www.bjorl.org
Brazilian
Journal
of
OTORHINOLARYNGOLOGY
ORIGINAL
ARTICLE
Impact
of
upper
airway
abnormalities
on
the
success
and
adherence
to
mandibular
advancement
device
treatment
in
patients
with
Obstructive
Sleep
Apnea
Syndrome
夽
,
夽夽
Renato
Prescinotto
a,b,∗,
Fernanda
Louise
Martinho
Haddad
a,
Ilana
Fukuchi
b,
Luiz
Carlos
Gregório
a,
Paulo
Afonso
Cunali
c,d,
Sérgio
Tufik
a,
Lia
Rita
Azeredo
Bittencourt
a,daDepartmentofPsychobiology,UniversidadeFederaldeSãoPaulo(UNIFESP),SãoPaulo,SP,Brazil bDepartmentofOtorhinolaryngology,FaculdadedeMedicinadoABC,SantoAndré,SP,Brazil cDentistryCourse,UniversidadeFederaldoParaná(UFPR),Curitiba,PR,Brazil
dDepartmentofMedicineandSleepBiology,UniversidadeFederaldeSãoPaulo(UNIFESP),SãoPaulo,SP,Brazil
Received9March2014;accepted6January2015 Availableonline7September2015
KEYWORDS Obstructivesleep apnea;
Removable orthodontic appliances;
Physicalexamination; Nose
Abstract
Introduction:The mandibular advancement device(MAD)is aoption totreatpatients with ObstructiveSleepApneaSyndrome(OSAS).
Objective: Toassesstheinfluenceofupperairwayabnormalitiesonthesuccessofand adher-encetoMADinpatientswithOSAS.
Methods:Prospectivestudywith30patientswithmildtomoderateOSASandindicationsfor MAD. The protocol included questionnaires addressing sleep and nasal complaints, polyso-mnography,andupperairwayassessment.Theanalyzedparametersofpatientswhoshowed therapeuticsuccessandfailureandthosewhoexhibitedgoodandpoortreatmentadherence werecompared.
Results:28patientscompletedtheprotocol;64.3%respondedsuccessfullytotreatmentwith MAD,and60.7%exhibitedgoodadherencetotreatment.Factorsassociatedwithgreatersuccess rateswereyoungerage(p=0.02),smallercervicalcircumference(p=0.05),andlowerAHIat baseline(p=0.05).Therewasapredominanceofpatientswithoutnasalabnormalitiesamong patientstreatedsuccessfullycomparedtothosewithtreatmentfailure(p=0.04),whichwas
夽
Pleasecitethisarticleas:PrescinottoR,HaddadFLM,FukuchiI,GregórioLC,CunaliPA,TufikS,etal.Impactofupperairwayabnormalities onthesuccessandadherencetomandibularadvancementdevicetreatmentinpatientswithObstructiveSleepApneaSyndrome.BrazJ Otorhinolaryngol.2015;81:663---70.
夽夽Institution:UniversidadeFederaldeSãoPaulo(UNIFESP),SãoPaulo,SP,Brazil.
∗Correspondingauthor.
E-mail:prescinotto@hotmail.com(R.Prescinotto).
http://dx.doi.org/10.1016/j.bjorl.2015.08.005
notobserved inrelationtoadherence.Neither pharyngealnorfacialskeletalabnormalities weresignificantlyassociatedwitheithertherapeuticsuccessoradherence.
Conclusion:MADtreatmentsuccesswassignificantlyloweramongpatientswithnasal abnor-malities;however,treatmentadherencewasnotinfluencedbythepresenceofupperairway orfacialskeletalabnormalities.
© 2015Associac¸ãoBrasileira de Otorrinolaringologiae CirurgiaCérvico-Facial. Publishedby ElsevierEditoraLtda.Allrightsreserved.
PALAVRAS-CHAVE Apneiadosonotipo obstrutiva;
Aparelhos ortodônticos removíveis; Examefísico; Nariz
Oimpactodasalterac¸õesdaviaaéreasuperiornaadesãoesucessodotratamento comaparelhointraoralnaSíndromedaApneiaObstrutivadoSono
Resumo
Introduc¸ão:OAparelhoIntraoral(AIO)éumaopc¸ãoparatratamentodaSíndromedaApneia ObstrutivadoSono(SAOS).
Objetivos: Avaliarainfluênciadas alterac¸ões daVASe esqueléticas faciaisatravésde uma avaliac¸ãoclinicasistematizadanosucessoeadesãoao(AIO)empacientescom(SAOS).
Método: Estudoprospectivoemqueforamavaliados30pacientescomSAOSleveamoderada eindicac¸ãodeAIO.Protocoloincluiuquestionáriosdesonoequeixasnasais;polissonografiae avaliac¸ãodaVASporrinoscopiaanterioreoroscopia.Osparâmetrosanalisadosforam compara-dosentrepacientescomsucessoeinsucesso,ecomboaemáadesãoàterapia.
Resultados: Completaramoprotocolo28pacientes.Osucessoao tratamentofoide64,3%e a adesão 60,7%. Os fatores associados ao sucesso foram menor idade, menor circunferên-ciacervicale menorIAH basal. Quantoàpresenc¸a dealterac¸ões nasais,houve predomínio depacientessem alterac¸ão nasalentre ospacientescomsucesso comparadosàqueles com insucesso (p=0,04); o que não foi observado em relac¸ão à adesão. Quanto às alterac¸ões faríngeasealterac¸õesesqueléticasfaciais,nãohouvesignificância.
Conclusão:OsucessodotratamentocomAIOfoisignificativamentemenornospacientescom alterac¸õesnasais,porémaadesãonãofoiinfluenciadapelapresenc¸adealterac¸õesdeVASou esqueléticasfaciais.
©2015Associac¸ãoBrasileira deOtorrinolaringologiaeCirurgiaCérvico-Facial.Publicadopor ElsevierEditoraLtda.Todososdireitosreservados.
Introduction
Thetreatment ofchoicefor ObstructiveSleepApnea Syn-drome (OSAS) is the use of continuous positive airway pressure(CPAP),especiallyinseverecases.1Inmildto
mod-erateandprimarysnoring cases,other treatmentscanbe
used,suchasthemandibularadvancementdevice(MAD).1,2
Itisestimatedthatnasalobstructionispresentin
approx-imately64%ofpatientswithOSASandmostofthesepatients
have associated anatomical alterations, such as deviated
septumandinferiorturbinatehypertrophy.3Althoughthere
havebeen studiesdemonstratingthe presenceor absence
ofanassociationbetweennasalalterationsandtheir
treat-mentwithCPAPadherence,3---5nostudieshavedemonstrated
whetherthenasalandupperairway(UA)alterationsmight
ormightnotinterferewithsuccessfultreatmentbyor
adher-encetoMAD.
Zengetal.obtaineddatasuggestingthatincreasednasal
resistance can negatively influence MAD treatment
out-comes;itrepresents, todate, theonlystudy inliterature
thatperformednasal assessmentthroughrhinomanometry
inpatientswithMAD.6
Thescarcityofstudiesthathaveassessedthepresence
ofUAandfacialskeletonalterationsusing
otorhinolaryngo-logicalphysicalexaminationinpatientswithOSASreferred
fortreatmentwithMAD,andhavealsoevaluatedthe
asso-ciation of these alterations with treatment success and
adherence,werethereasonsthatpromptedthisresearch.
Thus,thisstudyaimedtoevaluatetheinfluenceofUAand
facial skeletal alterations through a systematic and
stan-dardizedclinical assessmentofthesuccessandadherence
totreatmentofOSASwithMAD.
Methods
Sample
A total of 30 adult patients from the outpatient clinic
specializedin treatingsleep-relateddisordersduring 2006
and 2007, who had polysomnography-confirmed mild to
moderate OSASaccordingtothediagnostic criteriaof the
InternationalClassification ofSleepDisorders, 2005,7with
wassubmittedtotheethicsandresearchcommittee,CEP
No.0162/06.Patientswhoagreedtoparticipatesignedthe
informedconsent.
Inclusioncriteriawerepatientsaged25---65years,ofboth
genders,withmildtomoderateOSAS,withapnea---hypopnea
index(AHI)between5/hand30/h.
Exclusioncriteriaincludedpatientswithothersleep
dis-ordersratherthanOSAS,withprevious clinical orsurgical
treatmentsforOSAS,usersofalcohol,stimulants,or
seda-tives,thosewithlossofposteriordentalsupportthatwould
compromisetheretention ofMAD,thosewithactive
peri-odontal disease, and those with protrusion displacement
<6mm.
Protocol
Allpatientsweresubmittedtoanevaluationprotocol,which
consisted of applyinga sleepiness questionnaire (Epworth
SleepinessScale[ESS]),8anthropometricexamination(neck
circumference andbody mass index [BMI]),UAand facial
skeletalexamination,andovernightpolysomnographywith
MAD. The protocol was applied on the day the MAD was
providedandafter120daysofMADuse.
PatientsalsocompletedadailyquestionnaireonMADuse
andasleepdiary,whichwerecompletedduringall120days
ofthestudy.
Aftertheendoftheprotocol,itwaspossibletoseparate
patients between groups withgoodand poor compliance,
andbetweengroupswithtreatmentsuccessandtreatment
failurewithMAD.Theclinicaldata,polysomnographicdata,
andupperairwayandfacialskeletonphysicalexamination
findings werecomparedbetween the groups. The criteria
used for treatment success and adherence are described
below.
Toolsusedinthestudy
All dental assessment and follow-up of patients were
carried out by the same dentist, trained in the area
of sleep medicine. Before the study, all patients were
submitted to orthodontic assessment and the maximum
mandibularadvancementwasmeasured.Next,theMADwas
custom-made for each patient,withan initial mandibular
advancementof50%ofthemaximummandibular
advance-ment. After the start of the protocol, patients were
instructed to return weekly for the MAD to be advanced
by0.5mm ateach visit, untiltheyreached themaximum
comfortablemandibularadvancement.Duringthesereturn
visits,patientsbroughtthesleepandMADusediaries,which
willbefurtherdetailedbelow.Anyeventualcomplications
weretreated.
The MAD model used in the study was the Brazilian
Dental Appliance (BRD). BRD is an adjustable
mandibu-larrepositioningdevice.Ithastwoindependentexpanding
mechanisms--- screwspositionedwiththe longaxis in the
anteroposterior direction. Two independent palate rods
emerge from these expanding mechanisms, one on the
right and one on the left, which are inserted inferiorly
into twosmalltubes located in the anteriorportion,
dis-taltothemandibularcanines,oftheloweracrylicsupport
base.Thisproposeddesignallowssuccessiveadvancesinthe
mandibularposition,withoutpreventinglateralmandibular
movements.In other words, when the device is in place,
evenwhenthejawisinamoreanteriorposition,patients
mayperform lateral movements and have a small mouth
opening.9
Questionnaires
Thepatientswereassessedfordaytimesleepinessby
apply-ingthe ESS.8 The scale wasadministeredto both groups,
bothatthebaselineandattheendoftheassessment.The
sumofthetotalscorerangesfrom0(zero)to24,andscores
>9suggestexcessivedaytimesleepiness.
The sleep and MAD-use dairies consisted of notation
tables,whosepurposewastoprovidethenecessary
infor-mation for the study and that contained the days of the
monthandtheweek.Inthem,thepatientsrecordedaseries
ofinformationduringthestudyphases,includingthetime
theirsleepstartedandfinished,whentheyawakenedduring
thenight,andwhentheyputonorremovedthedevice.
The sleep and MAD-use diaries were used to define
whetherpatientshadgoodorpooradherencetoMAD,with
theformerbeingthosewhohaduseditformorethan90%
ofthetimeinthepreviousweek.
Upperairwayexamination3,10
Upperairway(UA)physicalexaminationconsistedof
ante-rior rhinoscopy, oroscopy, and flexible fiberoptic nasal
laryngoscopy.Patientsconsideredashavingnasalalterations
were thosewith septal deviation grade II (deviation that
compressestheinferiornasalturbinate)orIII(deviationthat
compressestheinferiornasalturbinate,touchingthelateral
wall),orthosewithgradeIseptaldeviation(deviationthat
doesnottouchtheinferiornasalturbinate)associatedwith
frequentnasalobstructioncomplaints(presenteverydayor
almosteveryday)orcomplaintsoffrequentrhinitis
(rhinor-rheaand/orsneezingand/orpruritus,everydayoralmost
everyday),orthosewithinferiorturbinatehypertrophyon
physicalexamination.
Thosewithpharyngealabnormalitieshadthreeormore
ofthefollowingalterations:softpalatewebbing,posterior
softpalate,thicksoftpalate,longuvula,andthickuvula.
ThevariablesmodifiedMallampaticlassificationandsize
ofpalatinetonsilswasstudiedseparately,withgradeIIIand
IVtonsils(occupying morethan 50% of theoropharyngeal
space)consideredhyperplastic.
Inaddition,patientswithpresenceorabsenceoffacial
skeletal alterations were grouped, considered as present
when one or more of the following alterations were
observed:retrognathiaat facialprofileassessment, ogival
hardpalate,orAngleclassIIdentalocclusion.
PolysomnographywithMAD
OvernightpolysomnographywithMADwasperformedby
pre-viously trained professionals, after 120 days of use. The
polysomnographydeviceusedwasanEMBLAcomputerized
system(EMBLATMS7000;EMBLASystems,Inc.---Broomfield,
byelectroencephalography(C3/A2,C4/A1,O1/A2,O2/A1),
bilateral electro-oculography, submental and tibial
elec-tromyography,electrocardiography(modifiedV2),oraland
nasalbreathingthroughathermistorandnasalflowthrough
acannulawithpressuretransducer,thoracicandabdominal
movements by uncalibrated inductance plethysmography,
snoringbyamicrophone,oxyhemoglobinsaturationbypulse
oximetry,andbodypositionsensor.
Sleep staging was performed by a trained
polysomno-graphist, based on the criteria of Rechtschataffen and
Kales.11 Respiratory and arousal events, as well as
spo-radic lower-limb movements, wereanalyzed according to
criteria established by the American Academy of Sleep
Medicine.12
Polysomnographywasalsousedtodefinewhichpatients
achievedtreatmentsuccess,asa50%AHIreductionand≤10
events/hdefinedthiscriterion.
Statisticalanalysis
TheKolmogorov---Smirnovnormalitytestwasappliedforall
variables,whichwereexpressedasmeanandstandard
devi-ation,astheyshowednormaldistribution.
Student’s t-test wasused for comparison between the
groupsforindependentsamplesandGLM(two-wayrepeated
measuresANOVA). Student’st-test fordependent samples
wasusedforcomparisonsbeforeandaftertreatmentinall
patients.
The chi-squared test was usedto compare categorical
variables.A logisticregression model wasalso used,with
treatmentsuccessandadherenceusedasdependent
varia-bles.Thesignificancevaluewassetat0.05andthesoftware
usedwasStatistic6.1.
Results
Of the 30 selected patients, two did not return for the
assessmentand,therefore,28completedtheprotocoland
wereincludedin thestudy.Nopatientsstoppedusingthe
MADduringtheprotocol.
As for the assessed descriptive data, the mean age
of patients was 48.8±11.3 years; nine (32.1%) were
males and 19 (67.9%) were females. The mean BMI was
27.4±3.8kg/m2, and the mean neck circumference was
38.3±3.3cm.
After all patients had completed the baseline
assess-ment prior tousing MAD andhad achieved the maximum
comfortableprotrusion with MAD, the questionnairesand
polysomnographicparametersrevealedsomesignificant
dif-ferences:decrease in the Epworth Sleepiness Scale (ESS)
score from 13.4±6.1 to 11.7±6.3 (t26=2.47; p=0.02);
reduction of AHI from 17.5±8.8 to 8.8±6.0 (t27=6.2,
p<0.001); decreased arousal index, from 15.9±6.7 to
10.1±5.1(t27=4.5;p<0.001),anddecreaseinthe
percent-ageoftimewithoxygensaturation<90%,from0.71±1.4to
0.07±0.14(t26=2.5,p=0.017).
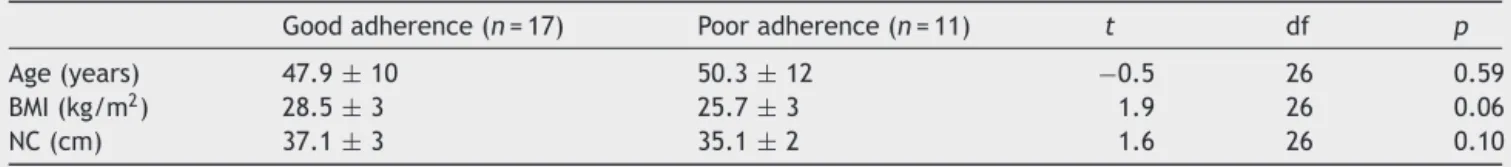
Of the28 patients, 17 (60.7%) had goodadherence to
MADuse,whereas11(39.3%)showedpooradherence.The
clinicalparametersatbaselineshowednostatistically
sig-nificantdifferencesbetweenthegoodandpooradherence
groups(Table1).
The AHI values (F=4.5; p<0.05) and arousal index
(F=6.9;p<0.05)differedbetweenthegroupsatbaseline,
andwerehigherinthepooradherencegroup(Table2).
WithuseoftheMADinbothgroups(bothgoodandpoor
adherence)therewasadecreaseintheESSscore(F7.1=5.9,
p<0.05), AHI (F=41.8; p<0.05), arousal index (F=24.4;
p<0.05),aswellasinthepercentageofdesaturationtime
below90%(F=8.18;p<0.05;Table2).
Ofthe28 patients,18 (64.3%)attained treatment
suc-cess, according tothe standard criteria. When comparing
the two groups at baseline --- successful and
unsuccess-ful treatment --- the only clinical parameter that showed
a statistically significant differencewas a youngerage in
thetreatmentsuccessgroup(44.8±9vs.56±10;t=−2.8;
df=26;p<0.001;Table3).
When comparing the groups with treatment success
and failure at baseline, therewere no differences in the
ESS and PSG parameters, but after treatment with MAD,
it was observed that the patients in the success group
hadlowerAHI values(F=14.2;p<0.01)andarousal index
(F=7.1;p<0.05),asexpectedbytheadoptedsuccess
crite-ria(Table4).
When patients in both groups were assessed together
(treatment successandfailure),afterMADuse,therewas
a reduction in the ESS (F=5.9; p<0.05); AHI (F=28.2,
p<0.001); arousal index per hour of sleep (F=13.0;
p<0.01); and the percentage of desaturation time <90%
(F=6.0;p<0.05;Table4).
When assessed individually or in groups, the variables
usedtoformthegroupsofpatientswithpharyngeal,nasal,
and craniofacial alterations showed no significant
differ-encesinrelation totreatmentadherence(Table5).Asfor
treatment success, it was observed that the presence of
obstructiveseptaldefects(gradesIIorIII;p=0.04)and
pres-enceof nasalalterations(p=0.04) weremorefrequent in
thetreatmentfailuregroup(Table6);thiswasnotobserved
forthepharyngealandcraniofacialvariables.
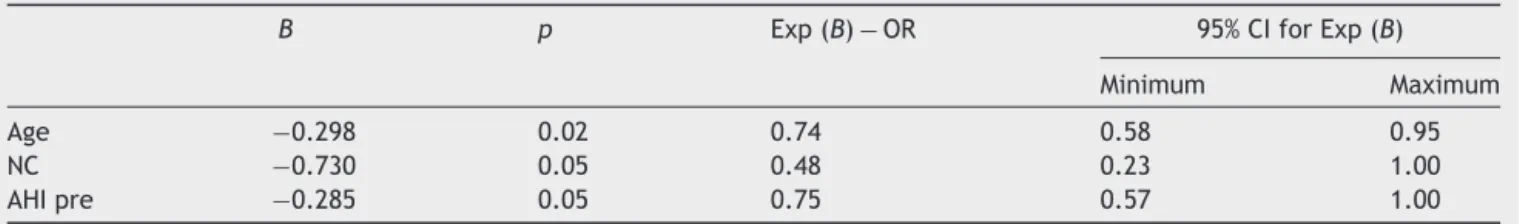
Thelogistic regressionmodel wasusedtoidentify
fac-tors associated with treatment adherence and success.
The following variables were included: age, gender, neck
Table1 ComparisonofclinicalparametersbetweenpatientswithgoodandpooradherencetoMADatbaseline.
Goodadherence(n=17) Pooradherence(n=11) t df p
Age(years) 47.9±10 50.3±12 −0.5 26 0.59
BMI(kg/m2) 28.5±3 25.7±3 1.9 26 0.06
NC(cm) 37.1±3 35.1±2 1.6 26 0.10
BMI,bodymassindex;NC,neckcircumference.
Table2 ComparisonoftheEpworthSleepinessScaleandpolysomnographyparametersbetweenpatientswithgoodandpoor adherencetothemandibularadvancementdevice(MAD)atbaselineandafter120daysofMADuse.
Goodadherence(n=17) Pooradherence(n=11) p(groupand timeinteraction)
Basal WithMAD Basal WithMAD
ESS 13.6±6 12.1±6a 12.0±6 9.6±6a 0.74
AHI(events/hour) 14.7±7 7.5±5a 23.2±9b 11.3±6a 0.18
SE(%) 87.2±5 87.6±5 88.3±9 86.0±9 0.15
N3(%) 18.1±5 17.7±7 18.2±5 21.2±11 0.32
REM(%) 18.9±3 19.3±4 20.0±6 22.3±6 0.66
AI(events/hour) 13.3±6 9.2±4a 20.7±4b 11.6±5a 0.09
SpO2MIN(%) 86.3±3 87.4±5 85.2±4 88.4±2 0.34
SpO2<90%(%) 0.4±1 0.04±0.1a 1.3±1.9 0.1±0.2a 0.18
ESS,EpworthSleepinessScale;AHI,apnea/hypopneaindexperhourofsleep;SE,sleepefficiency;N3,percentageofslow-wavesleep; REM,percentageofrapideyemovementsleep;AI:arousalindexperhourofsleep,SpO2MIN:minimumoxyhemoglobinsaturation;SpO2
<90%,percentageofdesaturationtime<90%;NS,non-significantstatisticalvalue.GLMtestforrepeatedmeasures(two-wayANOVA). Statisticallysignificantp-value<0.05.
a p<0.05(baseline×withMAD).
b p<0.05(goodadherence×pooradherenceatbaseline).
Table3 Comparison ofclinical parametersbetween patients showing successful andunsuccessfultreatment with MAD at baseline.
Successful(n=18) Unsuccessful(n=10) t df p
Age(years) 44.8±9 56±10 −2.8 26 <0.001
BMI(kg/m2) 27.1±4 28±3 −0.6 26 0.54
NC(cm) 36.3±3 36.4±2 −0.07 26 0.94
BMI,bodymassindex;NC,neckcircumference.
Statisticallysignificantp-value<0.05(Student’st-testforindependentsamples).
circumference, ESS, AHI, arousal index, BMI, pharyngeal alterations,nasalalterations,andcraniofacialalterations. The findings did not show statistically significant factors associated withadherence; however,regarding treatment success, the younger the age (OR: 0.74 [0.58---0.95];
p=0.02), the smaller the neck circumference (OR: 0.48 [0.23---1.00]; p=0.05) and the lower the baseline AHI
(OR: 0.75 [0.57---1.00]; p=0.05), the greater the success (Table7).
Discussion
Themainfindingofthisstudywasthatsuccessfultreatment
withMADwassignificantlylesslikelyinpatientswithnasal
Table4 ComparisonoftheEpworthSleepinessScaleandpolysomnographyparametersbetweenpatientsshowingsuccessful andunsuccessfultreatmentwithMADatbaselineand120daysafterMADuse.
Successful(n=18) Unsuccessful(n=10) p(groupand timeinteraction)
Basal WithMAD Basal WithMAD
ESS 13.8±4 11.9±5a 11.8±8 10.0±7a 0.95
AHI(events/hour) 15.2±8 5.2±2a 22.3±8 15.8±5a,b 0.26
SE(%) 89.0±5 89.3±5 85.0±9 82.8±8 0.34
N3(%) 17.5±6 20.2±8 19.4±4 16.3±10 0.09
REM(%) 19.4±5 20.7±4 19.1±4 19.6±7 0.71
AI(events/hour) 14.7±6 7.7±3a 17.9±6 14.5±5a,b 0.22
SpO2MIN(%) 86.2±3 88.9±2 85.4±3 85.6±6 0.27
SpO2<90%(%) 0.6±1 0.03±0.05a 0.9±1 0.1±0.2a 0.71
ESS,EpworthSleepinessScale;AHI,apnea/hypopneaindexperhourofsleep;SE,sleepefficiency;N3,percentageofslow-wavesleep; REM,percentageofREMsleep;AI,arousalindexperhourofsleep;SpO2MIN,minimumoxyhemoglobinsaturation;SpO2<90%,percentage
ofdesaturationtime<90%;NS,non-significantstatisticalvalue.GLMtestforrepeatedmeasures(two-wayANOVA). Statisticallysignificantp-value<0.05.
a p<0.001(basal×withMAD).
Table5 Comparisonofupperairwayassessmentand cra-niofacialparametersbetweenpatientswithgoodandpoor adherencetoMADatbaseline.
Individualvariables Good adherence (n=17)
Poor adherence (n=11)
p
Softpalatewebbing 11(64.7%) 9(81.8%) 0.30 Posteriorsoftpalate 6(35.3%) 5(45.4%) 0.44 Thicksoftpalate 3(17.6%) 1(9%) 0.48 Thickuvula 10(58.8%) 7(63.6%) 0.56 Longuvula 10(58.8%) 5(45.4%) 0.38 Pharyngealalteration 9(52.9%) 6(54.5%) 0.62 MMIclassIII/IV 16(94.1%) 10(90.9%) 0.64 GradeIII/IVpalatinetonsils 1(5.9%) 0(0.0%) 0.60 ClassIIdentalocclusion 1(5.9%) 1(9%) 0.64 Retrognathia 1(5.9%) 2(18.2%) 0.34 Craniofacialalteration 11(64.7%) 6(54.5%) 0.44 Ogivalhardpalate 9(52.9%) 4(36.4%) 0.32 Frequentnasalobstruction 11(64.7%) 4(36.4%) 0.14 Frequentrhinopathy
complaint
10(58.8%) 5(45.4%) 0.38
GradeIseptaldeviation 8(47%) 4(36.4%) 0.43 GradeII/IIIseptaldeviation 3(17.6%) 2(18.2%) 0.67 Inferiornasalturbinate
hypertrophy
10(58.8%) 4(36.4%) 0.22
Nasalalteration 10(58.8%) 5(45.5%) 0.38
MMI,modifiedMallampatiindex;p,p-value(chi-squaredtest).
alterations;thiswasnotinfluencedbythepresenceofother abnormalities.However,therewasnoinfluenceof UAand facialskeletalalterationsontreatmentadherence.
Whenpatients wereassessedfor adherencebeforeand afterMADtreatment,itwasobservedthatthosewithgood adherence(60.7%),accordingtothecriteriaused,hadlower values of AHI and arousals at baseline, suggesting that patientsinthisgrouphadamilderconditionthanthosein thepooradherencegroup.Althoughthestudiesare contra-dictorywhenstatingtheassociationbetweenOSASseverity andadherence toMAD,13,14 it is knownthat MAD is more
effectiveinpatientswithmildOSAS,inwhomanormalAHI
canbereachedmoreeasilyand,therefore,wherethe
dis-easeistreatedinamoresatisfactoryway.Thus,inthisgroup
ofpatientswithlowerAHIvaluesandlesssleep
fragmenta-tion,sleepconsolidationwasprobablymoreeffectiveand,
consequently,deviceusewaslonger-lastingandmayhave
alteredtheadherenceinapositivemanner.
The authors did not observe any association between
adherence to MAD treatment and any of the assessed
Table6 Comparisonofupperairwayassessmentand cra-niofacialparametersbetweenpatientswithsuccessfuland unsuccessfultreatmentwithMADatbaseline.
Individualvariables Successful (n=18)
Unsuccessful (n=10)
p
Softpalatewebbing 13(72.2%) 7(70%) 0.61 Posteriorsoftpalate 6(33.3%) 5(50%) 0.32 Thicksoftpalate 3(16.7%) 1(10%) 0.55 Thickuvula 13(72.2%) 4(40%) 0.10 Longuvula 11(61.1%) 4(40%) 0.25 Pharyngealalteration 12(66.7%) 3(30%) 0.07 MMIclassIII/IV 16(88.9%) 10(100%) 0.40 GradeIII/IVpalatine
tonsils
1(5.5%) 0(0.0%) 0.64
ClassIIdentalocclusion 2(11.1%) 0(0%) 0.40 Retrognathia 1(5.5%) 2(20%) 0.28 Ogivalhardpalate 9(50%) 4(40%) 0.46 Craniofacialalteration 11(61.1%) 6(60%) 0.66 Frequentnasal
obstruction
10(55.5%) 5(50%) 0.54
Frequentrhinopathy complaint
10(55.5%) 5(50%) 0.54
GradeIseptaldeviation 8(44.4%) 4(40%) 0.57 GradeII/IIIseptal
deviation
1(5.5%) 4(40%) 0.04a
Inferiornasalturbinate hypertrophy
7(38.9%) 7(70%) 0.12
Nasalalteration 7(38.9) 8(80%) 0.04a
MMI,modifiedMallampatiindex;p,p-value(chi-squaredtest).
a Statisticallysignificantvalue.
anatomical UA or craniofacial alterations although some
believethatUAalterationsasaresultofMADusecouldresult
insomedegreeofopen-mouthbreathingatnightthatcould
leadtodifficulty in maintaininglip occlusionduringsleep
andcausethepatienttoremoveit,decreasing thedevice
useandadherence,Todate,therehavebeennostudiesin
theliteraturethatmadeasystematicassessmentofUAsand
correlatedthesedatawithMADtreatmentadherence.
Adherenceto MADhas been assessed in other studies,
whichhaveshownthatadherencedoes notdependon
iso-lated factors, but ona number of them, making patients
successful or unsuccessful users of MAD. Marklund et al.
found that24%oftheir patientsstoppedusingMADinthe
firstyearof treatment,andtherewasnoassociationwith
diseaseseverity,age,gender,nasalobstruction,orsmoking
habits.14
Table7 LogisticregressionoffactorsassociatedwithsuccessfultreatmentwithMAD.
B p Exp(B)−OR 95%CIforExp(B)
Minimum Maximum
Age −0.298 0.02 0.74 0.58 0.95
NC −0.730 0.05 0.48 0.23 1.00
AHIpre −0.285 0.05 0.75 0.57 1.00
Almeida et al. affirmed that adherence can be vari-able (ranging from 4% to 82% in studies), depending on thetypeofdeviceemployed,diseaseseverity,andpossibly patientmanagement.13Accordingtotheseauthors,themost
common cause for treatment discontinuationwas patient
discomfort.Thesamestudystatedthatmostexisting
stud-iesassessadherencesubjectively,andthatonlyoneusedan
adherencemonitor,whichindicatedameantimeofuseof
6.8hpernight.15
Adherencewasevaluatedbasedonthequantificationof
the time of MAD use, according to information found in
patients’diaries.Althoughtheonlyavailabledatawasthat
providedbythepatient’sownaccount,whocouldomitor
altertheinformation,thiswayofobtaininginformationwas
theclosesttoquantitativedataconcerningadherence.
MAD therapy success was demonstrated withthe data
obtainedinthisstudyintheentiregroupandafteranalysis
ofadherenceandsuccessgroups,astherewasasignificant
reductioninAHI,arousalindexperhourofsleep,
percent-ageoftimewithoxyhemoglobinsaturation<90%,andtheESS
score.Thesedataareconsistentwiththeliterature,which
showsseveralstudieshighlightingthesefindingsinpatients
withmildtomoderateOSAS.2,13
Thesuccessratewas64.3%accordingtothecriteriawe
used,a50%reductioninbaselineAHIassociatedwithAHI<10
events/hwiththeimplementedtreatment.However,even
inthegroupconsideredunsuccessful,therewasadecrease
in ESSscore, AHI, andarousal index,aswell asimproved
oxyhemoglobinsaturation.Usingthesamecriteria,a
refer-encewasfoundintheliteratureinwhichthesuccessrate
was46%.16
Other authors have also demonstrated similar rates
according to the same criteria.17,18 We believe the wide
range of criteria used in the literature to characterize
MAD treatment success is a major limiting factor for the
comparisonoffurther studieswithwhathasalreadybeen
published.Currently,thereisatendencytoconsiderathird
group, that of patients with complete response to
treat-ment, characterized bya reduction in AHI <5 events/h.19
In our view this should be done cautiously, since
accord-ing to current diagnostic criteria for OSAS, an individual
is not considered as having this syndrome if he does not
show symptoms of snoring, excessive daytime sleepiness,
and witnessed apnea, even if the AHI is between 5 and
15events/h.7
Anotherstatisticallysignificant findingwastheyounger
age inthe group withsuccessfultreatment, confirmedby
logisticregressionasoneof thepredictorsforthesuccess
ofthe MAD.Thiswasalsoobservedby Almeidaetal.and
Dal-Fabbroetal.9,13
Dataregardingtreatmentsuccesspredictorsisaddressed
in the literature. Otsuka et al. observed that success is
lowerinpatients withweightgainand greater
anteropos-terior upper airwaydiameter.20 It has also been reported
that younger patients withpositional OSAS (supine),with
lower baselineAHI, and withsmaller neck circumference
have a higherchance ofsuccess.13,21 Marklund etal. also
reported that a successful outcome with positional OSAS
is more common in men, whereas the association with
mild apnea is more prevalent in women.14 The logistic
regressionobservedin thisstudyshowsthat reducedneck
circumferenceandlowerbasalAHI,inadditiontoyounger
age, can also be considered successful MAD treatment
predictors.
Patients were considered as having pharyngeal
alter-ations when they had three or more of the assessed
alterations.Thiswasbasedonthestudy byZonatoetal.,
whichshowedastatisticallysignificantassociationbetween
AHI and the presence of three or more of these same
alterations.3 No statistical correlation was observed with
respectto treatment success when comparing individuals
whohadthesealterationswiththosewhodidnothavethem.
Therearenostudiesintheliteraturethathaveperformed
thistypeofcorrelation.
InthestudybyMarklundetal.,theauthorsintroduced
newevidenceinrelationtothemechanismofactionofMAD;
accordingtothem,nasalpatencycanbepartofthis
mech-anism,althoughtheystatedthatmorestudiesarerequired
onthesubject. Also inthe same study,a correlation was
observedbetweentreatmentfailureandnasalobstruction,
and this was more evident in women. Nasal obstruction
assessmentwasperformedsubjectivelyinthatstudy.14
Onlyonestudyassessedtheinfluenceofnasalresistance
onthetreatmentofOSASwithMAD,in38patientsselected
for this treatment modality. Using rhinomanometry, Zeng
etal. showedthat patients considered as non-responders
hadhighernasalresistanceinthesittingpositionthanthe
responders,whichwasnotobservedwhenthesame
analy-siswasperformedinthesupineposition.The authorsalso
observedan increaseinnasalresistanceinnon-responding
patientswhentheywereundertheinfluenceofMAD.6
In spite of the limitations of the present study due
to the limited number of patients and the subjectivity
of otorhinolaryngology physical examination, a significant
association was observed between nasal alterations and
treatment failure. These data confirm assumptions
pre-viously raised by other authors. It is known that nasal
permeabilityincreasesduring mandibular advancementin
healthypatients,andthisisoneofthedesiredmechanisms
ofactionwiththisdevice’suse.22Anyanatomicalalterations
in this pathway (septal deviation, turbinate hypertrophy,
nasalpolyps)mayinterferewiththesuccessoftheapplied
therapy.23
Nasalobstructioncanresultininadequatelipocclusion
duringsleep.Mouthbreathingprevents ahorizontal force
frombeingappliedtothe jaw,an essential factorfor the
applicability of mandibular advancement, that limits the
optimumperformanceofMAD.24
Webelievethatnasalobstructionmayleadtoanincrease
intheforce performedduringinspiration,whichpromotes
upper airway collapse and, consequently, decreased
effi-ciencyof MADinthesepatients.This hypothesis hasbeen
raisedbyZengetal.,andthefindingsobservedinthisstudy
furthersupportit.6Thus,webelievethatanevaluationof
UAs,especiallyofnasalobstructivefactors,shouldbe
per-formedwithcautionduringtheinitialevaluationofpatients
undergoingtreatmentforOSASwithMAD,aspossible
treat-mentsofnasalalterations,suchasthoseproposedforCPAP,
maybeadjuvantsforthesuccessfuluseofMAD.25
Conflicts
of
interest
References
1.KushidaCA,MorgenthalerTI,LittnerMR,AlessiCA,Bailey D, Coleman Jr,et al. Practiceparametersfor thetreatmentof snoring andobstructivesleep apneawithoralappliances:an updatefor2005.Sleep.2006;29:240---3.
2.Saletu A,Gritsch F,Mailath-PokornyG, GruberG, AndererP, SaletuB.Objectiveassessmentandtherapeuticefficacyofan improvedmandibularadvancementdeviceforsnoringandsleep apneasyndromeswithpolysomnography.WienKlinWochenschr. 2002;114:807---15.
3.ZonatoAI,BittencourtLRA,MartinhoFL,SantosJFJr,Gregório LC,TufikS.Associationofsystematicheadandneckphysical examinationwithseverityofobstructivesleepapnea---hypopnea syndrome.Laryngoscope.2003;113:973---80.
4.SeriesF,StPierreS,CarrierG.Effectsofsurgicalcorrectionof nasalobstructioninthetreatmentofobstructivesleepapnea. AmRevRespirDis.1992;146:1261---5.
5.FriedmanM,TanyeriH,LimJW,LandsbergR,VaidyanathanK, CaldarelliD.Effectofimprovednasalbreathingonobstructive sleepapnea.OtolaryngolHeadNeckSurg.2000;122:71---4.
6.ZengB,NgAT,QianJ,PetoczP,DarendelilerMA,CistulliPA. Influenceofnasalresistanceonoralappliancetreatment out-comeinobstructivesleepapnea.Sleep.2008;31:543---7.
7.AASM---AmericanAcademyofSleepMedicine.Theinternational classificationofsleepdisorders,2nded.:diagnosticandcoding manual.Westchester,IL:AmericanAcademyofSleepMedicine; 2005.
8.JohnsMW.Anewmethodformeasuringdaytimesleepiness:the EpworthSleepinessScale.Sleep.1991;14:540---5.
9.Dal-Fabbro C, Chaves Junior CM, Bittencourt LRA, Tufik S. Avaliac¸ãoclínicaepolissonográficadoaparelhoBRDno trata-mento da síndrome da apneia obstrutiva do sono. Dental PressJOrthod.2010;15:107---17.Availablefrom:http://www. scielo.br/pdf/dpjo/v15n1/13.pdf[cited16.05.11].
10.MartinhoFL,TangerinaRP,MouraSM,GregórioLC,TufikS, Bit-tencourtLR.Systematicheadandneckphysicalexaminationas apredictorofobstructivesleepapneainclassIIIobesepatients. BrazJMedBiolRes.2008;41:1093---7.
11.RechtschataffenA,KalesA,editors.Amanualofstandardized terminology,techniquesandscoringsystemforsleepsofhuman subjects.LosAngeles,CA:UCLABrainInformationService/Brain ResearchInstitute;1968.
12.Iber C, Ancoli-Israel S, Cheeson A, Quan SF, for the Ameri-canAcademyofSleepMedicine.TheAASMmanualforscoring of sleepassociated events: rules, terminology and technical
specifications. Westchester, IL: American Academy of Sleep Medicine;2007.
13.AlmeidaFR,LoweAA.Principlesoforalappliancetherapyfor themanagement of snoring and sleep disordered breathing. OralMaxillofacSurgClinNorthAm.2009;21:413---20.
14.MarklundM,StenlundH,FranklinKA.Mandibularadvancement devicesin630menandwomenwithobstructive sleepapnea andsnoring:tolerabilityandpredictorsoftreatmentsuccess. Chest.2004;125:1270---8.
15.LoweAA,SjöholmTT,RyanCF,FleethamJA,FergusonKA, Rem-mersJE.Sleep.2000;23:172---8.
16.VecchieriniMF, LégerD, LaabanJP, PuttermanG, Figueredo M,LevyJ,etal.Efficacyand adherenceofmandibular repo-sitioningdeviceinobstructivesleepapneasyndromeundera patient-drivenprotocolofcare.SleepMed.2008;9:762---9.
17.VandervekenOM,BoudewynsAN,BraemMJ,OkkerseW, Ver-braecken JA, Willemen M, et al. Pilot study of a novel mandibularadvancementdeviceforthecontrolofsnoring.Acta Otolaryngol.2004;124:628---33.
18.Mohsenin N,Mostofi MT, Mohsenin V.The role oforal appli-ancesintreating obstructivesleep apnea.JAmDentAssoc. 2003;134:442---9.
19.FergusonKA,CartwrightR,RogersR,Schmidt-NowaraW.Oral appliancesforsnoringandobstructivesleepapnea:areview. Sleep.2006;29:244---62.
20.Otsuka R, Almeida FR, Lowe AA, Ryan F. A comparison of respondersandnonresponderstooralappliancetherapyforthe treatmentofobstructivesleepapnea.AmJOrthodDentofacial Orthop.2006;129:222---9.
21.Fergunson KA. The role of oral appliance therapy in the treatment of obstructive sleep apnea. Clin Chest Med. 2003;24:355---64.
22.HiyamaS,OnoT,IshiwataY,KurodaT. Effectsofmandibular positionand bodyposture onnasalpatencyinnormal awake subjects.AngleOrthod.2002;72:547---53.
23.IsonoS,TanakaA,NishinoT.Lateralpositiondecreases collapsi-bilityofthepassivepharynxinpatientswithobstructivesleep apnea.Anesthesiology.2002;97:780---5.
24.MarklundM.Predictorsoflong-termorthodontic sideeffects frommandibularadvancementdevicesinpatientswithsnoring andobstructivesleepapnea.AmJOrthodDentofacialOrthop. 2006;129:214---21.