Brazilian
Journal
of
OTORHINOLARYNGOLOGY
www.bjorl.org
ORIGINAL
ARTICLE
Evaluation
of
the
nasal
shape
after
orthognathic
surgery
夽
,
夽夽
Wagner
Ranier
Maciel
Dantas
a,b,
Márcia
Maria
Fonseca
da
Silveira
c,d,
Belmiro
Cavalcanti
do
Egito
Vasconcelos
e,∗,
Gabriela
Granja
Porto
a,f,gaOralandMaxillofacialSurgeryDivision,UniversidadedePernambuco(UPE),Recife,PE,Brazil bSurgeryDepartment,UniversidadeFederaldoRioGrandedoNorte(UFRN),Natal,RN,Brazil
cOraldiagnosisDivision,FaculdadedeOdontologiadeBauru,UniversidadedeSãoPaulo(USP),Bauru,SP,Brazil dStomatologyDivision,UniversidadedePernambuco(UPE),Recife,PE,Brazil
eUniversidadedePernambuco(UPE),Recife,PE,Brazil
fStrictuSensoForensicInvestigationDivision,FaculdadedeOdontologiadePernambuco,UniversidadedePernambuco(UPE),
Recife,PE,Brazil
gOralandMaxillofacialSurgeryDivision,HospitalRegionaldoAgreste(HRA),Caruaru,PE,Brazil
Received22March2012;accepted24May2014 Availableonline28August2014
KEYWORDS Maxilla;
Nasalobstruction; Orthodontics
Abstract
Introduction:Patientswithdentofacialdeformitiesmaybenefitfromorthognathicsurgeryin themaxilla.Maxillaryosteotomymayincludeproceduresinthebone,cartilaginous,andsoft tissuesofthenose,leadingtoshapealterations.
Objective: ToevaluatetheanatomicalterationsofthenasalregioninpatientsundergoingaLe FortIosteotomyforadvancementorsuperiorimpaction.
Methods:Thisisaclinicalprospectivestudy.Twenty-onepatientswereevaluatedduringthe pre-andpostoperativeperiods.Thepositioningofthenasaltipandthemodificationofthe nasalbasewereevaluated.
Results:Theresultsshowedthatthenasaltipwassuperiorlypositionedin85%ofthecases, advancedin80%,rotatedin80%,andtherewasawidenasalbasein95%,resultinginesthetic improvement.
Conclusions: Surgeriesofmaxillaryadvancementandsuperiorrepositiontendtocause eleva-tionandadvancementofthenasaltip,aswellasenlargementofthenasalbase.
© 2014Associac¸ãoBrasileira de Otorrinolaringologiae CirurgiaCérvico-Facial. Publishedby ElsevierEditoraLtda.Allrightsreserved.
夽 Pleasecitethisarticleas:DantasWR,daSilveiraMM,VasconcelosBC,PortoGG.Evaluationofthenasalshapeafterorthognathicsurgery.
BrazJOtorhinolaryngol.2015;81:19---23.
夽夽Institution:UniversidadedePernambuco(UPE),Recife,PE,Brazil.
∗Correspondingauthor.
E-mails:belmiro@pesquisador.cnpq.br,belmirovasconcelos@gmail.com(B.C.doEgitoVasconcelos).
http://dx.doi.org/10.1016/j.bjorl.2014.08.005
1808-8694/©2014Associac¸ãoBrasileirade OtorrinolaringologiaeCirurgiaCérvico-Facial.Published byElsevierEditoraLtda.Allrights
Maxila;
Obstruc¸ãonasal; Ortodontia
Resumo
Introduc¸ão:Pacientes comdeformidadesdento-faciaispodem ser beneficiadospela cirurgia ortognática namaxila. A técnicacirúrgicadaosteotomia damaxilaincluitambém procedi-mentosrealizadosnaparteósseaecartilaginosaetecidosmolesdonarizoquepodeprovocar mudanc¸asnaforma.
Objetivo:Estetrabalhotevecomopropostaavaliarasmudanc¸asanatômicasdaregiãonasal, decorrentesdecirurgiasmaxilarespelaosteotomiaLeFortIparaavanc¸oe/ouimpacc¸ão.
Método: Trata-sedeumestudoclínicoprospectivo.Foramincluídos21pacientes,submetidos àcirurgiaeavaliadosantese6mesesapósoatocirúrgicoemrelac¸ãoaosmovimentosdaponta nasalemodificac¸õesdabasedonariz.
Resultados: Osresultadosmostrarammudanc¸asdapontanasalparacimaem85%doscasos, para anterior em 80%, rotac¸ão em 80% e alargamento dabase nasal em 95%, promovendo melhoriasestéticas.
Conclusão:Cirurgias de avanc¸o e reposicionamento superior da maxila tendem a causar elevac¸ãoeavanc¸odapontadonariz,assimcomo,umalargamentodabasenasal.
©2014Associac¸ãoBrasileira deOtorrinolaringologiaeCirurgiaCérvico-Facial.Publicadopor ElsevierEditoraLtda.Todososdireitosreservados.
Introduction
Dentofacialdeformitycanbedefinedasanyconditionwhere thefacialskeletondiffersfromtheacceptednormal,with malocclusionand alteredfacialappearance. Orthognathic surgery is indicated for the correction of these deformi-ties, aiming to achieve functional and esthetic recovery. Thesurgery,whenassociatedwithorthodonticprocedures, improvesmasticatoryfunctionandfacialappearance,with astableresultfromthe occlusalpoint ofview, andisthe bestformoftreatmentforpatientswithdentalandskeletal problems.1
Patientswithdentofacialdeformitiesrepresent approx-imately 20% of the population and may exhibit varying degreesof functionalorestheticimpairment.2 These mal-formationscanoccurinonlyonemaxilla,extendtomultiple craniofacialstructures,orappearunilaterallyorbilaterally, aswell as occurring at different degrees in the vertical, horizontal,ortransverseheadplanes.
Accordingtothe extentof theproblem,surgery varies fromsmallmobilizationofgroupsofteethtofull mobiliza-tionof themandible andmaxilla.Orthognathicsurgery is indicatedwhenallgrowthfactorsarefinishedand orthodon-tictreatment isnolongersufficienttomaintainabalance between teethand bone.2 The goal of thesetreatments, surgical and orthodontic, is the correction of dentofacial deformitiesandthebalanceofteeth,bonestructure,and softtissueforimprovedfunctionandbetterfacial appear-ance.
LeFortI-typeosteotomyofthemaxillaincludes proce-duresperformedinbone,cartilage,andsofttissuesofthe nosethat can causechanges innasal shapeandfunction, whichsometimesareunpredictable.3
Therefore,theaimofthisstudywastoevaluatethenasal shapebycephalometricstudyinpatientsundergoing orthog-nathicsurgeryformaxillaryadvancementand/orimpaction throughLeFortIosteotomy.
Methods
All patients underwent maxilla advancement and/or impactionsurgerythroughLeFortItechniqueundergeneral anesthesia, without segmentation, for correction of hori-zontalandverticaldeformities.Beforesurgerythepatients underwentapre-operativeplanningphaseandpre-surgical orthodontictreatment, whichcontinuedafterthesurgery. Theywereassessedpre-andpostoperatively(sixmonths). Patientswithsyndromesorcleftpalatewereexcluded.All participantswhoagreedtoparticipatesignedaninformed consent.
The surgical technique consisted of a standard maxil-laryvestibularincision,fromthemidlinetothe2ndmolar, performedbilaterally,followedbytissuedissectionand sub-periosteal detachment toexpose the lower orbital ridges andmalarprominencewithinfraorbitalnervepreservation. The osteotomy wasinitiated witha surgical reciprocating sawinthegreatestconcavityof thepiriformrecess, hori-zontally,pastthezygomaticpillar.Thinchiselswereusedto completetheosteotomiesofthelateralnasalwallandnasal septum,andastrongcurvedchiselwasusedtoperformthe palatal-pterygoiddisjunction.
Mobilizationofthemaxillawasthenperformedcaudally withmanualmanipulationtoverifyitsmobility.Rowe for-ceps were employedto complete maxillary repositioning. Themaxillawaspositionedaccordingtothesurgicalguide or,inClassIocclusionofpatients,withmaxillo-mandibular fixation using steel wire. The osteosynthesis of the max-illa was performed using four 1.5-mm ‘‘L’’ plates with five orifices, pre-shaped to the desired advancement and positionedonthecanineandzygomaticpillars.4,5The mea-surementofthemaxillaryimpactionextentwasperformed fromtheincisalborderofincisorteethtoafixedpointon theglabella.
Pog b
li ID B
POG
eixo Y
ls a PR AANSsn cm
prn n N Y-axis
X-axis
S 7°
PM
S 7°
n N
prn
A
PR ENP
eixo X
gn
Figure1 Schematicdemonstrationofthecephalometricpointsemployed,basedonHeliövaaraetal.6
postoperativeperiods(sixmonths).Thewidthwasobtained bymeasuringthemostlateralpointofthenostrils,usinga caliper.
Bonemobilizationandthemodificationofthenasaltip aftersurgeryweremeasuredusingcephalometric radiogra-phyinpre-andpostoperativeprofile,whichwasperformed bythesameprofessionalandanalyzedthreetimes,witha periodofonemonthbetweeneach;therewasagreementin 90%ofcases.Subsequently,tracingswereperformedonthe radiographs,basedonHeliovaaraetal.6(Fig.1),whichwere thencomparedtoobservethe changesinsofttissues.For that purpose, the lateralcephalometric radiographs were performed usingstandardized method, obtained with the patient positioned in the Frankfurt plane, with occluded molarsandlipsatrest,preoperativelyandsixmonthsafter surgery.
Afterobtainingtheradiographs,acephalogramwas cre-ated, adapting an18cm×24cmsheet ofultraphan paper
andthen,witha0.5pencil,anatomicalstructuresand land-marksweretracedonthelightbox.TheSpoint(centerof sella),Npoint(nasion),theSNlines;theXaxis(horizontal linestartingatpointN,ascending7◦oftheSNline);Yaxis (vertical line perpendicular to the horizontal line passing throughtheSpoint)weretracedinthiscephalogram, corre-spondingtostructuresthatarenotalteredbysurgery,which serveasreferenceformovementanalysisofthestructures alteredbysurgery.
Then maxillary landmarkswere identified:PNS (poste-riornasalspine),A(deepestpointintheanteriorcontourof themaxillaryalveolararch),andthePRpoint(prosthion ---themostanterior---inferiorpointoftheupperdentoalveolar margin). Postoperativemaxillarypositionwasobtainedby thedistancesbetweenX,Y,andthePNSaxes;X,Y,andA axes;andX, Y,and PRaxes.Changes insofttissues were evaluatedusingthePRNpoint (mostanteriorpointof the nasaltip),measuringthedistance betweenthispoint and thereferencelinesXandYandtheSnPrnangle(Fig.1). Sta-tisticalanalysisconsistedof box-plotandpaired Student’s t-test,withsignificancesetat5%.
ThestudywasapprovedbytheUniversityEthics Commit-tee(178/02).
Results
Inthepresentstudy,thesampleconsistedof20patients(12 womenandmen).Themeanagewas21.4years(minimum 14andmaximum37).TwentypatientshadclassIIIskeletal deformities.
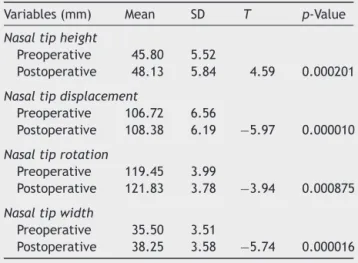
Therewasanelevationofthenasaltipin85%ofpatients, anadvancementofthenasaltipin80%,anincreaseinthe rotationangleofthenasaltipin80%,andincreasednasal widthin95%(Table1).
Inmostcases,thereweremodificationsinthenasaltip, increasednasalwidth,andupwardnasalrotation,according totheamount of maxillaryadvancement,and anterioror posteriorimpaction(Table2).
Table 1 Student’st-testfor nasal height, displacement, androtation;andnasalbasewidth.
Variables(mm) Mean SD T p-Value
Nasaltipheight
Preoperative 45.80 5.52
Postoperative 48.13 5.84 4.59 0.000201
Nasaltipdisplacement
Preoperative 106.72 6.56
Postoperative 108.38 6.19 −5.97 0.000010
Nasaltiprotation
Preoperative 119.45 3.99
Postoperative 121.83 3.78 −3.94 0.000875
Nasaltipwidth
Preoperative 35.50 3.51
Postoperative 38.25 3.58 −5.74 0.000016
Surgicalmanipulation Variablesanalyzed
Mod.nasaltip Increasednasalwidth Nasalrotation Totaln(%) Yesn(%) Non(%) Yesn(%) Non(%) Upn(%) Downn(%) Non(%)
Maxillaryadvancement 16(84.21) 3(15.79) 17(89.47) 2(10.53) 13(68.42) 2(10.53) 4(21.05) 19(100.00) Upto6mm 12(63.16) 3(15.79) 13(64.40) 2(10.53) 10(52.63) 1(5.26) --- 15(78.95) >6.1mm 4(21.05) --- 4(25.07) --- 3(15.79) 1(5.27) --- 4(21.05) Posteriorimpaction 16(80.00) 4(20.00) 18(90.00) 2(20.00) 13(65.00) 2(10.00) 5(25.00) 20(100.00) Upto2mm 7(32.00) 2(10.00) 8(40.00) 1(10.00) 6(30.00) --- --- 9(45.00) >2.1mm 9(48.00) 2(10.00) 10(50.00) 1(10.00) 7(35.00) 2(10.00) --- 11(55.00) Anteriorimpaction 14(87.50) 2(12.50) 16(100.00) --- 13(81.25) 2(12.50) 1(6.25) 16(100.00) Upto2mm 4(25.00) 4(25.00) --- 4(25.00) --- --- 4(25.00) >2.1mm 10(62.50) 2(12.50) 12(75.00) --- 9(56.25) 2(12.50) --- 12(75.00)
Regardingthesofttissuesofthenasalregion,adecrease intheX-Prnaxisdistancemeasurementwasobservedfrom thepre-tothepostoperativeperiod,indicatinganelevation ofnasaltipin85%ofcases.Aftercomparingthepre-and postoperativemeasurementsoftheY-Prnaxis,anincrease ofthisdistancewasobservedbetweenthetwoevaluations, indicatingthatadvancementofthenasaltipwasobserved in80%ofcases.
After comparingthe measurements of the SnPrn angle pre-andpostoperatively,therewasanincreaseinthe mea-surementoftheangle,indicatinganupwardrotationofthe nasaltipin80%ofcases,downwardrotationin10%,andno rotationofthenasaltipin10%ofpatients.Themeasurement ofpostoperativenasalwidthincreasedin95%ofcases.
Discussion
The correctionof dentofacial deformities through orthog-nathicsurgeryaimstoprovide amore functional maxilla-mandibular relationship and, consequently, improve the patient’sfacialharmony.
Le Fort I osteotomy is indicated for the mobilization of the maxilla in the three spatial planes, allowing the correction of several deformities. In the present study, this treatment was used for maxillary advancement and impactioninpatientswithclassIIandIIIdeformities.7---11All patientshadpostoperativealterations inthenasalregion, whichisinagreementwiththeliterature.3
Maxillary superior repositioning and advancement can cause nasal tip elevation and augmentation of the alar base.6Regardlessoftheamountofmaxillaryadvancement, andanteriororposteriorimpaction,inmostcasestherewas modification of the nasal tip, increased nasal width, and upwardnasalrotation.Aprobableexplanationforthisfact is that there wasa new positioning of the anteriornasal spineand,withthedissectionofsofttissues,thestandard preoperativemeasureswerepartiallylost,generatingslight distortions.
Bimaxillary surgery5 may be a good option when the anteroposterior discrepancy is greater than 8mm, which was not the case in the present study. Aydil et al.5 reportedthataLeFortIsurgerytogetherwithmandibular
sagittalosteotomy,whenindicatedformandibular advance-ment,significantlyaffectedtheverticalandanteroposterior position of the maxilla and mandible, respectively. When performed in combination, these surgical techniques can efficiently change the position of the upper incisors and nasalpositioninboththeverticalandanteroposterior direc-tions. Bimaxillary orthognathic surgery seems to be an efficientmethodtoobtainsatisfactoryresultsinthe appear-ance of soft,dental, andskeletal tissues,associatedwith facial profile in patients with high angle Class II skeletal deformity.
Araújo1comparedcephalometricpointsinpre-and post-operative lateral radiographs, observing that in maxillary advancementsurgeries,themostanteriorpointofthenose ischangedhorizontallyby30%,andifthealarbasesuture is performed, itmay reach35%.Regarding thefindings of thisexperiment,ameanratioof40%wasobservedamong patients who underwent surgery, although some patients demonstratedaverydifferentresult,eitherhigherorlower (0---90%),asallpatientsalsounderwentrepositioningofthe uppermaxillaandalarbasesuture,with3-0prolenesuture, fixingtheinnerregionoftherightandleftalarbases,while thelipwassuturedusingconventionalsuturesorV-Y, accord-ingtothepatient’sfacialtype;thisaspectisveryimportant inorderforthepatienttohaveanosethatisproportionalto therestoftheface,resultinginamoreharmonious appear-ance.
Themaxillacanbeimpactedinmostcaseswithout com-promisingairflow.12,13Theenlargementoftheanteriornasal area,reducingairresistanceevenafterthenasalskeletonis reduced,mayexplainthesignificantimprovementinnasal breathingaftermaxillaryimpaction.14,15Evenifthereisgain intheanteriornasalareaduetoanteriormobilizationofthe maxillaaftersurgery,theauthorsagreewithBottinietal.4 regarding thenon-performance ofrhinoplasty at thetime oforthognathicsurgerytocorrectpre-existingdefects,such asadorsal hump,averybroad orverynarrownasalbase, adeviationofthenasalpyramid,orothercosmeticdefects resultingfromtheorthognathicsurgery.
canbeusedfor thistypeof diagnosis.The patientin this study,a14-year-oldfemale,underwentsurgeryafterbeing assessedbyanendocrinologist,whenherwristradiographs werereviewed, upon which it wasobserved thatshe was alreadyinthefinalstageofgrowth.
Some aspects of the surgical technique may interfere withnasalbreathingandshape,suchasremovalofthebony andcartilaginousseptumtopreventinterferenceand devi-ationsinthemaxilla,removalofhypertrophiedturbinates, expansionofthepiriformaperture inpatients withalong faceinordertoincreasethenasalcavity,andsutureofthe nasalbase.2
Consideringtheseaspects,itis mandatorytointerview thepatientpre-andpostoperativelytodiscoverwhattheir actualestheticandfunctionalexpectationsare,aswellasto explainthepossibleappearanceoutcomesoforthognathic surgery.
Conclusion
Surgeriesofadvancementandsuperiorrepositioningofthe maxilla tend to cause elevation and advancement of the nasaltip,aswellasenlargementofthenasalbase.
Conflicts
of
interest
Theauthorsdeclarenoconflictsofinterest.
References
1.Araújo MM, PasseriLA, Araújo A. Pre and post cephalomet-ricanalysisofthedivineproportions ofFibonacciinpatients treatedbyamandibular advancement.Dent PressJOrthod. 2001;6:29---36.
2.MoloneyF, Worthington P.The origin of the LeFort I max-illary osteotomy: Cheever operation. J Oral Surg. 1981;39: 731---4.
3.MommaertsMY,Lippens F,AbeloosJV, NeytLF.Nasalprofile changesaftermaxillaryimpactionandadvancementsurgery.J OralMaxillofacSurg.2000;58:470---5.
4.BottiniDJ,Gentile P,CervelliG,CervelliV.Changesinnasal profilefollowingmaxillomandibularosteotomyforprognathism. Orthodontics(Chic).2013;14:e30---8.
5.AydilB,ÖzerN,Mars¸anG.BimaxillarysurgeryinclassIII maloc-clusion:softandhardtissuechanges.JCraniomaxillofacSurg. 2013;41:254---7.
6.HeliövaaraA, HukkiJ,RantaR, RintalaA.Soft tissueprofile changesafterLeFortI osteotomyin UCLPpatients.J Cran-iomaxillofacSurg.2000;28:25---30.
7.BellWH.LeFortIosteotomyforcorrectionofmaxillary defor-mities.JOralSurg.1975;33:412---26.
8.BellWH.Revascularizationandbonehealingafteranterior max-illary osteotomy:a studyusing adultrhesusmonkeys.JOral Surg.1969;27:249---55.
9.Bell WH, Levy BM. Revascularization and bone healing after posteriormaxillaryosteotomy.JOralSurg.1971;29:313---20.
10.Bell WH.Biologicbasisfor maxillary osteotomies.AmJPhys Anthrop.1973;38:279---89.
11.LiKK,MearaJG,AlexanderJRA.Locationofdescending pala-tinearteryintherelationtotheLeFortIosteotomy.JOral MaxillofacSurg.1996;54:822---5.
12.Turvey TA, Hall DJ, Warren DW. Alterations in nasal airway resistancefollowingsuperiorrepositioningofthemaxilla.AmJ Orthod.1984;85:109---14.
13.TurveyTA,EarrenDW.Impactofmaxillaryosteotomiesonnasal breathing:orthognaticsurgery.OralMaxillofacSurgClinNoth Am.1990;2:831---41.
14.GuenthnerTA,SatherAH,Kern EB.TheeffectofLeFortI ---maxillaryimpactiononnasalairwayresistance.AmJOrthod. 1984;85:308---15.
15.Erbe M,Lehotay M, GödeU, WigandME, NeukamFW. Nasal airwaychangesafterLeFortI---impactionandadvancement: anatomicalandfunctionalfindings.IntJOralMaxillofacSurg. 2001;30:123---9.