REVISTA
BRASILEIRA
DE
ANESTESIOLOGIA
PublicaçãoOficialdaSociedadeBrasileiradeAnestesiologiawww.sba.com.br
SCIENTIFIC
ARTICLE
Two-year
experience
with
cell
salvage
in
total
hip
arthroplasty
Mehmet
I.
Buget
a,∗,
Fatih
Dikici
b, ˙Ipek
S.
Edipo˘
glu
a,
Eren
Yıldız
b,
Natig
Valiyev
b,
Suleyman
Kucukay
aaDepartmentofAnesthesiology,IstanbulUniversity,IstanbulMedicalFaculty,Istanbul,Turkey
bDepartmentofOrthopedicsandTraumatology,IstanbulUniversity,IstanbulMedicalFaculty,Istanbul,Turkey
Received10August2014;accepted11September2014 Availableonline6March2015
KEYWORDS
Cellsalvage; Hiparthroplasty; Autologtransfusion
Abstract
Backgroundandobjective: The aimofthis study was to determinethe efficacy of thecell salvagesystem intotal hip arthroplastysurgeries andwhether the cellsalvagesystem can reducetheallogeneicbloodtransfusionrequirementintotalhiparthroplastypatients. Methods:We reviewed retrospectively the medicalrecords of patients who underwent hip arthroplastysurgeriesbetween2010and2012inauniversityhospital.Atotalof181arthroplasty patientswereenrolledinourstudy.
Results:Inthecellsalvagegroup,themeanperioperativerateofallogeneicbloodtransfusion wassignificantlylower(92.53±111.88mL)thanthatinthecontrolgroup(170.14±116.79mL; p<0.001).Whenthemeanpostoperative transfusionrateswerecompared,thecellsalvage group had lower values (125.37±193.33mL) than the control group (152.22±208.37mL), althoughthedifferencewasnotstatisticallysignificant.Thenumberofpatientsreceiving allo-geneicbloodtransfusionintheCSgroup(n=29;43.2%)wasalsosignificantlylowerthancontrol group(n=56;73.6%;p<0.05).Inthelogisticregressionanalysis,perioperativeamountof trans-fusion,oddsratio(OR)−4.257(95%CI−0.502to0.184)andoperationtime,OR:2.720(95%CI 0.001---0.004)wereindependentriskfactorsfortheusageofcellsalvagesystem.
Conclusion:Cell salvageisaneffective strategyfor reducing theneedfor allogeneicblood transfusionintheperioperativesetting;itprovidessupporttopatientbloodmanagement inter-ventions.Thus,werecommendthecellsalvagesystemforuseintotalhiparthroplastysurgeries toreducetheneedforallogeneicbloodtransfusion,ifpossible.
©2015SociedadeBrasileiradeAnestesiologia.PublishedbyElsevier EditoraLtda.Allrights reserved.
∗Correspondingauthor.
E-mail:mbuget@yahoo.com(M.I.Buget).
http://dx.doi.org/10.1016/j.bjane.2014.09.009
PALAVRAS-CHAVE
Recuperac¸ão intraoperatóriade sangue;
Artroplastiado quadril;
Sistemadetransfusão autólogo
Doisanosdeexperiênciacomrecuperac¸ãointraoperatóriadesangueemartroplastia
totaldoquadril
Resumo
Justificativaeobjetivo: Oobjetivodesteestudofoideterminaraeficáciadosistemade res-gatecelularemartroplastiatotaldequadrileseosistemaderecuperac¸ãointraoperatóriade sanguepodereduziranecessidadedetransfusãodesanguealogênicoempacientessubmetidos àartroplastiatotaldequadril.
Métodos: Análise retrospectiva dos prontuários de pacientes submetidos a cirurgias de artroplastiadequadrilentre2010e2012emumhospitaluniversitário.Nototal,181pacientes submetidosàartroplastiaforaminscritosnoestudo.
Resultados: A média da taxa de transfusão de sangue alogênico no período perioper-atório foi significativamente inferior no grupo de recuperac¸ão intraoperatória de sangue (92,53±111,88mL)quenogrupocontrole(170,14±116,79mL;p<0,001).Quandoasmédias dastaxasdetransfusãonopós-operatórioforamcomparadas,ogrupoderecuperac¸ão intra-operatóriade sangueapresentou valores inferiores(125,37±193,33mL)aosdogrupo cont-role(152,22±208,37mL),emboraadiferenc¸anãotenhasidoestatisticamentesignificativa.O númerodepacientesquerecebeutransfusãodesanguealogêniconogrupoRC(n=29;43,2%) tambémfoisignificativamenteinferioraodogrupocontrole(n=56;73,6%;p<0,05).Naanálise deregressãologística,aquantidadedetransfusãonoperíodoperioperatório,arazãodechance (OR)---4,257(95%CI---0,502---0,184)eotempocirúrgico,OR:2,720(IC95%0,001-0,004)foram fatoresderiscoindependentesparaousodesistemaderesgatecelular.
Conclusão:A recuperac¸ãointraoperatóriade sangueéuma estratégiaeficaz para reduzir a necessidadedetransfusãodesanguealogêniconoperíodoperioperatório,queauxilianomanejo sanguíneoduranteasintervenc¸ões.Portanto,recomendamososistemaderecuperac¸ão intra-operatóriadesangueparausoemartroplastiatotaldequadrilparadiminuiranecessidadede transfusãodesanguealogênico,quandopossível.
©2015SociedadeBrasileira deAnestesiologia.PublicadoporElsevierEditoraLtda.Todosos direitosreservados.
Introduction
Considerable blood loss is a frequent problemin patients undergoing major orthopedic surgery. Particularly for arthroplasty surgeries, allogeneic red cell transfusion is often necessary.1 However, the probability of
transi-tion of a wide variety of viral diseases such as those
caused by hepatitis B and C, human immunodeficiency
virus, transmission-transmitted virus, West Nile virus,
Cytomegalovirus, Epstein---Barr virus, as well as variant
Creutzfeldt---Jakob disease, bacterial contamination, and
sepsis are a concern for allogeneic blood transfusion
(ABT).2,3Theincidenceoftransfusion-transmitteddiseases
decreased to very low levels in many countries with the
modern laboratory techniques (nucleic acid testing)
dur-ingthepastyears,butABTstillhasconsiderableriskssuch ascardiacoverload, transfusion-relatedacutelung injury,
and transfusion-related immunomodulation. Medical staff
weldedincorrectbloodtransfusion,ABO-Rhmismatch,and
allergic reactions also as serious causes of morbidity and mortality.4 Although the risks for transfusion-transmitted
diseases decreased to a very low level in the developed
countries,manydevelopingcountrieswheretransfusion ser-vicesareinsufficientstillexperienceahigh prevalenceof suchinfections.5Meanwhile, for thedeveloped countries,
themajorconcernforABTisthefinancialcostofproviding andpreservingasafebloodproductratherthan transfusion-relatedinfectiousdiseases.5
Consequently, to reduce the need for ABT, different
methods are established, including preoperative
autolo-gousblood donation, normovolemic hemodilution, iron or
erythropoietinbasedpatientblood management, andcell
salvage(CS)systems.1,6,7CSistheprocessofcollectingand
reinfusing autologousblood.8 Itsmain targetis to reduce
and,ifpossible, eliminate theneed for ABT and diminish
probableinfectiousandnoninfectiouscomplications.9
The aim of this study was to examine the records of
patients who had the CS system used in their total hip
arthroplasty(THA)surgeryandcomparethemwithpatients
operated without the CS system. In addition, we
investi-gatediftheCSmethodcandecreasetheneedforABTs.
Methods
This study was conducted with the approval of the local
Ethical Committee under approval no. 2013/14, dated
27/12/2012.Wesearchedthedatabaseofthemedical
fac-ultyandretrospectivelyevaluatedpatientsoperatedinthe DepartmentofOrthopedicsandTraumatology.Atotalof181 THApatientswereenrolledinourstudy.Ofthepatients,38 wereexcludedfromthestudybecausetheirmedicalrecords
indicated hematological problems that met our exclusion
181 arthroplasties
143 patients enrolled 38 patients excluded
67 patients cell salvage group
30 patients perop transfusion 76 patients control group
13 patients both perop and postop transfusion
16 patients perop transfusion 13 patients
postop transfusion 26 patients both perop
and postop transfusion
12 patients postop transfusion
Figure1 Flowchartofpatients.
We reviewed retrospectively the medical records of
thepatients who had hiparthroplasty operation between
2010 and 2012. We excluded study patients with records
of a known history of hematological diseases, bleeding
conditions,or thromboembolicevents.Lowplateletcount
(plt=100.000) and any escalation in international
nor-malized ratio (INR>1.2) were also defined as exclusion
criteria. In our institution, we use CS system (Medtronic
Autolog,Medtronicinc.Minneapolis,USA)whensignificant
blood lossis estimated or preoperative anemia is present
(Hgb<10g/dL).Wedividedourpatientsinto2groups.One groupconsistedofpatientsforwhomtheCSsystemwasused
duringthe perioperative setting. CSsystem was not used
beforethe surgeryfor anypatientin anygroup.The
con-trolgroupconsistedofpatientsinwhomtheCSsystemwas notusedtheiroperation.Thetransfusionthresholdis8g/dL forhealthyadultsinourinstitutionandbetween8g/dLand 10g/dLforpatientswithseverecardiacdisease,andsevere co-morbidities.
Demographic data, preoperative hemoglobin level,
hematocrit and leukocyte values, amount of blood for
autologous transfusion during and after the surgery were
recorded.Hemoglobinlevel, hematocrit values,leukocyte
valuesat discharge, highest body temperature duringthe
postoperative period,and C-reactive protein (CRP) levels
werenoted for both groups. ABTs werealso recorded for
the2groups.
Statistical
analysis
Statistical analysis was performed using a computer
pro-gramNCSS(NumberCruncherStatisticalSystem)2007&PASS (PowerAnalysisandSampleSize)2008StatisticalSoftware (NCSSLLC,Kaysville,Utah,US).Descriptivestatistical meth-odswereused(mean,median,ratioandstandarddeviation)
toevaluatethestudydata.Independentsamplestestwas
used to compare normally distributed variables between
groups.MannWhitneyUtestwasusedforordinalvariables andchi-squaretestwasusedfornominaldata.For multivari-ateevaluations,enterlogisticregressionanalysiswasused. Ap-value<0.05wasconsideredasstatisticallysignificant.
Results
Therewere67patientsintheCSgroupand76patientsinthe controlgroup(Fig.1).IntheCSgroup,41patients(61.1%) receivedABT,and69patients(90.7%)inthecontrolgroup hadABT(preoperative,postoperative,orboth).
In terms of sex, type of anesthesia, and age, we did
not detect any significant difference between the groups
(Table1).Femalepatientsaccountedfor46patients(68.7%) intheCSgroupand56(73.7%)inthecontrolgroup.The per-centagesofneuroaxialandgeneralanesthesiausedintheCS
group(52.3%and47.7%, respectively)wereclosetothose
usedinthecontrolgroup(51.3%and48.7%,respectively).
Themeanagewas55.82±13.20yearsintheCSgroupand
57.82±13.43yearsinthecontrolgroup.Operationtime sig-nificantlydifferedbetweenthegroups;thatis,surgerytime waslongerintheCSgroup(152.72±55.08min)thaninthe controlgroup(130.13±40.71min)(p<0.05).
In the CS group, the mean amounts of
perioper-ative allogeneic blood transfused were significantly
lower (92.53±111.88mL) than that in the control group
(170.14±116.79mL; p<0.001). When comparing the
mean postoperative transfusion rates, the CS group
(125.37±193.33mL) had lower values than the control
group (155.22±208.37mL), although the difference was
notsignificant.Thenumberofpatientsreceivingallogeneic
Table1 Patients’demographicdata.
Cellsalvagegroup (n=67)
Controlgroup (n=76)
p-value
Sexa
Male 21(31.3%) 20(26.3%) >0.05
Female 46(68.7%) 56(73.7%)
Typeofanesthesiaa
Neuroaxial 35(52.3%) 39(51.3%) >0.05
General 32(47.7%) 37(48.7%)
Age(mean±SD)yearsb 55.82±13.20 57.82±13.43 >0.05
Operationtime(mean±SD)minb 152.72±55.08 130.13±40.71 0.016c
NS,nosignificant. a Chisquaretest.
b Independentsamplestest.
c p-value<0.05statisticallysignificant.
also significantly lower than control group (n=56; 73.6%;
p<0.05)(Table2).
DuringtheoperationofthepatientsintheCSgroup,the
meanamountofblood transfusedfromtheCSsystemwas
333.61±170.99mL.Themeanpreoperativehemoglobinand
hematocritvaluesdidnotdiffersignificantlyfromthevalues atdischargeinbothgroups(Table3).
The meanCRP level, postoperative body temperature,
and preoperative leukocyte levels did not show any
sig-nificantdifference. Thepostoperativeleukocytelevelwas a little higher, though not significantly, in the CS group (Table4).
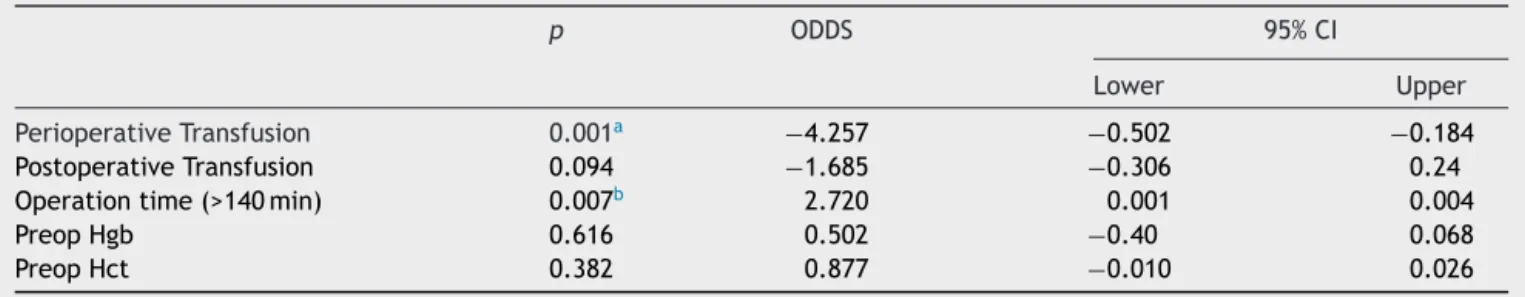
We evaluatedthe effects ofvariables for the usageof
autologousbloodtransfusionwithenterslogisticregression
analysis.Variables evaluatedwereoperation time,
preop-erative hemoglobin and hematocrit levels, perioperative
transfusionandpostoperativetransfusionamounts. Periop-erativetransfusionandoperationtime(>140min)variables wereidentifiedassignificant(p<0.05).Oddsratiofor peri-operativetransfusionwas−4.257(95%CI−0.502to−0.184)
whichmeansthat,4.257timeslesslikelyABTwasneeded
duringtheoperationintheCSgroup.ORforoperationtime
wasas2.720 (95% CI 0.001---0.004); whichmeans that we
used CS system in operations longer than 140min; 2.574
times morelikely. Per-op blood transfusionand operation
timeeffectswereindependentriskfactorsforCellSalvage group(Table5).
Discussion
Inmajororthopedicsurgeriessuchastotalhiparthroplasty surgeries,intraoperativeblood lossandassociatedanemia arefrequent.Inparticular,anemialeadstotheneedforABT,
declined physical functioning, augmented infection rates,
longerhospitalstay,andevenmortality.6 Inmanystudies,
patientbloodmanagementinterventionsbasedon
postop-erative transfusion of salvaged blood cells can provide a
significantreductioninABTs.6
In our study, the use of the CS system decreased the
need for ABT in the perioperative period. The mean ABT
rate was92.53mL in the control group and 170.14mL in
thecontrolgroup.Themeanpostoperativetransfusionrate
in the CS group was also lower than that in the control
group(125.37mLvs.155.22mL),butthedifferenceinthese resultsdidnotreachastatisticallysignificantlevel.In
addi-tion,thepercentageofthepatientswhoreceivedABTwas
alsosignificantlylowerintheCSgroup(n=29;43.2%)than inthecontrolgroup(n=56;73.6%).Ourresultsaresimilar totheresultsreportedintheliterature.Theresultsofthe studybyErsenetal.7areconcurrentwithoursandindicated
aperioperative decreasein ABT ratewhenthe CSsystem
wasusedinposteriorspinalfusion surgery.Theirreported
meanamount ofbloodtransfuseddecreasedfrom2.5Uto
1.04UwhentheCSsystemwasused.7Inaprospective
obser-vationalcohortstudyonhiparthroplastyrevisionsinwhich
Table2 Bloodtransfusiondata.
Cellsalvagegroup Controlgroup p-value
Perioperativetransfusion;n(%)a 29(43.2%) 56(73.6%) 0.022c
Postoperativetransfusion;n(%)a 25(37.3%) 39(51.3%) >0.05
Perioperativetransfusion(mL);mean±SDb 92.53±111.88 170.14±116.79 0.001c
Postoperativetransfusion(mL);mean±SDb 125.37±193.33 155.22±208.37 >0.05
Perioperativecellsalvagetransfusion(mL);mean±SD 333.61±170.99
NS,nosignificant. a Chisquaretest. b Mann---WhitneyUtest.
Table3 Hematologicaldata.
Cellsalvagegroup (mean±SD)
Controlgroup (mean±SD)
p-value
Preoperativehemoglobin(g/dL) 12.84±1.39 12.50±1.52 >0.05
Dischargehemoglobin(g/dL) 11.09±1.61 10.95±1.54 >0.05
Preoperativehematocrit 38.56±3.65 37.43±5.59 >0.05
Dischargehematocrit 33.76±4.92 33.05±4.54 >0.05
Independentsamplestest. p>0.05,nosignificant.
Table4 Infectionmarkers.
Cellsalvagegroup (mean±SD)
Controlgroup (mean±SD)
p-value
CRPa 10.14±15.82 6.57±9.24 >0.05
Bodytemperature(◦C)b 37.59±0.52 37.63±0.47 >0.05
Preoperativeleukocytesb 7620.82±1930.59 7649.53±2686.75 >0.05
Postoperativeleukocytesb 13007.00±4483.51 12158.00±4567.90 >0.05
aMann---WhitneyUtest. b Independentsamplestest.
p>0.05,nosignificant.
210caseswereincluded,perioperativeCSusedecreasedthe
chanceof needing an ABT.1The results ofthe studywere
paralleltoourfindings.In ourlogisticregression analysis, perioperativebloodtransfusionwasidentifiedassignificant.
In the control group, the possibility of having an ABT is
almost4times(OR=4.257)morelikelythanCSgroup.
The CSsystem hasshownpositive evidenceforits
effi-cacyin orthopedicsurgery.9 Manystudies supporttheuse
of the CS system to reduce the necessity for ABTs in hip
andkneesurgeries.10---12 In a prospectivestudy byThomas
etal.,12 which included a total of 231 knee replacement
patients,a decrease in allogeneic blood requirement was
observedintheCSgroup.12Despitethesatisfactoryresults
of knee and hip arthroplasties owing to the CS system,
other majororthopedic surgeriesshow conflictingresults. Forspinalsurgeryoracetabularfracturerepair,some
stud-iesdid not report any benefit of the CS system in terms
of reduction in the need for ABTs and cost.13---16 Scannel
et al. retrospectively evaluated patients who underwent
openreductioninternalfixationforacetabularfractureand found no beneficial results for CS.13 In the retrospective
study of Gause et al., the use of the CS system in adult
lumbarspinalsurgeryincreasedtheneedforABTs.14Owens
et al.also didnot reportany beneficial results of theCS systeminadultlumbarspinalsurgeryintheirretrospective review.15
Incontrast,Ersenetal.7andBowenetal.17demonstrated
adecreaseinABTs withtheCSsystemforadolescent
sco-liosiscases treatedwithposterior spinal fusion. Foradult lumbarfusion,Savvidouetal.18 reportedbeneficialresults
for the CS system in their prospective randomized trial
including50patients.Intheirretrospectivestudyon acetab-ularfracturesurgery,Bigsbyetal.3showedbeneficialresults
fortheCSsystemintermsofcost-effectivenessandreducing theneedforABTs.Intheirrecentstudydesignedfor pedi-atric orthopedic and cardiac surgeries,Samnaliev et al.19
reportedtheuseoftheCSsystemascost-effectiveandcost savingespeciallywhenusedalongwithABT.
Table5 Logisticregressionanalysisofriskfactorseffectingautologousbloodtransfusion.
p ODDS 95%CI
Lower Upper
PerioperativeTransfusion 0.001a −4.257 −0.502 −0.184
PostoperativeTransfusion 0.094 −1.685 −0.306 0.24
Operationtime(>140min) 0.007b 2.720 0.001 0.004
PreopHgb 0.616 0.502 −0.40 0.068
PreopHct 0.382 0.877 −0.010 0.026
Inourstudy,operationtimewassignificantlylongerinthe CSgroup.Thisisbecauseinourinstitution,theCSsystemis
generallypreferredformorecomplicatedcases(estimated
blood loss>1000mL,BMI>30,difficult surgical technique)
and the more complicated a case becomes, the longerit
takestocompletethesurgery.Enterlogisticregression anal-ysis, showed us, operation timeeffect (>140min) wasan independentrisk factor forCSgroup. Thispoints outs,an almost2.7timesmore(OR=2.720)likelyusageofCSsystem
inoperationslongerthan 140min. Althoughthe operation
timeswerelongerintheCSgroup,lessamountofABTwas
necessaryduringthesurgery,whichseemsasapossible ben-efitforthepatient.
Thedistributionofthemaleandfemalepopulationswas
similar between the groups. However, the proportion of
femalepatientswashigherinbothgroups.Thisphenomenon is alsospecific toour institution;that is, femalepatients
undergohip arthroplasty surgeries2 or 3 times more
fre-quently than malepatients. An epidemiological study for
a Turkish population who had undergone hip arthroplasty
surgeryshouldbeconductedtovalidateourresults.
In terms of infection markers, we reviewed
preopera-tive CRP levels, leukocyte levels,and body temperatures
for bothgroups. Wealsoreviewedfor thehighest
postop-erativeleukocytelevel,bodytemperature,andCRPlevels. We found nostatistical significance in terms of leukocyte level,bodytemperature,andCRPlevelbetweenthegroups.
A prospective observational study of 308 patients found
that ABT was associated with an increased incidence of
postoperative infections when compared with autologous
transfusion.20
DuringtheoperationofthepatientsintheCSgroup,the
meanamountofblood transfusedfromtheCSsystemwas
333mL.OurdataaresimilartothedataobtainedbyWalsh etal.,1 whoconducted aprospectivecohort studyfor hip
arthroplastyrevisionsin11hospitalsovera7-monthperiod
andfound amean reinfusionamount of312mL.21 In their
retrospectivestudy,JainandJain21reportedaslightlyhigher
amountofsalvagebloodthanthatreportedinourpresent
study,thatis,527mLfortotalkneearthroplastyand437mL fortotalhiparthroplasty.
Themainlimitationofourstudywasitsdesignasa ret-rospective study. Anotherlimitation wasthe fact that,in ourinstitution,ourtransfusionthresholdis8g/dLfor
allo-geneic blood transfusion for healthy adults and between
8g/dLand10g/dLforpatientswithseverecardiacdisease,
andsevereco-morbidities.But thereis anongoing debate
abouttransfusionthresholdsandconflictsareunsolved.Asa resultdifferentthresholdsindifferentinstitutionscancause variedresults.
Bloodtransfusionshould beavoidedwheneverpossible
because of the increased risk for transfusion-transmitted
diseasesandnoninfectiouscomplications.Allpatientblood
managementstrategiesshouldbeconsideredduringmajor
orthopedicsurgerytolessentheneedforABTs.
InaCochraneDatabaseReview,Carlessetal.5reported
thatincardiacandorthopedicsurgeries,thereisadequate proofofthebenefitsoftheCSsystemandthatitdoesnot
causeanyadverseevents.
Patient blood management is an important issue for
orthopedic patients who are candidates for arthroplasty
surgeries.Inourstudy,theneedforperioperativeABTwas
diminishedsignificantly. Thus,the CSsystemmay be
con-sideredasan effectivestrategy forreducing theneed for
ABTs;itprovidessupporttopatientbloodmanagement.We
recommendthe useof the CSsystem for hiparthroplasty
surgeriesifpossible.
Conflicts
of
interest
Theauthorsdeclarenoconflictsofinterest.
References
1.WalshTS,PalmerJ,WatsonD,etal.Multicentrecohortstudy ofredbloodcelluseforrevisionhiparthroplastyandfactors associatedwithgreaterriskofallogeneicbloodtransfusion.Br JAnaesth.2012;108:63---71.
2.Spiess BD. Risks of transfusion: outcome focus. Transfusion. 2004;4412Suppl.:4S---14S.
3.BigsbyE,AcharyaMR,WardAJ,et al.The useofbloodcell salvageinacetabularfractureinternalfixationsurgery.JOrthop Trauma.2013;27:230---3.
4.Engelbrecht S, Wood EM, Cole-Sinclair MF. Clinical transfu-sionpracticeupdate:haemovigilance, complications,patient blood management and national standards. Med J Aust. 2013;199:397---401.
5.CarlessPA,Henry DA,Moxey AJ,et al.Cellsalvagefor min-imisingperioperative allogeneicblood transfusion.Cochrane DatabaseSystRev.2006:CD001888.
6.SpahnDR.Anemiaandpatientbloodmanagementinhipand kneesurgery:asystematicreviewoftheliterature. Anesthesi-ology.2010;113:482---95.
7.ErsenO,KoseO,OguzE.Posteriorspinalfusioninadolescent idiopathic scoliosis with or without intraoperative cell sal-vagesystem:aretrospectivecomparison.MusculoskeletSurg. 2012;96:107---10.
8.WatersJH, YazerM, ChenYF, et al. Bloodsalvage and can-cersurgery:ameta-analysisofavailablestudies.Transfusion. 2012;52:2167---73.
9.AshworthA,KleinAA.Cellsalvageaspartofablood conserva-tionstrategyinanaesthesia.BrJAnaesth.2010;105:401---16.
10.Bridgens JP,EvansCR, DobsonPMS,etal. Intraoperativered blood-cellsalvage inrevisionhipsurgery.JBone JointSurg. 2007;89:270---5.
11.Zarin J, Grosvenor D, Schurman D, et al. Efficacy of intra-operativebloodcollectionandreinfusioninrevisiontotalhip arthroplasty.JBoneJointSurgAm.2003;85-A:2147---51.
12.Thomas D, Wareham K, Cohen D, et al. Autologous blood transfusion intotalkneereplacementsurgery.Br JAnaesth. 2000;86:669---73.
13.ScannelBP,LoefflerBJ,BosseMJ,etal.Efficacyof intraopera-tiveredbloodcellsalvageandautotransfusioninthetreatment ofacetabularfractures.JOrthopTrauma.2009;23:340---5.
14.GausePR,SiskaPA,WestrickER,etal.Efficacyof intraopera-tivecell saverindecreasingpostoperativebloodtransfusions in instrumented posterior lumbar fusion patients. Spine. 2008;33:571---5.
15.OwensRK,CrawfordCH,DjurasovicM,etal.Predictivefactors fortheuseofautologouscellsavertransfusioninlumbarspinal surgery.Spine(PhilaPa1976).2013;38:217---22.
16.WeissJM,SkaggsD,TannerJ,etal.Cellsaver:isitbeneficial inscoliosissurgery?JChildOrthop.2007;1:221---7.
18.Savvidou C, Chatziioannou SN, Pilichou A, et al. Effi-cacy and cost-effectiveness of cell saving blood auto-transfusion in adult lumbar fusion. Transfus Med. 2009;19: 202---6.
19.Samnaliev M,Tran CM,SloanSR,et al. Economicevaluation ofcellsalvageinpediatricsurgery.PaediatrAnaesth.2013;23: 1027---34.
20.InnerhoferP,KlinglerA,KlimmerC,etal.Riskofpostoperative infectionaftertransfusionofwhitebloodcell-filteredallogenic orautologousbloodcomponentsinorthopedicpatients under-goingprimaryarthoplasty.Transfusion.2005;45:103---10.