w w w . r b o . o r g . b r
Original
Article
Lateral
decubitus
for
treating
pertrochanteric
fractures
using
cephalomedullary
nails
夽
Elton
João
Nunes
de
Oliveira
∗,
José
Octávio
Soares
Hungria,
Davi
Gabriel
Bellan,
Jonas
Aparecido
Borracini
HospitalMunicipalDr.FernandoMauroPiresdaRocha,SãoPaulo,SP,Brazil
a
r
t
i
c
l
e
i
n
f
o
Articlehistory:
Received20November2014 Accepted28January2015 Availableonline1August2015
Keywords: Pertrochanteric Cephalomedullarynail Lateraldecubitus Femurfracture
a
b
s
t
r
a
c
t
Objective:Toperformaretrospectiveradiographicevaluationonthefracturereductionand implantpositioninthefemoralheadamongpatientswithpertrochantericfractureswho hadbeentreatedusingacephalomedullarynailinlateraldecubitus;andtoassessfactors thatmightinterferewiththequalityofthefracturereductionandwiththeimplantposition inusingthistechnique.
Methods:Nineteenpatientswithadiagnosisofpertrochantericfracturesofthefemurwho hadbeentreatedusingcephalomedullarynailsinlateraldecubituswereevaluated.For out-patientradiographicevaluations,weusedtheanteroposteriorviewofthepelvisandlateral viewofthesideaffected.Wemeasuredthecervicodiaphysealangle,tip-apexdistance(TAD), spatialpositionofthecephalicelementinrelationtothehead,andthebispinal diame-ter.Tomakeananthropometricassessment,weusedthebodymassindex.Twogroupsof patientswerecreated:oneinwhichallthecriteriawerenormal(TAD≤25mm, cervicodi-aphysealanglebetween130◦and135◦andcephalicimplantpositioninthefemoralhead
inthecentral–centralquadrant);andanothergrouppresentingalterationsinsomeofthe criteriaforbestprognosis.
Results:Female patients predominated (57.9%) andthe mean agewas 60 years. Seven patientspresentedacentral–centralcephalicimplantposition.Onepatientpresenta cervi-codiaphysealangle>135◦andthemaximumTADwas32mm;consequently,12patients
presented some altered criteria (63.2%). None of thecharacteristics evaluated differed betweenthepatientswithalltheircriterianormalandthosewithsomealteredcriteria, orshowedanystatisticallysignificantassociationamongthem(p>0.05).
Conclusion: Thetechniquedescribedhereenabledgoodreductionandgoodpositioningof theimplant,independentoftheanthropometricindicesandtypeoffracture.
©2015SociedadeBrasileiradeOrtopediaeTraumatologia.PublishedbyElsevierEditora Ltda.Allrightsreserved.
夽
WorkperformedintheOrthopedicsandTraumatologyService,HospitalMunicipalDr.FernandoMauroPiresdaRocha,CampoLimpo, SãoPaulo,SP,Brazil.
∗ Correspondingauthor.
E-mail:elton.joao@gmail.com(E.J.N.deOliveira). http://dx.doi.org/10.1016/j.rboe.2015.07.006
410
rev bras ortop.2015;50(4):409–415Decúbito
lateral
para
tratamento
das
fraturas
pertrocantéricas
com
hastes
cefalomedulares
Palavras-chave: Pertrocantérica Hastescefalomedulares Decúbitolateral Fraturadefêmur
r
e
s
u
m
o
Objetivo:Fazerumaavaliac¸ãoradiográficaretrospectivadareduc¸ãoeposic¸ãodoimplantena cabec¸afemoralempacientescomfraturaspertrocantéricastratadoscomhaste cefalomedu-laremdecúbitolateralefatoresquepossaminterferirnaqualidadedareduc¸ãodafratura eposic¸ãodoimplantenousodessatécnica.
Métodos: Foram avaliadosretrospectivamente19 pacientes comdiagnósticode fratura pertrocantérica do fêmur tratados com haste cefalomedular em decúbitolateral. Para avaliac¸ãoradiográficaambulatorialusamosasincidênciasanteroposteriordapelveeoperfil doladoafetado.Aferimosoângulocervicodiafisário,oTAD,aposic¸ãoespacialdoelemento cefáfiloemrelac¸ãoàcabec¸aeodiâmetrobiespinhal.Paraavaliac¸ãoantropométricausamos índicedemassacorporal.Foramcriadosdoisgruposdepacientes,umcomtodososcritérios normais(TAD<25mm,ângulocervicodiafisárioentre130◦e135◦eaposic¸ãodoimplante
cefáliconacabec¸afemoralnoquadrantecentral-central)eoutrocomalterac¸ãoemalgum doscritériosdemelhorprognóstico.
Resultados: Houvepredomíniodosexofeminino(57,9%),comidademédiade60anos.Sete pacientesficaramcomaposic¸ãodoimplantecefáliconaposic¸ãocentral-central,um apre-sentouângulocervicodiafisário>135◦eoTADmáximofoide32mm.Consequentemente,12
pacientesapresentaramalgumdoscritériosalterados(63,2%).Nenhumadascaracterísticas avaliadasdiferiuoumostrouassociac¸ãoestatisticamentesignificativaentrepacientescom todososcritériosnormaisealgumcritérioalterado(p>0.05).
Conclusão: Atécnicadescritapermiteuma boareduc¸ão eum bomposicionamentodo implante,independentementedosíndicesantropométricosedotipodefratura.
©2015SociedadeBrasileiradeOrtopediaeTraumatologia.PublicadoporElsevier EditoraLtda.Todososdireitosreservados.
Introduction
Pertrochantericfracturesarecommonintheelderly popula-tionbecauseofosteoporosis.Their incidencehasincreased significantly because ofgreater lifeexpectancy amongthe population,withtheestimatethatthismaydoubleoverthe next25years.1Everyyear,oneinevery1000inhabitantsof developedcountriesisaffectedbythesefracturesandithas been estimatedthatby2050, the annualcostoftreatment (currentlyUS$8billion)mayhavedoubled.Thus,thisis con-sideredtobeoneoftheworld’smostimportantpublichealth problems.2
Today, there is a consensus that fractures in the pertrochantericregionofthefemurshouldbefixedsurgically, giventhattheaimofsurgicaltreatmentistoachievestable reductionandfixationthatprovidepatientswithearlyactive andpassivemobilization.3,4
Many authors have recommended treatment for
unstable pertrochanteric fractures consisting of modern intramedullary implants because of their greater capacity for load absorption5 and their potential forapplication to allfracturepatterns.Fixationtechniquesforthesefractures consistingofcephalomedullarynailscanbeperformedbest onatractiontable.However,intheabsenceofthis,another formofdecubitusbecomesnecessary,suchasobliquelateral decubitus,6forthistreatment.
The aim of this study was to perform a retrospec-tive radiographic evaluation on fracture reduction and
implant positioning in the femoral head, in patients with pertrochanteric fractures that were treated using a cephalomedullarynail,withthepatientinlateraldecubitus; andtoevaluatefactorsthatmightinterferewiththequality ofthefracturereductionandimplantpositioningwhenthis techniqueisused.
Material
and
methods
Between June 2012 and November 2013, 29 patients with a diagnosis of pertrochanteric fractures ofthe femur were treatedusingacephalomedullarynailatthemunicipal hospi-talofSãoPaulo(SP).Amongthesepatients,19returnedfora retrospectivefinalassessment,eightcouldnotbefoundand twodiedwithinthehospitalenvironmentduringthe imme-diate postoperative perioddueto complicationsfrom their injuries.Elevenofthereassessedpatients(57.9%)werefemale and eight (42.1%)were male, witha mean age of60 years (range:18–87).Regardingthetraumamechanism,therewere 13casesofafalltotheground,fourcasesoffallsfrom motor-cycles,onecaseofgunshotwoundsandonecaseofafallfrom abicycle.Elevenofthesepatientspresentedfracturesonthe leftsideandeightontherightside.
Fig.1–Patientpositionedinlateraldecubitus–APradioscopicviewofthepelvis.
cortex;andA3alsopresentsabrokenlateralcortex(inverted obliquefractures).7Amongthepreoperativeradiographs eval-uated,onepresentedthe31A1pattern,eleven31A2andseven 31A3.Theminimumdurationofthepostoperativeevaluation wassixmonths.
Toperform the surgical procedure, the patient was put undergeneralor spinalanesthesia whileinlateral decubi-tus,withthe aid ofpadson the dorsum and abdomenon that side, using aradiotransparent table withan extender because of the short length. Radioscopic control was per-formedinanteroposterior(AP)viewandlateralview,inorder to ascertain the correct viewing of the entire femur and pelvisin the two planes. Following this,asepsis and anti-sepsiswere performed on the sideaffected, from the iliac cresttothefoot.Thereductionwasperformedbymeansof
manualtraction,withsomedegreeofrotation,adductionor abductionwhennecessary, withorwithoutamini-incision ontheproximallateralfaceofthethighforfracture reduc-tion.Weusedcephalomedullarynails(GammaTMnail®,TFN®) andthestandardtechnique8forosteosynthesisoffractures. Intheproximalfixation,itwassoughttopositionthecephalic fixation element at the center of the head, 1cm from the subchondralboneinnormalboneand0.5cminosteoporotic bone,inAPand lateralviews.Thelateralfixationwas per-formedbymeansofaguidewhenanailofstandardsizewas used,orfreehandinsituationsoflongnails.Ateachstage, radioscopiccontrolwasperformedbothinAPandinlateral view. All the cases were operatedby a third-year resident under supervision by the same senior attendingphysician (Figs.1and2).
412
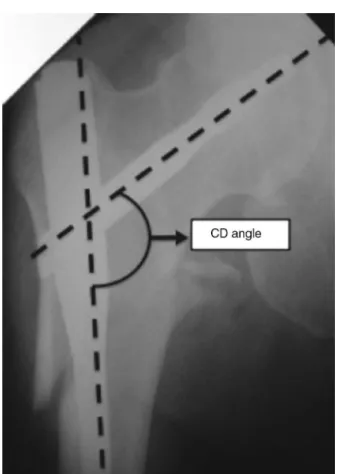
rev bras ortop.2015;50(4):409–415Fig.3–Cervicodiaphyseal(CD)angle.
Toperformoutpatientradiographicassessments,weused theAPviewofthepelviswiththepatientindorsal decubi-tus,withtheraysincidentonthemedianlineofthepublic symphysisandthe feetrotatedinternallyat15◦–20◦, inthe standardtechnique;andthelateralviewwiththepatientalso positionedindorsaldecubitus,withthehipaffectedflexedat 45◦andabductedat20◦,andwiththeraycenteredvertically onthecoxofemoraljoint,inthestandardtechnique.9Through theseviews,thefollowingwereevaluated:
Cervicodiaphysealangle:angleformedbetweentwolines, onecrossingthecenterofrotationofthefemoralheadand
Superior
Inferior 0
0 0
0 3
0
6 7 3
A n t e r i o r
P o s t e r i o r
Fig.5–Spatialpositionofthecephalicelementinrelation tothehead.
thecenterofthefemoralneck,andtheotheralongthelong axisofthefemur10(Fig.3).
Tip-apexdistance(TAD):definedinaccordancewithwhat wasdescribedbyBaumgaertneretal.11(Fig.4).
Spatialpositionofthe cephalicelementinrelationtothe head:thefemoralheadwasdividedintonineseparatezones, inwhichthecephalicelementmightbelocated,asfollows: upper,middleandlowerthirdsonAPradiographsand ante-rior, central and posterior thirds on lateral radiographs11 (Fig.5).
Bispinal diameter: this extendedfrom the anterosuperior iliacspineononesidetothatoftheoppositeside12(Fig.6).
To makeanthropometric evaluations,weused the body mass index (BMI), which was calculated using weight and height measurements according to the following formula: BMI=weight(kg)/height2(cm).13
Thequantitativecharacteristicsthatwereevaluatedwere described using summary measurements (mean, standard deviation,median,minimumandmaximum)andthe qualita-tivecharacteristicsweredescribedusingabsoluteandrelative frequenciesforallthepatientsinthestudy.14
Bispinal diameter
Fig.6– Bispinaldiameter.
Twogroupsofpatientswerecreated:onepresenting nor-malvalues for all criteria (TAD≤25mm, cervicodiaphyseal anglebetween130◦ and135◦ and cephalicimplant position inthefemoralheadlocatedinthecentral–centralquadrant); andtheotherwithalterationstosomeofthecriteriafor bet-terprognosis.Thequantitativecharacteristicsweredescribed accordingtogroupsofpatientsandwerecomparedbetween thegroupsusingStudent’st-test,whilethequalitative char-acteristicsweredescribedaccordingtothegroupsandwere correlated using Fisher’s exact test or the likelihood ratio test.14Thetestswereperformedusingthesignificancelevel of5%.
Fig.7–APradiographofthepelvisduringtheimmediate postoperativeperiod.
Fig.8–Lateralradiographofthepelvisduringthe immediatepostoperativeperiod.
Results
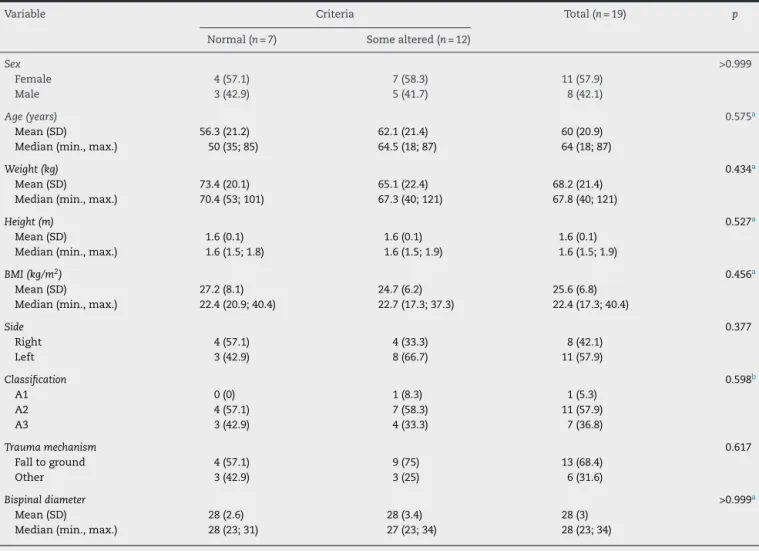
Amongthe19 patientsevaluated, wefoundthatthemean cervicodiaphyseal angle was 135◦, with a range from 130◦ (84.2% of the patients evaluated) to 140◦ (5.3% of the patients evaluated).Themean values,maximum and min-imum TAD,bispinal diameter, height, weight and BMIare described in Table 1. The distribution ofthe cephalic ele-mentisrepresentedschematicallyasshowninFig.5.With regard to AO classification, one fracture (5.3%) was con-sidered to be 31A1, eleven (57.9%) 31A2and seven(34.8%) 31A3.
Table1showsthatthemajorityofthepatientsevaluated werefemale(57.9%),withameanageof60years(SD=20.9). Sevenpatientshadthecephalicimplantinthecentral–central position;onlyonepatientpresentedacervicodiaphysealangle greater than 135◦; and the maximum TAD observed was 32mm.Consequently,12patientspresentedsomecriteriathat werealtered(63.2%).
Table2showsthatnoneofthe characteristicsevaluated differed or showed any statistically significant association betweenthepatientspresentingnormalvaluesforallcriteria andthosewithsomealteredvalues(p>0.05).
Discussion
414
rev bras ortop.2015;50(4):409–415Table1–Descriptionofthecharacteristicsofallthepatientsevaluated.
Variable Description(n=19) Variable Description(n=19)
Sex Traumamechanism
Female 11(57.9) Falltoground 13(68.4)
Male 8(42.1) Other 6(31.6)
Age(years) Widthofpelvis(cm)
Mean(SD) 60(20.9) Mean(SD) 28(3)
Median(min.,max.) 64(18;87) Median(min.,max.) 28(23;34)
Weight(kg) Positionofcephalicimplant
Mean(SD) 68.2(21.4) Superior-central 3(15.8)
Median(min.,max.) 67.8(40;121) Central-anterior 6(31.6)
Height(m) Central–central 7(36.8)
Mean(SD) 1.6(0.1) Central-posterior 3(15.8)
Median(min.,max.) 1.6(1.5;1.9) Cervicodiaphysealangle
BMI(kg/m2) 130◦ 16(84.2)
Mean(SD) 25.6(6.8) 135◦ 2(10.5)
Median(min.,max.) 22.4(17.3;40.4) 140◦ 1(5.3)
Side TAD(mm)
Right 8(42.1) Mean(SD) 22.5(4)
Left 11(57.9) Median(min.,max.) 22(15;32)
Classification Criteria
A1 1(5.3) Normal 7(36.8)
A2 11(57.9) Somealtered 12(36.2)
A3 7(36.8)
Table2–Descriptionofthecharacteristicsevaluatedaccordingtoalterationstothecriteriaandresultsfromthe statisticaltests.
Variable Criteria Total(n=19) p
Normal(n=7) Somealtered(n=12)
Sex >0.999
Female 4(57.1) 7(58.3) 11(57.9)
Male 3(42.9) 5(41.7) 8(42.1)
Age(years) 0.575a
Mean(SD) 56.3(21.2) 62.1(21.4) 60(20.9)
Median(min.,max.) 50(35;85) 64.5(18;87) 64(18;87)
Weight(kg) 0.434a
Mean(SD) 73.4(20.1) 65.1(22.4) 68.2(21.4)
Median(min.,max.) 70.4(53;101) 67.3(40;121) 67.8(40;121)
Height(m) 0.527a
Mean(SD) 1.6(0.1) 1.6(0.1) 1.6(0.1)
Median(min.,max.) 1.6(1.5;1.8) 1.6(1.5;1.9) 1.6(1.5;1.9)
BMI(kg/m2) 0.456a
Mean(SD) 27.2(8.1) 24.7(6.2) 25.6(6.8)
Median(min.,max.) 22.4(20.9;40.4) 22.7(17.3;37.3) 22.4(17.3;40.4)
Side 0.377
Right 4(57.1) 4(33.3) 8(42.1)
Left 3(42.9) 8(66.7) 11(57.9)
Classification 0.598b
A1 0(0) 1(8.3) 1(5.3)
A2 4(57.1) 7(58.3) 11(57.9)
A3 3(42.9) 4(33.3) 7(36.8)
Traumamechanism 0.617
Falltoground 4(57.1) 9(75) 13(68.4)
Other 3(42.9) 3(25) 6(31.6)
Bispinaldiameter >0.999a
Mean(SD) 28(2.6) 28(3.4) 28(3)
Median(min.,max.) 28(23;31) 27(23;34) 28(23;34)
consequent toimprovementof the qualityoflife and also betterhealthcare.Many methodshavebeen recommended fortreatingpertrochantericfracturesandthereisunanimity intheliteratureregardingtherecommendationthattraction tablesshouldbeusedfortheirtreatment,orobliquelateral decubitusintheabsenceofsuchtables.6 However,because ofthe characteristics of our hospitalservice, we have not achievedgood resultsthroughusingthis typeofdecubitus andwehavethereforestartedtousethealternativeoflateral decubitus.
Becausethisisanewtechnique,thereferencestandards thatweusedwerethevaluesencounteredincasesof frac-turesinwhichthetreatmentwasdoneon atraction table. Thus,wesoughtthroughreductiontoreconstitutethe nor-malcervicodiaphysealangleof130◦–135◦,sothattheimplant couldbeperfectlypositionedandwewouldespeciallybeable toavoidvarusreductions.15,16Inperformingtheproximal fix-ation,itwassoughttopositionthecephalicfixationelement atthecenterofthehead,bothinAPandinlateralview,ata distanceof1cmfromthesubchondralboneinbothviewsin normalboneandat0.5cminosteoporoticbone.Wefollowed theconceptintroducedbyBaumgaertneretal.11Inthepresent study,wesuccessfullyobtainedtheseparameters,giventhat wefound a mean TAD of22.5mm(this was described for osteosynthesis using DHS and can be used for assessing whether the cephalomedullary nails have been correctly positioned)15andameancervicodiaphysealangleof135◦.
Sinceweusedtruelateraldecubitusforobtaining lateral-viewradioscopicimages,webelievethatgreaterpelvicwidth orobesity(measuredindirectlyfromthebispinaldiameterand BMI)wouldmakeitdifficulttoviewandpositionthecephalic implant in lateral view. However, there was no statistical correlationbetweenpatientswithgreater BMIand bispinal diametersandthosewhopresentedTAD>25mmand/orpoor positioning of the cephalic fixation element, although we perceivedthattherewassomeintraoperativetechnical dif-ficultyamongthepatientswhowereobeseorwhosepelvis waswider.
Amongtheninepossiblelocationsfortheproximalfixation elementinthehead,thelocationwasdistributedbetweenfour zonesinour study:central–central(36.8%),central-anterior (31.6%),central-posterior(15.8%)andsuperior-central(15.8%). Thisshowsthattheareasatgreatestriskofcutout (superior-anteriorandinferior-posterior)11wereavoided(Fig.5).
Pertrochantericfractureshavespecialimportanceatpublic healthlevel,suchthatanyusefultechnicalevolutionwould havegreathumanandeconomicvalue.Thus,lateraldecubitus isatechniquethatcanbechosen,whichhasbeenshownto enablegoodfracturereductionandgoodimplantpositioning inthefemoralhead,independentofanthropometricindices.It thereforebecomesanoptionfortreatingthesefracturesinthe absenceoforimpossibilityofusingatractiontableoranother typeofdecubitus(Figs.7and8).
Conclusion
Thetechniquedescribedallowsgoodfracturereductionand good implant positioning, independent of anthropometric indicesandtypeoffracture.
Conflicts
of
interest
Theauthorsdeclarenoconflictsofinterest.
r
e
f
e
r
e
n
c
e
s
1.UlianaCS,AbaggeM,MalafaiaO,KalilFilhoFA,CunhaLAM. Fraturastranstrocantéricas–Avaliac¸ãodosdadosda admissãoàaltahospitalar.RevBrasOrtop.2014;49(2): 121–8.
2.TakanoMI,MoraesRCP,AlmeidaLGMP,QueirozRD.Análise doempregodoparafusoantirrotacionalnosdispositivos cefalomedularesnasfraturasdofêmurproximal.RevBras Ortop.2014;49(1):17–24.
3.BucholzRW,Court-BrownCM,HeckmanJD,TornettaPIII. Rockwood&Greenfraturasemadultos.7thed.Barueri,SP: Manole;2013.
4.PajarinenJ,LindahlJ,MichelssonO,SavolainenV,Hirvensalo E.Pertrochantericfemoralfracturestreatedwithadynamic hipscreworaproximalfemoralnail.Arandomisedstudy comparingpost-operativerehabilitation.JBoneJointSurgBr. 2005;87(1):76–81.
5.BridleSH,PatelAD,BircherM,CalvertPT.Fixationof intertrochantericfracturesofthefemur.Arandomised prospectivecomparisonofthegammanailandthedynamic hipscrew.JBoneJointSurgBr.1991;73(2):330–4.
6.SirkinMS,BehrensF,McCrackenK,AuroriK,AuroriB,Schenk R.Femorlnailingwithoutafracturetable.ClinOrthopRelat Res.1996;(332):119–25.
7.RüediTP.PrincípiosAOdotratamentodefraturas.2nded. PortoAlegre:Artmed;2009.
8.CanaleST.Campbell’soperativeorthopaedics.12thed.St. Louis:Mosby;2013.
9.PoleselloGC,NakaoTS,QueirozMC,DaniachiD,RicioliJunior W,GuimarãesRP,etal.Propostadepadronizac¸ãodoestudo radiográficodoquadriledapelve.RevBrasOrtop.
2011;46(6):634–42.
10.PajarinenJ,LindahlJ,SavolainenV,MichelssonO,Hirvensalo E.Femoralshaftmedialisationandneck-shaftanglein unstablepertrochantericfemoralfractures.IntOrthop. 2004;28(6):347–53.
11.BaumgaertnerMR,CurtinSL,LindskogDM,KeggiJM.The valueofthetip-apexdistanceinpredictingfailureoffixation ofperitrochantericfracturesofthehip.JBoneJointSurgAm. 1995;77(7):1058–64.
12.ZugaibM.Zugaibobstetrícia.2nded.Barueri,SP:Manole; 2012.
13.RezendeFAC,RosadoLEFPL,RibeiroRCL,VidigalFC,Vasques ACJ,BonardIS,etal.Índicedemassacorporale
circunferênciaabdominal:associac¸ãocomfatoresderisco cardiovascular.ArqBrasCardiol.2006;87(6):
728–34.
14.KirkwoodBR,SterneJAC.Essentialmedicalstatistics.2nded. Malden,MA:BlackwellScience;2006.
15.BorgerRM,LeiteFA,AraújoRP,PereiraTFN,QueirozRD. Avaliac¸ãoprospectivadaevoluc¸ãoclínica,radiográficae funcionaldotratamentodasfraturastrocantéricasinstáveis dofêmurcomhastecefalomedular.RevBrasOrtop. 2011;46(4):380–9.