REVISTA
PAULISTA
DE
PEDIATRIA
www.rpped.com.br
REVIEW
ARTICLE
Effects
of
obesity
on
lung
volume
and
capacity
in
children
and
adolescents:
a
systematic
review
Aline
Dill
Winck
a,
João
Paulo
Heinzmann-Filho
b,∗,
Rafaela
Borges
Soares
b,
Juliana
Severo
da
Silva
b,
Cristhiele
Taís
Woszezenki
b,
Letiane
Bueno
Zanatta
caUniversidadedeCaxiasdoSul(UCS),CaxiasdoSul,RS,Brazil
bPontifíciaUniversidadeCatólicadoRioGrandedoSul(PUC-RS),PortoAlegre,RS,Brazil cInstitutoCenecistadeEnsinoSuperiordeSantoÂngelo(Iesa),SantoÂngelo,RS,Brazil
Received4November2015;accepted28February2016 Availableonline25July2016
KEYWORDS
Lungfunctiontests; Lungvolume measurements; Total
plethysmography; Obesity;
Pediatrics
Abstract
Objective: Toassesstheeffectsofobesityonlungvolumeandcapacityinchildrenand adoles-cents.
Datasource: This is a systematic review, carried out inPubmed, Lilacs, Scielo and PEDro databases,usingthefollowingKeywords:Plethysmography;WholeBodyORLungVolume Mea-surementsORTotalLungCapacityORFunctionalResidualCapacityORResidualVolumeAND Obesity.Observational studiesor clinicaltrials thatassessed theeffectsofobesity onlung volumeandcapacity inchildren andadolescents(0---18 years)without anyotherassociated disease;inEnglish;PortugueseandSpanishlanguageswereselected.Methodologicalquality wasassessedbytheAgencyforHealthcareResearchandQuality.
Datasynthesis: Of the 1,030 articles, only four were included in the review. The studies amountedto548participants,predominantlymales,withsamplesizerangingfrom45to327 individuals.100%ofthestudiesevaluatednutritionalstatusthroughBMI(z-score)and50.0% reportedthedataonabdominalcircumference.Alldemonstratedthatobesitycausesnegative effectsonlungvolumeandcapacity,causingareductionmainlyinfunctionalresidualcapacity in75.0%ofthestudies;intheexpiratoryreservevolumein50.0%andintheresidualvolume in25.0%.Themethodologicalqualityrangedfrommoderatetohigh,with75.0%ofthestudies classifiedashavinghighmethodologicalquality.
Conclusions: Obesitycausesdeleteriouseffectsonlungvolumeandcapacityinchildrenand adolescents,mainlyby reducingfunctionalresidualcapacity,expiratoryreservevolumeand residualvolume.
©2016SociedadedePediatriadeS˜aoPaulo.PublishedbyElsevierEditoraLtda.Thisisanopen accessarticleundertheCCBYlicense(http://creativecommons.org/licenses/by/4.0/).
∗Correspondingauthor.
E-mail:joaopauloheinzmann@hotmail.com(J.P.Heinzmann-Filho). http://dx.doi.org/10.1016/j.rppede.2016.03.013
PALAVRAS-CHAVE
Testesdefunc¸ão pulmonar;
Medidasdevolume pulmonar;
Pletismografiatotal; Obesidade;
Pediatria
Efeitosdaobesidadesobreosvolumeseascapacidadespulmonaresemcrianc¸as eadolescentes:umarevisãosistemática
Resumo
Objetivo: Avaliarosefeitosdaobesidadesobreosvolumeseascapacidadespulmonaresem crianc¸aseadolescentes.
Fontesdedados: Trata-sede umarevisão sistemática,atravésdasbases dedadosPubmed, Lilacs,SciELOePEDro,pormeiodasseguintespalavras-chave:Plethysmography,WholeBody OR LungVolumeMeasurementsOR TotalLungCapacity ORFunctionalResidual CapacityOR ResidualVolumeANDObesity.Foramselecionadosestudosobservacionaisouensaiosclínicosque avaliaramosefeitosdaobesidadesobreosvolumeseascapacidadespulmonaresemcrianc¸ase adolescentes(0a18anos),semqualqueroutradoenc¸aassociada,nosidiomasinglês,português eespanhol.AqualidademetodológicafoiavaliadaatravésdaAgencyforHealthcareResearch andQuality.
Síntesedosdados: Dos1.030artigos,apenasquatroforamincluídosnestarevisão.Osestudos totalizaram548participantes,compredomíniodosexomasculinoetamanhoamostralentre45 e327indivíduos;100%dosestudosavaliaramoestadonutricionalatravésdoIMC(escore-z)e50% informaramosdadosdacircunferênciaabdominal.Todosdemonstraramqueaobesidadecausa efeitos negativossobre osvolumes eas capacidades pulmonares, causareduc¸ão, principal-mente,dacapacidaderesidualfuncionalem75%dosestudos,dovolumedereservaexpiratório em50%edovolumeresidualem25%.Aqualidademetodológicavariouentremoderadaealta, com75%dosestudosclassificadoscomaltaqualidademetodológica.
Conclusões: Aobesidadecausaefeitosdeletériossobreosvolumeseascapacidadespulmonares em crianc¸as eadolescentes, comreduc¸ãoprincipalmente dacapacidade residualfuncional, volumedereservaexpiratórioevolumeresidual.
©2016SociedadedePediatriadeS˜aoPaulo. PublicadoporElsevier EditoraLtda.Este ´eum artigoOpenAccesssobumalicenc¸aCCBY(http://creativecommons.org/licenses/by/4.0/).
Introduction
Childhoodobesityiscurrentlyamajorpublichealthproblem andincreasesatanalarmingrateintheworld’spopulation, includingtheBrazilianpopulation.1Itisestimatedthat150 millionadultsand15millionchildrenareobese.2Recently, epidemiologicaldataindicatedthattheprevalenceof obe-sityin theUnited Statesisapproximately17% andaffects about 12.7 million children and adolescents.3 In Brazil, some studies show that the prevalence of obesity ranges from2.4to19.2%,affectingmoretheSouthandSoutheast regions.4
AccordingtotheWorldHealthOrganization,obesitycan bedefinedasanabnormalconditionofbodyfator excess fattissue,whichcausesdamagetotheindividual’shealth.1 Somesituationsorclinicalconditionsseemtobeassociated withitsdevelopment,suchassedentarylifestyle,asthma, diabetes,hypertension,cardiovascularandrespiratory dis-eases.Amongthese,therespiratorysystemdeservesspecial attention,asexcessweightbringsdirectchangesto venti-latorymechanics.1,5,6
Inrecentdecades,previousstudiessuggestedthat obe-sity causes a major change in the respiratory system, resulting in loss on thoracoabdominal synchronism.7 The increaseinbodyweightcauseslimitationofdiaphragmatic mobility andreduced backmovement, withimpaired pul-monary gas exchange and breathing pattern control.7---10 Moreover,excessadiposetissueisassociatedwithincreased inflammatorymediatorsandcytokines,whichcouldalterthe
pulmonaryairwaysofthesesubjectsandcontributetothe developmentofbronchialhyperreactivity.11
Inadditiontotheabovementionedchanges,theresearch onthesubjectpointstothepresenceofimportantlung func-tionalterationsinchildrenandadolescentswithexcessfat, includingreducedforcedexpiratory volumein onesecond (FEV1), forced vital capacity (FVC) and forced expiratory flowbetween25and75%ofFVC(FEF25---75%).12,13
Asystematicreviewpublishedin201214showed,through acriticalanalysisoffivestudies,thatobesityleadstolosses mainly in FEV1 and FVC. However, this study only evalu-atedtheeffectsofbodyweightonspirometricvariables.14 Taking into account that the spirometry test directly investigates obstructive pulmonary parameters and that the obesity factor seems to affect more the restrictive pattern,1,5 the importance of investigating, through ple-thysmography, the effects of body mass on lung volume andcapacityinchildrenisemphasized.Moreover,todate, the results are contradictory in terms of the impact of obesityonthesepulmonary outcomesin samplesofyoung individuals.15
Method
Thestudyconsistsofasystematicreviewcarriedoutthrough asearchinthePubMed,Lilacs,SciELOandPEDrodatabases. Observational studies and clinical trials were selected in English,PortugueseandSpanish,withoutanyfiltersforage andyearofpublicationofthearticles.Theperiodofstudy selectionwasfromSeptembertoOctober2015.
Thesearchusedfor theselection ofarticleswasbased onsixkeywords associatedwithBooleandescriptors.The followingstrategywasused:plethysmography,wholebody ORlung volume measurementsOR total lung capacityOR functionalresidualcapacityORresidualvolumeANDobesity. Thesedescriptorsshouldbe includedat least inthe title, abstractorinthekeywords.
Studiesthatevaluatedlungfunctionbyplethysmography inobesechildrenandadolescents(0---18years)wereusedas inclusioncriteria.Obesitywasdefinedasbodymass index (BMI)z-score values>+2or≥97thpercentile.On theother hand, review studies, case reports, articles that did not assesslung volumeand capacitythroughbody plethysmo-graphy,studies that assessedrespiratory function through otherevaluationmethods ordidnotnormalizetheresults ofpulmonary function(plethysmography)in z-scores, per-centageofpredictedortheonesthatdidnotcomparethe results with those from a control group were excluded. Studies evaluatingthe adultage group or did notinclude onlychildrenandadolescentswerealsoexcluded.Moreover, studieswithsubjectswithanyotherchronicdiseaseswere excluded.
After identifying the descriptors in the title, abstract and/or keywords, the abstracts of selected articles were readtoassesstheadequacyaccordingtotheeligibility crite-ria.Studiesthatmetthepredeterminedcriteriahadthefull text read for detailed analysis and data extraction. Arti-clesearchandanalysis,according totheabovementioned strategywerecarriedoutindependentlybytworeviewers anddisagreementswereresolvedwithathirdreviewer,by consensus.
The following characteristics of the studies were recorded: first author’s name, year of publication of the study,country(source)ofdatacollection,agerange,sample size,bodymass index(BMI),waistcircumference, plethy-smography equipment, methodology used, type of data presentation (z-score, percentage of predicted or liters), assessed plethysmographic variables [expiratory reserve volume(ERV),inspiratoryreservevolume(IRV),residual vol-ume(RV),functionalresidualcapacity(FRC),vitalcapacity (VC),inspiratorycapacity(IC)andtotallungcapacity(TLC)], extrapulmonarytests, mainplethysmographic resultsand additionalresults.
Methodological quality was assessed by two reviewers andanydivergenceswereresolvedbyconsensus.An appro-priate scale for observational studies by the Agency for HealthCareResearchandQuality(AHRQ)wasused.16 This tool evaluates nine items related to the study subject, methodologicalaspects, consistency of results, discussion andsponsorship.Thefinalsumofeachevaluateditemtotals a score of 100, with the studies being classified as low (<50points),moderate(50---66points)andhigh(>66points) methodologicalquality.
Results
Atotalof1030articleswereidentified,808inPubmed,218 inLilacs,twoinSciELOandtwoinPEDro.Ofthese,199were excludedforbeingrepeatedintheassesseddatabasesand 827becausetheydidnotmeettheeligibilitycriteriaofthis review.Thus,onlyfourstudieswereincluded,which eval-uatedthe effects ofobesity onlung volume andcapacity inchildrenandadolescentsthroughbodyplethysmography.
Fig.1showsaflowchartrelatedtothetotalnumberof arti-clesfoundintheassesseddatabasesandreasonsfor study exclusion.
Theselectedstudiestotaledasampleof548participants, withaprevalenceof296(54%)ofmaleindividuals.The sam-plesizeofthestudiesvariedgreatly,rangingfrom45to327 subjects.Theageoftheselectedparticipantsrangedfrom 6 to18.9 years.Allstudies evaluatedBMI throughz-score andtwo(50%)reporteddatafromthewaistcircumference. Of the fourstudies, two were carriedout in Asia, one in AmericaandoneinEurope(Table1).
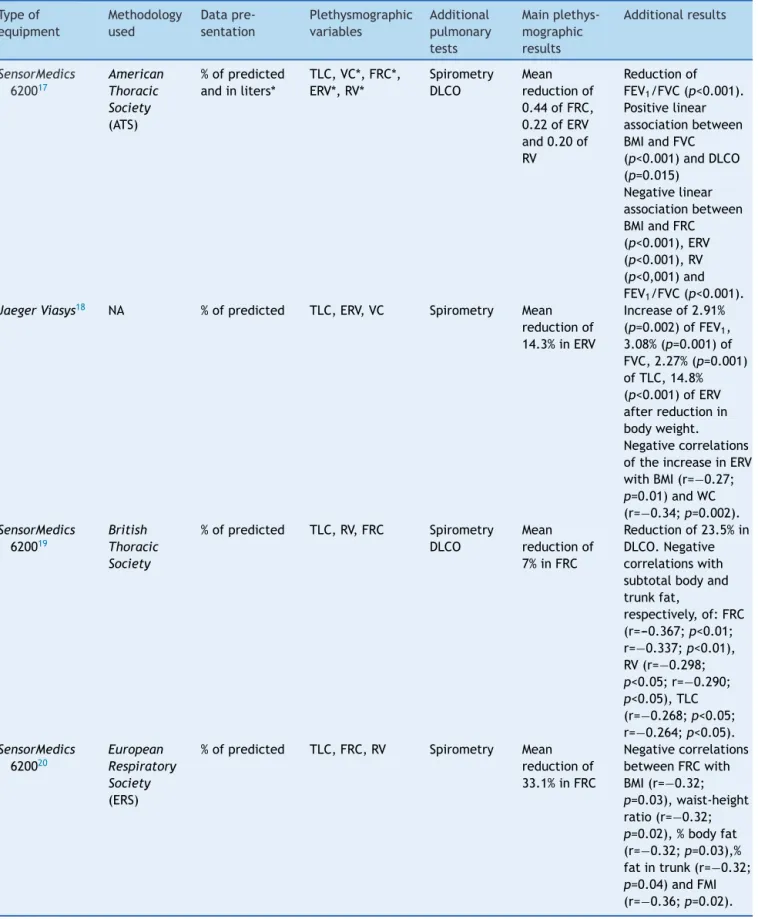
Regardingthecharacteristicsof theequipmentusedto measure lung volume and capacity by plethysmography, three(75%) studiesusedthe SensorMedics equipmentand onlyoneusedaJaegerdevice.Ofthestudies,three(75%) followedtherecommendationsofinternationalguidelines, while one did notreport themethodology usedto obtain the pulmonary data. All studies included normalized the findingsonlungvolumeandcapacitythroughthe percent-ageof predicted,althoughonlyone(25%)evaluatedsome plethysmographicvariablesinabsolutevalues(liters). Addi-tionally,allofthemmeasuredspirometricvariablesand50% measuredthecarbonmonoxidediffusion(DLCO).
The assessed plethysmographic data included VC, ERV, RV,FRCandTLC.Allstudiesshowedthatobesityhasa neg-ative effectonlung volumeandcapacity,mainly reduced FRCin75%ofstudies,ofERVin50%andRVin25%.Overall, thestudieshavealsotestedtheassociationsofventilatory variables and outcomes relatedto obesity,including BMI, waist circumference, fat mass index and waist-to-height ratio(Table2).
Finally, regarding the methodological quality of the selectedarticles(Table3),theaveragescorewas71points, rangingbetween63and83.Ofthese,one(25%)studyhad a scorecompatiblewithmoderate methodologicalquality and three(75%) withhigh quality,according tothe AHRQ scale.Factorsthatloweredthequalityscoreoftheselected studieswereassociatedtoitemsrelatedtothestudy pop-ulation, comparison of subjects, outcome measurement, statistical analysis, discussion of data and informationon supportand/orfundingofthestudy.Itisnoteworthythatof thefourstudies,only onehadjustificationforthesample size,aswellasreportedinformationonblindingregarding whenassessing theresults.Furthermore,only twostudies reportedresearchsupportandfunding,noneof them cal-culated the power of analysis, as well as how potential confoundersandresultbiaseswereassessed.
Discussion
Pubmed (n=808)
Identification
Included
Eligibility criteria
Lilacs (n=218)
Total of studies (n=1030)
Excluded repeated studies (n=199)
Excluded studies (n=827) Assessed studies
(n=831) Reasons for exclusion 298 studies in adults 225 did not assess volumes
189 associated diseases
75 reviews 26 experimental studies
10 case reports
4 without access to article
Included studies (n=4)
Scielo (n=2)
PEDro (n=2)
Figure1 Flowchartofthetotalnumberofarticlesfoundinthedatabases.
Table1 Identificationandcharacteristicsofthestudiesincludedinthisreview.
Firstauthor Year Country Agerange
(years)
Sample size
BMI(z-score) WaistCircumference
Davidsonetal.17 2014 Canada 6---17 327 2.18±0.41 NA
vandeGriendtetal.18 2012 TheNetherlands 8.5---18.9 112 3.38±0.40(2.50---4.62) 122.2±15.7
Lietal.19 2003 China 7---18 64 2.42(2.13---2.66) NA
Kongkiattikuletal.20 2015 Thailand 8.6---17.3 45 3.2±0.5(1.9---4.6) 99.1±10.4(81---134)
BMI,bodymassindex;NA,informationnotavailable.
effectsofobesityonlungvolumeandcapacityinchildren andadolescents.17---20Thefindingsshowedareductionmainly in FRC, ERV and RV, indicating negative effects of excess bodyweightonthesepulmonaryoutcomes.
Studies carried out in obese individuals with no associated comorbidities indicate that the increase in adipose tissue in the chest and abdomen area causes an increase in the intra-abdominal pressure, with con-sequent reduction in lung compliance and chest wall mobility.14,15
Thesealterationsresultinthoracoabdominalasynchrony, lead to diaphragmatic contraction impairment due to increasedloadontheabdomenandalsoimpairtheincrease inchestdiameterthroughthemovementoftheribs.Some findingssuggestthattheincreasedbodymassisassociated withhighertensilestrengthanddecreaseddistensibilityof extrapulmonarystructures.15,21
Under normal physiological conditions, the FRC is the pointofbalanceofelasticretractionsbetweenthelungand thechestwall.22Thus,whereasFRCisthesumofRVandERV, anychangeintheseventilatoryvariablesimpliesinchanges ofthispointofbalance,asdemonstratedbyDavidsonetal.17 Changesinpulmonarybellowscausereducedlungvolumes, withsubsequentestablishmentofarestrictivepattern.23,24 Kongkiattikuletal.20alsoreportedthatthereductionofFRC leadstoincreasedairresistance,peripheralvascular resis-tanceandimpairsalveolarventilation.Furthermore,these datasuggestthatphysiologicalchangesincreasetheriskof atelectasisandhypoxiainobeseindividuals.20,25A system-aticreviewcarriedout intheobeseadult populationalso showedreductionofthesameplethysmographicvariables, withtheadditionofTLCandVC.15
Table2 Characteristicsandmainresultsofthestudiesincludedinthisreview.
Typeof equipment
Methodology used
Data pre-sentation
Plethysmographic variables
Additional pulmonary tests
Main plethys-mographic results
Additionalresults
SensorMedics
620017
American Thoracic Society (ATS)
%ofpredicted andinliters*
TLC,VC*,FRC*, ERV*,RV*
Spirometry DLCO
Mean reductionof 0.44ofFRC, 0.22ofERV and0.20of RV
Reductionof FEV1/FVC(p<0.001). Positivelinear associationbetween BMIandFVC (p<0.001)andDLCO (p=0.015)
Negativelinear associationbetween BMIandFRC (p<0.001),ERV (p<0.001),RV (p<0,001)and FEV1/FVC(p<0.001). JaegerViasys18 NA %ofpredicted TLC,ERV,VC Spirometry Mean
reductionof 14.3%inERV
Increaseof2.91% (p=0.002)ofFEV1, 3.08%(p=0.001)of FVC,2.27%(p=0.001) ofTLC,14.8% (p<0.001)ofERV afterreductionin bodyweight. Negativecorrelations oftheincreaseinERV withBMI(r=−0.27; p=0.01)andWC (r=−0.34;p=0.002). SensorMedics
620019
British Thoracic Society
%ofpredicted TLC,RV,FRC Spirometry DLCO
Mean reductionof 7%inFRC
Reductionof23.5%in DLCO.Negative correlationswith subtotalbodyand trunkfat,
respectively,of:FRC (r=---0.367;p<0.01; r=−0.337;p<0.01), RV(r=−0.298; p<0.05;r=−0.290; p<0.05),TLC (r=−0.268;p<0.05; r=−0.264;p<0.05). SensorMedics
620020
European Respiratory Society (ERS)
%ofpredicted TLC,FRC,RV Spirometry Mean reductionof 33.1%inFRC
Negativecorrelations betweenFRCwith BMI(r=−0.32; p=0.03),waist-height ratio(r=−0.32; p=0.02),%bodyfat (r=−0.32;p=0.03),% fatintrunk(r=−0.32; p=0.04)andFMI (r=−0.36;p=0.02).
%,Percentage;VC,vitalcapacity;TLC,totallungcapacity; FRC,functionalresidual capacity;RV,residual volume,ERV, expiratory
reservevolume;FEV1,forcedexpiratoryvolumeinonesecond;FVC,forcedvitalcapacity;DLCO,carbonmonoxidediffusioncapacity;
Table3 Assessmentofthemethodologicalqualityofthestudiesincludedinthesystematicreview.
Criteriaassessed Referencescore Davidsonetal.17 vandeGriendtetal.18 Lietal.19 Kongkiattikuletal.20
Questionofthestudy 2 2 2 2 2
Studypopulation 8 5 5 5 8
Comparabilityof individualsforthe observationalstudies
22 16 14 11 11
Exposureorintervention 11 11 11 11 11
OutcomeMeasures 20 20 15 15 15
StatisticalAnalysis 19 12 9 7 7
Results 8 8 8 8 8
Discussion 5 4 3 4 4
Fundingandsponsorship 5 5 0 0 5
Totalscore 100 83 67 63 71
continents.17,18 Todate,nostudywasfound carriedoutin the Brazilian pediatric population that aimed to evaluate theinfluenceofobesityonlungvolumeandcapacity. Per-hapsthislackofinformationatthenationallevelisbecause therearefewbodyplethysmographsinthecountry,aswell asthehighcostoftheequipmentandalsothefactthatitis hardertoobtainasatisfactorytestinapediatricsample.26 MoststudiesusedSensorMedicsequipment17,19,20andallof them normalized of lung volumeresults through the per-centageof predicted,17---20 although astudydid notreport theequationused.18
Of the included studies, three followed international guidelinesforbodyplethysmography,includingthe Ameri-canThoracicSociety,EuropeanRespiratorySocietyandthe BritishThoracicSociety.17,19,20Ingeneral,themethodsused seemtoincludethesameventilatorymaneuverstoobtain lung volume and capacity, which contributes to greater externalvalidityoftheresults.
Recently, a systematic review showed the negative effectsofchildhoodobesityonspirometricvariables, indi-catedareductioninFEV1,FVCandFEV1/FVCratio.However, this study did not investigate the effects of the obesity factor onlung volumeandcapacity.14 Takingintoaccount thatobesitymaybeconsideredadiseasewitharestrictive pattern,1,5thedatashownhereaddimportantinformation about the impact of the disease onchildren’s respiratory system, compared to the study published in 2012.14 It is expectedthatfutureresearch,particularlyatthenational level,bedesignedtoassesstheeffectsofthischronic condi-tiononthepulmonarysystem.However,weemphasizethe importancethatnewstudiesstratifytheiragegroups (chil-drenandadolescents),toinvestigatethepossibleinfluence ofmaturationalstateontheseoutcomes.
Moreover,itbecomesessentialtodividethesesubjects astodifferentdegreesofobesity,asinthepresentreview it was not possible to assess the influence of these fac-tors. Although it is possible to evaluate the body mass of childrenand adolescentsthroughseveralmethods, BMI quantificationstands out asa simple and low-cost tool.27 Itis alsoknownthatnormalization usingpercentilesor z-scoresisessentialforabetterassessmentofthenutritional statusofthepediatricpopulation.27,28 Allstudiesincluded in thisreview evaluatedBMIthroughz-scores,which isin accordancewithpediatricrecommendations.27,28Ofthese,
two studies17,20 showed the negative influence of BMI on FRC, ERV and RV through correlation testing and regres-sionmodels.Theseresultssuggestthatthehigherthebody composition,thelowerthelungvolumeandcapacity. Fur-thermore,previousstudieshaveshownnegativecorrelation betweenBMIandspirometricvariables,includingFEV1,FVC, FEF25---75%andFEV1/FVCratio.10,17,20,29Thesefindingssupport thehypothesisthatincreasedbodymasscauselimitationin diaphragmaticmobility,reductionofcostalmovement,and impairspulmonaryphysiology.7,10 Griendtetal.,18 demon-stratedthatbodyweightreductionisrelatedtosignificant improvements in FEV1,FVC, TLC and ERV, indicating that theBMIreductioncontributestotheincreaseinthese out-comes.The authorsexplain these results due tothe fact that,byreducingbodyweight,oneincreasesthethoracic compartment space and improves lung compliance, thus facilitatingventilatorymechanics.Thecorrelationbetween theincreaseinERVanddecreasedwaistcircumference sup-portsthisrationale.18
18.9years)withsevereobesity,weighingbetween52.3and 192.2kg.
Overall, the quality of the selected studies was high, ranging between moderate19 and high methodological quality.17,18,20Forthisevaluation,weusedamodifiedscale to quantify observational studies.16 This scale has shown to be adequate for this type of design14 and evaluates theresearchquestion, thestudypopulation, the compari-sonofparticipants,exposuremeasures,statisticalanalysis, results,discussionandfunding.16Thestudiesincludedinthis reviewseemtohavesomelimitations,althoughitisbelieved thatsuchrestrictionsdidnotinfluencetheassessedresearch question,consideringthegoodmethodologicalqualitythat wasattained.
Some factorsloweredthe qualityscore of thestudies, suchas the absenceof sample calculation17---19 the power of analysis,17---19 the information regarding blinding in the quantificationofresults,18---20thecareregardingthepossible confoundingvariables17---20 andtheimpactofbiasesonthe results.17---20 As mostof thestudies included in thereview hadacross-sectional design,17,19,20 none of themassessed subjects for a period of follow-up, except for the study ofvandeGriendtetal.,18 whichanalyzed theeffectofa weightreduction programonpulmonary function parame-tersinobesechildrenandadolescents.Additionally,noneof thestudiesevaluatedtheeffectsofdose-responseandfew carriedoutmultivariatemodelsoranalyses,multiple com-parisontests17,18,20 and reportedfunding of the study.17,20 Theabovementioneditemsdirectlycollaboratedtoreduce thescoreintheassessedstudies.
In summary, the findings of this review demonstrate thedeleteriouseffectsof obesity onthe lungvolumeand capacityinchildren andadolescents,reducing mainlythe functionalresidualcapacity,expiratoryreservevolumeand residual volume. The results highlight the need to cre-atestrategiceffectivemeasurestofightchildhoodobesity throughintervention programstoprevent or mitigatethe negativeimpactofobesityonlungfunctioninthis popula-tion.
Funding
Thisstudydidnotreceivefunding.
Conflicts
of
interest
Theauthorsdeclarenoconflictsofinterest.
References
1.Ofei F. Obesity: a preventable disease. Ghana Med J. 2005;39:98---101.
2.Netto-Oliveira ER, Oliveira AA, Nakashima AT, Rosaneli CF, OliveiraFilhoAO, RechenchoskyL, etal. Sobrepesoe obesi-dade em crianc¸as de diferentesníveiseconômicos.Rev Bras CineantropomDesempenhoHum.2010;12:83---9.
3.OgdenCL,CarrollMD,KitBK,FlegalKM.Prevalenceof child-hoodandadultobesityintheUnitedStates,2011---2012.JAMA. 2014;311:806---14.
4.NiehuesJR,GonzalesAI,LemosRR,BezerraPP,HaasP. Preva-lence ofoverweightand obesity inchildren andadolescents
fromtheagerangeof2to19yearsoldinBrazil.IntJPediatr. 2014;2014:583207.
5.NgM,FlemingT,RobinsonM,ThomsonB,GraetzN,Margono C,et al. Global, regional, and nationalprevalence of over-weightand obesityin childrenandadultsduring1980---2013: asystematicanalysisfor theGlobalBurdenofDiseaseStudy 2013.Lancet.2014;384:766---81.
6.Prentice-DunnH,Prentice-DunnS.Physicalactivity,sedentary behavior, and childhood obesity: a review of cross-sectional studies.PsycholHealthMed.2012;17:255---73.
7.ParameswaranK,ToddDC,SothM.Alteredrespiratory physiol-ogyinobesity.CanRespirJ.2006;13:203---10.
8.RosenkranzSK,TownsendDK,SteffensSE,HarmsCA.Effectsof ahigh-fatmealonpulmonaryfunctioninhealthysubjects.Eur JApplPhysiol.2010;109:499---506.
9.Ferreira MS, Mendes RT, de Lima Marson FA, Zambon MP, PaschoalIA,ToroAA, et al.The relationshipbetween physi-calfunctionalcapacityandlungfunctioninobesechildrenand adolescents.BMCPulmMed.2014;14:199.
10.JonesRL,NzekwuMM.Theeffectsofbodymassindexonlung volumes.Chest.2006;130:827---33.
11.Fantuzzi G. Adipose tissue, adipokines, and inflammation. J AllergyClinImmunol.2005;115:911---9.
12.EisenmannJC,ArnallDA,KanuhoV,InterpretterC,CoastJR. ObesityandpulmonaryfunctioninNavajoand Hopichildren. EthnDis.2007;17:14---8.
13.Ulger Z, Demir E, Tanac¸ R, Göks¸en D, Gülen F, Darcan S, etal.Theeffectofchildhoodobesityonrespiratoryfunction testsandairwayhyperresponsiveness.TurkJPediatr.2006;48: 43---50.
14.TenórioLH,SantosAC,OliveiraAS,LimaAM,Brasileiro-Santos MS. Obesidade e testes de func¸ão pulmonar em crianc¸as e adolescentes: uma revisão sistemática. Rev Paul Pediatr. 2012;30:423---30.
15.MeloLC,SilvaMA, CallesAC.Obesidadeefunc¸ãopulmonar: umarevisãosistemática.Einstein(SãoPaulo).2014;12:120---5.
16.WestS,KingV,CareyTS,LohrKN,McKoyN,SuttonSF,etal. Systemsto ratethestrengthofscientificevidence. EvidRep TechnolAssess(Summ).2002:1---11.
17.Davidson WJ, Mackenzie-Rife KA, Witmans MB, Montgomery MD, Ball GD, Egbogah S, et al. Obesity negatively impacts lungfunctionin childrenand adolescents.Pediatr Pulmonol. 2014;49:1003---10.
18.Van de Griendt EJ, van der Baan-Slootweg OH, van Essen-Zandvliet EE, van der Palen J, Tamminga-Smeulders CL, BenningaMA,etal.Gaininlungfunctionafterweightreduction inseverelyobesechildren.ArchDisChild.2012;97:1039---42.
19.LiAM,ChanD,WongE,YinJ,NelsonEA,FokTF.Theeffectsof obesityonpulmonaryfunction.ArchDisChild.2003;88:361---3.
20.KongkiattikulL,Sritippayawan S,ChomthoS,Deerojanawong J, Prapphal N. Relationship between obesity indices and pulmonaryfunctionparametersinobeseThaichildrenand ado-lescents.IndianJPediatr.2015;82:1112---6.
21.Boran P, Tokuc G, Pisgin B, Oktem S, Yegin Z, Bostan O. Impactof obesity onventilatory function.JPediatr (Rio J). 2007;83:171---6.
22.BarretoS.Volumespulmonares.JBrasPneumol.2008;28Suppl. 3:S83---94.
23.Sociedade Brasileira de Pneumologia e Tisiologia. Dire-trizes para testes de func¸ão pulmonar. J Bras Pneumol. 2002;28:155---65.
24.MillerMR,CrapoR,HankinsonJ,BrusascoV,BurgosF,Casaburi R,etal.Generalconsiderationsforlungfunctiontesting.Eur RespirJ.2005;26:153---61.
25.SalomeCM,KingGG,BerendN.Physiologyofobesityandeffects onlungfunction.JApplPhysiol.2010;108:206---11.
andinductanceplethysmographyinhealthyBrazilian preschool-ers.PediatrPulmonol.2013;48:716---24.
27.SigulemDM,DevincenziMU,LessaAC.Diagnósticonutricional decrianc¸as.JPediatr(RioJ).2000;76Suppl.3:S275---84.
28.WHOMulticentreGrowthReferenceStudyGroup.WHOChild GrowthStandardsbasedonlength/height,weightandage.Acta PaediatrSuppl.2006;450:76---85.
29.DubernB,TounianP,MedjadhiN,MaingotL,GirardetJP,Boulé M.Pulmonaryfunctionandsleep-relatedbreathingdisordersin severelyobesechildren.ClinNutr.2006;25:803---9.
30.BottonJ,HeudeB,KettanehA,BorysJM,LommezA,Bresson JL,etal.Cardiovascularriskfactorlevelsandtheirrelationships withoverweightandfatdistributioninchildren:theFleurbaix LaventieVilleSantéIIstudy.Metabolism.2007;56:614---22.
31.BitsoriM,LinardakisM,TabakakiM,KafatosA.Waist circum-ferenceasascreeningtoolfortheidentificationofadolescents withthemetabolic syndromephenotype.IntJPediatrObes. 2009;4:325---31.
32.GlueckCJ,WooJG,KhouryPR,MorrisonJA,DanielsSR,WangP. Adolescentoligomenorrhea(age14---19)tracks intothe third
decade of life (age 20---28) and predicts increased cardio-vascular risk factors and metabolic syndrome. Metabolism. 2015;64:539---53.
33.Nathan BM, Moran A. Metabolic complications of obesity in childhoodandadolescence:morethanjustdiabetes.CurrOpin EndocrinolDiabetesObes.2008;15:21---9.
34.MorrisonJA,FriedmanLA, HarlanWR,HarlanLC,BartonBA, SchreiberGB,etal.Developmentofthemetabolicsyndrome inblackandwhiteadolescentgirls:alongitudinalassessment. Pediatrics.2005;116:1178---82.
35.Pereira PF,SerranoHM, CarvalhoGQ,LamounierJA, Peluzio MC, Franceschini SC, et al. Circunferência da cintura como indicadordegorduracorporalealterac¸õesmetabólicasem ado-lescentes:comparac¸ãoentrequatroreferências.RevAssocMed Bras.2010;56:665---9.