rev bras reumatol.2016;56(6):554–556
ww w . r e u m a t o l o g i a . c o m . b r
REVISTA
BRASILEIRA
DE
REUMATOLOGIA
Case
report
Livedoid
vasculopathy
夽
Vasculopatia
livedoide
José
Roberto
Provenza
a,
Lucas
Eduardo
Pedri
a,∗,
Gabriel
Mesquita
Provenza
baPontifíciaUniversidadeCatólicadeCampinas,HospitaleMaternidadeCelsoPierro,Servic¸odeReumatologia,Campinas,SP,Brazil
bPontifíciaUniversidadeCatólicadeCampinas,HospitaleMaternidadeCelsoPierro,Servic¸odeRadiologia,Campinas,SP,Brazil
a
r
t
i
c
l
e
i
n
f
o
Articlehistory:
Received18September2014 Accepted25September2015 Availableonline19March2016
Introduction
Livedoidvasculopathy(LV)isarecurrent,chronicandpainful skindisease,characterizedbylesionsthatariseaspunctateor lenticularpurple-coloredmaculesand/orpapulesoccurringin thelower limbs(lowerthirdofthelegsand ankles),which commonly progress to ulceration, and subsequently heal slowlyoverweeksormonths,givingrisetopearlyatrophic scars(whiteatrophy),punctatetelangiectasia,andbrownish pigmentation,accompaniedbyaracemouslivedo.1–3
Thedisease usuallysettles bilaterally inthe legs, often causingedemainthelowerthirdofthelimbs.Livedoid vascu-lopathymainlyaffectswomen(aboutthreewomenforevery man)between15and50(mean32)yearsold.2,3
Wereportacaseofafemalepatientwithlivedoid vascu-lopathy,withexcellenthealingoflowerlimbulcersafterusing ananti-TNFagent.
夽
StudyconductedatHospitalandMaternityCelsoPierro,PontifíciaUniversidadeCatólicadeCampinas,Campinas,SP,Brazil. ∗ Correspondingauthor.
E-mail:lucaspedri@hotmail.com(L.E.Pedri).
Case
report
Femalepatient,60,married,tradeswoman.Twelveyearsago, thispatientbeganaclinicalpictureofbilateralulcersinher legs and feet,accompaniedbycolor changes,withintense worseningincoldweather.Initially,thesuperficialulcerswere fewinnumber,withagradualincreaseintheirnumberand depth.Thepatienthadnoothersystemicand/orjoint com-plaint,nocomorbidities,andnofamilyhistoryofrheumatic disease.
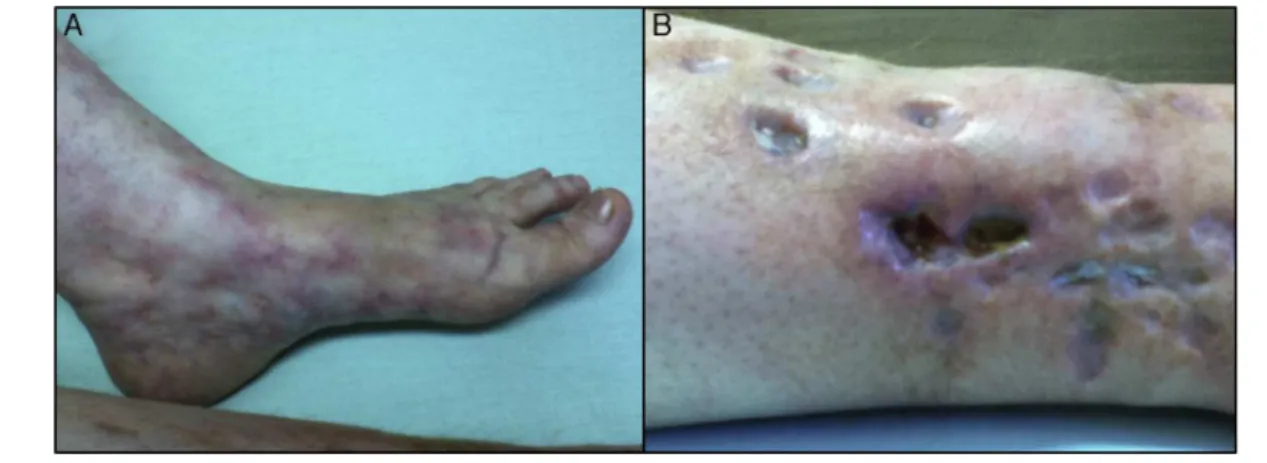
Onphysicalexamination,nochangeincardiac,pulmonary andmusculoskeletalsystemswasnoted.Thelowerlimbs(legs andfeet)presentedwithanintenselivedoracemosa(Fig.1), with multipleinfected, deepulcers showing destructionof subcutaneousfatandallowingmusclevisualization(Fig.1).
In 2010, the patient had already been treated with several doses of corticosteroids (20–60mg/day), with only
http://dx.doi.org/10.1016/j.rbre.2016.02.014
rev bras reumatol.2016;56(6):554–556
555
Fig.1–LivedoRacemosaonaleftfoot,andulcerationinrightleg.
slightimprovementandalwayswithrecurrentlesionsafter decreasingthedose.Shehadalsobeentreatedwitha com-binationofaspirin200mg/dayandpentoxifylline800mg/day, withnoclinicalimprovement.In2011,thepatientwastreated withmethotrexate15mg/weekinassociationwith corticoste-roids,buttonoavail.
Her lab work showed no change in blood count, renal function,liverfunctionandurinarysediment. The comple-mentproteins(C3and C4)werenormal; ANA1/320with a finespeckledpattern.Anti-DNA,anti-RNP,anti-Sm,anti-RO, anticardiolipin antibodies (IgM and IgG), lupus anticoagu-lant,rheumatoidfactor,andcryoglobulinswerenegative;ESR: 25mm, and CRP: 2.4mg/dL.Anulcer biopsy wasobtained, andthepathologicalexaminationdescribedocclusionof der-malbloodvessels,causedbydepositionofintravascularfibrin; andthrombosisassociatedwithsegmentalhyalinizationand endothelial proliferation, with the presence of a discrete perivascular inflammatory infiltrate, suggestive of livedoid vasculopathy/Milian’swhiteatrophy.
In2012,afterthefailureofmultipletreatments,a combi-nationoftheanti-TNFagentadalimumabandcorticosteroids wasinstituted,withasubsequentdecreaseofcorticosteroids. Ayearafterthistherapeuticregimen,thepatientshoweda significantimprovementofherlowerlimbulcers(Fig.2).
Discussion
Livedoidvasculopathyisadiseasewhosepathophysiologyis notwell understood.Thisfact reflectsthe manysynonyms forthisdisease,suchasMilian’swhiteatrophy,livedo vasculi-tis,segmentalhyalinizingvasculitis,livedoidvasculitis,livedo reticulariswithsummerulcers,andPURPLE(Purpuricpainful ulcerswithReticularPatternoftheLowerExtremities).1
Thisvasculopathy may beprimary orsecondary. In the first type, this condition is not associated with any other disease. On the other hand, the secondary form is com-monlyrelated tothrombophilia (factor V Leidenmutation, proteinC and/orS deficiency, hyperhomocysteinemia, pro-thrombingenemutation),andtoconnectivetissuediseases (SLE,cryoglobulinemia,APS).Therefore,inthefaceofa sus-picion of this diagnosis, it is important to start a clinical
Fig.2–Improvementofulcersandlivedoracemosainright legandfoot.
investigationofthepatientand his/herfamily,with partic-ular emphasisonhypercoagulablestatesandinflammatory diseases.1,4 Wesuggestedthe exclusion ofall those
condi-tionsthatmaydeterminepunch-like(“piecemeal”)reticulated ulcerationsanddifficult-tohealconditions;suchdisorderscan causestellate-likewhitishscars(i.e.,septicand leukocytoclas-ticvasculitides).2
Inadditiontoacompletephysicalexamination,the doc-torshouldrequestacompletebloodcount,coagulationtests, CRPlevels,fibrinogen,anti-nuclearfactor,anti-DNAantibody, rheumatoidfactor,antiphospholipidantibodies,and cryoglob-ulins.Inaddition,itisimportanttogetaDopplerultrasoundof lowerlimbs,withtheaimofdiscardingchronicvenousstasis.4
Withtheexceptionoffibrinogendosage,thepatientinthis studyobtainedresultsforalltestssuggested.
556
rev bras reumatol.2016;56(6):554–556primarilyinlatelesions,consistingofasecondaryevent.The thrombosisintothesevesselswouldoccurthroughmultiple changesinthecoagulationcascade–fromplatelet dysfunc-tion to a defect in the production of tissue plasminogen activator.1–5
Furthermore, the link between coagulation and inflam-mation has been investigated in cases of LV, taking into accountthatthrombinactivatesthosereceptorsactivatedby proteasetype1(which,ininflammatorycells,produce inflam-matorymediatorssuchasIL-6,IL-8,chemotacticsubstancesof monocytes,andadhesionmolecules)and,moreover,recruits leukocytestowardtheintravascularenvironment.1
Asnotedinthispatient’sbiopsy,inthehistological descrip-tion oflivedoidvasculopathyonecan observe occlusionof vesselsofthedermisthroughdepositionofintravascularfibrin andbyintraluminalthrombus,besidessegmental hyaliniza-tion and endothelial proliferation. The perivascular mixed inflammatory(neutrophilic atits onset,and then lympho-cytic)infiltratearisesataminimumdegree.Ingeneral,direct immunofluorescenceshowsdepositionofimmunoglobulins, fibrin,andcomponentsofcomplement.1–4
Largely duetoits uncertain pathogenesis,there isno a single effective treatment for this skin condition. Current treatmentoptionsarebasedonreportsofisolatedcases,or ofcaseseries.Mosttreatmentsaimtoimprovethephysical manifestationsandalleviatethepain.5
The therapeutic arsenal – described in the literature – consists of antiplatelet and anticoagulant agents, fib-rinolytic agents, vasodilators, phototherapy with PUVA, hyperbaric chamber, and immunosuppressants (corticoste-roids,cyclosporine,sulfasalazine,immunoglobulin).Allthese agentsare described in the literature,inattempts ofulcer treatment.5
Among antiplatelet drugs and hemorheologic agents, acetylsalicylicacidandpentoxifylline,respectively,havebeen successfullyusedinthetreatmentofLV,andtheirassociation isone ofthe mostcommonlyused therapeuticregimens.5
Yangetal.reportedthat13of27patientswithLVresponded to a combination of local care of wounds, rest, and low-doseaspirinincombinationwithdipiridamol.6Acasereport
described the successful treatment of LV associated with sickle cell trait with ASA.7 Sams et al. reported the use
of pentoxifylline in eight patients; in seven, a significant improvementofulcerationswasnoted.8Ourpatientdidnot
benefitfromthecombinationofthesetwodrugs.
Immunosuppressiveagentsare generallyusedfor recur-rent cases, such as rescue therapy.9 However, the use of
methotrexatewasnoteffectiveforourpatient.
Sheinbergetal.describedacaseofa38-yearoldfemale with LV refractory to treatment with anticoagulants and immunosuppressants, and who obtained a good response after the institution of rituximab. These authors reported that,inspiteofitsunknownetiology,LVcorrelatesstrongly
with immune complex diseases; and its histology shows consistentlyinflammatoryinfiltrates;itmaycomethatB lym-phocytes are involved inthe pathogenesisof this disease, butfurtherstudiesareneededtoclarifythispoint.10Inthis
report, we have succeeded in healing our patient’s ulcers aftertheuse ofadalimumab.Toourknowledge,this isthe firstreportdescribingthetreatmentofLVwithananti-TNF agent.
Tumor necrosisfactor (TNF) contributesto the develop-mentofthrombosis,becauseTNFstimulatestheexpressionof tissuefactorbyendothelialcells(i.e.anactivatorofthe extrin-siccoagulationpathway) andofthrombomodulin(apotent inhibitorofcoagulation).11Thus,adalimumab,whichisafully
humananti-tumornecrosisfactormonoclonalantibody,can reducetheformationofthrombiintodermalvessels,actively participatinginthepathophysiologyoflivedoidvasculopathy andprovidinganewperspectivetoitstreatment.
Conflicts
of
interest
Theauthorsdeclarenoconflictsofinterest.
r
e
f
e
r
e
n
c
e
s
1.HairstonBR,DavisMDP,PittelkowMR,AhmedI.Livedoid vasculopathy:furtherevidenceforprocoagulant pathogenesis.ArchDermatol.2006;142:1413–8. 2.CriadoPR,RivittiEA,SottoMN,ValenteNYS,AokiV,de
CarvalhoJF,etal.Vasculopatialivedoide:umadoenc¸a cutâneaintrigante.AnBrasDermatol.2011;86:961–77. 3.ZaniniM,BertinoD,WulkanC,ItoL.Vasculiteou
vasculopatialivedoide?AnBrasDermatol.2003;78:755–7. 4.KheniferS,ThomasL,BalmeB,DalleS.Livedoid
vasculopathy:thromboticorinflammatorydisease.ClinExp Dermatol.2009;35:693–8.
5.Gonzalez-SantiagoTM,DavisMDP.Updateofmanagementof connectivetissuediseases:livedoidvasculopathy.Dermatol Ther.2012;25:183–94.
6.YangLJ,ChanHL,ChenSY,KuanYZ,ChenMJ,WangCN,etal. Atrophieblanche.Aclinicopathologicalstudyof27patients. ChanggengYiXueZaZhi.1991;14:237–45.
7.ElKhouryJ,TaherA,KurbanM,KibbiAG,AbbasO.Livedoid vasculopathyassociatedwithsicklecelltrait:significant improvementonaspirintreatment.IntWoundJ.2012;9:344–7. 8.SamsWMJr.Livedovasculitis.Therapywithpentoxifylline.
ArchDermatol.1988;124:684–7.
9.PolettiED,SandovalNRM,GonzálezJLM,TorresAS. Vasculopatíalivedoide:significadoactual.Comunicaciónde doscasos.DermatologíaRevMex.2008;52:175–81.
10.ZeniP,FingerE,ScheinbergMA.Successfuluseofrituximab inapatientwithrecalcitrantlivedoidvasculopathy.Ann RheumDis.2008;67:1055–6.
11.AbbasAK,LichtmanAH,PillaiS.Imunologiacelulare molecular.7a