavoidincreaseof eitherICPor systemicarterialpressureyetmaintain cere-bralperfusion.1
Ventilation with supplemental oxygen should prevent hypoxemiaandavoidiatrogeniclunginjury.Initialtidal vol-umesshouldbe6---7mL/kgutilizingPEEPtoaidclearanceof theedemaandmaintainalveolarrecruitment.1
Mechanical ventilation with PEEP should be used with caution because it reduces cardiac output and impairs venous return, increasing ICP.12 PEEP values lower than
15cm H2O have been shown not to impede the cerebral
perfusionpressure.13
AnypatientwithraisedICPshouldbeventilated accord-ingtoneuroprotectiveparameterswhichmaybeinconflict with optimal ventilation for NPE. Permissive hypercapnia or ventilation inproneposition shouldnotbe usedin the presenceofraisedICPunlessICPmonitoringisinplace.1A
reductioninICPmaybesuccessfullyachievedby hyperven-tilation,osmoticandloopdiuretics,raised headboardand anticonvulsivanttherapy.3
Patientsshouldbeassessedfor volumestatusandfluid responsiveness,andintravenousfluidsshouldbeused judi-ciously.
Dobutamine, which may increase cardiac output, decrease pulmonary artery balloon pressure and promote diuresis, is a first line drug in NPE treatment. Additional agents that have been advocated in the treatment of
NPE include fosfodiesterase inhibitors, beta1-antagonists alone or in combination with a vasodilator, and alfa-antagonists.1,14
The pureformof NPE mayresolvewithin48---72h with adequate treatment.1,3,5 The patients prognosis generally
dependsontheneurologiccondition.5Overallmortalityin
NPEisestimatedin7---10%range.15
This reportaddresses theimportance ofrecognition of NPEasapossibleperioperativecomplicationresultingfrom anincreasein intracranialpressure.Ifnotrecognizedand treated appropriately, NPE can lead to acute cardiopul-monaryfailurewithglobalhypoperfusionandhypoxia.
Conflicts
of
interest
Theauthorsdeclarenoconflictsofinterest.
References
1.O’LearyR,McKinlayJ.Neurogenicpulmonaryoedema.Contin EducAnesthCritCare.2011;V1:87---92.
2.DavidsonD,TerekM,ChawlaL.Neurogenicpulmonaryedema. CritCare.2012;16:212.
3.BaumannA, AudibertG, McDonnellJ,etal. Neurogenic pul-monaryedema.ActaAnaesthesiolScand.2007;51:447---55. 4.TanC,LaiC.Neurogenicpulmonaryedema.CanMedAssocJ.
2007;177:250.
5.VenkatesanAM,KarmpaliotisD,SilvermanES.Neurogenic pul-monaryedemafollowingcatastrophicsubaracnoidhemorrhage: acasereportandpathophysiologicreview.JIntensiveCareMed. 2001;16:236---42.
6.LakkireddigariS, DurgaP,Nayak M,et al.Preoperative neu-rogenic pulmonary edema: a dilemma for decision making. JAnaesthesiolClinPharmacol.2012;28:232---4.
7.Davidyuk G, Soriano S, Goumnerova L. Acute intraoperative neurogenic pulmonary edema during endoscopic ventricu-loperitoneal shunt revision. Int Anesth Res Soc. 2010;110: 594---5.
8.WestJB.Cellularresponsestomechanicalstressinvitedreview: pulmonary capillary stress failure. J Appl Physiol. 2000;89: 2483---9.
9.FigueiredoE,OliveiraA,AlmeidaC,etal.Subarachnoid hemor-rhageandhydrocephaluscausingneurogenicpulmonaryedema. ArqNeuropsiquiatr.2010;68:461---2.
10.AhrensJ,CapelleH,PrzemeckM.Neurogenicpulmonaryedema in a fatal case of subarachnoidhemorrhage. J Clin Anesth. 2008;20:129---32.
11.YabumotoM,Kuriyama T, IwamotoM.Neurogenic pulmonary edema associated withruptured intracranial aneurism: case report.Neurosurgery.1986;19:300---4.
12.BritoJ,DinizM,RosasR,etal.Edemapulmonaragudo neu-rogênico:relatodecaso.ArqNeuro-psiquiatr.1995;53:288---93. 13.McGuireG,CrossleyD,RichardsJ,etal.Effectsofvaryinglevels ofpositiveend-expiratorypressureonintracranialpressureand cerebralperfusionpressure.CritCareMed.1997;25:1059---62. 14.Dehan P. Haemodynamic changes in neurogenic pulmonary
edema: effectof dobutamine. Intensive CareMed. 1996;22: 672---7.