REVISTA
BRASILEIRA
DE
ANESTESIOLOGIA
OfficialPublicationoftheBrazilianSocietyofAnesthesiologywww.sba.com.br
SCIENTIFIC
ARTICLE
Effects
of
ketamine
and
midazolam
on
emergence
agitation
after
sevoflurane
anaesthesia
in
children
receiving
caudal
block:
a
randomized
trial
夽
Ayse
Ozcan
a,∗,
Ayse
Gunay
Kaya
a,
Namik
Ozcan
a,
Gul
Meltem
Karaaslan
a,
Esen
Er
b,
Bulent
Baltaci
a,
Hulya
Basar
aaDepartmentofAnesthesiologyandReanimation,AnkaraTrainingandResearchHospital,Ankara,Turkey bAnesthesiologyandReanimationClinic,VanTrainingandResearchHospital,Van,Turkey
Received22November2013;accepted2January2014
Availableonline7February2014
KEYWORDS
Caudalblock; Children;
Emergenceagitation; Sevoflurane
anaesthesia; Ketamine; Midazolam
Abstract
Backgroundandobjectives: Emergence agitation is a common postanaesthetic problem in children after sevoflurane anaesthesia. We aimedto compare the effectsof ketamine and midazolamadministeredintravenously,beforetheendofsurgery,forpreventionofemergence agitationinchildrenwhoreceivedcaudalblockforpainreliefundersevofluraneanaesthesia. Methods:62AmericanSocietyofAnesthesiologistspatientclassificationstatusIchildren,aged 2---7years,scheduledforinguinalherniarepair,circumcisionororchidopexywereenrolledto thestudy.Anaesthesiawasinducedwithsevoflurane8%inamixtureof50%oxygenandnitrous oxide.Afterachievingadequatedepthofanaesthesia,alaryngealmaskwasplacedandthen caudalblockwasperformedwith0.75mLkg−1,0.25%bupivacaine.Attheendofthesurgery, ketamine0.25mgkg−1,midazolam0.03mgkg−1andsalineweregiventoketamine,midazolam andcontrolgroups, respectively.Agitationwas assessed usingPaediatric Anaesthesia Emer-genceDeliriumscaleandpostoperativepainwasevaluatedwithmodifiedChildren’sHospital ofEasternOntarioPainScale.
Resultsandconclusions:ModifiedChildren’sHospitalofEasternOntarioPainScalescoreswere foundhigherincontrolgroupthaninketamineandmidazolamgroups.PaediatricAnaesthesia EmergenceDeliriumscoresweresimilarbetweengroups.ModifiedChildren’sHospitalofEastern OntarioPainScaleandPaediatricAnaesthesiaEmergenceDeliriumscoresshowedasignificant decreasebytimeinallgroupsduringfollow-upinpostanaesthesiacareunit.Thepresentstudy resulted insatisfactory Paediatric Anaesthesia EmergenceDelirium scores which arebelow 10 inall groups. Asa conclusion, neither ketamine nor midazolam added to caudal block
夽 ThepresentstudywaspresentedintheCongressofTurkishSocietyofAnesthesiology,2011,inoralpresentationcontest.
∗Correspondingauthor.
E-mail:ayseongun@gmail.com(A.Ozcan).
0104-0014/$–seefrontmatter©2014SociedadeBrasileiradeAnestesiologia.PublishedbyElsevierEditoraLtda.Allrightsreserved.
undersevofluraneanaesthesiadidshowfurthereffectonemergenceagitation.Inaddition,pain reliefstillseemstobethemajorfactorinpreventingemergenceagitationaftersevoflurane anaesthesia.
©2014SociedadeBrasileiradeAnestesiologia.PublishedbyElsevier EditoraLtda.Allrights reserved.
PALAVRAS-CHAVE
Bloqueiocaudal; Crianc¸as; Incidênciade agitac¸ão; Anestesiacom sevoflurano; Cetamina; Midazolam
Efeitosdecetaminaemidazolamsobreaincidênciadeagitac¸ãopós-anestesiacom sevofluranoemcrianc¸assubmetidasaobloqueiocaudal:estudorandomizado
Resumo
Justificativaeobjetivos: Aincidênciadeagitac¸ãoéumproblemapós-anestésicocomumem crianc¸asapósaanestesiacomsevoflurano.Nossoobjetivofoicompararosefeitosdecetamina emidazolamadministradosporviaintravenosa,antesdotérminodacirurgia,paraprevenir aincidênciade agitac¸ãoem crianc¸assubmetidas ao bloqueiocaudal para alíviodadorsob anestesiacomsevoflurano.
Métodos: Foraminscritosno estudo62 pacientes pediátricos,entre 2-7anos, estado físico classificadode acordocomaSociedadeAmericana deAnestesiologistas(ASA: I), programa-dospara correc¸ãode hérniainguinal,circuncisãoouorquidopexia.A anestesiafoi induzida com sevoflurano a8% em uma mistura de oxigênio (50%) e óxido nitroso (50%). Depois de atingir a profundidade adequada da anestesia, uma máscara laríngea foi colocada e, em seguida,obloqueiocaudalfoifeitocombupivacaínaa0,25%(0,75mLkg−1).Nofimda cirur-gia,cetamina(0,25mgkg−1),midazolam(0,03mgkg−1)esoluc¸ãosalinaforamadministrados aosgrupos cetamina, midazolame controle, respectivamente.A incidência deagitac¸ão foi avaliadacomaescalaPaediatricAnaesthesiaEmergenceDelirium(PAED)eadornoperíodo pós-operatórioavaliadacomaescalamodificadaChildren’sHospitalofEasternOntarioPain Scale(mCHEOPS).
Resultadoseconclusões: OsescoresdedordaescalamodificadamCHEOPSforammaioresno grupocontroledoquenosgruposcetaminaemidazolam.OsescoresPAEDforamsemelhantes entreos grupos.Osescores dessas duasescalasmostraram umadiminuic¸ão significativado tempoemtodososgruposduranteoacompanhamentoemsaladerecuperac¸ãopós-anestesia. OpresenteestudoresultouemescoressatisfatóriosdaescalaPAED,queficaramabaixode10em todososgrupos.Comoconclusão,tantocetaminaquantomidazolam,adicionadosaobloqueio caudal sob anestesiacom sevoflurano,não mostraram efeitos adicionais sobre aincidência deagitac¸ão.Alémdisso,oalíviodadoraindapareceseroprincipalfator naprevenc¸ãoda incidênciadeagitac¸ãoapósanestesiacomsevoflurano.
©2014SociedadeBrasileiradeAnestesiologia.PublicadoporElsevierEditoraLtda.Todosos direitosreservados.
Introduction
Emergenceagitation(EA)isacommonpostanaesthetic prob-leminchildren aftersevofluraneanaesthesia.1---4 However,
the aetiology of EA has not yet been identified clearly. The predisposing factors are preschool age, preoperative anxiety, lack of premedication, type of surgery, awaken-ing in a strange environment.4,5 The incidence of EA had
beenreportedbetween10%and80%indifferentstudies.5,6,7
Although EA is also seen in pain-free procedures, pain is thoughttobethemajorcontributingfactorforEA.In addi-tiontopaintreatment,benzodiazepines,opioids,ketamine, alpha-2agonistsandpropofolhavealsobeenusedtoprevent EA.8
Inthepresentstudy,weaimedtocomparetheeffectsof ketamineandmidazolamforpreventionofEAafter sevoflu-raneanaesthesia,inchildrenwhoreceivedcaudalblockfor painrelief.
Methods
ThestudywasapprovedbytheInstitutionalEthics Commit-teeof AnkaraResearchandTrainingHospital(Chairperson AssocProfY.Aral)withprotocolnumber00165on13March 2008. Writteninformedconsentswere obtainedfrom par-ents of the children. Sixty-two ASA I children, aged 2---7 years who were scheduled for inguinal hernia repair, circumcision or orchidopexy were enrolled in the study. Exclusioncriteriawerementalretardation,physical devel-opmentaldelay,preoperativeagitationandcontraindication forcaudalblock.
depthofanaesthesia,alaryngealmaskwasplacedandthen childrenwerepositionedinthelateraldecubituspositionfor caudalanaesthesia.0.75mLkg−1,0.25% plain bupivacaine was injected using a 20-22 G caudal needle. Thereafter, anaesthesia was maintained with sevoflurane 3% in 50% oxygen---nitrous oxidemixture. No other hypnotic, muscle relaxantoranalgesicdrugwasadministeredduringsurgery. Skin incision wasmade 15min after caudal block. Caudal blockwasacceptedadequateifheartrateandblood pres-suredidnotincreasemorethan20%ofbaselinevalueafter skinincision.Thechildrenwithfailedblockwereexcluded fromthestudyandfentanyl2gkg−1wasadministered.
Patients were randomized into 3 groups as control (GroupC,n=20),midazolam(GroupM,n=21)andketamine (GroupK,n=21)groups.Ketamine0.25mgkg−1,midazolam 0.03mgkg−1andsalineatequalvolumeswereadministered intravenouslytochildrenapproximately10min beforethe endofsurgery,inketamine,midazolamandcontrolgroups, respectively in a blinded fashion.9,10 Then, sevoflurane
concentration was reduced, laryngeal mask was removed andinhaled anaesthetics werediscontinued.The children were allowed tobreathe 100% oxygen for 5min andthen transferredtothepostanaesthesiacareunit(PACU).Before the transfer to PACU, the caudal blocks were confirmed as functioning by lack of response to toe pinch. Heart rate,NIBP,andSpO2weremonitoredandthechildrenwere assessed in the PACU by an anaesthetist blinded to the study groups. Agitation was assessed using PAED (Paedi-atric Anaesthesia Emergence Delirium) scale at 0, 5, 10 and30thminandmCHEOPS(modifiedChildren’sHospitalof EasternOntarioPainScale)wasusedtoevaluate postopera-tive painat 5, 10and 30thmin in therecovery room.11,12
Allagitatedchildren withPAED scoremorethan10at the 10thmin received1mgkg−1 propofol,and ifthe agitation was notcontrolled in following 10min, propofol adminis-tration was repeated. Children with mCHEOPS score ≥6 receivedmorphine0.05mgkg−1ivforrescueanalgesic. Chil-drenwereobserved60mininthePACUandthendischarged totheward.The sideeffectslikenausea,vomiting, bron-chospasm,laryngospasm,desaturation,hallucination were alsorecorded.
Statistical analysis was performed by using Medcalc softwareprogramme(MedcalcSoftwarebvba,Mariakerke, Belgium),version11.3.3.0.Todeterminethesamplesize,a pilotstudywith10patientsreceivingonlycaudalanalgesia, likeincontrolgroup,wasperformed.WeobservedEAin6of 10patients.A40%reductioninEAwasconsideredtobe clin-icallysignificant, wecalculated20patientswererequired
foreachgroupwithtypeIerror(˛=0.05)andtypeIIerror (ˇ=0.2).Kolmogorov---Smirnovtestwasusedtoanalyzethe normaldistributionofmeasuredvariables.Intergroup com-parisonsweremadewithANOVAorKruskal---Wallisvariance test and Friedman test was used for with-in group com-parisons.Dataarepresentedasthemean±SDandmedian (minimum---maximum). Chi-square test was used for com-parisonofcategorical data.p Valueofless than0.05 was consideredstatisticallysignificant.
Results
Sixty-twochildrenwereenrolledinthestudy.Twochildren wereexcludedfromthestudybecauseofinadequatecaudal block.
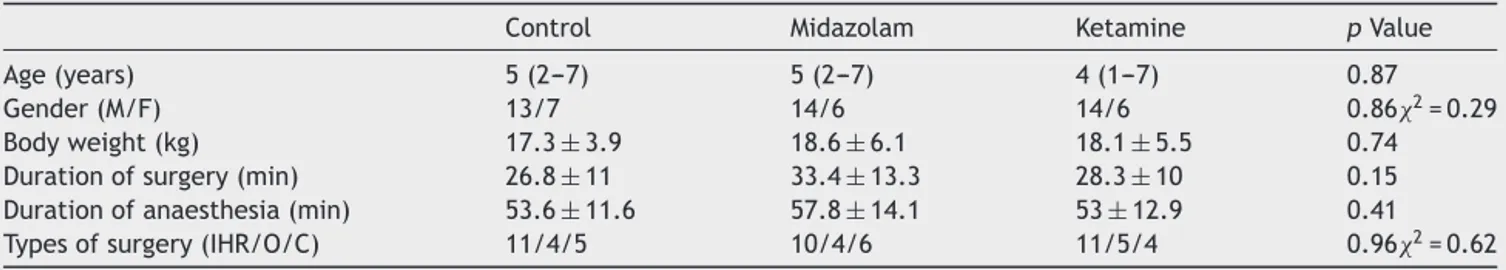
Thecharacteristicsofthepatients(age,gender,weight), durationof anaesthesiaand surgery and types of surgery weresimilarbetweengroupsandshowninTable1.
Systolic blood pressure values were found similar betweengroups at all measurement times.Systolic blood pressurewasmeasuredlowerwithinketaminegroupatthe 15thand30thminfollowingcaudalblockthanatinduction (p=0.026).
Heart rates were found similar between groups at all measurementtimes.Heartratesdecreasedsignificantly dur-inganaesthesiawithineachgroup.
Pain was evaluated using mCHEOPS scoring system at postoperative5,10and30mininPACU.Themedianvalues werefoundbelow6atallmeasurementtimesinallgroups. Scoreswerehigher incontrolgroup thanin ketamineand midazolamgroupsatallmeasurementtimes(Fig.1).When thegroupswereassessedindividually,therewere5,2and3 childrenat5thminwithmCHEOPS≥6incontrol,ketamine andmidazolamgroups,respectively.At10thmin,therewere 1 and 2 patients with mCHEOPS score ≥6 in midazolam andcontrolgroups,respectively.Onepatientofthecontrol groupalsohadahigherPAEDscoreatthesamemeasurement timeand received propofol. The other twochildren, one ineachgroup,withmCHEOPSscore≥6receivedmorphine 0.05mgkg−1ivasrescueanalgesic.ThemCHEOPSscoresof thepatientsinallgroupsdecreasedgraduallyduring follow-upinPACU.
PAEDscoresweresimilarbetweengroupsatall measure-menttimes (Fig.2).The median valuesofPAED scores of the groups were found below 10 except at the arrival of the control group toPACU. There were 11, 6 and 9 chil-dren with PAED score above 10 in control, ketamine and
Table1 Thecharacteristicsofthepatients,durationofanaesthesiaandsurgery.Valuesareexpressedasmean±SD,median (min-max).
Control Midazolam Ketamine pValue
Age(years) 5(2---7) 5(2---7) 4(1---7) 0.87
Gender(M/F) 13/7 14/6 14/6 0.862=0.29
Bodyweight(kg) 17.3±3.9 18.6±6.1 18.1±5.5 0.74
Durationofsurgery(min) 26.8±11 33.4±13.3 28.3±10 0.15 Durationofanaesthesia(min) 53.6±11.6 57.8±14.1 53±12.9 0.41 Typesofsurgery(IHR/O/C) 11/4/5 10/4/6 11/5/4 0.962=0.62
10
8
6
4
2
0
5 min 10 min 30 min
Group Ketamine Control Midazolam
Time
mCHEOPS
Figure1 mCHEOPSscoresofthegroups.*p<0.05vsketamine andmidazolamgroups.(Valuesareexpressedasmedian (min-max)).
20
18
16
14
12
P
AED 10
8
6
4
2
0
0 min 5 min 10 min 30 min
Group Ketamine Control Midazolam
Time
Figure2 PAEDscoresofthegroups.(Valuesareexpressedas median(min-max)).
midazolam groups, respectively at the arrival. Since EA couldshowspontaneousresolution, we observedthe chil-dren for 10min to administer the rescue drug propofol. In fact, 8, 6 and 8 children with EA showed spontaneous resolution in 10min in control, ketamine and midazolam groups,respectively.Threepatientsincontroland1patient in midazolam groups with PAED score above 10 received 1mgkg−1propofol,intravenously.AlsoPAEDscoresshowed
a significant decrease in all groups during follow up in PACU.
No side effects like nausea, vomiting, bronchospasm, laryngospasm,desaturation,hallucinationwererecordedin anypatientofthegroups.
AllpatientscouldbedischargedfromPACUafter60min follow-up.
Discussion
Inthepresent study,theeffects ofketamineand midazo-lamonEAwereassessedinagroupofpatientswhoareat highriskforEAregardingtotheirageandtheusedinhaled
anaesthetic. The results showed that ketamine or mida-zolam added to caudal block decreased mCHEOPS scores butdidnotaffectPAEDscoresinchildrenaftersevoflurane anaesthesia.
Pain,rapidemergenceinanunknownenvironment, sep-aration fromparents,and preoperativeanxiety aremajor factorscontributingtoEA.8
DifferentdefinitionsandscalesexistforevaluationofEA, butPAEDscaleispreferredinmostofthestudies.Ascoreof 10/20onthePAEDscalewasreportedasthebestthreshold pointfordeterminingthepresenceofEA.13However,Bajwa
etal.reportedthataPAEDscoregreaterthan12hadgreater sensitivity thana score of≥10.14 In ourstudy, we useda
scoreof≥10onPAEDscalefortheassessmentofEA. Painisthoughttobethemajorfactor thatcontributes to EA. In previous studies several analgesics including acetaminophen, ketorolac, fentanylwere administeredto preventEAaftersevofluraneanaesthesia.Inmostofthese studies, addition of analgesics reduced the incidence of EA.1,15,16 Caudal block is another preferred technique for
painreliefinchildren.Aouadetal.hadshownthatthe inci-dence of EA and pain scores in patients receiving caudal block were significantly lower compared to those receiv-ingintravenousfentanylundersevofluraneanaesthesiafor inguinal hernia repair.6 However,Aono etal. reported EA
in 40%ofchildren withcaudalblockfollowing sevoflurane anaesthesiaforminorurologicsurgery.17WeusedmCHEOPS
scoring system to evaluate andtoexclude pain asa con-tributingfactorofEA.
Althoughpainisthoughttobeimportantinaetiology,EA isalsoseeninpainfreeprocedures.2,3Thismayduetorapid
emergenceinanunknownenvironmentwithaltered cogni-tivefunctionwhichisanotherriskfactorforEA.Itisdifficult forthechildrentocooperatetoastrangeenvironmentupon rapid emergencefollowing anaesthesia.Therefore,agents thatprovidesedationatthetimeofemergencemaybe help-fulinpreventionofEA.17---19Thispointwasoneofthereasons
toestablishthisstudy.
Lowdoses of midazolam andketamine aresafely used for sedation. Chen et al. found that 0.05mgkg−1 mida-zolam in combination with 0.5gkg−1 of fentanyl at the endofsurgerywaseffectiveinreducingtheincidenceand severityofEA.19Ozcengizetal.found0.5mgkg−1oral mida-zolam,givenforpremedication,veryeffectiveinreducing EA.20Kararmazetal.hadshownthatoralketaminereduced
the incidence of EA after desflurane anaesthesiawithout delayingrecovery.21 Abu-Shahwanshowedthat
administra-tionof0.25mgkg−1iv ketamineattheendofanaesthesia reducedsignificantlytheincidenceandseverityofEAin chil-drenundergoingdentalrepair.22Dalensetal.administered
0.25mgkg−1ketamine,0.1mgkg−1nalbuphineandsalinein threegroupsofpatients,andtheyfoundsignificantlylower EAinketamineandnalbuphinegroupscomparedtocontrol without a delay in awakeningand discharge.9 In contrary
toliterature,ketamineandmidazolamdidnotaffectEAin childreninwhompainwasrelievedbycaudalblockinthe presentstudy.
parentalpresencealonegroups.23Inourstudy,parentswere
presentatthearrivaltoPACU.
Inchildrenitisdifficulttoassesspainandalsoitcanbe confusingtodifferentiatepainandEA.Inthepresentstudy, althoughthePAEDscoresweresimilar,mCHEOPSscoreswere statistically different among groups. Since all the caudal blockswerefunctioningandallpatientswereconsideredto befreeofpain,sedationcausedbyketamineandmidazolam might havereduced themCHEOPS scoresin thesegroups. ThismayduetotheparametersofmCHEOPSwhicharenot specificforpainandmayberelatedwithsedation.12,24
Inthisstudy,weacceptedparentstoPACUandprovided effective pain reliefwith caudalblock in all groups. This resultedin satisfactoryPAEDscores whicharebelow10in allgroups. As aconclusion, neitherketaminenor midazo-lamaddedtocaudalblockundersevofluraneanaesthesiadid showfurthereffectonEA.Inaddition,painreliefstillseems tobethe majorfactor in preventingEAafter sevoflurane anaesthesia.
Conflicts
of
interest
Theauthorsdeclaresnoconflictsofinterest.
References
1.Johannesson GP,Floren M, Lindahl SG. Sevoflurane for ENT-surgery in children. A comparison with halothane. Acta AnaesthesiolScand.1995;39:546---50.
2.UezonoS, GotoT, Terui K,et al. Emergence agitationafter sevofluraneversuspropofolinpediatricpatients.AnesthAnalg. 2000;91:563---6.
3.CraveroJ,SurgenorS,WhalenK.Emergenceagitationin pae-diatricpatientsaftersevofluraneanaesthesiaandnosurgery: a comparison with halothane. Paediatr Anaesth. 2000;10: 419---24.
4.LapinSL, AudenSM,Goldsmith LJ,et al. Effects of sevoflu-raneanaesthesiaonrecovery inchildren:a comparisonwith halothane.PaediatrAnaesth.1999;9:299---304.
5.Voepel-LewisT,MalviyaS,TaitAR.Aprospectivecohortstudyof emergenceagitationinthepediatricpostanesthesiacareunit. AnesthAnalg.2003;96:1625---30.
6.Aouad MT, Kanazi GE, Siddik-Sayyid SM, et al. Preopera-tive caudal block prevents emergence agitation in children following sevoflurane anesthesia. Acta Anaesthesiol Scand. 2005;49:300---4.
7.WelbornLG,HannallahRS, Norden JM,etal. Comparison of emergenceandrecoverycharacteristicsofsevoflurane, desflu-rane,andhalothaneinpediatricambulatorypatients.Anesth Analg.1996;83:917---20.
8.DahmaniS,StanyI,BrasherC,etal.Pharmacologicalprevention ofsevoflurane-anddesflurane-relatedemergenceagitationin children:ameta-analysis ofpublishedstudies.Br JAnaesth. 2010;104:216---23.
9.Dalens BJ, Pinard AM, Letourneau DR, et al. Prevention of emergence agitation after sevoflurane anesthesia for pedi-atriccerebralmagnetic resonanceimagingbysmalldosesof ketamineornalbuphineadministeredjustbeforediscontinuing anesthesia.AnesthAnalg.2006;102:1056---61.
10.KarlHW, CoteCJ,Mc CubbinMM,etal.Intravenous midazo-lamforsedationofchildrenundergoingprocedures:ananalysis of age- and procedure-related factors. Pediatr Emerg Care. 1999;15:167---72.
11.SikichN,LermanJ.Developmentandpsychometricevaluation ofthepediatricanesthesiaemergencedeliriumscale. Anesthe-siology.2004;100:1138---45.
12.SplinterWM,BassJ,KomocarL.Regionalanaesthesiafor her-niarepairinchildren:localversus caudalanaesthesia.CanJ Anaesth.1995;42:197---200.
13.BongCL,NgAS.EvaluationofemergencedeliriuminAsian chil-drenusingthePediatricAnesthesiaEmergenceDeliriumScale. PaediatrAnaesth.2009;19:593---600.
14.BajwaSA,CostiD,CynaAM.Acomparisonofemergence delir-iumscalesfollowing generalanesthesia inchildren. Paediatr Anaesth.2010;20:704---11.
15.Davis PJ, Greenberg JA, Gendelman M, et al. Recovery characteristics of sevoflurane and halothane in preschool-aged children undergoing bilateral myringotomy and pres-sure equalization tube insertion. Anesth Analg. 1999;88: 34---8.
16.Galinkin JL, Fazi LM, Cuy RM,et al. Use of intranasal fen-tanylinchildrenundergoingmyringotomyandtubeplacement duringhalothane andsevoflurane anesthesia.Anesthesiology. 2000;93:1378---83.
17.AonoJ,UedaW,MamiyaK,etal.Greaterincidenceofdelirium duringrecoveryfromsevofluraneanesthesiainpreschoolboys. Anesthesiology.1997;87:1298---300.
18.BreschanC,PlatzerM,JostR,etal.Midazolamdoesnotreduce emergencedeliriumaftersevofluraneanesthesia inchildren. PediatrAnesth.2007;17:347---52.
19.ChenJ,LiW,HuX,etal.Emergenceagitationaftercataract surgeryinchildren:acomparisonofmidazolam,propofoland ketamine.PediatrAnesth.2010;20:873---9.
20.OzcengizD,GunesY,OzmeteO.Oralmelatonin, dexmedetomi-dine,andmidazolamforpreventionofpostoperativeagitation inchildren.JAnesth.2011;25:184---8.
21.KararmazA,Kaya S,TurhanogluS, etal.Oralketamine pre-medicationcanpreventemergenceagitationinchildrenafter desfluraneanesthesia.PaediatrAnaesth.2004;14:477---82.
22.Abu-ShahwanI,ChowdaryK.Ketamineiseffectiveindecreasing theincidence ofemergenceagitation inchildrenundergoing dental repair under sevoflurane general anesthesia. Pediatr Anesth.2007;17:846---50.
23.Arai YC, Ito H, KandatsuN, et al. Parentalpresence during inductionenhancestheeffectoforalmidazolamonemergence behaviorofchildrenundergoinggeneralanesthesia.Acta Anaes-thesiolScand.2007;51:858---61.