Offi cial Publication of the Brazilian Society of Anesthesiology www.sba.com.br
REVISTA
BRASILEIRA DE
ANESTESIOLOGIA
Abstract
Background and objectives: Vaginal birth delivery may result in acute and persistent perineal pain postpartum. This study evaluated the association between catastrophizing, a phenomenon of poor psychological adjustment to pain leading the individual to magnify the painful experience making it more intense, and the incidence and severity of perineal pain and its relationship to perineal trauma.
Method: Cohort study conducted with pregnant women in labor. We used the pain catastrophizing scale during hospitalization and assessed the degree of perineal lesion and pain severity in the fi rst 24 hours and after 8 weeks of delivery using a numerical pain scale.
Results: We evaluated 55 women, with acute pain reported by 69.1%, moderate/severe pain by 36.3%, and persistent pain by 14.5%. Catastrophizing mean score was 2.15 ± 1.24. Catastrophizing patients showed a 2.90 relative risk (RR) for perineal pain (95% CI: 1.08-7.75) and RR: 1.31 for developing persistent perineal pain (95% CI: 1.05-1.64). They also showed a RR: 2.2 for developing acute and severe perineal pain (95% CI: 1.11-4.33).
Conclusions: The incidence of acute and persistent perineal pain after vaginal delivery is high. Catastrophizing pregnant women are at increased risk for developing acute and persistent perineal pain, as well as severe pain. Perineal trauma increased the risk of persistent perineal pain. © 2013 Sociedade Brasileira de Anestesiologia. Published by Elsevier Editora Ltda. All rights reserved.
Association of Pain Catastrophizing with the Incidence
and Severity of Acute and Persistent Perineal Pain after
Natural Childbirth: Longitudinal Cohort Study
Anne Danielle Santos Soares
1, Tânia Cursino de Menezes Couceiro*
2, Luciana Cavalcanti Lima
3,
Fernanda Lobo Lago Flores
4,
Eusa Maria Belarmino Alcoforado
5, Roberto de Oliveira Couceiro Filho
61. Anesthesiologist, Instituto de Medicina Integral Professor Fernando Figueira (IMIP), Recife, PE, Brazil 2. Holder of Superior Title in Anesthesiology (TSA); Master in Neuroscience, Universidade
Federal de Pernambuco, Recife; Coordinator, IMIP, Recife, PE, Brazil
3. PhD in Anesthesiology, Universidade Estadual Paulista Júlio de Mesquita Filho, São Paulo; Professor & Coordinator, Faculdade Pernambucana de Saúde, Recife, PE, Brazil
4. Resident, IMIP, Recife, PE, Brazil
5. TSA; MD, Assistant Physician of Ministry of Health Hospitals, Brazil 6. TSA; Anesthesiologist
Received from Instituto de Medicina Integral Professor Fernando Figueira, Recife, PE, Brazil.
Received on April 11, 2012. Approved on December 5, 2012.
Keywords: Acute Pain; Catastrophization; Natural Childbirth; Obstetric Surgical Procedures; Pain Measurement; Perineum.
SCIENTIFIC ARTICLE
*Corresponding author: Tânia Cursino de Menezes Couceiro, Instituto de Medicina Integral Professor Fernando Figueira. Departamento de Anestesiologia. Rua dos Coelhos 300, Recife, PE, Brasil. CEP: 50070-550.
E-mail: taniacouceiro@yahoo.com.br
Introduction
Childbirth is a natural process that may result in maternal
morbidity for a long period of time 1. According to the
litera-ture, 87-94% of women report some health problems in the
fi rst three months after delivery 2. Acute perineal pain is a
major problem affecting 57-92% of postpartum women 3-6.
Its incidence is related to several factors, including parity, duration of active expulsion period, degree of perineal
trau-ma, type of suture used, and episiotomy 6,7,8. The severity
of acute pain is related to a relative risk (RR) 2.5 higher for developing chronic pain and RR: 3.0 for postpartum depres-sion, regardless of the type of delivery (vaginal or cesarean
section) 1,9. Recent studies have evaluated the relationship
between catastrophizing pain during labor and severity of acute perineal pain, incidence of postpartum depression,
and ability to recover after childbirth 4,10. Originally,
resear-chers studied catastrophizing in patients with chronic pain,
but its infl uence on labor remains open to further research4.
In this study, we evaluated the association of catastrophizing pain during labor and perineal trauma with the incidence and severity of acute and persistent perineal pain.
Method
After approval by the Ethics and Research Committee and obtaining written informed consent from all participants or guardians, we conducted a longitudinal cohort study at the Obstetric Center of the Instituto de Medicina Integral Professor Fernando Figueira (IMIP), Recife (PE), between June 2010 and October 2011. We collected at two times: during hospitalization for childbirth and 8 weeks after delivery, by
telephone. Participants were low-risk women, age over 16 years, admitted in labor, whose fetuses were born via spon-taneous vaginal delivery. Exclusion criteria were women with previous perineal disease and those who, after inclusion, did not understand the explanation of the scales used or did not respond to telephone calls for persistent pain evaluation. In total, 127 women agreed to participate in the study. Of these, 97 met the inclusion criteria and participated in the fi rst phase of data collection. However, only 55 responded to the second contact via phone.
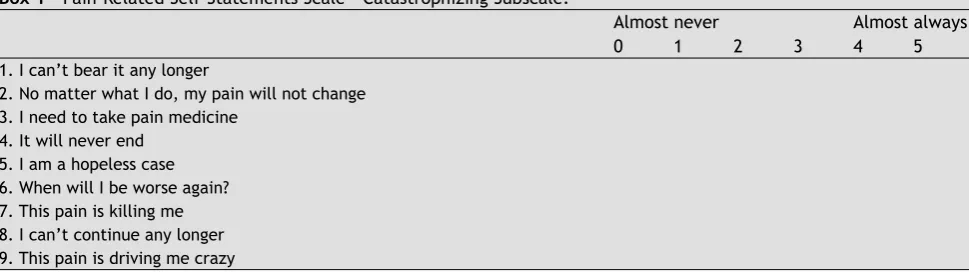
We chose to apply the Pain-Related Self-Statements
Scale – Catastrophizing Subscale (PRSS-Catastrophizing) 11
to measure catastrophizing pain due to its simplicity as it is composed of only nine items listed on a Likert scale with a score ranging from zero (almost never) to 5 (almost always) points (Box 1). The total score is the sum of the items divided by the number of items answered, in which the higher scores indicate greater catastrophic thinking in a self-administered questionnaire. We applied this scale, which was validated
in Portuguese 12, to the study participants during
hospitali-zation. We considered labor pain as the painful experience (Table 1).
Pain severity was evaluated at two-time periods using the Numerical Pain Scale. Participants were asked to quan-tify a value for their pain (0 = no pain, 10 = worst pain
imaginable) 15,16. The fi rst evaluation occurred within 24
hours after delivery and pain was classifi ed as acute. The second evaluation was conducted by phone 8 weeks after delivery, and pain was classifi ed as persistent, if present. For statistical analysis, pain was categorized as mild (≤ 3), moderate (4-7), and severe (> 7). The service protocol for postpartum analgesia (natural childbirth) was maintained for
Box 1 – Pain-Related Self-Statements Scale – Catastrophizing Subscale.
Almost never Almost always
0 1 2 3 4 5
1. I can’t bear it any longer
2. No matter what I do, my pain will not change 3. I need to take pain medicine
4. It will never end 5. I am a hopeless case 6. When will I be worse again? 7. This pain is killing me 8. I can’t continue any longer 9. This pain is driving me crazy
Table 1 - Incidence and Severity of Acute and Persistent Perineal Pain.
Incidence Acute Perineal Pain (%) Persistent Perineal Pain (%)
Absent 17 (31%) 47 (85.5%)
Present 38 (69%) 8 (14.5%)
Total 55 (100%) 55 (100%)
Severity Acute Perineal Pain (%) Persistent Perineal Pain (%)
Mild 18 (47.3%) 6 (75%)
Moderate 19 (50%) 2 (25%)
Severe 1 (2.6%)
319 Natural Childbirth: Longitudinal Cohort Study
the participants, and consisted of oral analgesics (dipyrone or paracetamol) or anti-infl ammatory non-steroidal drugs (NSAIDs), if necessary.
The obstetrician or obstetric nurse who conducted the delivery assessed the degree of perineal trauma, based on a specifi c annex previously presented to the laboring women. The classifi cation used considered the following degrees of trauma: intact perineum, which corresponds to the absence of injury; fi rst degree injury, which involves the skin around the vaginal opening; second degree injury, which involves the vaginal mucosa and perineal muscles; third degree injury, which involves the anal sphincter, in addition to vaginal mucosa and perineal muscles; fourth degree injury, which involves the third degree injury affected tissues and the rectum wall.
For data analysis, we used Epi Info software, version 3.5.3. The outcomes were considered statistically signifi cant when p < 0.05.
Results
The sample consisted of 55 women, mean age 25 ± 5.6 years, with an average education of 10 ± 2 years. Patients with more than 11 years schooling were attending college and consti-tuted 18% of the sample. The mean number of pregnancies was equal to two per participant.
Regarding the occurrence of pain, 69.1% of participants reported pain in the fi rst 24 hours after delivery and 14.5% reported persistent pain after 8 weeks of delivery. Among the patients who reported pain, 52.6% rated it as moderate to severe in the fi rst 24 hours (Table 1).
Regarding the occurrence of perineal injury, 80% of patients had some degree of injury. Only two patients un-derwent episiotomy (Table 2).
The mean score on the scale of catastrophic thinking about pain was 2.15 ± 1.24, and a median of 2.11 was used as the cut-off point for inclusion (or not) of patients in the catastrophizing group. We observed that catastrophizing patients have a relative risk (RR) equal to 2.90 (95% CI: 1.08-7.75) to present with acute perineal pain and a RR of 1.31 (95% CI: 1.05-1.64) to develop persistent pain. We also observed among catastrophizing patients a risk 2.2 higher to develop more severe pain in the fi rst 24 hours (95% CI: 1.11-4.33) (Table 3).
As for perineal trauma, we found that the presence of trauma was not signifi cantly related to increased risk of acute perineal pain. However, in patients with perineal trauma, the risk of persistent pain is 1.15 higher. The relationship between perineal trauma and severity of pain was not sta-tistically signifi cant (Table 4).
Table 2 - Incidence and Degree of Perineal Injury.
Perineal Injury Incidence
Absent (16.4%)
Present 44 (80%)
Episiotomy 2 (3.6%)
Total 55 (100%)
Degree of injury Incidence
1st degree 31 (10.3%)
2nd degree 13 (29.7%)
3rd degree 44 (100%)
Table 3 – Association between Pain Catastrophizing, Incidence, and Severity of Acute and Persistent Perineal Pain. Acute Perineal
Pain P value
Without pain (%)
With pain (%)
Mild (%)
Moderate/severe (%)
Non-catastrophizing 13 (76.5%) 15 (41.7%) RR = 2.90 11 (61.1%) 4 (22.2%)
Catastrophizing 4 (23.5%) 21 (58.3%) (95%CI: 1.8-7.75) 7 (38.9%) 14 (77.8%) 0,01 Persistent Perineal
Pain
Without pain (%)
With pain (%)
Mild (%)
Moderate/severe (%)
Non-catastrophizing 28 (59.6%) 0 RR = 1.31 0 0
Catastrophizing 19 (40.4%) 6 (100%) (95%CI: 1.05-1.64) 5 (100%) 1 (100%) 0,022 Values expressed as number (percent); RR: relative risk; CI: confi dence interval.
Incidence Severity
Discussion
In our sample, 69% of patients presented acute pain after childbirth, an incidence similar to that described in the
literature (57-92%) 1,6,9. The incidence of persistent perineal
pain was 14.5%, which is higher than that reported in the
literature (9.7-10%) 6,9,15. However, when we exclude the
patients who underwent episiotomy, the incidence is simi-lar to those already published (10.8%). Patients undergoing episiotomy were excluded from the analysis assessing the relationship between catastrophizing and perineal pain, as there is strong evidence that episiotomy is a risk factor for
perineal pain 6,7, which could act as a confounding variable
in this study.
We found that about 70% of patients had acute pain and, of these, 52.6% reported moderate to severe pain. This indi-cates that postpartum pain is not being managed properly, which is due to the fact that the institutional protocol only contemplates treatment for mild pain. This fi nding indicates the need for reevaluation of this protocol.
Our study found no signifi cant relationship between pe-rineal trauma and acute pain. The severity of pain differed from a previous study that reported positive association between the degree of trauma and severity of perineal
pain after vaginal delivery 7. This can be explained by the
following reason: although we found a high incidence of
perineal trauma (80%), the degree of injury was low (1st and
2nd), which probably contributed to the lack of relationship
between the degree of trauma and severity of perineal pain in the outcomes. The prevalence of low-grade lesions may simply refl ect the reality of the data collection place: a cen-ter offering humanized and spontaneous birth services, with low incidence of episiotomy, provided by obstetric nurses for low-risk women, so that the patients who progressed to assisted vaginal delivery (with the use of forceps) or showed some distorted progression were taken to the high risk unit and excluded from data analysis.
As for catastrophic thoughts, considering its impor-tance as a disability and stress arising from the painful stimulus, several measures have been developed to assess this construct. The most frequently used tools are the Catastrophizing Scale of the Coping Strategies Questionnaire
(CSQ) 16, Pain Catastrophizing Scale (PCS) 17, and Pain-Related
Self-Statements Scale – Catastrophizing Subscale
(PRSS-Catastrophizing) 11, which have no cut-off points 12,18. The
latter was the scale used in this study. In an initial validity
study 19, the mean score was 2.03 ± 1.22. The mean score
of our sample was 2.15 ± 1.24, and a median of 2.11 was used as cut-off point for inclusion (or not) of patients in the catastrophizing group. Although there are no cut-off points for this scale, we chose to use the median score to classify catastrophizing and non-catastrophizing patients in an at-tempt to improve and facilitate the understanding during data analysis. This strategy was adopted in previous studies
using the PCS 4, which also has no cut-off points, although
in the original validation study, the author has used the scores that limited the upper and lower third distribution
of the PCS scores of his sample 17. In our study, we found
that catastrophizing patients have a 2.9 higher risk for acute perineal pain and 1.31 risk for developing persistent perineal pain. Although catastrophizing was not originally described as a predictor of pain, it seems to be particularly important to predict the occurrence of acute pain. In line with the fi ndings of Flink who, comparing catastrophizing with non-catastrophizing patients, found that the catas-trophizing patients experienced more severe pain up to
one month after childbirth (p < 0.0125) 4, in our study, we
found that these patients have a 2.2 higher risk of presen-ting more severe pain in the fi rst 24 hours. We also found a statistically signifi cant relationship between catastrophizing and persistent pain severity (p < 0.023), which corroborates the fi ndings of previous studies assessing chronic pain and reporting that catastrophizing patients are more likely to
experience more severe pain 17,18,19. Given these fi ndings, we
suggest the identifi cation of catastrophizing pregnant women during prenatal and the development of interventions to improve these patients’ adaptation to postpartum pain. One option that has been successfully used in other populations is cognitive behavioral therapy. However, further studies are needed to evaluate the effectiveness of this therapy to
prevent pain in women 4,18.
This study has limitations that should be discussed. First, some factors that could infl uence the incidence of perineal pain after childbirth, such as fetal weight at birth Table 4 – Association between Perineal Trauma and Acute and Persistent Perineal Pain.
Acute Perineal Pain
Trauma Without pain (%) With pain (%)
Absent 3 (17.6%) 6 (16.7%)
Present 14 (82.4%) 30 (83.3%) RR = 1.04 (95% CI: 0.37-2.9)
Persistent Perineal Pain
Trauma Without pain (%) With pain (%)
Absent 9 (19.1%)
-Present 38 (80.9%) 6 (100%) RR = 1.15 (95% CI: 1.02-1.3)
321 Natural Childbirth: Longitudinal Cohort Study
and delivery duration, were not evaluated. However, these factors are indirectly related to perineal trauma, which we analyzed. Second, the catastrophic thoughts scale used in this study is self-administered, which could hinder unders-tanding and cooperation by the participants. To minimize this fact, the investigator administered and later verbally confi rmed the scale.
With this study, we conclude that there is a high inciden-ce of acute and persistent perineal pain after spontaneous vaginal delivery. Catastrophizing pregnant women seem to have a higher risk of developing acute, persistent, and se-vere perineal pain. First-degree perineal trauma discreetly increased the risk of persistent perineal pain. Further studies are needed to identify the best strategy to support catas-trophizing patients postpartum and for better understanding the role of catastrophizing in the incidence and severity of acute pain.
References
1. Eisenach JC, Pan PH, Smiley R, Lavand’homme P et al. - Severity of acute pain after childbirth, but not type of delivery, predicts persistent pain and postpartum depression. Pain, 2008;140:87-94.
2. Borders N - After the afterbirth: a critical review of postpartum health relative to method of delivery. J Midwifery Womens Health, 2006;51:242-248.
3. Olofsson N. Labor pain and the treatment. Lund: Studentlitteratur, 2003.
4. Flink IK, Mroczek MZ, Sullivan MJL et al. - Pain in childbirth and postpartum recovery. The role of catastrophizing. Eur J Pain, 2009;13:312-316.
5. Andrews V, Thakar R, Sultan AH et al. - Evaluation of postpartum perineal pain and dyspareunia. A prospective study. Eur J Obstet Gynecol Reprod Biol. 2008;137:152-156.
6. Leeman L, Fullilove AM, Borders N et al. - Postpartum perineal pain in a low episiotomy setting: association with severity of genital trauma, labor care, and birth variables. Birth, 2009;36:283-288.
7. Macarthur AJ, Macarthur C - Incidence, severity, and determinants of perineal pain after vaginal delivery: a prospective cohort study. Am J Obstet Gynecol, 2004;191:1199-1204.
8. Fernando RJ, Sultanb AH - Risk factors and management of obstetric perineal injury. Curr Obstet Gynaecol. 2004;14:320-326.
9. Lavand’homme P - Chronic pain after vaginal and cesarean delivery: a reality questioning our daily practice of obstetric anesthesia. Int J Obstet Anesth, 2010;19:1-2.
10. Ferber SG, Granot M, Zimmer EZ - Catastrophizing labor pain compromises later maternity adjustments. Am J Obstet Gynecol, 2005;192:826-831.
11. Flor H, Behle DJ, Birbaumer N - Assessment of pain – Related cognitions in chronic pain patients. Behav Res Ther, 1993;31:63-73.
12. Junior JS, Nicholas MK, Pereira IA et al. - Validação da escala de pensamentos catastrófi cos sobre dor. Acta Fisiatr, 2008;15:31-36.
13. Marquié L, Duarte LR, Mariné C et al. - How patients and physicians rate patients’ pain in a French emergency department using a verbally administered numerical rating scale and a visual analog scale. Acute Pain, 2008;10:31-37.
14. Pitangui ACR, Sousa L, Ferreira CHJ et al. - Mensuração e características da dor perineal em primíparas submetidas à episiotomia. Acta paul. Enferm. 2009;22:77-82.
15. Eisenach JC, Pan PH, Smiley R et al. - Severity of acute pain after childbirth, but not type of delivery, predicts persistent pain and postpartum depression. Pain, 2008;140:87-94. 16. Rosenstiel AK, Keefe FJ - The use of coping strategies in chronic
low back pain patients: relationship to patient characteristics and current adjustment. Pain, 1983;17:33-44.
17. Sullivan MJL, Bishop SR, Pivik J - The Pain Catastrophising Scale: development and validation. Psychol Assess, 1995;7:524-32. 18. Sullivan MJ, Thorn B, Haythornthwaite JA et al. - Theoretical
perspectives on the relation between catastrophizing and pain. Clin J Pain, 2001;17:52-64.