RevBrasAnestesiol.2015;65(4):306---309
REVISTA
BRASILEIRA
DE
ANESTESIOLOGIA
OfficialPublicationoftheBrazilianSocietyofAnesthesiology www.sba.com.brCLINICAL
INFORMATION
Bilateral
subdural
hematoma
secondary
to
accidental
dural
puncture
Sofía
Ramírez
∗,
Elena
Gredilla,
Blanca
Martínez,
Fernando
Gilsanz
ServiciodeAnestesiologíayReanimación,HospitalUniversitarioLaPaz,Madrid,Spain
Received25May2014;accepted4July2014 Availableonline28April2015
KEYWORDS
Accidentaldural puncture;
Epiduralanalgesia; Post-duralpuncture headache;
Subduralhematoma; Epiduralbloodpatch
Abstract
Wereportthecaseofa25-year-oldwoman,whoreceivedepiduralanalgesiaforlaborpainand subsequently presentedpost-dural punctureheadache. Conservativetreatment was applied andepiduralbloodpatchwasperformed.Intheabsenceofclinicalimprovementanddueto changesintheposturalcomponentoftheheadache,abrainimagingtestwasperformedshowing abilateralsubduralhematoma.
Thepost-duralpunctureheadacheisrelativelycommon,butthelackofresponseto estab-lished medicaltreatment aswell as the change in its characteristics andthe presence of neurologicaldeficit,shouldraisethesuspicionofasubduralhematoma,whichalthoughisrare, canbelethalifnotdiagnosedandtreatedattherighttime.
©2014SociedadeBrasileiradeAnestesiologia.PublishedbyElsevier EditoraLtda.Allrights reserved.
PALAVRASCHAVE
Dura-Máter; Analgesiaepidural; Cefaleiapós-punc¸ão dural;
Hematomasubdural; Placadesangue epidural
Hematomasubduralbilateralsecundárioapunc¸ãoduralacidental
Resumo
Apresentamosocasoclínicodeumapacientede25anosdeidade,naqualumatécnicaperidural foirealizada duranteotrabalhode partoeposteriormenteapresentou cefaleiacom carac-terísticas de cefaleia pós-punc¸ão dural. Foi iniciado tratamento conservador e tampão de sangueperidural.Devidoaausênciademelhoraclínicaeàmudanc¸adocomponente postu-raldacefaleia,decidiu-serealizarumexamedeimagemcerebralquedemostrouapresenc¸a dehematomasubduralbilateral.
Acefaleiapós-punc¸ãodural érelativamentefrequente,mas afaltade respostaao trata-mentomédicoinstaurado,assimcomoamudanc¸aemsuascaracterísticaseapresenc¸adefoco
∗Correspondingauthor.
E-mail:sofiramirez@gmail.com(S.Ramírez).
http://dx.doi.org/10.1016/j.bjane.2014.07.017
Bilateralsubduralhematomasecondarytoaccidentalduralpuncture 307
neurológico,devemlevantarasuspeitadepresenc¸adeumhematomasubduralque,embora infrequente,podechegaraserdevastadorsenãofordiagnosticadoetratadooportunamente. ©2014SociedadeBrasileira deAnestesiologia.PublicadoporElsevierEditoraLtda.Todosos direitosreservados.
Introduction
Thepost-duralpunctureheadache(PDPH)isthemost com-moncomplication aftera neuroaxial1 anesthesia. Inturn,
the subdural hematoma (SDH) is a rare, but potentially severecomplicationofduralpuncture,whichrequiresearly diagnosis and treatment. Initially the diagnosis of SDH is complicated because the early symptoms are similar to thoseofPDPH,butwhentheheadachedoesnotrespondto standardmedicaltreatment,losingitspostural characteris-ticsorbeingaccompaniedbyotherneurologicaldisorders, itis necessarytosuspectof anintracranial pathologyand urgentlyperformaneuroimagingscantoallowdiagnosisand correcttreatment.
Clinical
case
A25-five-year-oldwoman,gestathreeat39thweekof gesta-tion,wasadmittedtohospitalduetoearlyuterineactivity. Herpersonalhistorypointedoutthatin herfirstbirthshe did not receive epidural analgesiadue to impossibilityof performingthetechnique.Withacervicaldilationof2cm, andafter gynecological evaluation,the patientrequested epiduralanalgesiatocontrollaborpain.Withprior expla-nationoftherisks,andaftersigninginformedconsent,an epiduraltechniquewasperformed.Aftervariousattempts, usinga18GTuohyneedleandlossofresistancetoair,the epiduralspacewaslocatedat L3---L4andthecatheterwas leftin this position. Following a negative aspirationtest, adosetest of3mLbupivacaine0.25%withepinephrine1: 200,000wasadministeredwithnohemodynamicchangesor immediatesensoryormotorblockade.Theinitialdosewas 0.25%levobupivacaine10mLandthenanepiduralinfusion of0.125%levobupivacaine+fentanila2gmL−1at10mLh−1
wasconnected.
Laborwasuneventfuland2hlater,aftereutocicbirth,a girlof3090gwasbornwithApgarscore8at1minand9at 5min.Afterstayingforsurveillanceinpostpartumarea,the epiduralcatheterwasremoved,andthepatientwenttothe room.
With24h postpartumtheanesthesiaservice wascalled becausethepatienthadsevereheadache,withappreciation of pain in simple verbal scale (SVS) 9/10, which wors-enedwithstandingpositionandimprovedwhenrecumbent. Althoughduramaterpuncturehasnotbeennoticed,there was suspicion of a possible PDPH and with this supposed diagnosis analgesic treatment wasstarted with paraceta-mol1gIV/6handdexketoprofen50mgIV/8h.After48hof headacheonset,duetopersistentsymptomsdespite medi-caltreatmentadministeredanddiagnosisofPDPH,epidural blood patch (EBP) was performed with no other events.
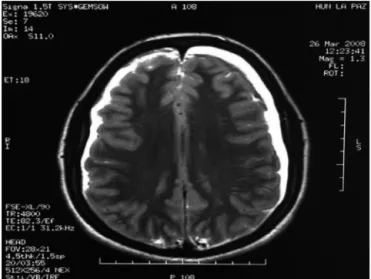
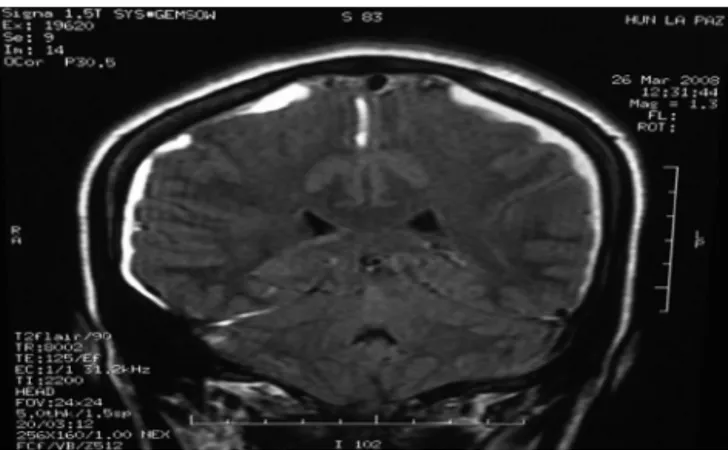
Initially, the results were satisfactory, since the patient reportedimprovementin headacheduringthefirst hours, but the next day she showed non-orthostatic headache, withmaximumintensityinthesupineposition,inSVS10/10 associated withtinnitus and cervical contracture. Due to lack of clinical improvement, with change of headache characteristics and after ruling out neurological focus on physicalexamination,brainandlumbarspinenuclear mag-neticresonance(MRI)wasordered,whichshowedbilateral intracranialSDH(Figs.1and2).The NeurosurgeryService wasconsulted,indicatingtreatmentwithIVcorticosteroids (dexamethasone4mgIVevery8h)andrequestingcomputed tomography(CT)controlinaweek.
With 24h of treatment initiation with corticosteroids, thepatient reportedimprovementin headache, SVS3/10 and after 48h she reported no headache or other symp-toms.Thepatientremainedinhospitalforanotherweekfor medicaltreatmentandmedicalsupervision.Controlcranial CTshowedimprovementoflesionsandduetosatisfactory progress,withtotalremissionofheadacheandwithoutthe presenceofneurologicalfocus,shewasdischargedwith cor-ticoidoraltreatmentinadescendingregimenduring20days andcontrolbyneurosurgeryservice.
Discussion
Theincidenceofaccidentalduralpuncturedescribedinthe literatureafterperformanceofanepiduraltechniquevaries from0.4to6%,2butonly60%ofpatientsdevelopPDPH.3In
ouranesthesiaserviceatMaternalHospitalLaPaznumbers
308 S.Ramírezetal.
Figure2 Coronalsectionofbrainmagneticresonancewhere bilateralsubduralhematomaisobserved.
aresimilar,withanincidenceofaccidentalduralpuncture of0.6%,andofPDPHof56%.4
According tothe diagnostic criteriaestablished by the International Headache Society, PDPH is characterized by itsposturalcharacter,worseningatthe15minofstandingor sittingposition,andimprovinginasimilartimewith decu-bitus; it develops within 5 daysof puncture and resolves spontaneouslywithinaperiodofoneweek in95%ofcases orinthefollowing48hoftheperformanceofanEBP.3
The SDHis ararebut potentially fatal complicationof duralpuncture, asaresultof a spinalanesthesiaor acci-dentalduralpunctureduringepiduraltechnique.2Although
theliteraturecollectsonlyisolatedcasesofSDHsecondary toneuroaxialanesthesia,itisestimatedthattheprevalence ofthisconditionis1/500,000---1/1,000,000.5
PostulatedmechanismsforPDPHandSDHaresimilar:the lossofcerebrospinalfluid(CSF)throughtheholecreatedin the dura mater causes a reduction of volume and subse-quentlyinspinalandintracranialpressure.Thisintracranial hypotensioncausesacaudaldisplacementofthespinalcord andthebrain,withtractionofbrainstructuresthatare sen-sitive topain,thereby causing the headache.The venous drainageofthebrainisperformedthroughtheveinsinthe duralbridges,thatrunfromthebrainintotheduralsinuses, and that have their weakest part in the subdural space, and it is precisely the traction of these veins that cause theirdetachmentandsubsequentemergenceofaSDHand increasedintracranialpressure.6Thus,inpatientswithSDH,
twoclinicalphasescanbeobservedasaresultofchanges generated on intracranial pressure: initially they present witha headachewitha clearposturalcomponent (associ-ated withintracranial hypotension). In a later stage they showincreasedintensityofheadachewithlossoforthostatic component,withoutimprovementwiththeusualtreatment ofPDPHandincludingclinicalworseningafterperformance of an EBP and that may be accompanied by neurological focussigns(relatedtointracranialhypertension).1
Conventional treatment of PDPH includes the adminis-trationofanalgesicsandantiemetics.Incaseofpersistent headachedespitethesemeasures,anEBPcanbeperformed, whichiscurrentlyconsideredthedefinitivetreatmentofthis clinicalentity.Thepostulatedmechanismforitsefficacyis dual:firstitcompressesthethecalsac,increasingthe pres-sureonthelumbarneuraxialchannel,leadingtothepassage
ofCSFfromthespinalcanaltothebrainandtherebycausing improvementofheadache;ontheotherhand,maintenance ofthetherapeuticeffectisattributedtotheformationofa clotwhichpreventsescapeofCSF.3
Inourhospitalweperformed theEBPincaseof severe PDPH that persists 48h after puncture and initiation of analgesic treatment.The procedure consistsofmakingan epidural puncture, preferably in the same intervertebral spacewheretheaccidentalduralpuncturewasperformed orbelow,andoncetheepiduralspaceislocated,15---20mL ofautologousbloodfromaforearmveinisaseptically col-lected, and is injected through epidural route, with care beingtakentostopinjectionifthepatientcomplainsofback painor pain inthe lowerlimbs. Subsequentlythepatient shouldremainsupineforonehourintheresuscitationarea. Regarding the diagnosis of SDH after accidental dural puncture,itisimportanttonotethatifthereisaheadache thatdoesnotrespondtousualtreatmentfor PDPH,which losesitsposturalcharacter(orthostaticornon-orthostatic), whichworsensafterthecompletionofaEBPorthat reap-pearsafter remission,an intracranial complicationshould besuspected,andaneuroradiologystudy---brainCTorMRI --- shouldbeperformedtoruleoutthepresenceofaSDH.7As
forthesediagnostictests,itwasshownthatbothCTandMRI inisodensephasemaynotshowthepresenceofaSDH,and thereforetheyshouldbeperformedwithcontrasttoavoid false negativesin their results.1,8 This was theprocedure
thatwasfollowedinourpatient’scase.
TreatmentofSDHcanbemedicalorsurgical,depending onitssizeandtheseverityofsumptoms.2Mostofthetime,
small(<5mm)and littlesymptomatic hematomasrespond clinicallyandradiologicallysatisfactorilywithconservative medicaltreatment.Ontheotherhand,patientswithlarger hematomas andmarkedneurological deteriorationusually requireurgentsurgicaldrainage.9,10Inourcase,thepatient
hadnoneurologicalfocus,soaconservativeapproachwas chosen,withgoodclinicalresults.
In conclusion, after an accidental dural puncture, the presence of severe, progressive headache, with changing of itsposturalcomponent,noimprovementor even wors-ening after thecompletion of a EBP, andassociated with other neurological signs,awarningsign should be consid-eredforintracranialcomplications,asitisforSDH.Thisisan infrequentsituation,butcanbecomecatastrophic, produc-ingpersistentneurologicalsequelaeandevendeath.Thus, itisnecessarytoinsistonearlydiagnosisandtreatmentof thisclinicalentity.
Conflict
of
interests
Theauthorsdeclarenoconflictofinterest.
References
1.Zeidan A, FarhatO, Maaliki H, et al. Does postdural punc-ture headache left untreated lead to subdural hematoma? Casereportandreviewoftheliterature.IntJObstetAnesth. 2006;15:50---8.
Bilateralsubduralhematomasecondarytoaccidentalduralpuncture 309
3.GaiserRR. Postduralpunctureheadache:aheadachefor the patientandaheadachefortheanesthesiologist.CurrOpin Anes-thesiol.2013;26:296---303.
4.MartínezSerranoB[thesis]Cefaleapostpunciónduraltras anal-gesia epidural para trabajo de parto. Madrid: Facultad de Medicina,UniversidadAutónoma;2006.
5.MachurotPY,VergnionM,FraipontV,etal.Intracranialsubdural hematomafollowingspinalanesthesia:casereportandreview oftheliterature.ActaAnaesthesiolBelg.2010;61:63---6.
6.KK,ChatterjeeN,ShrivastavaA,etal.Sub-duralhematoma fol-lowingspinalanesthesiatreatedwithepiduralbloodpatchand burr-holeevacuation:acasereport.MiddleEastJAnesthesiol. 2013;22:117---20.
7.Liang MY, Pagel PS. Bilateral interhemispheric subdural hematomaafterinadvertentlumbarpunctureinaparturient. CanJAnaesth.2012;59:389---93.
8.Vaughan DJ, Stirrup CA, Robinson PN. Cranial subdural haematoma associated with dural puncture in labour. Br J Anaesth.2000;84:518---20.
9.Abbinante C, Lauta E, di Venosa N, et al. Acute subdural intracranialhematomaaftercombinedspinal-epidural analge-siainlabor.MinervaAnestesiol.2010;76:1091---4.