Open Access Article│www.njcmindia.org pISSN 0976 3325│eISSN 2229 6816
National Journal of Community Medicine│Volume 3│Issue 4│Oct – Dec 2012 Page 736
Original Article
▌
ROLE OF ZINC SUPPLEMENTATION IN GROWTH AND
NEURO-DEVELOPMENT OF PREMATURE AND SMALL
FOR GESTATIONAL AGE (SGA) BABIES
Parakh Manish1, Gupta BD2, Bhansali Suman3, Parakh Poonam4, Sharma Pramod1, Gurjar Manisha5,
Chhangani Narendra3
Financial Support: None Declared
Conflict of interest: None Declared
Copy right: The Journal retains the copyrights of this article. However, reproduction of this article in the part or total in any form is permissible with due
acknowledgement of the source.
How to cite this article:
Parakh M, Gupta BD, Bhansali S, Parakh P, Sharma P, Gurjar M: Role of zinc supplementation in growth and neuro-development of
premature and small for gestational age (SGA) babies. Natl J
Community Med. 2012; 3(4):736-9.
Author’s Affiliation:
1 Associate Professors, 2 Professor
and Head (retd), 3Professor, 4Assistant Professor, 5Senior
Demonstrator, Department of Paediatrics, Umaid Hospital for Women and Children, Dr S.N. Medical College, Jodhpur
Correspondence:
Dr Suman Bhansali,
Email: manparkh@hotmail.com
Date of Submission: 1-11-12
Date of Acceptance: 25-12-12
Date of Publication: 30-12-12
ABSTRACT
Objectives: A negative Zinc balance exists in preterm and small for gestational age infants. The current study evaluates the role of zinc supplementation on growth and neurodevelopmental outcome of these infants.
Methods: One hundred and twenty eight infants who were born either premature and/or small for gestational age were followed for six months. A detailed assessment of anthropometry, neurodevelopment and morbidity patterns due to Diarrhea and Acute Respiratory Infection were recorded during each visit.
Results: At birth and at six months the mean serum Zinc level in the study and control group was 0.87±0.398, 1.03±0.567, 0.88±0.248, 0.83±0.355mg/L respectively. The SZnR 6/B is significantly higher in study group as compared to controls (1.153 ± 0.55 Vs 0.913±0.438, p<0.01) suggesting better maintained serum zinc levels in zinc supplemented infants. Zinc supplemented exclusively breast fed infants had significantly higher SZnR 6/B as compared to non supplemented exclusively breast fed infants (1.555±0.654 vs 0.850±0.406,p<0.01). Further Zinc supplemented exclusively breast fed infants had significantly higher SZnR 6/B as compared both Zinc supplemented mixed and top fed infants. No effect of zinc supplementation was observed on growth, neurodevelopmental out come and morbidity pattern due to Diarrhea and ARI.
Conclusion: It can be concluded from the present study that zinc supplementation and exclusive breast feeding in premature and/or SGA infants results in better serum Zinc ratio. However Zinc supplementation has no role in the growth or neurodevelopmental outcome or morbidity patterns due to acute diarrhea and respiratory infections of premature and/or small for gestational age infants. But the breast milk has a definite value to improve morbidity patterns due to diarrhea in these infants
Key words: Zinc Supplementation, Small for Gestational Age (SGA), Premature infants
GLOSSARY:
SGA: Small for Gestational Age ARI: Acute Respiratory Infection
SZN R 6/B: Ratio of serum zinc level at birth and at 6 months of age
CDS: Corrected Development Score
INTRODUCTION
Open Access Article│www.njcmindia.org pISSN 0976 3325│eISSN 2229 6816
National Journal of Community Medicine│Volume 3│Issue 4│Oct – Dec 2012 Page 737 infants until approximately 36 weeks of
gestation.1,2Several workers have recorded an improved Zinc status, good weight gain and better linear growth velocities in preterm infants supplemented with Zinc.3,4,5,6 Whether the effect of Zinc is a direct consequence of improved supply of this nutrient for growth and metabolism or is mediated through stimulation of appetite and /or less diarrhoeal episodes is unclear.
The current study was planned to evaluate the importance of Zinc supplementation in growth, development and morbidity pattern of preterm and SGA babies with the objectives to determine the serum Zinc levels at birth and compare the values at six months of age. The study also attempted to find out correlation, if any, between babies supplemented with Zinc compared with a control group for neuro-developmental outcome, number of episodes of diarrhea, acute respiratory infections (ARI) and other morbidity. Role of exclusive breast feeding in prevention of Zinc deficiency was also studied.
METHODS
A total of 176 consecutively born preterm and SGA babies were enrolled in the study and followed up for a period of one year. Babies with congenital malformations, asphyxia, congenital infections and babies whose mothers had diabetes or pre-eclampsia were excluded. An informed verbal consent was obtained from the parents. The babies were alternately assigned to group A and B with infants in Group A receiving 0.8mg/kg of elemental Zinc per day from birth to 6 months of age and infants in Group B supplemented with a multivitamin solution not containing Zinc. Parents were counselled to exclusively breast feed their babies till 6 months of age. All episodes of diarrhoea, acute respiratory infections and other morbidity were recorded in the proforma during their monthly follow up visits. Zinc levels were assessed in the serum within 3 days of birth and again at 6 months of age. The estimation was done using atomic absorption spectrophotometry.7
Babies were followed up monthly in well baby clinics for their anthropometry, morbidity pattern and compliance of supplemental Zinc or multi-vitamin syrup. Development of these infants was assessed using the Woodside scale of development.8 Statistical analysis was done using the Student’s t test and the Z test to assess the
significance of difference in mean between the two variables.
OBSERVATIONS
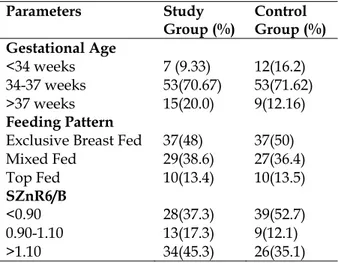
The study cohort consisted of 75 babies in the study group (Group A) and 74 babies in the control group (Group B) who could complete the study period. Two babies died during the study period of 6 months and a total of 25 babies from both groups (14 and 11 respectively) dropped out of the study for various reasons. Babies were further categorised into three groups based on their feeding pattern-exclusively breast fed, top fed or mixed feeding groups. Maximum babies in both the groups (A and B) were exclusively breast fed (Table 1).
Table 1: Distribution of infants according to gestational age, feeding pattern and Serum Zn Ratio
Parameters Study Group (%)
Control Group (%) Gestational Age
<34 weeks 7 (9.33) 12(16.2) 34-37 weeks 53(70.67) 53(71.62) >37 weeks 15(20.0) 9(12.16) Feeding Pattern
Exclusive Breast Fed 37(48) 37(50)
Mixed Fed 29(38.6) 27(36.4)
Top Fed 10(13.4) 10(13.5)
SZnR6/B
<0.90 28(37.3) 39(52.7)
0.90-1.10 13(17.3) 9(12.1)
>1.10 34(45.3) 26(35.1)
Open Access Article│www.njcmindia.org pISSN 0976 3325│eISSN 2229 6816
National Journal of Community Medicine│Volume 3│Issue 4│Oct – Dec 2012 Page 738 The ratio was significantly higher in the study
group compared to the control group (p<0.01) (Table No.2). The mean SZN R 6/B amongst the exclusively breast fed infants in the study group (1.55±0.654) was significantly higher as compared to the mixed fed (1.157±0.424;p<0.01) and top fed groups(1.134±0.489; p<0.02) respectively.
The mean weight at birth of both the groups was comparable (p>0.05). At six months of age the
mean weight in group A was higher as compared to group B, but the difference was not statistically significant (Table No.2). No effect of Zinc supplementation was observed on mean head circumference, length and mid arm circumference in the current study (Table No.2). However mean increment in weight in the study group was better in exclusively breast fed infants compared to mixed fed (p<0.001) or top fed babies (p<0.001).
Table 2: Serum Zinc level and its effect on growth
Parameters At Birth At 6months
Group A Group B Group A Group B
Mean Serum Zinc (mg/L) 0.87±0.398 1.03±0.567 0.88±0.248 0.83±0.355
Mean SZnR6/B --- --- 1.153 ±0.55 0.913± 0.438
Mean Weight (Kg) 1.79±0.20 1.72±0.32 4.962±0.75 4.77±0.75
Mean Head Circumference(cms) 30.37±1.65 29.88±1.52 41.13±1.53 41.15±1.42
Mean Length(cms) 44.49±2.15 43.97±2.40 62.27±1.73 61.95±2.23
Mid Arm Circumference (cms) 7.51±1.13 7.26±0.58 11.78±0.71 11.65±1.54
All value in mean±SD format
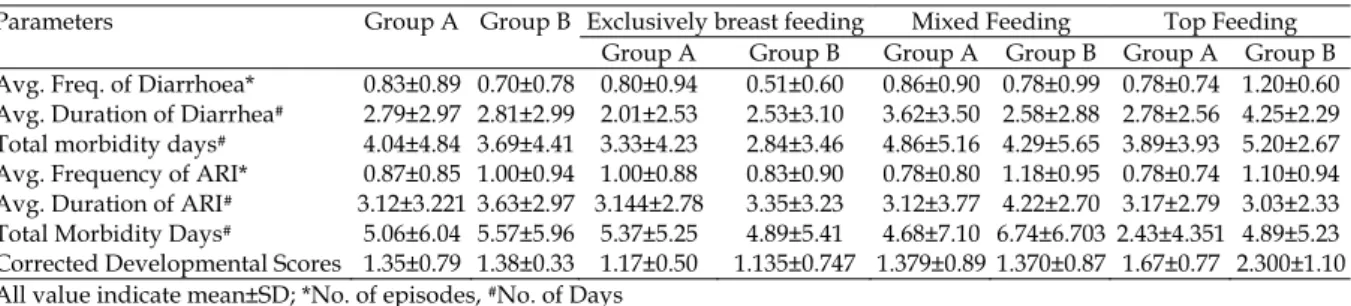
Average frequency and duration of episodes of diarrhoea and total morbidity days in the two groups were not significantly different (p >0.05) (Table No.3). But it was seen that the infants in control group who were exclusively breast fed had statistically significant lower episodes of diarrhoea (p<0.01) and duration of total
morbidity days (p<0.05) as compared to those who were only top fed (Table No.3). There was no statistically significant difference in the morbidity patterns due to ARI among infants in both the groups and among the infants who had different patterns of feeding in either study or control group(Table No.3).
Table 3: Effect of zinc and feeding pattern on morbidity due to diarrhea, ARI and neurodevelopmental outcome
Parameters Group A Group B Exclusively breast feeding Mixed Feeding Top Feeding Group A Group B Group A Group B Group A Group B Avg. Freq. of Diarrhoea* 0.83±0.89 0.70±0.78 0.80±0.94 0.51±0.60 0.86±0.90 0.78±0.99 0.78±0.74 1.20±0.60 Avg. Duration of Diarrhea# 2.79±2.97 2.81±2.99 2.01±2.53 2.53±3.10 3.62±3.50 2.58±2.88 2.78±2.56 4.25±2.29
Total morbidity days# 4.04±4.84 3.69±4.41 3.33±4.23 2.84±3.46 4.86±5.16 4.29±5.65 3.89±3.93 5.20±2.67
Avg. Frequency of ARI* 0.87±0.85 1.00±0.94 1.00±0.88 0.83±0.90 0.78±0.80 1.18±0.95 0.78±0.74 1.10±0.94 Avg. Duration of ARI# 3.12±3.221 3.63±2.97 3.144±2.78 3.35±3.23 3.12±3.77 4.22±2.70 3.17±2.79 3.03±2.33
Total Morbidity Days# 5.06±6.04 5.57±5.96 5.37±5.25 4.89±5.41 4.68±7.10 6.74±6.703 2.43±4.351 4.89±5.23
Corrected Developmental Scores 1.35±0.79 1.38±0.33 1.17±0.50 1.135±0.747 1.379±0.89 1.370±0.87 1.67±0.77 2.300±1.10 All value indicate mean±SD; *No. of episodes, #No. of Days
The corrected development score (CDS) of the study group differed non significantly from control group (Table No.3), but it was significantly better ( p < 0.001 ) in the breast fed control group babies compared to the babies who received only top milk (Table No.3).
DISCUSSION
Mild subclinical Zinc deficiency is frequent in infants and its role in growth and neurodevelopment has been much talked about. Increasing values of mean serum Zinc levels at
Open Access Article│www.njcmindia.org pISSN 0976 3325│eISSN 2229 6816
National Journal of Community Medicine│Volume 3│Issue 4│Oct – Dec 2012 Page 739 serum Zinc levels from birth to 6 months of age.
In our study 37.3 % babies in the supplemental group and 52.7 % babies in group B had the ratio < 0.9, but supplementation of Zinc did show a favourable effect on the Zinc balance in the body. Human breast milk contains a special Zinc binding ligand which increases the bioavailability of Zinc to the infant. Mothers of preterm babies have higher levels of Zinc throughout lactation to meet the increased requirement of these infants.11
In the current study we observed that serum Zinc ratio (SZN R 6/B) in the supplemented group was better compared to the control (Table No. 2). Castillo Duran et al4 in their pioneer study had similar observations. Similarly, mean serum Zinc ratio (SZN R 6/B) was significantly higher in the Zinc supplemented exclusively breast fed infants.
We tried to study the effect of Zinc supplementation on physical growth but did not note statistically significant difference (Table No.3). This was in contrast to the observations of Castillo Duran et al4 and Islam et al6 who demonstrated significantly higher increments in the supplemented groups. This was probably because of non existence of subclinical deficiency in our infants as the serum Zinc levels were normal at birth and better maintained throughout the first eight months of life. But we could establish that exclusive breastfeeding is a more crucial factor determining increments in weight during the first 6 months of life.
The observations that Zinc supplementation has no effect on reducing the frequency and duration of acute diarrhea in the current study was in contrast to those made by Islam et al6, Osendarp et al12 and Sur et al13. They demonstrated that Zinc supplementation was effective in reducing diarrhea incidence.
CONCLUSION
Thus it can be concluded from the present study that Zinc supplementation in premature and/or small for gestational age infants results in better serum Zinc ratio. Further, it has been clearly demonstrated in the current study that breast milk has an additive effect on maintenance of higher serum Zinc levels at six months of age among Zinc supplemented premature and/or small for gestational age infants. However Zinc supplementation neither improves the growth or neurodevelopment of premature and/or
small for gestational age infants, nor it affects the morbidity patterns due to acute diarrhea and respiratory infections in infants who were born premature and/or small for gestational age. We also conclude that breast milk has a definite value to improve morbidity patterns due to diarrhea in these infants
REFERENCES
1. Itabashi K, Saito T, Ogawa Y, Uteni Y. Incidence and predicting factors of hypozincemia in very low birth weight infants at near term postmenstrual age. Biol Neonate 2003; 83: 235-240.
2. Hambidge KM, Krebs NF. Zinc in the fetus and neonate.
In: Polin R, Fox W, Abman SH, editors. Fetal and
Neonatal Physiology. 3rd edn. Philadephia: Elsevier Science 2004. p. 324-346.
3. Friel JK, Andrews WL, Matthew JD, Long DR, Cornel AM, Cox M, et al. Zinc supplementation in very low
birth weight infants. J Pediatr Gastroenterol Nutr 1993; 17: 97-104.
4. Castillo-Duran C, Rodriguez A, Venegas GV, Alvarez P, Icaza P. Zinc supplementation and growth of infants born small for gestational age. J Pediatr 1995; 127: 206-211.
5. Díaz-Gómez NM, Domenech E, Barroso F, Castells S, Cortabarria C, Jimenez A. The effect of zinc supplementation on linear growth, body composition and growth factors in preterm infants. Pediatrics 2003; 111: 1002-1009.
6. Islam MN, Chowdhury MAKA, Siddika M, Qurishi SB, Bhuiyan MKJ, Hoque MM and Akhter S: Effect of Oral Zinc Supplementation on the Growth of Preterm Infants. Indian Paed.2010;47;17.
7. Beaty RD and Kerber JD: Theoretical concepts and definitions. In: Concepts, instrumentation and techniques in Atomic Absorption Spectrophotometry. Eds Beaty RD and Kerber JD. Perkin Elmer Corporation, Norwalk CJ, USA. 1993;1;1-3.
8. EU BSL: Evaluation of a developmental screening system for use by child health nurses. Arch. Dis. Child; 1986;61: 34-41.
9. Gupta AP, Bhandari B,Gupta AB: Serum Copper, Zinc,Magnesium and Calcium in neonates. Indian Paed. 1984; 21; 469-473.
10. Kapoor RK, Misra PK, Dixit S, Wakhlu I, Sharma B, Seth TD. Zinc and intrauterine growth. Indian Paed. 1988; 25; 972-976.
11. Bhaskaram P and Hemlatha P: Is zinc deficiency in children a nutritional problem in India. Nutrition News 1994; 15; 1-4.
12. Osendarp SJM, Santosham M, Black RE, Wahed MA, Van Raaij JMA Fuchs GJ. Effect of zinc supplementation between 1 and 6 month of life on growth and morbidity of Bangladeshi infants in urban slums. Am J Clin Nutr 2002; 76: 114-119.
13. Sur D, Gupta DN, Mondal SK, Ghosh S, Manna B, Rajendran K, et al. Impact of zinc supplementation on