REVISTA
BRASILEIRA
DE
ANESTESIOLOGIA
PublicaçãoOficialdaSociedadeBrasileiradeAnestesiologiawww.sba.com.br
SCIENTIFIC
ARTICLE
A
prospective,
randomized,
double-blinded
control
study
on
comparison
of
tramadol,
clonidine
and
dexmedetomidine
for
post
spinal
anesthesia
shivering
Rajagopalan
Venkatraman
∗,
Krishnamoorthy
Karthik,
Anand
Pushparani,
Annadurai
Mahalakshmi
SRMMedicalCollegeHospitalandResearchCentre,DepartmentofAnesthesia,Chennai,India
Received7March2016;accepted2August2016 Availableonline20August2016
KEYWORDS
Clonidine;
Dexmedetomidine; Hypothermia; Shivering; Spinalanesthesia; Tramadol
Abstract
Introduction:Shivering,acommonintraoperativeproblemunderspinal anesthesiaincreases theoxygenconsumptionconsiderablyandisuncomfortableanddistressingtothepatient, anes-thesiologistaswellassurgeon.Thepresentstudywasdesignedtoexploretheeffectivenessof tramadol,clonidineanddexmedetomidineinthetreatmentofpostspinalanesthesiashivering andtolookfortheiradverseeffects.
Methods:Thisprospective,randomized,doubleblindedcontrolstudywasdoneon90patients who developedshiveringunderspinal anesthesia.Theywere randomlyallocatedinto three groupswithGroupTreceivingtramadol1mg.kg−1,GroupCgettingclonidine1mcg.kg−1and GroupDpatientsreceivingdexmedetomidine0.5mcg.kg−1.Thetimetakentocontrolshivering, recurrencerate,hemodynamicvariables,sedationscoreandadverseeffectswereobserved. Results:Dexmedetomidinewas fasterinthecontrolofshiveringin5.7±0.79minutes (min) whereas tramadol took 6.76±0.93min and clonidinewas slower with 9.43±0.93min. The recurrence rate was much lower in the dexmedetomidine group with 3.3% thanfor cloni-dine(10%) and tramadol (23.3%) group.The sedation achieved with dexmedetomidine was betterthanclonidineandtramadol.Thetramadolgrouphadmorecasesofvomiting(four)and dexmedetomidinegrouphadsixcasesofhypotensionandtwocasesofbradycardia.Twoofthe clonidinepatientsencounteredbradycardiaandhypotension.
Conclusion:Dexmedetomidineisbetterthantramadolandclonidineinthecontrolofshivering becauseofitsfasteronsetandlessrecurrencerate.Thoughcomplicationsareencounteredin thedexmedetomidinegroup,theyaretreatable.
©2016SociedadeBrasileiradeAnestesiologia.PublishedbyElsevierEditoraLtda.Thisisan openaccessarticleundertheCCBY-NC-NDlicense( http://creativecommons.org/licenses/by-nc-nd/4.0/).
∗Correspondingauthor.
E-mail:drvenkat94@gmail.com(R.Venkatraman). https://doi.org/10.1016/j.bjane.2016.08.001
PALAVRAS-CHAVE
Clonidina;
Dexmedetomidina; Hipotermia; Tremor; Raquianestesia; Tramadol
Estudoprospectivorandômico,duplo-cegoecontroladocomparandotramadol, clonidinaedexmedetomidinaparatremorespós-raquianestesia
Resumo
Introduc¸ão: O tremor, problema comum no período intraoperatório sob raquianestesia, aumenta consideravelmente o consumo de oxigênio, além de ser desconfortável e angus-tianteparaopaciente,oanestesiologistaeocirurgião.Opresenteestudofoiconcebidopara explorar aeficácia de tramadol, clonidina e dexmedetomidina no tratamentode tremores pós-raquianestesiaeobservarseusefeitosadversos.
Métodos: Esteestudoprospectivo,randômico,controladoeduplo-cegofoirealizado com90 pacientesquedesenvolveramtremoressobraquianestesia.Ospacientesforamrandomicamente alocadosemtrêsgruposparareceber1mg.kg−1detramadol(GrupoT),1mcg.kg−1declonidina (GrupoC)e0,5mcg.kg−1dedexmedetomidina(GrupoD).Otemponecessárioparacontrolaros tremores,ataxaderecorrência,asvariáveishemodinâmicas,osníveisdesedac¸ãoeosefeitos adversosforamregistrados.
Resultados: Dexmedetomidina foi mais rápida para controlar os tremores, com tempo de 5,7±0,79minutos(min);otempodetramadolfoide6,76±0,93min;clonidinafoimaislenta, comtempode9,43±0,93min.Ataxaderecorrênciafoimuitomenornogrupo dexmedeto-midina (3,3%) que nos grupos clonidina (10%) e tramadol (23,3%). A sedac¸ão obtida com dexmedetomidinafoimelhorqueaobtidacomclonidinaetramadol.Ogrupotramadolteve maiscasosdevômito(quatro);ogrupodexmedetomidinateveseiscasosdehipotensãoedois casosdebradicardia.Doispacientesdogrupoclonidinaapresentarambradicardiaehipotensão. Conclusão:Dexmedetomidinafoimelhorquetramadoleclonidinaparaocontrolodetremores devidoaoseuiníciodeac¸ãomaisrápidoetaxaderecorrênciamaisbaixa.Emboracomplicac¸ões tenhamsidoobservadasnogrupodexmedetomidina,elasforamtratáveis.
©2016SociedadeBrasileiradeAnestesiologia.PublicadoporElsevierEditoraLtda.Este ´eum artigo OpenAccess sobumalicenc¸aCCBY-NC-ND( http://creativecommons.org/licenses/by-nc-nd/4.0/).
Introduction
Shivering is an oscillatory, involuntarymechanical
muscu-lar activity and a natural protective mechanism to the
reduction of body temperature. The body tries to raise
the metabolic heat generation to restore homeostasis by
shivering.1 The core temperature in humans is normally
maintained within a tight range of 36.5---37.5◦C which is
knownastheinterthresholdrangeorthermoneutralzone.
Thermoregulatoryresponseslikevasoconstrictionand
shiv-eringareactivatedwhencoretemperaturefallsbelowthe
normalrange.2Thespinal␣-motorneuronsandtheiraxons
mediatetheneurologicalmechanismofshiveringwith
cen-teratthepreopticnucleusoftheanteriorhypothalamus.3
Theincidenceofshiveringfollowingspinalanesthesiais
notexactlyknownforreferencesquotingashighas30---60%.4
The shivering increases heat production up to 600% and
oxygen consumption is tripled. This can lead to several
metabolicabnormalitieslikehypoxemia,hypercarbia,lactic
acidosis,increasedintraocularandintracranialpressure.5,6
Inpatientswithcoronaryarterydisease,shiveringcan
fur-thercompromisemyocardialfunction.7
Severalpharmacologicandnonpharmacologicstrategies
areavailableforthetreatmentofshiveringwithno
consen-sus onthe gold standard therapy.8 The nonpharmacologic
strategiesincludeblankets,warmingintravenousfluidsand
use of external warmer. Several drugs have been
stud-iedfor the prophylaxis as well astreatment of shivering.
This includes pethidine, tramadol, nefopam, ketamine,
dexmedetomidine, granisetron, physostigmine, clonidine,
magnesium sulphate, dexamethasone, and urapidil.9 But
unfortunately,nosingledrughas been found tobe
effec-tive and without any adverse effects. Pethidinewas long
consideredastheagentofchoicetocontrolshiveringbut
manyinstitutionsarenowadaysavoidingpethidinebecause
ofitsadverseeffects.8
The objectiveof thisprospective,randomized,
double-blindedcontrolstudyistocomparetheefficacy,recurrence
rate,hemodynamicsandcomplicationsoftramadol,
cloni-dine and dexmedetomidine in the treatment of shivering
followingspinalanesthesia.
Materials
and
methods
The study was performed after obtaining institutional
ethical committee approval and written, informed
con-sent from patients in a tertiary medicalcollege hospital.
Patients in the age group of 18---70, American Society of
Anesthesiologists(ASA)1 and2 andscheduled toundergo
elective surgeries underspinal anesthesia and developing
shiveringwere included in the study.Patients withASA 3
and above, cardiac, liver and renal diseases, allergic to
any of the study drugs or patient refusal and pregnant
patientswere excluded fromthe study.The patients who
developedshiveringunderspinalanesthesiawererandomly
dividedinto threegroups with30 patientsin each group.
hadclonidine1mcg.kg−1andGroupDreceived
dexmedeto-midine0.5mcg.kg−1.Thegroup allotmentwasdecidedby
the computer generated random envelope method. The
first anesthesiologist opens the envelope and adds the
study drugin a 100mL normal salineand hands it tothe
secondanesthesiologistwhoisblindedtothestudydrug.He
administersthedrugover10minandmonitorsthepatient.
Standard monitoring of Electrocardiogram,noninvasive
bloodpressure,oxygensaturationandaxillarytemperature
weredoneonallpatients.Theoperatingroomtemperature
wasmaintainedat 22◦C forall thesurgeries. Noexternal
warming devices were usedand fluids were administered
atroomtemperaturetoallpatients.Thepatientsreceived
spinal anesthesiawith 25 gauge Quincke spinal needle to
achieve a level of at least T10 depending on thetype of
surgery.Patientswhodevelopedshiveringwereincludedin
the study. The shivering intensity was graded on a scale
of 1---4 as per Wrench. Grade 1 was patients having one
ormoreofthefollowing:piloerection,peripheral
vasocon-striction, peripheral cyanosis, but without visible muscle
activity.Grade 2 includes visible muscle activity confined
toonemusclegroup.Grade3wasvisiblemuscleactivityin
morethan onemuscle group.Grade 4 wastakenasgross
muscleactivityinvolvingthewholebody.Thepatientswere
includedinthestudy whentheydevelop shiveringwithat
leastaGradeof2.
The hemodynamic monitoring was continued after the
administrationof study drugs. The time taken to control
shivering,recurrenceandadverseeffectslikenausea,
vomi-ting, dry mouth and sedation score were observed. The
sedationscoreproposedbyFilosetal.wasfollowed.Grade1
wastakenasawakeandalertpatient.Grade2beingdrowsy
patientrespondingtoverbalstimuli.Grade3wastakenas
drowsybut arousabletophysical stimuliand Grade4 was
unarousablepatient.Themonitoringwascontinuedfortwo
hoursaftertheadministrationofspinalanesthesia.
Statisticalanalysiswasperformedusingastandard
sta-tisticalprogram,TheStatisticalPackageforSocialSciences
version17.0software(IBMCorporation,Armonk,NY,USA).
Demographic data were analyzed using One-way Analysis
of Variance (ANOVA)test. The timetakentocontrol
shiv-ering, heart rate and blood pressure were expressed as
mean±standarddeviationandstatisticalanalysiswasdone
byOne-wayANOVAwithposttest.Thelevelforallanalyses
wassetatp=0.05withap-valuelessthan0.05were
con-sidered statistically significant and p-value less than 0.01
were considered extremelysignificant. Ifp-value was
sig-nificantthenStudents’t-testwasdonebetweentwogroups
todeterminethestatisticalsignificance.Thesedationscore,
recurrencerateandadverseeffectswereanalyzedusingtwo
wayANOVAtestforblockdesign.
Results
Threehundredandtwelvepatientswererecruitedintothe
studyandaConsolidatedStandardsofReportingTrialsflow
diagramdepictingthepassageof participantsthroughthe
trialhasbeenprovidedinFig.1.10
The two groups were comparable with respect to the
demographic profileand therewas nostatistically
signifi-cant differenceas shown in Table 1. There were also no
significant baselinevariationsinhemodynamicparameters
and mean axillary temperature. The time taken to
con-trol shiveringwassignificantly faster indexmedetomidine
(5.76±1.14min)groupthantramadol(6.72±1.27min)and
clonidine(9.48±0.95min)group.Thep-valuewas<0.0001
whichwashighlysignificantbyOnewayAnalysisofvariance
Assessed for eligibility n=312 Excluded (n=222)
Did not develop shivering (n=205)
Randomized (n=90)
Allocation
Allocated to group T-Tramadol (n=30)
Lost to follow up (n=0) Discontinued intervention (n=0)
Analysed (n=30) Excluded from analysis (n=0)
Analysis
Analysed (n=30) Excluded from analysis (n=0)
Analysed (n=30) Excluded from analysis (n=0) Allocated to group C-clonidine
(n=30)
Allocated to group D-Dexmedetomidine (n=30)
Follow-up
Lost to follow-up (n=0) Discontinued intervention (n=0)
Lost to follow-up (n=0) Discontinued intervention (n=0)
•
Declined to participate (n=205)
•
Table1 Demographiccharacteristics.
Patientcharacteristics GroupT GroupC GroupD p-Value
Age(years) 37.42±6.27 36.84±5.87 35.78±6.76 0.596a
Bodyweight(kg) 66.65±7.46 68.73±8.34 67.34±7.62 0.578a
Height(cm) 166.34±10.45 164.42±11.23 162.72±10.72 0.433a
ASAphysicalstatus1/2 14/16 15/15 12/18 1.001a
Gender(M/F) 12/18 13/17 12/18 0.667a
Meandurationofanesthesia(min) 62.43±3.78 64.54±4.42 63.32±4.43 0.157a
Meanaxillarytemperature(◦C) 36.88±0.55 36.77±0.14 36.83±0.24 0.097a
Allvaluesaremean±SDornumbers.StatisticalanalysisbyOne-wayAnalysisofVariance(ANOVA)withposttest.
a Notsignificant.
(ANOVA)test.Thereweresignificantvariationsintheheart
rateaftertheadministrationofthestudydrugbetweenthe
threegroupsandisdepictedinTable2.Therewasreduction
inheartrateindexmedetomidineandclonidinegroupwith
nosignificant changesinthetramadolgroup.The changes
insystolicanddiastolicpressureafterdrugadministration
weregiveninTables3and4.Therewasreductioninsystolic
anddiastolicbloodpressuremoresointhe
dexmedetomi-dinegroupthanclonidineandtramadolgroups.
The sedation score was significantly higher in the
dexmedetomidinegroupwith70%ofpatientshavingascore
of2% and23.3%patients developing ascoreof 3(Fig.2).
However,nopatientinany groupdeveloped ascoreof 4.
Thesedationachievedduringthetreatmentofshiveringwas
beneficialfor these patientsunder spinal anesthesia. The
recurrenceratewassignificantlylessinthe
dexmedetomi-dinegroup(3.3%)andhighestinthetramadolgroup(23.3%).
Theclonidinegrouphadarecurrencerateof10%.The
shive-ringwasnotcontrolledintwopatientsintheclonidinegroup
andonein the tramadolgroupand rescuedrug pethidine
wasusedfor them.The incidence of vomitingwashigher
in the tramadol group (13.3%) than clonidine (3.3%) and
dexmedetomidinegroup(0patients).Howevertwopatients
developed bradycardia each in the dexmedetomidine as
wellasclonidine groupwhichrespondedwell toatropine.
Theincidenceofhypotensionwassignificantlyhigherinthe
dexmedetomidine(20%)thanclonidine(13.3%)andtramadol
(6.6%)groups.
Table2 Variationsinheartrateafterstudydrugadministration.
Time(min) GroupT(beats/min) GroupC(beats/min) GroupD(beats/min) p-Value Intergroup comparison whenp<0.05
0 73.72±4.68 74.9±5.21 74.41±4.25 0.625c
---10 76.83±3.78 70.42±3.17 68.53±2.49 <0.0001b <0.001d
<0.001e
0.013f
20 74.41±5.21 71.28±5.39 65.42±4.95 <0.0001b 0.0259d
<0.001e
<0.001f
30 70.5±3.94 72.39±4.27 68.42±4.83 0.002a 0.065d
0.060e
0.001f
40 71.31±3.19 71.43±3.55 69.39±2.73 0.023a 0.890d
0.065e
0.023f
50 71.19±4.82 72.37±4.57 70.33±5.03 0.258c
---60 72.1±4.04 72.32±4.44 71.49±3.89 0.734c
---StatisticalanalysisbyOne-wayANOVAwithposttest.Allvaluesaremean±SD.
Table3 Variationsinsystolicbloodpressureafterstudydrugadministration.
Time(min) GroupT(mmHg) GroupC(mmHg) GroupD(mmHg) p-Value Intergroup
comparison when(p<0.05)
0 108.32±9.56 107.54±8.72 108.47±9.52 0.916c
---10 104.65±7.41 102.53±9.58 98.68±10.72 0.047a 0.3417d
0.0149e
0.1478f
20 106.53±8.63 98.8±7.91 94.88±8.48 <0.0001b 0.0006d
0.0001e
0.0692f
30 104.59±8.29 103.5±9.48 99.39±9.48 0.069c
---40 104.89±10.42 103.6±6.92 103.77±9.38 0.834c
---50 102.66±6.83 104.7±8.99 102.79±10.29 0.582c
---60 103.58±9.82 102.69±10.69 102.29±8.73 0.872c
---StatisticalanalysisbyOne-wayANOVAwithposttest.Allvaluesaremean±SD.
aSignificant. b Highlysignificant. c Notsignificant. d GroupTvs.GroupC. e GroupTvs.GroupD. f GroupCvs.GroupD.
Discussion
Theshiveringisaprotectiveresponseoccurringaspartof
acentrallymediatedthermoregulatorydefensemechanism
to hypothermia.11 The shivering is a frequent
complica-tionunderregionalanesthesiaoccurringeither asa result
ofadecreaseincorebodytemperatureormisinformation
fromreceptors.12 The shivering underanesthesianotonly
increasestheoxygenconsumptionbutalsocauses
tachycar-dia,hypertensionandinterfereswiththemonitoringofpulse
oximeter,electrocardiogramandbloodpressure.Inspiteof
theavailabilityofnumerousdrugstotreatshivering,thereis
noconsensusdrugthateffectivelycontrolsshiveringwithout
anysideeffects.
The␣2agonistscommonlyusedtotreatshiveringactsby
decreasingthecentralthermosensitivitybysuppressingthe
neuronalconductance.13Theydecreasethereleaseof
nor-adrenalinefromtheaxonalterminalsinthehypothalamus.14
There is high density of ␣2 receptors in the
hypothala-mus and these receptors activation leads to hypothermia
byreducingthegenerationofheatbymetabolicactivity.15
Dexmedetomidinehasanadvantageinitsabilitytoproduce
dose dependent sedation and can be used as an
anes-theticadjuvant.16,17Tramadolactsbyinhibitingtheneuronal
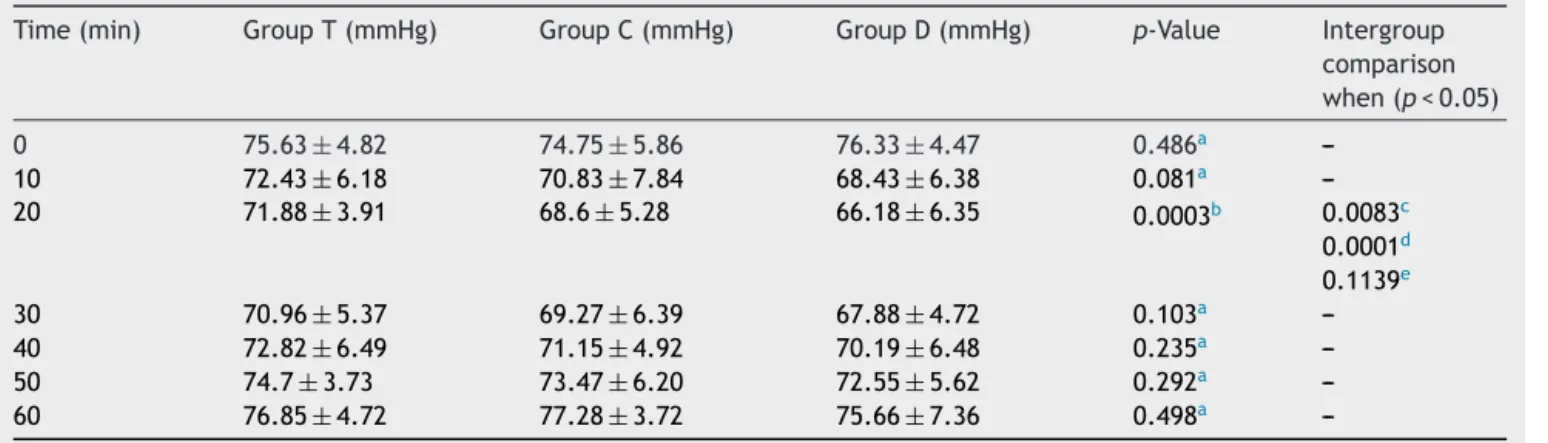
Table4 Variationsindiastolicbloodpressureafterstudydrugadministration.
Time(min) GroupT(mmHg) GroupC(mmHg) GroupD(mmHg) p-Value Intergroup
comparison when(p<0.05)
0 75.63±4.82 74.75±5.86 76.33±4.47 0.486a
---10 72.43±6.18 70.83±7.84 68.43±6.38 0.081a
---20 71.88±3.91 68.6±5.28 66.18±6.35 0.0003b 0.0083c
0.0001d
0.1139e
30 70.96±5.37 69.27±6.39 67.88±4.72 0.103a
---40 72.82±6.49 71.15±4.92 70.19±6.48 0.235a
---50 74.7±3.73 73.47±6.20 72.55±5.62 0.292a
---60 76.85±4.72 77.28±3.72 75.66±7.36 0.498a
---StatisticalanalysisbyOne-wayANOVAwithpost-test.Allvaluesaremean±SD.
25 12 5 16 19 21 Group T Group C Group D 2
0 0 0 6 7 2 20 15 5 0 1 2 Sedation score 3 4 10
Number of patients
Figure2 Sedationscore.
uptake of serotonin and noradrenaline and enhances the
hydroxytryptaminesecretion.18
The shiveringwas controlledfaster in the
dexmedeto-midine group and it took a longer time in the clonidine
group than tramadol group. Mittal et al. performed a
studyonthecomparisonofdexmedetomidineandtramadol
for post spinal anesthesia shivering. They concluded that
dexmedetomidine in a dose of 0.5mcg.kg−1 had a faster
onset tocontrol shivering in 2.52±0.44min.19 Bansal did
a comparative study on control of shivering with
cloni-dine, butorphanol and tramadol under spinal anesthesia.
They reported that tramadol was more effective than
clonidinein suppressingshivering.20 Ustaetal.conducted
a study on dexmedetomidine infusion for the prevention
of shivering during spinal anesthesia. They observed that
dexmedetomidine infusion of 0.4mcg.kg−1.h−1 was
effec-tiveinpreventingshiveringandprovidingsedationforminor
surgicalprocedures.21
The sedation achieved was better in the
dexmedeto-midine group than clonidine and tramadol group. Since
the surgery was done under spinal anesthesia, sedation
achievedwasbeneficialforthesepatients.However,none
ofthepatientsbecameunarousableinallthethreegroups.
Bozgeyik etal. performed a study on the effects of
pre-emptivetramadolanddexmedetomidineonshiveringduring
arthroscopy.Theyobservedthatinadditiontoits
effective-nessinpreventingshivering,dexmedetomidinewassuperior
inincreasingthelevelofsedationtopreventanxietywithout
sideeffects.22
Only onepatientinthedexmedetomidine group
devel-opedrecurrenceofshiveringwhereassevenpatientsinthe
tramadolgroup and threepatients in the clonidine group
encounteredrecurrencewhichwastreatedwithpethidine.
Mittal et al. reported the shivering recurrence was
dou-bledinthetramadolgroupthandexmedetomidinegroup.19
Bansaletal.reportedarecurrenceof26%withclonidineand
30%withtramadol.20Thesestudiesalsoconfirmthat
recur-renceofshiveringwasmuchlowerinthedexmedetomidine
groupthantramadolandclonidine.
The vomitingwasobservedmorefrequently inthe
tra-madol group with four patients and one patient in the
clonidine group. The bradycardia was observed in two
patientseachinclonidineanddexmedetomidine.However,
theincidenceofhypotensionwasobservedmorefrequently
inthedexmedetomidinegroup.Buthypotensionand
brady-cardia responded well to treatment. Kim et al. reported
hypotensionin 6.6% and bradycardia in 16.6% of patients
withdexmedetomidine 1mcg.kg−1.23 Mittal et al. didnot
haveanyhypotensionwithdexmedetomidine0.5mcg.kg−1
butvomitingwasobserved20%intramadolgroup.19
Thelimitationsofourstudyincludearelativelysmaller
sizesample.Thoughdexmedetomidinewaseffectiveinthe
treatmentof shivering,sideeffectswerereportedwithit
which was treatable. A larger study is needed to report
anidealdrug forshivering.Secondly, we didnotmeasure
thecoretemperaturebutusedtheaxillarytemperaturein
allpatients.Thirdly,theincidenceofshiveringwouldhave
beenlessifwehaveusedexternalwarmingdevicesforall
patients.
We conclude that dexmedetomidine is more effective
than tramadol and clonidine in the treatment of
shive-ring because of its faster onset, lesser recurrence rate,
and better sedation. The complications reported with
dexmedetomidine were easily treatable anddid not have
muchclinicalimpact. Tramadolis betterthanclonidinein
treating shivering but has more incidence of unpleasant
vomiting.
Conflicts
of
interest
Theauthorsdeclarenoconflictsofinterest.
References
1.DeWitteJ,SesslerDI.Perioperativeshivering:physiologyand pharmacology.Anaesthesiology.2002;96:467---84.
2.Weant KA, Martin JE, Humphries RL, et al. Pharmacologic options for reducing the shivering response to therapeutic hypothermia.Pharmacotherapy.2010;30:830---41.
3.HennemanE.Organizationof themotoneuronpool: thesize principle.In:MountcastleVB,editor.Medicalphysiology.14th ed.StLouis:CVMosby;1980.p.718---41.
4.Dhimar AA, Patel MG, Swadia VN. Tramadol for control of shivering (comparison with pethidine). Indian J Anaesth. 2007;51:28---31.
5.GiesbrechtGG,SesslerDI,MekjavicIB,etal.Treatmentofmild immersionhypothermiabydirectbody-to-bodycontact.JAppl Physiol.1994;76:2373---9.
6.CiofoloMJ,ClergueF,DevilliersC,etal.Changesinventilation, oxygenuptake,andcarbondioxideoutputduringrecoveryfrom isofluraneanesthesia.Anesthesiology.1989;70:737---41. 7.PowellR,BuggyD.Ondansetrongivenbeforeinductionof
anes-thesiareducesshiveringaftergeneralanesthesia.AnesthAnalg. 2000;90:1413---7.
8.Available from: https://pharmacy.uic.edu/departments/ pharmacy-practice/centers-and-sections/drug-information-group/2014/2013/september-2013-faqs
9.ParkSM,MangatHS,BergerK,etal.Efficacyspectrumof anti-shiveringmedications:meta-analysisofrandomizedcontrolled trials.CritCareMed.2012;40:3070---82.
11.Choi HA, Ko SB, Presciutti M, et al. Prevention of shive-ringduringtherapeutictemperaturemodulation:TheColumbia Anti-ShiveringProtocol.NeurocritCare.2011;14:389---94. 12.Chaturvedi S, Domkondwar G. Control of shivering under
regional anaesthesiausing Tramadol.AsianArchAnaesthesiol Resusc.2002;57:491---6.
13.BoulantJA.Theeffectoffiringrateonpreopticneuronal ther-mosensitivity.JPhysiol.1974;240:661---9.
14.PiperSN,MaleckWH,BoldtJ,etal.Acomparisonofurapidil, clonidine,meperidineandplaceboinpreventingpostanesthetic shivering.AnesthAnalg.2000;90:954---7.
15.QuanN,XinL,UngarAL,etal.Preopticnorepinephrine-induced hypothermiaismediatedby␣2-adrenoceptors.AmJPhysiol. 1992;262:407---11.
16.Gunalan S, Venkatraman R, Sivarajan G, et al. Comparative evaluation of bolus administration of dexmedetomidine and fentanylforstressattenuationduringlaryngoscopyand endo-trachealintubation.JClinDiagnRes.2015;9:06---9.
17.ElcıcekK,TekınM,KatıI.Theeffectsofintravenous dexmedeto-midineonspinalhyperbaricropivacaineanesthesia.JAnesth. 2010;24:544---8.
18.RaffaRB,FriderichsE,ReimannW, etal.Opioidand nonopi-oidcomponentsindependentlycontributetothemechanismof actionoftramadol,an‘‘atypical’’opioidanalgesic.JPharmacol ExpTher.1992;260:275---85.
19.Mittal G, Gupta K, Katyal S, et al. Randomised double-blindcomparativestudyofdexmedetomidineandtramadolfor post-spinalanaesthesiashivering. IndianJAnaesth.2014;58: 257---62.
20.Bansal P,Jain G. Control of shiveringwithclonidine, butor-phanol,andtramadolunderspinalanesthesia:acomparative study.LocalRegAnesth.2011;4:29---34.
21.UstaB,GozdemirM,DemirciogluRI,etal.Dexmedetomidine forthepreventionofshiveringduringspinalanesthesia.Clinics. 2011;66:1187---91.
22.Bozgeyik S, Mizrak A, Kilic¸ E, et al. The effects of pre-emptivetramadol and dexmedetomidine onshivering during arthroscopy.SaudiJAnaesth.2014;8:238---43.