REVISTA
BRASILEIRA
DE
ANESTESIOLOGIA
OfficialPublicationoftheBrazilianSocietyofAnesthesiologywww.sba.com.br
SCIENTIFIC
ARTICLE
Total
knee
replacement
induces
peripheral
blood
lymphocytes
apoptosis
and
it
is
not
prevented
by
regional
anesthesia
---
a
randomized
study
Juliusz
Kosel
a,∗,
Małgorzata
Rusak
b,
Łukasz
Gołembiewski
a,
Milena
D˛
abrowska
b,
Andrzej
Siemi˛
atkowski
aaDepartmentofAnesthesiologyandIntensiveTherapy,MedicalUniversityofBialystok,Bialystok,Voivodia,Poland bDepartmentofHaematologicalDiagnostics,MedicalUniversityofBialystok,Bialystok,Voivodia,Poland
Received1April2014;accepted16July2014 Availableonline28October2014
KEYWORDS
Totalknee
replacement;
Regionalanesthesia;
Generalanesthesia;
Lymphocytes; Apoptosis
Abstract
Background: Among the many changes caused by asurgical insult oneof theleast studied is postoperative immunosuppression.This phenomenon isan important cause ofinfectious complicationsofsurgerysuchassurgicalsiteinfectionorhospitalacquiredpneumonia.Oneof themechanismsleadingtopostoperativeimmunosuppressionistheapoptosisofimmunological cells.Anesthesiaduringsurgeryisintendedtominimizeharmfulchangesandmaintain perioper-ativehomeostasis.Theaimofthestudywasevaluationoftheeffectoftheanesthetictechnique usedfortotalkneereplacementonpostoperativeperipheralbloodlymphocyteapoptosis.
Methods:34patientsundergoingprimarytotalkneereplacementwererandomlyassignedto tworegionalanestheticprotocols:spinalanesthesiaandcombinedspinal---epiduralanesthesia. 11 patients undergoingtotal knee replacementunder generalanesthesia served as control group.Beforesurgery,immediatelyaftersurgery,duringfirstpostoperativedayandsevendays afterthesurgeryvenousbloodsamplesweretakenandtheimmunologicalstatusofthepatient wasassessedwiththeuseofflowcytometry,alongwithlymphocyteapoptosisusingfluorescent microscopy.
Results:Peripheral blood lymphocyteapoptosis was seenimmediately inthe postoperative periodandwasaccompaniedbyadecreaseofthenumberofTcellsandBcells.Therewere nosignificantdifferencesinthenumberofapoptoticlymphocytesaccordingtotheanesthetic protocol.ChangesinthenumberofTCD3/8cellsandthenumberofapoptoticlymphocytes wereseenontheseventhdayaftersurgery.
Conclusion: Peripheralbloodlymphocyteapoptosisisanearlyeventinthepostoperativeperiod thatlastsuptosevendaysandisnotaffectedbythechoiceoftheanesthetictechnique. © 2014SociedadeBrasileirade Anestesiologia.Publishedby ElsevierEditoraLtda.Allrights reserved.
∗Correspondingauthor.
E-mail:jkosel@umb.edu.pl(J.Kosel).
http://dx.doi.org/10.1016/j.bjane.2014.07.008
PALAVRAS-CHAVE
Artroplastiatotaldo
joelho;
Anestesiaregional;
Anestesiageral;
Linfócitos; Apoptose
Artroplastiatotaldojoelhoinduzapoptoseemlinfócitosdesangueperiféricoenãoé evitadaporanestesiaregional---estudorandômico
Resumo
Justificativaeobjetivo:Dentreasmuitasalterac¸õescausadasporumaferidacirúrgica,uma dasmenosestudadaséaimunossupressãopós-operatória.Essefenômenoéumacausa impor-tantedascomplicac¸õesinfecciosas relacionadasácirurgia, comoinfecc¸ão dosítiocirúrgico oupneumonianosocomial.Umdosmecanismosquelevamàimunossupressãopós-operatória éaapoptosedecélulasimunológicas.Duranteacirurgia,aanestesiasedestinaaminimizar asalterac¸õesprejudiciaisemanterahomeostaseperioperatória.Oobjetivodesteestudofoi avaliaroefeitodatécnicaanestésicausadaparaartroplastiatotaldejoelhosobreaapoptose emlinfócitosdesangueperifériconopós-operatório.
Métodos: 34 pacientes submetidos à artroplastia total primária de joelho foram randomi-camente designados para dois protocolos de anestesia regional: raquianestesia e bloqueio combinadoraqui-peridural.Onzepacientessubmetidosàartroplastiatotaldojoelhosob aneste-siageralformaramogrupocontrole.Antesdacirurgia,logoapósacirurgia,duranteoprimeiro diadepós-operatórioesetediasapósacirurgia,amostrasdesanguevenosoforamcolhidase oestadoimunológicodopacientefoiavaliadocomousodecitometriadefluxo,juntamente comapoptosedelinfócitosusandomicroscopiadefluorescência.
Resultados: Apoptoseemlinfócitosdesangueperiféricofoiobservadaimediatamenteno pós-operatórioeacompanhadaporumareduc¸ãodonúmerodecélulasTeB.Nãohouvediferenc¸a significativa no número de linfócitos apoptóticos de acordo com o protocolo anestésico. Alterac¸õesnonúmerodecélulasTCD3/8enonúmerodelinfócitosapoptóticosforam obser-vadasnosétimodiaapósacirurgia.
Conclusão:Apoptoseemlinfócitosdesangueperiféricoéumeventoprecocenoperíodo pós-operatórioqueduraatésetediasenãoéafetadopelaescolhadatécnicaanestésica. ©2014SociedadeBrasileiradeAnestesiologia.PublicadoporElsevierEditoraLtda.Todosos direitosreservados.
Introduction
Surgical trauma leads to a complex systemic response
includingsympatheticnervoussystemactivation,endocrine
response, and inflammatory and immunological
distur-bances.Simultaneouslywithinflammatoryresponse
activa-tion, which reduces the surgical stress damage area and
facilitatesrepairprocesses,immunologicalsystem
impair-ment occurs. This mechanism seems to have a defensive
function --- the organism defends itself from the
auto-immunologicalresponseinasituationof itsownantigens’
excessandastimulationoftheprocessesoftheir
recogni-tion.Unfortunately,italsoleadstoadverseconsequences
---directdamageofnaturaldefensivebarrierssuchasskinand
mucousmembranesinassociationwithimpairmentof
defen-sivemechanismsthatincreasesthepossibilityofinfections.
Inoncologicsurgerythatalsomeansmetastaticprogression
andaccelerationofneoplasmaldisease.
Postoperative lymphopoenia is a phenomenon that has
beenknownforalongtime,anditappliestoalllymphocyte
populationsanditsintensificationisdirectlyproportionalto
theextentoftheinjury.1Itiscausedbyaseriesof
perioper-ativeeventsandoneofthemhasbeenintensivelyexamined inrecentyears.Apoptosisistheprocessofprogrammedcell death, a termwhich was proposedin 1972 by Kerr etal. todescribemorphologicallydifferenttypesofcelldeath.2
Intensiveresearchwhichhasbeencontinuedintheyears fol-lowingallowedthespecificationofmechanismsleadingto programmedcelldeathandprecisecontrolofthecellcount.
Itis especiallyimportantin relationtotheimmunological system, since cell deficiency involves uncontrolled tumor cell growth and increases the risk of infection, whereas excessofimmunologicalcellsmayleadto autoimmunolog-icalresponse.Themainapoptosispathwaysare:extrinsic, associated withparticular ‘‘death ligand’’ (FasL, CD195), and intrinsic --- mitochondrial, which depends onphysical andchemicalfactorssuchashypoxiaortoxinsthatleadto changesinmitochondrialstructure.Thethirdpathdescribed inrelationtocytotoxiclymphocyteTis perforin/granzyme-mediatedapoptosis.3
Surgical trauma includes direct tissue damage as well asotherfactorsincluding:administeredanesthetics,blood lossfollowedbybloodtransfusions,hypothermia, immobil-ity,in someproceduresalsogeneralorlocalischemiaand reperfusioninjury.Alloftheabovecaninduceapoptosisof immunecells.Clinicalresearchshowedaninfluenceof surgi-calproceduresoncirculatingbloodlymphocyteapoptosis.4
Thisraisesaquestionaboutanoptimalanesthetictechnique andanestheticsusedinit.Researchfocusedontheinfluence of anesthetics onlymphocyte apoptosis in in vitro condi-tionsshowspro-apoptoticeffectofalmostallinhalational, intravenous and local anesthetics.5,6 Unfortunately, data
collected fromclinicalresearchare ambiguous. Compara-tiveresearchfrom2009didnotindicateregionalanesthesia beingsuperiortogeneralanesthesia(GA).7
cancer recurrenceand metastasis is less frequent among patients who underwentradical prostatectomy procedure withepiduralanesthesiacomparedtothesameprocedure with GA.8 Two years later another study partially
con-firmed previous observations and showed the superiority ofepidural anesthesiain patientsundergoinga prostatec-tomyprocedure.9Unfortunately, Canadianresearchersdid
not confirm these findings, however, their retrospective researchperiodwasshorter---3years.10 Similarlong-term
effectswereobservedinbreastcancerpatientswho under-wentamastectomy.Rarercancerrecurrenceandmetastasis wereobservedinpatientswhohadGAcombinedwith par-avertebral anesthesia.11 These findings, despite the short
periodofobservationandambiguousresults,suggestaneed forintensiveresearchontheinfluenceofanesthesiaonthe systemicdefensemechanisms.
Aim
of
the
study
The aimof thestudy wastheassessment oftheeffectof theanesthetictechniqueonlymphocytecountsinperipheral blood during perioperative period in patients undergoing primary total knee replacement (TKR) and the influence of lymphocyteapoptosis in thesechanges. The study was undertakenduringan18-monthperiodbetweenAugust2009 andApril2011attheDepartmentofOrthopedicSurgeryof theUniversityHospitalinBialystok.Thestudyprotocolwas approvedbytheUniversityBioethicsCommitteeofthe Medi-calUniversityofBialystok,noR-I-002/268/2009.Allpatients wereinformedabout thestudy protocol andgavewritten informedconsent.
Patients
and
methods
45 consecutive patients scheduled for primary TKR were recruited for the study. The inclusion criterion was osteoarthrosis.Exclusioncriteriawerediseases suchasRA (rheumatoidarthritis),systemiclupuserythrematosus(SLE), diabetesmellitusandtreatmentwithglucocorticosteroids, methotrexateandotherimmunosuppressiveandcytostatic drugswithin24monthsprecedingthesurgery.Demographic characteristicsof patientsarepresentedinTable1.Blood samples were taken at 4 time points: before the surgery (T1), directly after closing the surgical wound (T2), 24h afterthesurgery(T3)andonthe7thdayafterthesurgery (T4). The immunological status and microscopic study of apoptoticlymphocyteswereassessedforallbloodsamples.
All patients qualified to regional anesthesia were randomlyassignedtotwoanestheticprotocols:spinal anes-thesia(SA)andcombinedspinal---epiduralanesthesia(CSE). 11patientsundergoingsurgeryunderGAservedascontrol group.
GA:forinductionofGAfentanylwasused(FentanylWZF, Polfa Warszawa, Poland) at a dose of 1g/kg bw, propo-fol (1% Propofol-Lipuro, B.Braun, Germany) at a dose of 2mg/kg bw and suxamethonium chloride (Chlorsuccillin, Jelfa, Jelenia Gora, Poland) at a dose of 1mg/kg bw. Afterorotrachealintubationtheanesthesiawasconducted withcontinuous infusionof propofol,remifentanil(Ultiva, GlaxoSmithKline, UK) and cisatracurium (Nimbex, Glaxo-SmithKline, UK). Artificial ventilation was provided with themixtureof air andoxygen withFiO2 0.4.Tenminutes
beforetheend ofthesurgerythe infusionofremifentanil wasstoppedandintravenousmorphine(MorphinisulfasWZF, Polfa Warszawa, Poland) was administered at a dose of 0.1mg/kgbwand1.0gofparacetamol(Perfalgan, Bristol-Myers Squibb Pharmaceuticals, USA). Postoperative pain managementwasprovidedwithsubcutaneousmorphineper requestandparacetamol1.0gevery6h.
SAwasprovidedwith0.5%hyperbaricbupivacaine (Mar-cainaSpinalHeavy®,AstraZenecaPharmaceuticals,UK)at
adoseof2.8---3.4mLaccordingtotheheightofthepatient. Postoperative pain management was the same as in the groupofGA.
CSEwasdoneusingthe‘‘singlespace---doubleneedle’’ technique.Inthelateralpositionontheoperatedsidethe spinalneedle27Gpencil-pointshape(Balton,Poland)was introducedat theL3---L4level.Aftera doseof 2.8---3.4mL of hyperbaric bupivacaine (MarcainaSpinal Heavy®, Astra
ZenecaPharmaceuticals,UK)anepiduralcatheter(Perifix®
B.Braun, Germany)was inserted. The epidural space was identified using the ‘‘loss of resistance’’ technique with a saline-filled low resistance syringe. Negative aspiration testwastheconfirmationofpropercatheterposition.After motor recovery and before first pain symptoms a bolus of 8---12mL of 0.5% ropivacaine (Naropin®, Astra-Zeneca
Pharmaceuticals, UK) was given. Subsequentlycontinuous infusionof0.2%ropivacainewithfentanyl4g/mLatdose 6---10mL/hwasstarted.Theinfusionwasstoppedafter48h andtheepiduralcatheterwasremoved.
Surgery
Knee arthroplasty (TKR --- total knee replacement) was performed using implant Triathlon® (Stryker Co., USA) or
Table1 DemographiccharacteristicsofpatientsundergoingTKAwithrespecttoanesthesiaprotocol.
Typeofanesthesia
General Spinal CSE Total
No.ofpatients 11 17 17 45
AgeMedian(min-max) 69(59---84) 72(59---78) 72(59---77) 72(59---84)
Sex(M:F) 2:9 2:13 3:16 7:38
Timeofsurgeryinminutes 95 100 100 105
Vanguard® (Biomet Inc., USA). Both systems require
tib-ialandfemoralcomponentfixationwithbonecement,and
in both of them a plastic element for providing distance
andfriction reductionis inserted between the twometal
components.Allsurgeriesweredonewiththeuseofa
pneu-matictourniquetatthefemorallevelafterexsanguination
oftheextremitywithelasticgumtape.Thetourniquetwas
inflatedtothepressureof 150mmHgabovesystolicblood
pressureanddeflatedafterbonecement hardening.After
obtaining surgical haemostasis the autotransfusion drain
wasleftin. Afterstratified wound closure theautologous
bloodcollectionsystemforautotransfusionHandyVacTMATS
(Unomedical,A/S, Denmark) wasinitiated. The operation
woundwascoveredwithasteriledressing.Timeofsurgery
wasassessedasstartingfromthetimeoflegexsanguination
toskinclosure.
Postoperativetreatment
Autologousbloodtransfusionwasprovidedaccordingtothe
volume of collected blood, but not later than 6h after
thestart of theATS system.Surgical wound drainage was
performed up to the second postoperative day. If
neces-sary the leucoreduced Red Blood Cells Concentrate was
given,butinnocasewasitontheday ofthesurgery.All
patientshadthromboprophylaxiswithLMWH(lowmolecular
weightheparins)accordingtothePolishOrthopedicsSociety
Guidelines.12Allpatientswerealsogivenantibiotic
prophy-laxiswithcefazoline(Biofazolin®,Polpharma,Poland)1.0g
andamikacin(Biodacyna®,Polpharma,Poland)0.5g,30min
beforethestartofthesurgery.Postoperativerehabilitation wasstartedwithContinuousPassiveMotiondevice24hafter thesurgery.Activerehabilitation wasstarted onthethird postoperativeday.
Bloodsamplespreparation
Bloodsamplesforlaboratorystudywerecollectedinto2mL test-tubeswithEDTA in 4timepoints: beforethesurgery (T1),immediatelyafterclosingthesurgicalwound(T2),24h afterthesurgery(T3)and7daysafterthesurgery(T4).
The immunological status of peripheral blood lympho-cytes wasassessed withflow cytometryusing SimultestTM
IMK-LymphocyteKit(BDBiosciences,SanJose,CA,USA)and aFASCCaliburBDcytometer.Thekitallowsforquantitative assessmentoflymphocytecountaccordingtothefollowing surfaceantigens: Tcells(CD3) withsubpopulationsCD3/4 (Thelper),TCD3/8(Tsuppressor),Bcells(CD19),andNK cells(CD16/56).Theassessmentofapoptoticcellswas per-formedafterlymphocyteisolationwithHistopaque-1077and Histopaque-1119(Sigma---AldrichCo.,USA),and centrifuga-tionof peripheralbloodsamplesat 3000/minandstaining withethidiumbromide(10M)andacridineorange(10M). AcridineorangebindstoDNAandstainsitsstructuregreen. It also binds to cytoplasmic RNA staining it red-orange. Ethidium bromide does not cross the cytoplasmic mem-brane,soitonlystainsnecroticcellsorange.Thestructure oflymphocyteswasassessedwithfluorescentmicroscopyat 1000×magnification. 100consecutive cells wereassessed asalive,apoptoticornecrotic.13
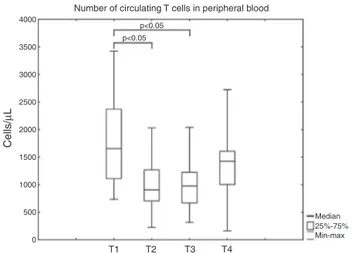
Number of circulating T cells in peripheral blood
Cells/
µ
L
4000
T1 T2 T3 T4
Median p<0.05
p<0.05
Min-max 25%-75% 3500
3000
2500
2000
1500
1000
500
0
Figure1 ThenumberofcirculatingTcells(CD3)beforethe surgery(T1),justaftersurgery(T2),24hpostoperatively(T3) and7daysaftersurgery(T4).Thebox-and-whiskerplotsshow minimalandmaximalvalues,25and75percentilesandmedians (horizontalbars).
Statisticalmethods
Statistical analysis wasperformed with‘‘Statistica 10.0’’ software(StatsoftInc.,Tulsa,OK,USA).Dataarepresented asamedianandas25and75percentilewithminimaland maximalvalues.TheWSchapiro-Wilktestwasusedtotest for normality.Sincethedata didnotfollownormal distri-bution we used a non-parametrical test for analysis. We comparedthedatainconsecutivetimepointsofthestudy withtheWilcoxontest andpatients’groupsinsingletime pointswithKruskal---Wallistest.Ap-valuelessthan0.05was consideredstatisticallysignificant.
Results
Immunologicalstatus
Immediatelyafterthesurgerythenumberofcirculating lym-phocyteswasdecreased.ThelowestcellcountwasseeninT cellpopulation.AttheT1timepointthenumberofTcells was reducedto 55% of baseline values (p<0.01). A small increase ofTcells wasseen 24h aftersurgery (upto58% ofpre-operative values).7daysafterthesurgery(T4)the numberofcirculatingTcells wasstill14%lowerthan pre-operatively(Fig.1). Thepattern ofparticular subtypesof Tcellchangeswasdifferent.Thegreatestdecreaseinthe numberofcirculatingTCD3/4 cellswasseen immediately afterthesurgery---andwas45%ofpreoperativevalues.24h afterthesurgeryweobservedanincreaseinthenumberof circulatingTCD3/4cellsto56%ofpreoperativevalues.On the seventhday of thestudy the number ofcirculating T CD3/4cells reached90%ofpreoperativevalues(Fig.2).A differentpatternofchangewasobservedinTCD3/8cells. ThegreatestdecreaseincirculatingTCD3/8cellswasseen 24haftersurgery---itdecreasedto55%ofpreoperative val-ues.ThenumberofCD3/8cellsonthe7thdaywasthesame asbeforethesurgery(Fig.3).
Number of circulating T CD3/4 cells in peripheral blood
Cells/
µ
L
2000
T1 T2 T3 T4
Median p<0.01 p<0.05
Min-max 25%-75% 1800
1600
1400
1200
1000
800
600
400
200
0
Figure2 ThenumberofcirculatingThcells(CD3/4)before thesurgery(T1),justaftersurgery(T2),24hpostoperatively (T3)and7daysaftersurgery(T4).Thebox-and-whiskerplots showminimalandmaximalvalues, 25and75 percentilesand medians(horizontalbars).
Number of circulating T CD3/8 cells in peripheral blood
Cells/
µ
L
T1 T2 T3 T4
Median p<0.05
p<0.05
Min-max 25%-75% 1800
1600
1400
1200
1000
800
600
400
200
0
Figure3 Thenumber ofcirculating Tscells(CD3/8)before thesurgery(T1),justaftersurgery(T2),24hpostoperatively (T3)and7daysaftersurgery(T4).Thebox-and-whiskerplots showminimalandmaximalvalues, 25and75 percentilesand medians(horizontalbars).
24hafterthesurgeryanincreaseinthenumberof circulat-ingCD19cellswasobserved,andonthe7thdayafterthe surgerythe numberof Bcells washigherthan beforethe surgery,althoughthedifferencedidnotachievestatistical significance(Fig.4).
Thesmallestdifferenceswereobservedinthenumberof circulatingNK(CD16/56)cells.Differencesinthenumberof circulatingNKcells didnotachievethelevelofstatistical significanceduringthetimeofthestudy(Fig.5).Changesin theimmunologicalstatusinthe3groupsofpatients accord-ingtotheanestheticprotocolwerestudied,butwedidnot observeanydifferencesatalltimepoints.
Peripheralbloodlymphocyteapoptosis
An all time pointswe assessed the numberof circulating lymphocytes for macroscopic signsof apoptosisusing flu-oroscopic microscopy. Before the surgery the number of
Number of circulating B cells in peripheral blood
Cells/
µ
L
T1 T2 T3 T4
Median p<0.05
Min-max 25%-75% 1400
1200
1000
800
600
400
200
0
Figure4 ThenumberofcirculatingBcells(CD19)beforethe surgery(T1),justaftersurgery(T2),24hpostoperatively(T3) and7daysaftersurgery(T4).Thebox-and-whiskerplotsshow minimalandmaximalvalues,25and75percentilesandmedians (horizontalbars).
Number of circulating NK cells in peripheral blood
Cells/
µ
L
T1 T2 T3 T4
Median
Min-max 25%-75% 1400
1200
1000
800
600
400
200
0
Figure5 ThenumberofcirculatingNKcells(CD16/56)before thesurgery(T1),justaftersurgery(T2), 24hpostoperatively (T3)and7daysaftersurgery(T4).Thebox-and-whiskerplots showminimalandmaximalvalues,25and75percentilesand medians(horizontalbars).
apoptoticlymphocytes variedfrom0to8%.Astatistically significantincreaseinthenumberofapoptoticlymphocytes wasobservedimmediatelyafterthesurgery.Thedifference betweenthenumberofapoptoticlymphocytesbeforethe surgery and after 24h did not achieve statistical signifi-cance,butontheseventhdayofthestudyitwashigherthan beforethesurgery.Aftercomparingthisdataforparticular anestheticprotocolsnostatisticallysignificantdifferences betweenthegroupswereobserved(Fig.6).
Discussion
Postoperative lymphopenia is a well-established and pre-cisely described phenomenon.14 It affects all lymphocyte
The percentage of apoptotic lymphocytes in peripheral blood with respect to anaesthetic technique
P
ercentage of lymphocytes (%)
T1 T2 T3 T4
Median Spinal General Combined spinal-epidural Anaesthetic technique p<0.05
p<0.05
Min-max 25%-75% 8
7
6
5
4
3
2
1
0
Figure 6 The number of circulating apoptotic peripheral blood lymphocytes with respect to anesthetic protocol (CSE group,GA group,spinal group) before the surgery(T1),just aftersurgery(T2),24hpostoperatively (T3)and7daysafter surgery(T4).Thebox-and-whiskerplotsshowminimaland maxi-malvalues,25and75percentilesandmedians(horizontalbars). Statisticallysignificantdifferenceswereseenbetween particu-lartimepoints,butnotbetweengroups.
circulatingT CD3/4 cells andT CD3/8 cells wasobserved very early, just after the end of surgery. Similar findings wereseeninpreviousstudiesandthisrefersto postopera-tiveandposttraumaticpatients.15,16Adecreasednumberof
circulatingTcellswasseen24h afterthesurgery,butthe numberofThcells(CD3/4)increased24hafterthesurgery achievingvaluessimilartovaluesseenpreoperatively.The numberof cytotoxicTCD3/8 cells wassignificantlylower thanbefore the surgeryand a statistically significant dif-ferencewasobserved untiltheseventhday aftersurgery. In contrast the number of circulating B cells (CD19) only immediatelyafterthesurgerywassignificantlylowerthan beforethesurgery. 24h afterthesurgery weobserved an increaseinthenumberofcirculatingBcells,and7daysafter thesurgerythenumberofcellswashigherthanbeforethe surgery,although thedifferencedidnotachieve thelevel ofstatisticalsignificance.Thecauseofsuchadifferent pat-ternofchangesmaybeexplainedbyapresenceofforeign substancessuchasjointimplantsorbonecement.17
NodifferencewasseeninthenumberofcirculatingNK cells.ThenumberofcirculatingNKcellsdidnotdiffer dur-ingtheentireobservationalperiod.Itisincontrasttomost previousstudies,whereasignificantdecreaseinthenumber ofcirculatingNKcellswasobserved.18,19Theexplanationfor
thisdifferencemaybethedifferenceinthepatient popu-lation---in our studygeneral patients withoutmalignancy werestudiedwhereasinthestudies mentionedabovethe patients were oncologic. The number and function of NK cellsisofparticularinteresttocliniciansbecausethesecells arethe firstline ofdefence againstneoplasmalcells. The possibilityof the influence of the anesthetic technique ---generalvs.regionalanesthesia---onthenumberandfunction ofNK cells wasevenstudied inmeta-analysis by Conrick-Martin and co-workers.20 The results of thisstudy donot
confirmthesuperiorityofregionaltechniquesoverGAbut maybe an importantcontribution tofurther studies. The slightinfluenceofanesthesiaandsurgeryonthenumberof circulatingNKcellsobservedinourstudymaybeexplained
by the exclusion of patients withneoplasmal disease and takingimmunosuppressiveagentsfromtheresearch.
The apoptosis of lymphocytes in response to surgical traumaisanoccurrencewhichwaswellconfirmedininvitro
and in vivo settings.4,21 It may be one of the causes of
posttraumatic and postoperativelymphopenia. This is the reason thequestion of the effect of theanesthetic tech-nique on peripheral blood lymphocytes may be clinically important.The optimalchoiceofananestheticprocedure andagentsshouldminimizetheimmunosuppressiveeffect ofsurgicalinsult.Wemaypointoutsuchapoptosis-inducing factorsas:preoperative---psychologicalstressandfasting, and intraoperative --- pneumatic tourniquet, tissue dam-age, bone cement and anesthetic agents used during the operation.22---24 Some of the factors initiated earlier are
maintainedinthepostoperativeperiod,butsomenewones, includinglong-termimmobilization,presenceofanimplant and complexpostoperative pain managementwith use of strong and long-acting opioids, also occur. In our study, immediately after the end of the surgery and the clos-ingof thesurgical wound, thepercentageof lymphocytes with macroscopic features of apoptosis was significantly higherthanpreoperatively.On thefirstpostoperativeday, 24h after surgery, the number of apoptotic lymphocytes wasalsohigherthanpreoperativelybutthedifferencedid not achieve a level of statistical significance. This may be explained by the manner of presenting the results ---the numberof apoptoticlymphocytes wascountedin 100 consecutive cells. A relatively lowernumber of apoptotic lymphocytes may be the result of the activation of lym-phopoiesis andthe appearance of newcells inperipheral blood.Confirmationofthisexplanationisanincreaseofthe number ofall lymphocytepopulations in peripheralblood on the first postoperative day. An increased percentage of apoptoticlymphocytes werealsoseen 7daysafter the surgerycomparedtopreoperatively.Itmeansthatnotonly intraoperativebutalsopostoperativefactorsmayaffectthe processesofapoptosis.
The effect of the anesthetic technique on peripheral blood lymphocyteapoptosis wasthe topic of few clinical trials.Pro-apoptoticeffectofvolatileandintravenous anes-thetics, local anesthetics and opioids was established in vitro.5,6Inoneofthestudiescomparingtheeffectofgeneral
and epidural anesthesia on peripheral blood lymphocytes apoptosis no difference was found in patients undergo-ing abdominal surgery.7 The difference wasthe patients’
population --- in the previous study patients were under-going abdominal surgery for nonmetastatic colon cancer. TKAisastrongproapoptoticstimulusbecauseofmajor tis-sue damage,use of pneumatictourniquet,blood loss and postoperativepain.Thechoiceofdrugs usedinthestudy, propofoland ropivacaine,haddiscreteor noinfluence on theperipheralbloodlymphocyteapoptosis.
Conclusion
notseeninrespecttoNKcells(CD16/56).Theconcomitant change is the increase of the percentage of lymphocytes withmacroscopicallyseenapoptoticchanges.The process of lymphocyte apoptosismay be partially responsible for postoperativelymphopoenia.Thechoiceof theanesthetic technique:GA,SAorCSE,inthisparticulartypeofsurgery, doesnotaffectthenumberofapoptoticlymphocytes.
Conflicts
of
interest
Theauthorsdeclarenoconflictsofinterest.
Acknowledgements
ThestudywasfinanciallysupportedbytheMedical Univer-sityofBialystok,Bialystok,Poland,Grantno.3-14594L.The authors thank Piotr Laskowski from the Institute of Soci-ology, Methodology andStatistics, University of Bialystok, Bialystok,Polandforhishelpfuladviceandsupervisionover statisticalanalyses.
References
1.KirovSM, Shepherd JJ,Donald KD. Intraoperativeand post-operativechangesinperipheralwhite bloodcellcounts: the contributionofstress.AustNZJSurg.1979;49:738---42.
2.KerrJF,WyllieAH,CurrieAR.Apoptosis:abasicbiological phe-nomenonwithwide-rangingimplicationsintissuekinetics.BrJ Cancer.1972;26:239---57.
3.ElmoreS.Apoptosis:areviewofprogrammedcelldeath.Toxicol Pathol.2007;35:495---516.
4.DeloguG,MorettiS,AntonucciA,etal.Apoptosisandsurgical trauma:dysregulatedexpressionofdeathandsurvivalfactors onperipherallymphocytes.ArchSurg.2000;135:1141---7.
5.OsmanES,KhafagyHF, Samhan YM,et al. Invivoeffects of differentanestheticagentsonapoptosis.KoreanJAnesthesiol. 2012;63:18---24.
6.WerdehausenR,FazeliS,BraunS,etal.Apoptosisinduction bydifferentlocalanestheticsinaneuroblastomacellline.BrJ Anesth.2009;103:711---8.
7.PapadimaA, Boutsikou M, LagoudianakisEE, et al. Lympho-cyteapoptosisaftermajorabdominalsurgeryisnotinfluenced byanesthetictechnique:acomparativestudyofgeneral anes-thesiaversuscombinedgeneralandepiduralanalgesia.JClin Anesth.2009;21:414---21.
8.Papadima A, Boutsikou M, Lagoudianakis EE, et al. Anes-thetic technique for radical prostatectomy surgery affects cancer recurrence: a retrospective analysis. Anesthesiology. 2008;109:180---7.
9.WuethrichPY,HsuSchmitzSF,KesslerTM,etal.Potential influ-ence of the anesthetic technique used during open radical prostatectomyon prostate cancer-relatedoutcome: a retro-spectivestudy.Anesthesiology.2010;113:570---6.
10.Tsui BC,RashiqS, SchopflocherD,et al.Epidural anesthesia andcancerrecurrenceratesafterradicalprostatectomy.CanJ Anesth.2010;57:107---12.
11.ExadaktylosAK,BuggyDJ,MoriartyDC,MaschaE,SesslerDI.Can anesthetictechniqueforprimarybreastcancersurgeryaffect recurrenceormetastasis?Anesthesiology.2006;105:660---4.
12.Zasady profilaktyki ˙zylnej choroby zakrzepowo-zatorowej w ortopediiitraumatologiinarz˛aduruchu.OrtopTraumatol Reha-bil.2009;11:86---92[inPolish].
13.MartinD,LenardoM.Morphological,biochemical,andflow cyto-metricassaysofapoptosis.CurrProtocMolBiol.2001[chapter 14:unit14.13].
14.Salo M. Effects of anesthesia and surgery on the immune response.ActaAnesthesiolScand.1992;36:201---20.
15.Bartal I, Melamed R, Greenfeld K, et al. Immune perturba-tionsinpatientsalongtheperioperativeperiod:alterationsin cellsurfacemarkersandleukocytesubtypesbeforeandafter surgery.BrainBehavImmun.2010;24:376---86.
16.Yadav K, Zehtabchi S, Nemes PC, et al. Early immunologic responsestotraumaintheemergencydepartmentpatientswith majorinjuries.Resuscitation.2009;80:83---8.
17.Anderson JM, McNally AK. Biocompatibility of implants: lymphocyte/macrophage interactions. Semin Immunopathol. 2011;33:221---33.
18.NgCS,LeeTW,WanS,etal.Thoracotomyisassociatedwith significantlymoreprofoundsuppressioninlymphocytesand nat-uralkillercellsthanvideo-assistedthoracicsurgeryfollowing majorlungresectionsforcancer.JInvestSurg.2005;18:81---8.
19.WangZY,WangCQ,YangJJ,etal.Whichhastheleastimmunity depressionduringpostoperativeanalgesia-morphine,tramadol, ortramadolwithlornoxicam?ClinChimActa.2006;369:40---5.
20.Conrick-MartinI,KellMR,BuggyDJ.Meta-analysisoftheeffect ofcentral neuraxialregional anesthesia compared with gen-eralanesthesia on postoperativenaturalkillerTlymphocyte function.JClinAnesth.2012;24:3---7.
21.YamadaR,TsuchidaS,HaraY,TagawaM,OgawaR.Apoptotic lymphocytes induced by surgical trauma in dogs. J Anesth. 2002;16:131---7.
22.PehlivanogluB,BayrakS,GurelEI,BalkanciZD.Effectofgender andmenstrualcycleonimmunesystemresponsetoacute men-talstress:apoptosisasa mediator.Neuroimmunomodulation. 2012;19:25---32.
23.PiresJ,CuriR,OttonR.Inductionofapoptosisinrat lympho-cytesbystarvation.ClinSci.2007;112:59---67.