Original article
Disseminated histoplasmosis and aids: relapse and late mortality in
endemic area in north-eastern Brazil
Lisandra Serra Damasceno,1,2Alberto Novaes Ramos Jr,1 Carlos Henrique Morais Alencar,1,4 Daniel Teixeira Lima,3Jose Julio Costa Sidrim,3Maria V^ania Freitas Goncßalves,2
Jaco Ricarte Lima de Mesquita2and Terezinha do Menino Jesus Silva Leit~ao1,2
1Department of Community Health, School of Medicine, Federal University of Ceara, Fortaleza, CE, Brazil, 2Hospital Sao Jos~ e of Infectious Diseases, Health
Department of Ceara, Fortaleza, CE, Brazil, 3Specialized Medical Mycology Center, Federal University of Ceara, Fortaleza, CE, Brazil and 4Swiss Tropical
and Public Health Institute, University of Basel, Basel, Switzerland
Summary
The State of Ceara in north-eastern Brazil has one of the highest rates in the world of relapse and death due to disseminated histoplasmosis (DH) in acquired immunode-ficiency syndrome (AIDS) patients. The objective of this study is to characterise the relapse and mortality of DH in AIDS cases residents in Ceara. We performed a retro-spective analysis of the medical records of AIDS patients who had a first episode of DH from 2002 to 2008. We analysed the outcomes until December 31, 2010. A total of 145 patients participated in the study. The mean clinical follow-up duration was 3.38 years (SD =2.2; 95% CI=3.01–3.75). The majority of the subjects weremale with a mean age of 35 years (SD =2.2; 95% CI= 3.01–3.75) and were born
in the capital of Ceara. DH was the first manifestation of AIDS in 59% of the patients. The relapse rate was 23.3%, with a disseminated presentation in 90% of these patients. The overall mortality during the study period was 30.2%. The major-ity of patients who relapsed or died had irregular treatment with antifungals or highly active antiretroviral therapy and did not have active clinical follow-up. High rates of recurrence and mortality were found in AIDS-associated DH in this area of the country.
Key words: disseminated histoplasmosis, AIDS, mortality, mycoses.
Introduction
Disseminated histoplasmosis (DH) is considered to be present when Histoplasma capsulatum is found in extrapulmonary and/or extranodal organs.1 Before the acquired immunodeficiency syndrome (AIDS) pan-demic, cases of DH were rarely observed and were
limited to patients with malignant haematological diseases, immunosuppression due to drug use, primary cellular immunodeficiencies,2–4 advanced age, chronic
alcoholism, diabetes mellitus or in children less than 2 years of age.5,6
Currently, AIDS is the most important risk factor for DH,7 affecting predominantly male young adults due to primary acquisition or reactivation of a latent infec-tion.7–10The estimated incidence of histoplasmosis varies
from 5% to 25% in HIV residents of endemic areas.11,12 The Ceara State in the north-east region of Brazil reports one of the largest numbers of cases of DH in the world.13
Relapses for histoplasmosis in immunodeficiency virus (HIV) patients in endemic areas of the US and Panama occur in less than 6%.14,15However, a preli-minary study conducted in Ceara from 1999 to 2005 in patients with this co-infection indicated a relapse
Correspondence:Ms. Lisandra Serra Damasceno Department of
Commu-nity Health, School of Medicine, Federal University of Ceara, Rua Professor
Costa Mendes, 1608, Bloco Didatico– 5°andar. Rodolfo Teofilo. CEP:
60430-140. Fortaleza, Ceara, Brazil
Tel: 55-85-33668044. Fax: 55-85-33668050 Email: lisandraserra@yahoo.com.br
Submitted for publication26 July 2012
Revised3 February 2013
Accepted for publication7 February 2013
index greater than 20% during a 2-year follow-up per-iod.16There is no consensus regarding the suspension of secondary prophylaxis; however, clinical follow-up data have demonstrated that interruption is possible once immune recovery is achieved after highly active antiretroviral therapy (HAART).11,17–21
Mortality due to DH and AIDS is variable throughout the world and is ~10% in developed countries and
~30% in areas with limited financial resources.16,17In the early 2000s, the mortality of the first DH episode in AIDS patients in the state of Ceara was 32.8%, with a higher figure of 47.8% if the deaths occurred in the 2-year period of follow-up.16 The purpose of this study was to better characterise the relapse and late mortal-ity (death after the hospital discharge) of AIDS patients after the first DH episode that were followed up in the reference units of an endemic area from 2002 to 2008.
Methods
The medical records of AIDS patients with a first epi-sode of DH diagnosed during hospitalisation in refer-ence units from 2002 to 2008 were reviewed. Three public reference health units for HIV patients partici-pated in the study: Hospital S~ao Jose of Infectious Dis-eases (HSJ), Hospital Universitario Walter Cantıdio (HUWC) and the outpatient clinic Centro de Especialid-ades Medicas Jose de Alencar, located in Fortaleza, the capital of Ceara State in north-eastern Brazil, with 2.5 million inhabitants. The HSJ is responsible for attending to 85% of the HIV patients in Ceara.
The patients were identified through a review of the laboratory records of HSJ and the Specialized Medical Mycology Center, which provides mycology laboratory support to HUWC. The study included AIDS patients who were diagnosed according to the Brazilian Ministry of Health criteria,22 males and females who were over 18 years of age and who had confirmed DH byH. cap-sulatum identification for microscopy (histology or stained smears) and/or culture of the affected tissues or fluids, and survivors of their first DH episode. The data were collected from the date of a DH diagnosis until December 31, 2010. We excluded the patients with no medical records available after the DH diagnosis, patients cared for by other institutions and cases with histoplasmosis in lung tissue and/or the ganglion only.
The epidemiological, laboratory, treatment and out-come (relapse and death) variables were evaluated. The risk activity for histoplasmosis was considered when a patient had an occupation that was related to soil till-age (excavation, construction, demolition or agricul-ture), worked directly with chickens or visited caves.
Regular use of antifungals was evaluated in the medical records according to patient’s self-reports that were systematically recorded by the attending physi-cian during follow-up. The induction dose for the DH treatment was considered when amphotericin B de-oxicholate (ABdes) was administered in a dose of 0.7–1.0 mg Kg 1day 1, followed by itraconazole 400 mg day 1.20The total induction time was consid-ered to be the period of time that the antifungals (ABdes and itraconazole) were used in the induction dose. The maintenance dose of antifungals in patients was considered to be the use of ABdes one time a week or itraconazole 200 mg day 1.20
The regular use of HAART was assessed from the medical records of patients, according to self-reports that were systematically recorded by the physician during follow-up and through viral load undetectabili-ty. The mean time for the first readmission was the period after hospital discharge after the first DH event until the next hospitalisation. A relapse of histoplas-mosis was considered in patients who presented another episode at least 60 days after the first DH event and that was confirmed by isolation of the fun-gus in any tissue or body fluid. Patients who stopped clinical follow-up for more than a year before the end of the study (December 31, 2010) were excluded from the outcomes (relapse and mortality) analysis.
Presumed DH was considered for the patients who presented clinical improvement after treatment based on the signs, symptoms and laboratory tests, but with-out H. capsulatumidentification for microscopy (histol-ogy or stained smears) and/or culture.11,23 That is a common practice in AIDS patients cared for in the studied hospitals. Active clinical follow-up was consid-ered to be at least three outpatient visits per year. The Ministry of Health of Brazil recommends clinic visits at 3–4-month intervals.
Epi-Info, version 3.5.1 (Centers for Disease Control and Prevention, Atlanta, Georgia, USA), was used for data entry. Parametric and non-parametric tests were performed using the software program STATA 9.0 (StataCorp LP, College Station, Texas, USA). We per-formed a descriptive analysis of the variables studied. The study protocol was reviewed and approved by the ethical boards of HSJ (protocol no. 029/2008) and HUWC (protocol no. 115.09.09).
Results
these, 40 patients were excluded due to being cared for at another institution or because of missing records; consequently, 145 patients participated in the analysis.
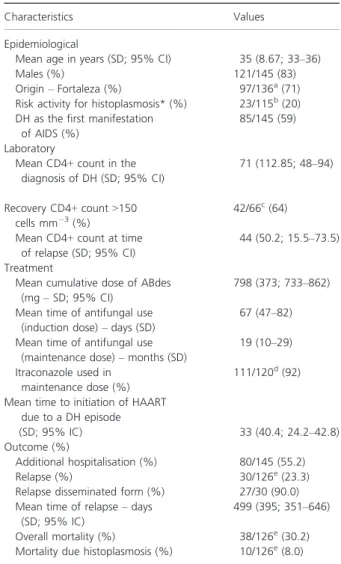
Figure 1 shows the annual distribution of the patients who were followed in this study, with a mean of 38 cases per year (SD=10). The epidemiological, laboratory, treatment and outcome characteristics are presented in Table 1. The subjects had a mean age of 35 years (SD= 8.7; 95% CI=33.2–36.0) and the majority were males who were born in Fortaleza (the state capital) and did not have a known risk activity for histoplasmosis. DH was the first AIDS manifesta-tion in 59% of the patients, and the mean CD4+count at that time was 71 cells mm 3 (SD=112.8; 95% CI=46–94).
Amphotericin B deoxicholate was used in 97% of the patients during the first DH event. The mean cumulative dose of ABdes was 798 mg (SD= 373; 95% CI=733–862). The mean total induction time (ABdes plus 400 mg itraconazole) was 67 days (SD=46.8; 95% CI =46.7–87.2). Determining the total induction time of the antifungal treatment was possible in only 23 medical records due to the lack of information concerning the itraconazole induction dose. The maintenance dose of itraconazole was better recorded, and it was initiated in 92% of the patients, only 51% of whom used it regularly.
The clinical mean follow-up time was 3.38 years (SD=2.2; 95% CI=3.01–3.75). Active clinical
fol-low-up was observed in 79 (54.5%) patients. At the end of the study, 86 (59%) patients had information concerning the use of the antifungal maintenance dose. Discontinuation of the antifungal on medical advice was observed in 27 of 86 patients; the mean CD4+ count at the time of the suspension was 378 cells mm 3 (SD= 147.65; 95% CI=317–438), and all of the patients had undetectable viral loads. The mean follow-up period after discontinuation was 2.85 years (SD=1.47; 95% CI =2.24–3.46) and one
patient relapsed with the pulmonary form of histoplas-mosis by the end of the study; this patient had a his-tory of being lost to clinical follow-up 1 year before the diagnosis of recurrence. The remaining 59 patients continued in antifungal prophylaxis.
Of the 145 patients, 19 were lost to follow-up, with more than 12 consecutive months without a medical
Table 1 Characteristics and outcomes of patients with dissemi-nated histoplasmosis and AIDS, Fortaleza, Ceara, Brazil, 2002– 2008.
Characteristics Values Epidemiological
Mean age in years (SD; 95% CI) 35 (8.67; 33–36)
Males (%) 121/145 (83) Origin–Fortaleza (%) 97/136
a(71)
Risk activity for histoplasmosis* (%) 23/115b(20)
DH as the first manifestation of AIDS (%)
85/145 (59) Laboratory
Mean CD4+count in the diagnosis of DH (SD; 95% CI)
71 (112.85; 48–94)
Recovery CD4+count>150 cells mm 3(%)
42/66c(64)
Mean CD4+count at time of relapse (SD; 95% CI)
44 (50.2; 15.5–73.5)
Treatment
Mean cumulative dose of ABdes (mg–SD; 95% CI)
798 (373; 733–862)
Mean time of antifungal use (induction dose)–days (SD)
67 (47–82)
Mean time of antifungal use (maintenance dose)–months (SD)
19 (10–29)
Itraconazole used in maintenance dose (%)
111/120d(92)
Mean time to initiation of HAART due to a DH episode
(SD; 95% IC) 33 (40.4; 24.2–42.8)
Outcome (%)
Additional hospitalisation (%) 80/145 (55.2) Relapse (%) 30/126e(23.3)
Relapse disseminated form (%) 27/30 (90.0) Mean time of relapse–days
(SD; 95% IC)
499 (395; 351–646)
Overall mortality (%) 38/126e(30.2)
Mortality due histoplasmosis (%) 10/126e(8.0)
*Risk activity for histoplasmosis: the patient had an occupation that was related to soil tillage (excavation, construction, demoli-tion, or agriculture), working directly with chickens or visiting caves.
a
A total of nine patients has not registered about origin; b30 patients has not registered about risk activity for histoplasmosis; c
Only 66 patients has registered about recovery CD4+count;d25 patients has not registered about antifungal use in maintenance dose; e19 patients were lost to follow-up before the end of the study.
2002 0 5 10 15 20 25 30 35
2003 2004 2005 2006 2007 2008
N
u
m
b
e
r
o
f c
a
s
e
s
=
1
4
5
Year
visit until the end of the study, and thus 126 patients were submitted to an analysis of the outcomes. Relapse was detected in 23.3% (30/126) of the patients, and the shortest time to relapse was 71 days. The mean time to relapse was 499 days (SD= 395.75; 95% CI=351–646). Eighty per cent (24) of the patients had one relapse, and 20% (6) had more than one relapse. The disseminated form was observed in 27 patients (90%), and the localised form presented in three patients (two patients with involvement in the lungs and one patient with involvement in the lymph nodes). Of the patients who relapsed, 78% used anti-fungals irregularly, 73% had no active medical super-vision and 6% were taking HAART regularly; 55% of the patients who relapsed used efavirenz (EFZ) in the HAART regimen, and, of those who had not relapsed, 53% were also taking EFZ as a part of their drug regi-men. In 14 patients, the mean of the CD4+counts at the time of relapse was 44 cell mm 3 (SD =50.2; 95% CI=15.5–73.5).
All patients diagnosed with HIV and AIDS (59%) due to a DH episode had HAART initiated in a mean time of 33 days (SD=40.4; 95% CI=24.2–42.8)
after the identification of the fungus. For those cases with a previous AIDS diagnosis (41%), the majority of the subjects (92%) were already using HAART, with a mean time of 1.4 years of therapy (SD=2.5; 95% CI=0.29–2.3). The antiretroviral regimens used by
the majority of the participants were two nucleoside analogue reverse transcriptase inhibitor (NRTI) com-bined with EFZ (53%) or lopinavir plus ritonavir (27%). More than 60% of the patients recovered to a CD4+ count >150 cells mm 3 during the clinical follow-up period.
After discharge from the hospital following the first DH episode, 55.2% (80/145) of the patients were read-mitted. Of these, 38 (47.5%) patients had one readmis-sion after a mean time of 405 days (SD=498.9; 95% CI=291–519), whereas 42 (52.5%) patients required
readmission more than once. The most frequent diag-noses in the first additional hospitalisation period were DH (19%), neurotoxoplasmosis (17%), presumed DH (15%), pulmonary tuberculosis (11%) and other opportunistic diseases (38%).
The 126 patients followed until the end of the study had an overall mortality of 30.2%. The mean time until death was 1.5 years (SD=1.83; 95% CI=0.85
–2.17). The primary causes of death were confirmed
histoplasmosis (10/38 – 26%), presumed DH (6/38 – 16%) and another opportunistic diseases (13/38 – 34%). In nine (24%) patients, the primary cause of death was not identified. Of the patients who died,
72% did not use antifungal medication regularly, 68% had not had active clinical follow-up and 92% did not take HAART regularly; 20% (6/30) of the patients who relapsed died during their first relapse episode and the mortality by confirmed histoplasmosis was 8% (10/126).
Discussion
This study found that concurrent DH and AIDS illness is a common presentation in this region of Brazil, with high rates of recurrence and overall mortality. A high number of cases of this co-infection (38 cases per year) was detected in this study when compared with a pre-vious series (19 cases per year) from the same area16,24 and with other endemic areas of Panama (28 cases per year) and Guyana (9 cases per year).13,14 This larger number of DH cases appears to be consistent with the increased number of AIDS cases detected in the same study period in Ceara. According to data from the Ministry of Health of Brazil from 2002 to 2008, 5899 new cases of AIDS were detected in Ceara, with 48% of these detected in the last 3 years.25 It is likely that our results represent the involvement of more than one centre and a greater sensitivity of physicians to the diagnosis of new cases rather than to an actual increase in disease occur-rence. Further studies based on the population at risk for DH are needed to better understand the occurrence of this disease in the area.
The epidemiological characteristics of the patients in this study were similar to those that have been observed in other studies.16,26,27 The mean age of 35 years was in accordance with studies conducted in the US and French Guiana15,28in the same population and with the most frequent age group of people with HIV/AIDS in Ceara (20 –39 years of age).29 No risk
activity was associated with DH in this study. Unis
et al.(2004) evaluated 70 patients with DH and AIDS and found microfoci that were contaminated with
H. capsulatum in 5.7% of the cases.9 Chang et al.
(2007) found an association between histoplasmosis and risk factors in a small proportion of patients (26.7%).30
The number of patients who had DH as the first manifestation of AIDS varied from 34% to 100% in the literature.8,10,15In this series, the proportion was
~60%. It is estimated that a late diagnosis of HIV infection occurs in 20–60% of patients throughout the world.31–34 In Brazil, patients first detected with a
et al. (2011) analysed the survival of adult patients with AIDS in the southern and south-eastern regions of Brazil in a cohort from 1998 to 1999 and observed that a late diagnosis of AIDS was a significant predic-tor of mortality.37Other studies conducted in Brazilian children showed similar results.38,39 Fagundes et al.
(2010) analysed 175 patients in Brazil who had opportunistic infections in the pre- and post-HAART era and found that 42.3% of the patients had an opportunistic disease, including oral thrush, diarrhoea and pneumocystosis, in the post-HAART era.40 The same observation was found in a study from French Guiana conducted by Nacher et al. (2011) that observed a high incidence of histoplasmosis in the post-HAART era.41
Regarding treatment, ABdes was used in the major-ity (97%) of cases as the initial induction therapy and the mean cumulative dose in excess of 700 mg was compatible with the current recommendations pub-lished in 2009.11 In the Infectious Diseases Society of America (IDSA) guideline of 2007, the induction time was modified for 12 months21 instead of 12 weeks as was previously recommended in 2000. The current study found a mean induction time that was below the recommendation (12 weeks) for that period (because the study was done primarily before the 2007 guideline update). The duration of antifungal use (induction and maintenance) could have been underestimated due to the lack of information in many of the outpatient medical records concerning the itrac-onazole 400 mg dose.
The relapse rate of 23.3% was similar to the rate that was observed in a study by Pontes et al. (2010) in the same area.16 This rate is considered very high compared with other endemic regions, such as Pa-nama and the US, where rates of recurrence range from 0% to 6%.14,15 Based on these data, Ceara became one of the regions with the highest rates of relapse due to histoplasmosis in the world. This rate may be even higher because several patients had pre-sumed DH (22 patients) and their symptoms subsided after specific treatment. The sensitivities of smear staining and culture are ~50% and 77% respec-tively15,42; therefore, several of the presumed DH cases could have been unable to be confirmed.
The Brazilian distribution programme of antiretrovi-rals had a remarkable effect on morbidity and mortal-ity of AIDS in Brazil.43 However, opportunistic infections remain the major cause of morbidity and mortality of AIDS patients, predominantly in north-eastern Brazil. In this study, very few patients who relapsed were taking HAART regularly, and, in more
than 50% of the studied cases, the patients were mitted during follow-up, with the majority of the read-missions due to opportunistic diseases. Consequently, new strategies to care for the AIDS population in this part of Brazil are urgently needed.
Histoplasmaantigen detection has become an impor-tant tool in the US for the rapid diagnosis of histoplas-mosis.44 This antigen test can be performed in blood or urine and has a high sensitivity and specificity.15 These tests are used for the diagnosis of DH in AIDS patients and to predict relapse. Patients with signs or symptoms of histoplasmosis and positive antigen tests (a value greater than 4.1 UI) or asymptomatic patients with an increased value in test levels and a drop in the basal CD4+ count are considered to be in relapse.15 Unfortunately, these diagnostic tests are not available in Brazil or in most countries that are ende-mic for histoplasmosis.
There is no consensus in the literature regarding the discontinuation of antifungal maintenance doses for histoplasmosis. A study of 32 patients in the US and a study of 20 patients in Argentina demonstrated that discontinuation of secondary prophylaxis is possi-ble when patients use itraconazole prophylaxis for more than 12 months and there is immunity reconsti-tution due to HAART.15,18 These studies did not find an episode of recurrence after a follow-up that was longer than 24 months. The 27 patients who had medical advice for prophylaxis discontinuation in this series exhibited immune recovery (CD4+ count
>150 cells mm 3) with HAART; one patient relapsed
by the end of the study, but this patient had aban-doned clinical follow-up 1 year before the recurrence.
The overall mortality (30.2%) in our study was con-sidered high when compared with the study by Gut-ierrez et al. (2005), in which mortality rate was 12.5% after following 104 patients in Panama.14 Baddley et al. (2008) detected a mortality of 39.0% during a short period of observation (3 months) after a diagnosis of histoplasmosis in patients in Alabama, US.45 Pontes et al. (2010) found an overall mortality of 47.8% in Ceara after studying 134 patients with DH and AIDS at HSJ during 2 years of follow-up; how-ever, the authors included the obituaries that occurred during the first event in the analysis, which accounted for the majority of the deaths (69%).16
were preferred drugs used in the HAART by the study participants (taken by more than 50% of the patients). It is known that the use of EFZ or lopinavir plus riton-avir (used by 27% of the patients) interacts with itrac-onazole, decreasing or increasing serum levels of this antifungal respectively.46–49 This could have
influ-enced the higher number of relapses and death noticed here, as well as increased risk drug toxicity. In the hospitals studied, the serum level of itraconazole was not monitored, so data concerning drugs interactions were not obtained and consequently limited the evalu-ation of this issue; no modificevalu-ation in the HAART or antifungal dosage to optimising treatment was men-tioned in the records as this is not a common proce-dure in hospitals from Ceara. An important fact revealed in this study was that of those who had not relapsed, 53% were also taking EFZ as a part of their drug regimen. Another study determining the factors related to these outcomes is in course and the results will be submitted for publication soon. It is necessary to monitor patients effectively regarding treatment and clinical follow-up, as well as to provide greater train-ing to physicians regardtrain-ing the treatment of this co-infection.
Some limitations should be considered in this study. The retrospective design did not allow a standardised collection of data, and the deficit of registers concern-ing the time of antifungal treatment (induction and maintenance) caused some difficulty with the actual evaluation of this variable. The missing records were another important aspect that prevented a more com-plete analysis of the outcomes variables. However, this study was of primary relevance because it more effec-tively characterised the relapse and the late mortality rates in patients with DH and AIDS in the post-HA-ART era and corroborated previous findings of the pos-sibility of a suspension of prophylatic antifungal medication after immune recovery with the use of HAART.
In summary, this study has demonstrated that DH is a common opportunistic disease in people living with HIV/AIDS in Ceara, with high rates of relapse and late mortality during the follow-up period.
Acknowledgments
We are very grateful to the patients and the institu-tions that were involved in this research.
Conflicts of interest
We declare that there are no conflicts of interest.
References
1 Centers for Disease Control and Prevention. 1987 revision of the CDC surveillance case definition for acquired immunodeficiency syn-drome.MMWR Morb Mortal Wkly Rep, 1987;36(Suppl. 1): 1–15.
2 Ferreira MS, Borges AS. Histoplasmose.Rev Soc Bras Med Trop2009; 42: 192–8.
3 Kauffman CA. Histoplasmosis: a clinical and laboratory update.Clin Microbiol Rev2007;20: 115–32.
4 Zerbe CS, Holland SM. Disseminated histoplasmosis in persons with interferon-receptor 1 deficiency.Clin Infect Dis2005;41: 38–41.
5 Severo LC, Oliveira FM, Irion K, Porto NS, Londero AT. Histoplasmo-sis in Rio Grande do Sul, Brazil: a 21 year experience.Rev Inst Med Trop Sao Paulo2001;43: 183–7.
6 Tobon AM, Agudelo CA, Rosero DSet al.Disseminated histoplasmo-sis: a comparative study between patients with acquired immunode-ficiency syndrome and non-human immunodeimmunode-ficiency virus-infected individuals.Am J Trop Med Hyg2005;73: 576–82.
7 Pietrobon D, Negro-Marquinez L, Kilstein J, Galındez J, Greca A, Battagliotti C. Disseminated histoplasmosis and AIDS in an Argen-tine hospital: clinical manifestations, diagnosis and treatment.
Enferm Infecc Microbiol Clin2004;22: 156–9.
8 Casotti JA, Motta TQR, Ferreira Junior CUG, Cerutti Junior C. Disseminated histoplasmosis in HIV positive patients in Espirito Santo state, Brazil: a clinical-laboratory study of 12 cases (1999-2001).Braz J Infect Dis2006;10: 327–30.
9 Unis G, Oliveira FM, Severo LC. Histoplasmose disseminada no Rio Grande do Sul.Rev Soc Bras Med Trop2004;37: 463–8.
10 Mora DJ, dos Santos CT, Silva-Vergara ML. Disseminated histoplas-mosis in acquired immunodeficiency syndrome patients in Uberaba, MG, Brazil.Mycoses2007;51: 136–40.
11 Centers for Disease Control and Prevention. Guidelines for prevention and treatment of opportunistic infections in HIV-infected adults and adolescents. Recommendations from CDC, the National Institutes of Health, and the HIV Medicine Association of the Infectious Diseases Society of America.MMWR Morb Mortal Wkly Rep2009;58: 1–
216.
12 Wheat LJ, Kauffman CA. Histoplasmosis.Infect Dis Clin North Am
2003;17: 1–19.
13 Couppie P, Aznar C, Carme B, Nacher M. American histoplasmosis in developing countries with a special focus on patients with HIV: diagnosis, treatment, and prognosis.Curr Opin Infect Dis2006;19: 443–9.
14 Gutierrez ME, Canton A, Sosa N, Puga E, Talavera L. Disseminated histoplasmosis in patients with AIDS in Panama: a review of 104 cases.Clin Infect Dis2005;40: 1199–202.
15 Goldman M, Zackin R, Fichtenbaum CJet al.Safety of discontinua-tion of maintenance therapy for disseminated histoplasmosis after immunologic response to antiretroviral therapy.Clin Infect Dis2004; 38: 1485–9.
16 Pontes LB, Leit~ao TMJS, Lima GG, Gerhard ES, Fernandes TA. Caract-erısticas clınico-evolutivas de 134 pacientes com histoplasmose dis-seminada associada a SIDA no Estado do Ceara.Rev Soc Bras Med Trop2010;43: 27–31.
17 Karimi K, Wheat LJ, Connoly Pet al.Differences in histoplasmosis in patients with acquired immunodeficiency in the United States and Brazil.J Infect Dis2002;186: 1655–61.
18 Negroni R, Helou SH, Lopez-Daneri G, Robles AM, Arechavala AI, Bianchi MH. Interrupicion de la prophilaxis secundaria antifungica em la histoplasmosis asociada al sida.Rev Iberoam Micol2004;21: 75–8.
19 Sun HY, Chen MY, Hsieh SM, Hung CC, Chang SC. Successful dis-continuation of secondary prophylaxis for histoplasmosis after higly active antiretroviral therapy.J Formos Med Assoc2004;103: 546–8.
20 Wheat J, Sarosi G, McKinsey Det al.Practice guidelines for the man-agement of patients with histoplasmosis.Clin Infect Dis2000;30: 688–95.
patients with histoplasmosis: 2007 update by the Infectious Diseases Society of America.Clin Infect Dis2007;45: 807–25.
22 BRASIL. Ministerio da Saude. Secretaria de Vigil^ancia em Saude. Programa Nacional de DST e Aids. Criterios de definicß~ao de casos de AIDS em adultos e criancßas. Brasılia: Ministerio da Saude, 2003. 23 Daher EF, Silva GB Jr, Barros FASet al.Clinical and laboratory
fea-tures of disseminated histoplasmosis in HIV patients from Brazil.Trop Med Int Health2007;12: 1108–15.
24 De Franchesco Daher E, Barros FAS, da Silva Junior GBet al.Risk factors for death in acquired immunodeficiency syndrome-associated disseminated histoplasmosis.Am J Trop Med Hyg2006;74: 600–3.
25 BRASIL. Ministerio da Saude. Secretaria de Vigil^ancia em Saude. De- partamento de DST, Aids e Hepatites Virais. Boletim Epidemiologico–
AIDS e DST, Brasılia: Ministerio da Saude, 2010.
26 Huber F, Nacher M, Aznar Cet al.AIDS-relatedHistoplasma capsula-tumvar.capsulatuminfection: 25 years experience of French Guiana.
AIDS2008;22: 1047–53.
27 Couppie P, Sobesky M, Aznar Cet al.Histoplasmosis and Acquired Immunodeficiency Syndrome: a study of prognostic factors.Clin Infect Dis2004;38: 134–8.
28 Couppie P, Clity E, Nacher M, Aznar C, Sainte-Marie D, Carme B, Pradinaud R. Acquired immunodeficiency syndrome-related oral and/or cutaneous histoplasmosis: a descriptive and comparative study of 21 cases in French Guiana.Int J Dermatol2002;41: 571–5.
29 CEARA. Governo do Estado. Secretaria de Sa ude do Estado. Informe Epidemiologico AIDS. Fortaleza, 2011.
30 Chang MR, Taira CL, Paniago AMM, Taira DL, Cunha RV, Wanke B. Study of 30 cases of histoplasmosis observed in the Mato Grosso do Sul State, Brazil.Rev Inst Med Trop S Paulo2007;49: 37–9.
31 Girardi E, Sabin CA, Monforte AD. Late diagnosis of HIV infection: epidemiological features, consequences and strategies to encourage earlier testing.J Acquir Immune Defic Syndr2007;46(Suppl. 1): 3–8.
32 Girardi E, Sampaolesi A, Gentile M, Nurra G, Ippolito G. Increasing proportion of late diagnosis of HIV infection among patients with AIDS in Italy following introduction of combination antiretroviral therapy.J Acquir Immune Defic Syndr2000;25: 71–6.
33 Althoff KN, Gange SJ, Klein MBet al.Late presentation for human immunodeficiency virus care in the United States and Canada.Clin Infect Dis2010;50: 1512–20.
34 Girardi E, Aloisi MS, Arici Cet al.Delayed presentation and late test-ing for HIV: demographic and behavioral risk factors in a multicenter study in Italy.J Acquir Immune Defic Syndr2004;36: 951–9.
35 Fernandes JR, Acurcio FA, Campos LN, Guimar~aes MDC. Inicio da terapia anti-retroviral em estagio avancado de imunodeficiencia entre individuos portadores de HIV/AIDS em Belo Horizonte, Minas Gerais, Brasil.Cad Saude Publica2009;25: 1369–80.
36 Grangeiro A, Escuder MM, Menezes PR, Alencar R, Castilho EA. Late entry into HIV care: estimated impact on AIDS mortality rates in Brazil, 2003–2006.PLoS ONE2011;6: e14585.
37 Guibu AI, Barros MBA, Donalısio MR, Tayra A, Alves MCGP. Sur-vival of AIDS in the Southeast and South of Brazil: analysis of the 1998–1999 cohort.Cad Saude Publica2011;27(Suppl. 1): 579–92.
38 Ramos AN Jr, Matida LH, Hearst NG, Heukelbach J. AIDS morbidity and mortality in Brazilian children before and after HAART imple-mentation: an assessment of regional trends.Pediatr Infect Dis J2011; 30: 773–7.
39 Ramos AN Jr, Matida LH, Hearst NG, Heukelbach J. Opportunistic ill-nesses in Brazilian children with AIDS: results from two national cohort studies, 1983–2007.AIDS Res Ther2011;8: 23.
40 Fagundes VHV, Oliveira JHT, Vieira S, Spack Junior M, Pupulin ART. Infeccß~oes oportunistas em indivıduos com infeccß~ao pelo HIV e relacß~ao com uso de terapia antiretroviral.Acta Sci Health Sci2010;32: 141–5.
41 Nacher M, Antoine Adenis A, Adriouch Let al.Short report: what is AIDS in the Amazon and the Guianas? Establishing the burden of disseminated histoplasmosis.Am J Trop Med Hyg2011;84: 239–40.
42 Leimann BCQ, Pizzini CV, Muniz MMet al.Histoplasmosis in a Brazil-ian center: clinical forms and laboratory tests.Rev Iberoam Micol
2005;22: 141–6.
43 Polejack L, Seidl EMF. Monitoramento e avaliacß~ao da ades~ao ao tratamento antiretroviral para HIV/aids: desafios e possibilidades.
Cien Saude Colet2010;15(Suppl. 1): 1201–8.
44 Wheat LJ, Connolly-Stringfield P, Blair R, Connolly K, Garringer T, Katz BP. Histoplasmosis relapse in patients with AIDS: detection usingHistoplasma capsulatumvarietycapsulatumantigen levels.Ann Intern Med1991;115: 936–41.
45 Baddley JW, Sankara IR, Rodriguez JM, Pappas PG, Many Jr DJ. Histoplasmosis in HIV-infected patients in a southern regional medi-cal center: poor prognosis in the era of highly active antiretroviral therapy.Diagn Microbiol Infect Dis2008;62: 151–6.
46 Andrade RA, Evans RT, Hamill RJ, Zerai T, Giordano TP. Clinical evi-dence of interaction between itraconazole and non nucleoside reverse transcriptase inhibitors in HIV-infected patients with disseminated histoplasmosis.Annals of Pharmacother2009;43: 908–13.
47 Koo HL, Hamill RJ, Andrade RA. Drug-drug interaction between itr-aconazole and efavirenz in a patient with AIDS and disseminated his-toplasmosis.Clin Infect Dis2007;45: 77–9.
48 Huet E, Hadji C, Hulin A, Botterel F, Bretagne S, Levy Y. Therapeutic monitoring is necessary for the association itraconazole and efavirenz in a patient with AIDS and disseminated histoplasmosis.AIDS2008; 22: 1885–96.
49 Crommentuyn KML, Mulder JW, Sparidans RW, Huitema ADR, Schellens JHM, Beijnen JH. Drug-drug interaction between Itraconaz-ole and the antiretroviral drug Lopinavir/Ritonavir in an HIV-1–
infected patient with disseminated histoplasmosis.Clin Infect Dis