www.bjorl.org
Brazilian
Journal
of
OTORHINOLARYNGOLOGY
ORIGINAL
ARTICLE
The
effects
of
the
time
of
intranasal
splinting
on
bacterial
colonization,
postoperative
complications,
and
patient
discomfort
after
septoplasty
operations
夽
Abdullah
Karatas
a,∗,
Filiz
Pehlivanoglu
b,
Mehti
Salviz
a,
Nuray
Kuvat
b,
Isil
Taylan
Cebi
a,
Burak
Dikmen
a,
Gonul
Sengoz
baHasekiTrainingandResearchHospital,EarNoseandThroatClinic,Istanbul,Aksaray,Turkey
bHasekiTrainingandResearchHospital,InfectiousDiseasesandClinicalMicrobiology,Istanbul,Aksaray,Turkey
Received1June2015;accepted15November2015 Availableonline6February2016
KEYWORDS
Nasalsplint; Patientcomfort; Septoplasty
Abstract
Introduction:Themainreasonfornasaltamponplacementafterseptoplastyistoprevent post-operativehemorrhage,whilethesecondarypurposeisinternalstabilizationafteroperations involvingthecartilaginous-bonyskeletonofthenose.Siliconeintranasalsplintsareas success-fulasothermaterialsincontrollingpostoperativehemorrhagesofseptalorigin.Thepossibility ofleavingthesplintsintranasallyforextendedperiodshelpsstabilizetheseptuminthe mid-line.However,thereisnothingintheliteratureabouthowlongthesesplintscanberetained insidethenasalcavitywithoutincreasingtheriskofinfection,postoperativecomplications, andpatientdiscomfort.
Objective:The current study aimed to evaluate the association between the duration of intranasalsplinting andbacterialcolonization,postoperativecomplications,andpatient dis-comfort.
Methods:Patientswhohadundergoneseptoplastyweredividedintothreegroupsaccordingto thedayofremovalofthesiliconesplints.Thesplintswereremovedonthefifth,seventh,and tenthpostoperativedays.Theremovedsplintsweremicrobiologicallycultured.Earlyandlate complicationswereassessed,includinglocalandsystemicinfections,tissuenecrosis,granuloma formation,mucosalcrusting,synechia,andseptalperforation.Postoperativepatientdiscomfort wasevaluatedbyscoringthelevelsofpainandnasalobstruction.
Results:Nosignificantdifferencewasfound intherateofbacterialcolonization amongthe
differentgroups.Decreasedmucosalcrustingandsynechiaweredetectedwithlongerusage
intervals ofintranasal silicone splints. Postoperative pain and nasal obstruction were also diminishedbythethirdpostoperativeday.
夽 Pleasecitethisarticleas:KaratasA,PehlivanogluF,SalvizM,KuvatN,CebiIT,DikmenB,etal.Theeffectsofthetimeofintranasal splint-ingonbacterialcolonization,postoperativecomplications,andpatientdiscomfortafterseptoplastyoperations.BrazJOtorhinolaryngol. 2016;82:654---61.
∗Correspondingauthor.
E-mail:akrts2000@yahoo.ca(A.Karatas). http://dx.doi.org/10.1016/j.bjorl.2015.11.008
Conclusions: Siliconesplintswerewelltoleratedbythepatientsandanynegativeeffectson postoperativepatientcomfortwerelimited.Infact,prolongedsplintusageintervalsreduced latecomplications.Long-termsiliconenasalsplintusageisareliable,effective,and
comfort-ablemethodinpatientswithexcessivemucosaldamageandinwhomlong-termstabilization
ofthebonyandcartilaginousseptumisessential.
© 2016Associac¸˜aoBrasileira de Otorrinolaringologiae CirurgiaC´ervico-Facial.Publishedby Elsevier EditoraLtda.Thisisanopenaccess articleundertheCCBY-NC-NDlicense(http://
creativecommons.org/licenses/by-nc-nd/4.0/).
PALAVRAS-CHAVE
Splintnasal;
Confortodopaciente; Septoplastia
Efeitosdotempodepermanênciadesplintsintranasaissobreacolonizac¸ão bacteriana,complicac¸õesnopós-operatórioedesconfortodopacienteapós septoplastia
Resumo
Introduc¸ão: A principal razão para a colocac¸ão de tampões nasais em septoplastias é a prevenc¸ão dehemorragia pós-operatória, enquanto oobjetivo secundário é aestabilizac¸ão internaapóscirurgiasqueenvolvamoesqueletocartilaginosodonariz.Ossplintsintranasais desiliconesãotãoeficazescomooutrosmateriaisparaocontroledehemorragiasdoseptono pós-operatório.Apossibilidadedemanterossplintsintranasaisporlongosperíodosajudaa esta-bilizaroseptonalinhamédia.Noentanto,nãohánadanaliteraturasobrequantotempoesses
splintspodemsermantidosnacavidadenasalsemaumentaroriscodeinfecc¸ão,complicac¸ões nopós-operatórioecausardesconfortoaopaciente.
Objetivos: Opresenteestudotevecomoobjetivoavaliaraassociac¸ãoentreotempode tam-ponamentocomsplintsintranasaisecolonizac¸ãobacteriana,complicac¸õesnopós-operatório edesconfortodopaciente.
Método: Ospacientessubmetidos aseptoplastiaforamdivididos em trêsgrupos,de acordo com odia daremoc¸ão dos splintsde silicone.Os splintsforam removidos no5◦, 7◦ e 10◦
diasdepós-operatório,easeguir,cultivadosmicrobiologicamente.Complicac¸õesprecocese tardiasforamavaliadas,incluindoinfecc¸õeslocaisesistêmicas,necrosedotecido,formac¸ão degranulomas,crostasnamucosa,sinéquiaseperfurac¸ãodosepto.Odesconfortodopaciente nopós-operatóriofoiavaliadocomousodepontuac¸ãodosníveisdedoredeobstruc¸ãonasal.
Resultados: Nenhumadiferenc¸asignificantefoiencontradanataxadecolonizac¸ãobacteriana entreosdiferentesgrupos.Diminuic¸õesdaformac¸ãodecrostasnamucosaedesinéquiasforam detectadascomtemposmaislongosdeusodesplintsdesilicone.A doreaobstruc¸ãonasal
tambémdiminuíramnoterceirodiadepós-operatório.
Conclusões: Ousodesplintsdesiliconefoibemtoleradopelospacientes,eseusefeitos
neg-ativos sobre o conforto do paciente no pós-operatório foram limitados. De fato, o tempo
prolongado deusoteve um efeitoredutorsobreascomplicac¸ões tardias.Ousoprolongado
desplintnasaldesiliconeéummétodoconfiável,eficazepoucodesconfortávelempacientes comlesãoexcessivadamucosaenaquelescujaestabilizac¸ãoósseaecartilaginosadoseptoa longoprazoéessencial.
©2016Associac¸˜ao BrasileiradeOtorrinolaringologiaeCirurgiaC´ervico-Facial.Publicado por Elsevier EditoraLtda. Este ´eum artigo Open Accesssob umalicenc¸a CC BY-NC-ND(http://
creativecommons.org/licenses/by-nc-nd/4.0/).
Introduction
Surgicalinterventionsdirectedatthenasalseptumare fre-quently applied in the daily practices of Ear, Nose, and Throat(ENT) specialists.Septalsurgeryforfunctional and esthetic purposes is commonly performed. The methods andmaterials used innasal packingare numerous in sep-toplasty. Various materials including cotton tape, gauze, paraffingauze,Tefla,Merocel,sponges,andsiliconenasal splintshavebeenrecommendedforthispurpose.1
Althoughthesematerialshavebeenemployedprimarily topreventpossiblehemorrhagefollowingseveral interven-tions,theyarealsoexpectedtocontributetothe stabiliza-tionofthenasalcartilaginousbonyskeletonatthemidline andpromotemucosalhealing.2,3Additionally,nasalpacking
isusedtopreventsynechiaeorrestenosis,particularlyafter surgery.2,3 Recently, silicone nasal splints have been used
siliconesplintsaidhemostasisasmuchasothermaterials.1,2
However,thesupporttheyprovidetoassistinmaintaining theseptum in themidline andtheir facilitating effecton mucosalhealingincasesofpossiblemucosalinjuryarethe mainreasonsfortheselectionofsiliconenasalsplints.2---4
Recently,siliconesplintshavebecome morepreferable inseptumsurgerycomparedtotheothermaterials.Silicone splints have the advantage of being safely and comfort-ablyretainedintranasallylongerthanothermaterials.This intervalcan be lengthenedup to 10 days in some cases. However,somelocalandraresystemiccomplications(e.g., tissuenecrosis,infections,etc.)mayariseduringintranasal tamponapplications.5---11
Unfortunately, there is no information in the litera-ture concerning how long these splints can be retained intranasally without increasing the risk of complications. Also,studies are limited concerning the effects of splint usage intervals on patient discomfort and complications, such as mucosal crusting and synechia. The current study aimed to evaluate the association of intranasal splinting intervals with bacterial colonization, early and latecomplications (tissue necrosis, mucosal crusting,and synechia), and patient discomfort. Another goal was to determinetheoptimalintranasalretentiontimeforsilicone splintsaftersurgery.
Methods
Subjects
This was a prospective randomizedclinical trial. Patients whohadundergoneseptoplastyandfunctional septorhino-plastybetweenFebruary 2014andSeptember2014 atthe HasekiTrainingandResearchHospitalwereincludedinthe study.Thepatientswerechosenbysealedenvelopeand ran-domlyassignedintooneof threegroups (Groups1---3).All patientsunderwentadetailedexaminationincludingnasal endoscopy,anteriorrhinoscopy,andcomputedtomography (CT)scan,ifnecessary,inordertoexcludeothersinonasal pathologies.The patients receiving operationsother than septoplasty, such as turbinate surgery, sinus surgery, and revisioncases,wereexcludedfromthisstudy.Patientswho requiredarhinoplastyandosteotomywerealsoexcluded. However,patients whohad a high dorsal septaldeviation andrequiredopenseptoplastywereadmittedtothestudy. Thesepatients were preoperatively equallydistributed to allgroups. Patientswithsystemicdiseases or immunosup-pressionwerealsoexcluded.Patientswhofailedtofollow postoperative instructions and take medications properly wereexcludedintheevaluationphase.
Three patient groups were created according to the removal time of the silicone splints. The splints were removedonthefifth,seventh,andtenthpostoperativedays inGroups1,2,and3,respectively.Thenumberofpatients in Groups 1, 2, and 3 were 32, 33, and 30, respectively. Group 1 consisted of 24 male and eight female patients withameanageof 30.0±8.1years(range:19---47 years); Group2consistedof25maleandeightfemalepatientswith amean ageof 29.7±8.1 years(range:19---47 years);and Group3consistedof20maleandtenfemalepatientswith ameanageof29.0±7.14years(range:18---42years).The
meanagesofthethreegroupswerenotdifferentfromeach other(p=0.890).Allsubjectswerevolunteersandwritten informedconsentwasobtainedoncethepatientswerefully apprisedofthedesign,aim,andclinicalimplicationsofthe study.
Surgicalprocedures
All procedures were performed under general anesthesia bythe samesurgeon.Eitheran open approachor Killian’s methodwaschosen for theseptoplastytechnique accord-ing tothe septalpathology. Polyglactin910 suture (Vicryl RapideTM;Ethicon---CA,UnitedStates)wasusedinKillian’s
methodandpolypropylenesuture(Prolene®;Ethicon---CA,
UnitedStates)wasusedintheopenapproach.Thesesuture materials wereonly usedfor closing atthe initialincision lines. Transseptal sutures were not used in any patients. Silicone splints withairway tubes (DoyleTM Intranasal
Air-waySplint; Medtronic--- MN,United States)wereinserted in each nasalcavity afterthe surgery. Preoperative intra-venousantibioticprophylaxiswithsulbactam---ampicillinwas administered toall patients. Postoperative oral antibiotic treatmentswereadministereduntiltheremovalofthe sil-icone splints, in accordance with the routine practice in this clinic. In the current study, cefdinir tablets (300mg) wereadministeredpostoperativelytwotimesperday. Cef-dinirwaspreferredforitsGram-positiveandGram-negative efficacy.12---14Additionally, nasallavagewithsalinesolution
wasprescribedfourtimesperday.
Patientdiscomfort
Postoperative patient discomfort wasevaluated by visual analogscale(VAS)scoringofnasalobstructionandpain.VAS scores for postoperative pain measurements(0---10; 0: no pain, 10: unacceptable pain) were noted by the patients everymorningbeforetakinganalgesicsfromthefirst post-operativedayuntilthesplintswereremoved.Postoperative nasalobstructionwasalsoevaluatedbyVASscoring(0to10; 0:noobstruction,10:fullobstruction)everymorningafter nasallavage.
Complications
Complications were evaluated in two categories, which included bacterial colonization/infection related to early complicationsandlatecomplications(mucosalcrustingand synechia).
Atthecontrolexamination, allpatients wereobserved and evaluated for pressure tissue necrosis and local and systemicinfectionsigns(e.g.,nasal vestibularhyperemia, tenderness, purulent discharge, septal hematoma, septal abscess,fever,andgeneralpoorhealthinthepostoperative period).
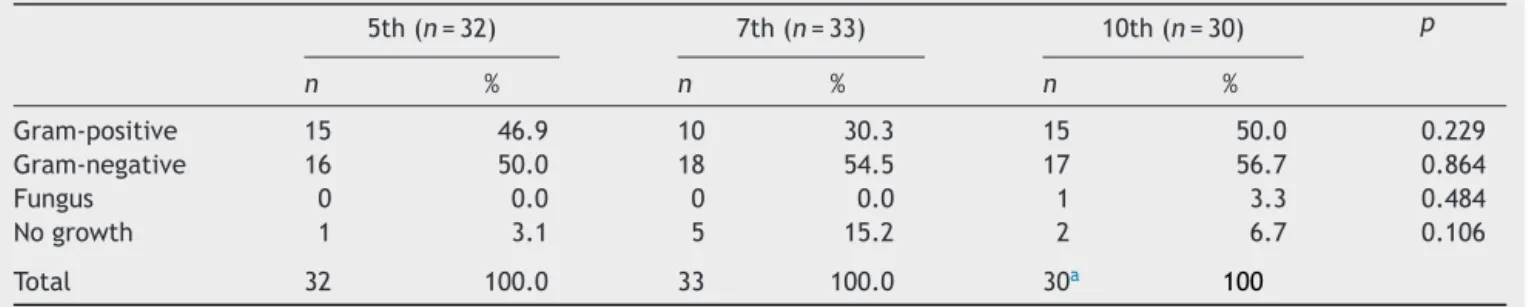
Table1 Cultureresultsaccordingtothegroups.
5th(n=32) 7th(n=33) 10th(n=30) p
n % n % n %
Gram-positive 15 46.9 10 30.3 15 50.0 0.229
Gram-negative 16 50.0 18 54.5 17 56.7 0.864
Fungus 0 0.0 0 0.0 1 3.3 0.484
Nogrowth 1 3.1 5 15.2 2 6.7 0.106
Total 32 100.0 33 100.0 30a 100
a TwodifferentbacterialcolonizationoccurredtogetherinfivepatientsinGroup3.
performedbythesameperson.Thesurgeonwhoperformed theoperationsdidnotparticipateinthisevaluation.
Microbiologicalprocedures
Materialremovedfromtherightnasalcavitywasincludedin thestudyinallpatients.Trypticsoybroth(2mL)waspoured onthe splints, which were then sent to themicrobiology laboratorytobeincubatedfor2hat37◦C.A0.01mLsample
fromthefluidsamplescontainingthesplintswasobtained andcultivatedinchocolateagarandMcConkeyagar.Plaques keptintheincubatorwereevaluatedafter24and48hand colonycountswereperformed.Bacterialidentificationwas performedforeachcolonyusingconventionalmethods.
Statisticalanalysis
Rate and frequency values were used in the descriptive statistics.Thechi-squaredtestandFischer’stest(when chi-squared test conditions were not met) were used in the analysisofcategoricaldata.SPSS22.0software(SPSSInc. ---Chicago,IL,UnitedStates)wasusedforstatisticalanalysis. Ethical approval for the study was obtained from the HasekiTrainingandResearchHospitalEthicsCommitteeon February5,2014(ProtocolNo.38).
Results
Bacterialcolonizationandinfection-relatedearly complications
No significant differences between the three groups regardingbacterialcolonizationratesofGram-positiveand Gram-negative bacteria (p=0.229), fungi (p=0.864), or
othermicroorganisms(p=0.484),andnogrowth(p=0.106) werefound(Table1).
When Gram-negative bacterial colonization was evalu-atedaccording to theintranasal splint retention interval, thegrowthrateofthemainpathogenicspecies( Enterobac-ter spp., Escherichia coli, and Klebsiella spp.) and other specieswerenotsignificantlydifferentamongGroups1---3 (p=0.616, p=0.322,p=0.582,andp=0.962,respectively;
Table2).
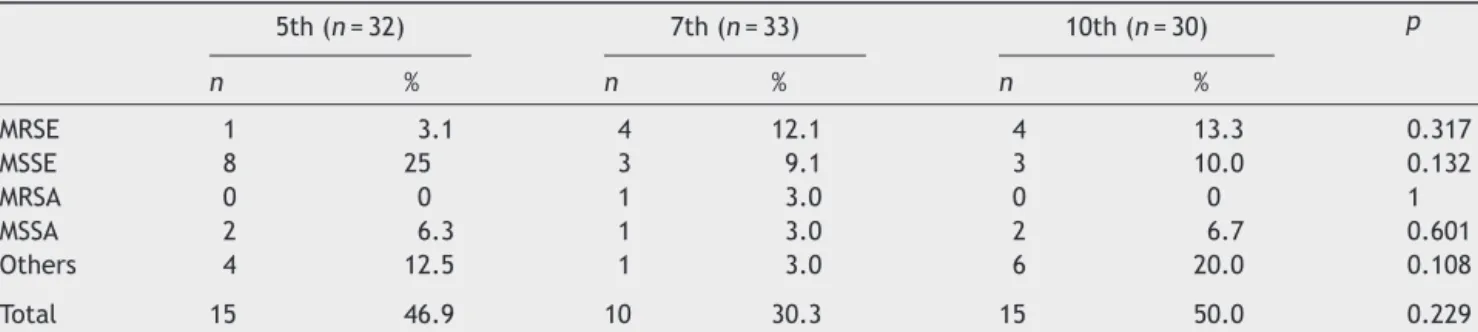
When Gram-positive bacterial colonization was evalu-atedaccording to theintranasal splint retention interval, the growth rate of methicillin-resistant Staphylococcus epidermidis (MRSE), methicillin sensitive S. epidermidis
(MSSE),methicillin-resistantStaphylococcusaureus(MRSA), methicillin-sensitiveS. aureus (MSSA), and other types of specieswerenotsignificantlydifferentamongGroups1---3 (p=0.317,p=0.132,p=1,p=0.601,andp=0.108, respec-tively;Table3).
When the staphylococci with and without methicillin-resistance were analyzed together, the growth rate of MRSE/MRSA (major pathogenic species), MSSE/MSSA (can befound in nasal flora), andother species inGroups 1---3 were not significantly different (p=0.239, p=0.134, and
p=0.108,respectively;Table4).
Allpatients wereobserved andevaluatedfor infection relatedtoearlylocalandsystemiccomplications(e.g., pres-suretissuenecrosis,nasalvestibularhyperemia,tenderness, purulent discharge,septalhematoma, abscess,fever, and generalpoorhealth).Nolocalorsystemiccomplicationsin thepostoperativeperiodweredetected.
Patientdiscomfort
Inallgroups,themeanpainVASscoreswerehigherinthe first three days than in the other days. The mean pain
Table2 DistributionofthemainGram-negativepathogenbacteriaamongthegroups.
5th(n=32) 7th(n=33) 10th(n=30) p
n % n % n %
Enterobacterspp. 4 12.5 4 12.1 6 20.0 0.616
E.coli 3 9.4 6 18.2 2 6.7 0.322
Klebsiellaspp. 4 12.5 2 6.1 4 13.3 0.582
Others 5 15.6 6 18.2 5 16.7 0.962
Table3 DistributionofGram-positivebacteriaamongthegroups.
5th(n=32) 7th(n=33) 10th(n=30) p
n % n % n %
MRSE 1 3.1 4 12.1 4 13.3 0.317
MSSE 8 25 3 9.1 3 10.0 0.132
MRSA 0 0 1 3.0 0 0 1
MSSA 2 6.3 1 3.0 2 6.7 0.601
Others 4 12.5 1 3.0 6 20.0 0.108
Total 15 46.9 10 30.3 15 50.0 0.229
MRSE,methicillinresistantStaphylococcusepidermidis;MSSE,methicillinsensitiveStaphylococcusepidermidis;MRSA,methicillin resis-tantStaphylococcusaureus;MSSA,methicillinsensitiveStaphylococcusaureus.
Table4 DistributionofGram-positivebacteriaamongthegroupsaccordingtothemethicillinresistance.
5th(n=32) 7th(n=33) 10th(n=30) p
n % n % n %
MRSE/MRSA 1 3.1 5 15.2 4 13.3 0.239
MSSE/MSSA 10 31.3 4 12.1 5 16.7 0.134
Others 4 12.5 1 3.0 6 20.0 0.108
Total 15 46.9 10 30.3 15 50.0 0.229
MRSE,methicillinresistantStaphylococcusepidermidis,MSSE,methicillinsensitiveStaphylococcusepidermidis;MRSA,methicillin resis-tantStaphylococcusaureus;MSSA,methicillinsensitiveStaphylococcusaureus.
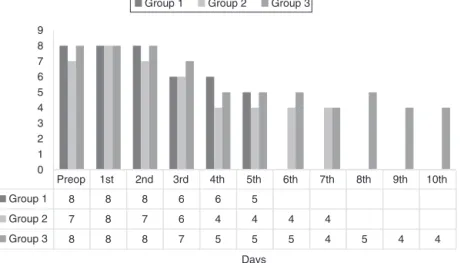
VASscoresdecreasedsignificantlyafterthethirddayinall groups(p<0.05)(Fig.1).
Inallgroups,themeannasalobstructionVASscoreswere loworsimilarwithpreoperativevaluesforalldays. There-fore,itcouldbesuggestedthattherewasatolerablelevel ofnasalobstructionforthepatients(Fig.2).
Latecomplications
Mucosalcrusting:prolongedmucosalcrustingwasdetected in 12 patients in Group 1, six patients in Group 2, and
two patients in Group 3. The rate of mucosal crusting wasdecreasedwithprolongedintranasalsplintingintervals (p=0.0105;Table5).
Synechiae
SynechiaewerefoundinsixpatientsinGroup1,twopatients in Group 2, and no synechiae were found in Group 3. Therateofsynechiaformationwassignificantlydecreased with prolonged intranasal splinting intervals (p=0.0244;
Table5).
1st day
2nd day
3rd day
4th day
5th day
6th day
7th day
8th day
9th day
10th day
Group 1 8 8 7 5 4
Group 2 8 7 7 4 4 2 2
Group 3 8 8 7 4 4 3 2 2 1 1
0 1 2 3 4 5 6 7 8 9
Group 1 Group 2 Group 3
Preop 1st 2nd 3rd 4th 5th 6th 7th 8th 9th 10th
Group 1 8 8 8 6 6 5
Group 2 7 8 7 6 4 4 4 4
Group 3 8 8 8 7 5 5 5 4 5 4 4
0 1 2 3 4 5 6 7 8 9
Days Group 1 Group 2 Group 3
Figure2 Nasalobstructionscoresinthegroups.
Table5 Latecomplicationsinthegroups.
5th(n=32) 7th(n=33) 10th(n=30) p
n % n % n %
Mucosalcrusting 12 37.5 6 18.2 2 6.6 0.0105
Synechia 6 18.8 2 6.0 0 0.0 0.0244
Discussion
Nasal packing methods andapplication intervals are vari-ableafterseptoplastyoperations. Severalsurgeonsdonot use any nasal packing materials, preferring transseptal sutures only. Patient discomfort and local or systemic adversereactionsduetonasalpackingresultedindifferent applicationsconcerningtheselectionofpackingmaterials, postoperative antibiotic therapies, and the duration of nasalpacking.Theuseofantibioticsinpatientswithnasal packing is controversial. Nasal packing applications have beenacceptedasatechniquethatmightpossiblyresultin localandevensystemicinfectionsincludingStaphylococcal Toxic Shock Syndrome (STSS).5---11 Therefore, as a routine
application in manyclinics, oral antibiotics arecontinued untilthetamponsareremoved.Recommendationsfor post-operative antibiotherapy are commonly found in classical textbooks.15,16 However, a number of reports have been
published recently in the medical literature suggesting that postoperative antibiotherapy is unnecessary after septoplastyorrhinoplasty.Georgiouetal.,intheirreview of antibiotic prophylaxis in rhinoplasty and septoplasty, evaluated the outcomes of 11 different studies.17 These
studies confirmed that the risk of infection is very low in elective nasal operations and thus, routine antibiotic prophylaxis is unnecessary. Antibiotic prophylaxis has been recommended in cases of complicated revisions, in patients with a tendency to develop infection, and in patientsinwhomlong-termnasaltamponapplicationsare planned.17,18However,althoughtherearepublishedreports
not recommending postoperative antibiotic prophylaxis, manyENTspecialistscontinue toprescribeoralantibiotics untiltheremovalofthetampons.
InastudyperformedbytheAmericanRhinology Associa-tion,therateofantibioticprescriptionofthesurgeonsafter septoplastywasreportedas70%. Therationale for antibi-oticusewasreportedasinfectioncontrolin60%ofcases, preventionof toxic shock in 31.5% of cases,medico-legal purposesin4.9%ofcases,andpreventingfoulodorsin3.1% of cases.19 In the current study,cefdinir tablets (300mg)
were administered postoperatively two times a day. We foundthattherewerenochangesinbacterialcolonization propertiesduetosplintingintervalsandnoinfectionswere relatedtoearlycomplications.However,severalpathogenic agentsalongwithnormalflorabacteriawereisolatedinthe cultures(Tables1---4).Therefore,werecommendthat post-operativeantibioticprophylaxisshouldbeprescribeduntil theremovalofthenasalsplints.
Intheirliteraturereview,Weber etal.evaluatednasal packing materials (other than silicone splints) according toretention timesand side effects.In their study, reten-tionintervalsformaterialssuchasMerocel,paraffingauze, gauze,fingerstalls, and silastic splints ranged from24 to 72h.20 However,therehasbeennoconsensusinretention
intervalsofsiliconenasalsplints.Inourstudy,wefoundthat siliconenasalsplints might be retainedintranasally up to 10dayswithout increasinginfection-relatedearly compli-cationrates.
present study. In the literature, facial pain, headaches, nasalobstruction,xerostomia,anddysphagiadue tonasal obstructionaremajorparametersintheassessmentof post-operativepatientdiscomfort.21,22
In our study, postoperative pain scores were higher in the first three days and decreased significantly after the fourthday.Splintusageintervalsdidnothaveanyincreasing effectonthepainscores.Withtheuseofanalgesics,pain complaintsweresustainedatareasonablelevel.
Preoperativeandpostoperativenasalobstructionscores werecomparableandVASscoresmeasuredduringtheuseof siliconesplintsweresimilartopreoperativevaluesorlower. Therefore, nasal obstruction due to silicone nasal splints wasconsideredacceptable.Whentheeffectofsplintusage intervals onpain and nasal obstruction scores was evalu-ated,long-termuseofnasalsplintswaseasilytoleratedby thepatients anddidnothaveaseriousnegativeeffecton patientcomfort.
Prolonged mucosal crusting and synechia are two late complicationsafterseptoplastythatcanobstructnasal air-flow.Wefoundthatthelongersplintusageintervalresulted in decreased mucosal crusting and synechia rates. These findings correlate well with other studies suggesting that siliconesplintshaveapositiveeffectonhealingand epithe-lizationbyprovidingthedurabilityofnasalmucosa.2,3
Limitations
No significant changes in bacterial colonization proper-ties due to splint usage intervals were detected and no infection-related early complications were observed in this study. However, toxic shock syndrome (TSS) is a rarebutveryimportantsystemicinfectionthatcan result fromnasal packingapplications(siliconesplintsandother materials).3---11Thesamplesizeofthisstudywasverysmall
fortheassessmentofararecomplicationsuchasTSS; there-fore,studieswithlargersamplesizesareneededtoobtain aconclusivedecisionconcerningSTSSrisk.
Conclusion
Theuse ofsiliconesplintswaswelltolerated bypatients; negativeeffectsonthepostoperativepatientcomfortwere limited.Infact,aprolongedsplintusagetimeintervalhad a reducing effecton later complications such asmucosal crustingandsynechia.Long-termsiliconenasalsplintusage isareliable,effective,andcomfortablemethodforpatients withexcessivemucosaldamageandinwhomlong-term sta-bilizationofthebonyandcartilaginousseptumisessential.
Financial
support
Financialsupportwasprovidedbythemanagementofthe HasekiTrainingandResearchHospital.
Conflicts
of
interest
Theauthorsdeclarenoconflictsofinterest.
References
1.Acıoglu E, Edizer DT, Yigit O, Onur F, Alkan Z. Nasal sep-talpacking:whichone?EurArchOtorhinolaryngol.2012;269: 1777---81.
2.JungYG,HongJW,EunYG,KimMG.Objectiveusefulnessofthin silasticseptalsplintsafterseptalsurgery.AmJRhinolAllergy. 2011;25:182---5.
3.CookJA,MurrantNJ,EvansKL,LavelleRJ.Intranasalsplints andtheireffectsonintranasaladhesionsandseptalstability. ClinOtolaryngolAlliedSci.1992;17:24---7.
4.AsakaD,YoshikawaM,OkushiT,NakayamaT,MatsuwakiY,Otori N, et al. Nasalsplinting using siliconeplates without gauze packingfollowingseptoplastycombinedwithinferiorturbinate surgery.AurisNasusLarynx.2012;39:53---8.
5.MárquezMoyanoJA,JiménezLuqueJM,SánchezGutiérrezR, RodríguezTemblequeL,OstosAumenteP,RoldánNoguerasJ, etal.Toxicshocksyndromeassociatedwithnasalpacking.Acta OtorrinolaringolEsp.2005;56:376---8.
6.AllenST,LilandJB,NicholsCG,GlewRH.Toxicshocksyndrome associatedwithuseoflatexnasal packing.ArchIntern Med. 1990;150:2587---8.
7.Hull HF, Mann JM, Sands CJ, Gregg SH, Kaufman PW. Toxic shock syndrome related to nasal packing. Arch Otolaryngol. 1983;109:624---6.
8.Fishman G, Ophir D. Toxic shock syndrome. Harefuah. 1997;132:622---4.
9.Wagner R, Toback JM. Toxic shock syndrome following sep-toplasty using plastic septal splints. Laryngoscope.1986;96: 609---10.
10.BredaSD,JacobsJB,Lebowitz AS,TiernoPMJr. Toxicshock syndromeinnasalsurgery:aphysiochemicalandmicrobiologic evaluation of Merocel and Nugauze nasal packing. Laryngo-scope.1987;97:1388---91.
11.MoserN,HoodC,ErvinD.Toxicshocksyndromeinapatient using bilateral siliconenasal splints.Otolaryngol Head Neck Surg.1995;113:632---3.
12.JacobsaMR,JonesRN,GiordanoPA.Oralbeta-lactamsapplied touncomplicatedinfectionsofskinandskinstructures.Diagn MicrobiolInfectDis.2007;57:55S---65S.
13.JonesaNR, SaderaHS. Updateonthesefdinir spectrumand potencyagainst pathogensisolated from uncomplicated skin andsofttissueinfectionsinNorthAmerica:areweevaluating theorallyadministeredcephalosporinscorrectly?Diagn Micro-biolInfectDis.2006;55:351---6.
14.SaderaHS,StreitaJM,FritscheaTR,JonesaRN.Potencyand spectrum reevaluation of cefdinir tested against pathogens causing skin and soft tissue infections: a sample of North American isolates. Diagn Microbiol Infect Dis. 2004;49: 283---7.
15.Richard LG, Lane FS. Nasal septoplasty and submucous resection. In: Bailey BJ, CalhaunKH, editors. Atlas of head andnecksurgery---otolaryngology,vol.1,2nded.Philadelphia: Lippincott,PA:Williams&Wilkins;2001.p.462---6.
16.HabesogluTE,HabesogluM.Septoplasty.In:HathiramBT, Khat-tarVS,editors.Atlasofoperativeotorhinologyandheadneck surgery.1sted.NewDelhi:JaypeeBrothersMedicalPublishers; 2013.p.396---8.
17.Georgiou I, Farber N, Mendes D, Winkler E. The role of antibioticsinrhinoplastyandseptoplasty:aliteraturereview. Rhinology.2008;46:267---70.
18.DubinMR,PletcherSD.Postoperativepackingafterseptoplasty: isitnecessary?OtolaryngolClinNorthAm.2009;42:279---85. 19.RechtwegJS,PaoliniRV,BelmontMJ,WaxMK.Postoperative
20.WeberR,HochapfelF,DrafW.Packingandstentsinendonasal surgery.Rhinology.2000;38:49---62.
21.BernardoMT,AlvesS,LimaNB,HelenaD,CondéA.Septoplasty withorwithoutpostoperativenasalpacking?Prospectivestudy. BrazJOtorhinolaryngol.2013;79:471---4.