w w w . r e u m a t o l o g i a . c o m . b r
REVISTA
BRASILEIRA
DE
REUMATOLOGIA
Original
article
Sleep
quality
in
patients
with
ankylosing
spondylitis
Elif
Aydin
a,∗,
Kevser
Bayraktar
a,
Yasemin
Turan
a,
Imran
Omurlu
b,
Engin
Tastaban
a,
Omer
Faruk
Sendur
aaDepartmentofPhysicalTherapyandRehabilitation,SchoolofMedicine,AdnanMenderesÜniversitesi,Aydin,Turkey bDepartmentofBiostatistics,SchoolofMedicine,AdnanMenderesÜniversitesi,Aydin,Turkey
a
r
t
i
c
l
e
i
n
f
o
Articlehistory:
Received20January2014 Accepted8December2014 Availableonline16March2015
Keywords:
Ankylosingspondylitis Diseaseactivity
PittsburghSleepQualityIndex Sleepquality
a
b
s
t
r
a
c
t
Introduction:Ankylosingspondylitis(AS)isachronic,inflammatoryrheumaticdisease char-acterizedbytheinflammationofthepelvisandspinethatresultsinarestrictioninthe mobilityofthespine.Duetothealteredpostureandnocturnalinflammatorypain,sleep disturbancesarelikelytooccurinpatientswithAS.
Objective:This cross-sectionalstudy aimed atdetermining thedifferences betweenthe patientswithASandhealthycontrolsinsleepquality,aswellasassessingtherelationship betweenthesleepqualityanddiseaseactivity.
Method:Inordertoassesssleepquality,fifty-fivepatientswithAS(40men,15women;mean age,43±1years)whofulfilledthemodifiedNewYorkcriteriaandfifty-fivecomparable controls(40men,15women;meanage,42±9years)completedthePittsburghSleep Qual-ityIndex(PSQI)questionnaire.ThediseaseactivitywasassessedbytheBathAnkylosing SpondylitisDiseaseActivityIndex(BASDAI).
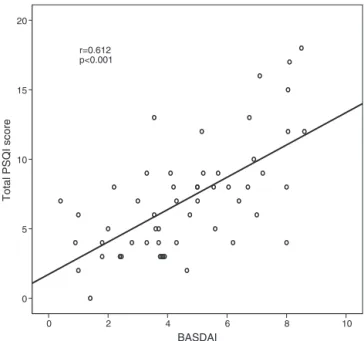
Results:Ankylosingspondylitiswasassociatedwithasignificantlyimpairedsleepquality accordingtothetotalPSQIscores(p=0.001).Significantdifferenceswerefoundbetween thepatientswithASandhealthycontrolsinPSQIdomains,including“subjectivesleep quality”(p=0.010),“sleepduration”(p=0.011),“habitualsleepefficiency”(p=0.034),“sleep disturbances”(p=0.003)and“daytimedysfunction”(p=0.009)butnotin“sleeplatency”,“use ofsleepmedication”.TherewasasignificantpositivecorrelationbetweentheBASDAIand PSQIscores(r=0.612,p=0.001).
Conclusion:Inthecurrentstudy,wefoundthatthesleepdisturbancesweresignificantly higherinpatientswithASincomparisontocontrols.Patientswithactivediseasehadworse sleepquality.Inaddition,diseaseactivitywascorrelatedwiththescoresofmostofthePSQI subscales.SleepqualityassessmentshouldbeatoolforevaluatingpatientswithAS.
©2015ElsevierEditoraLtda.Allrightsreserved.
∗ Correspondingauthor.
E-mail:drebulak@yahoo.com(E.Aydin).
http://dx.doi.org/10.1016/j.rbre.2014.12.007
Qualidade
do
sono
em
pacientes
com
espondilite
anquilosante
Palavras-chave:
Espondiliteanquilosante Atividadedadoenc¸a
ÍndicedeQualidadedoSonode Pittsburgh
Qualidadedosono
r
e
s
u
m
o
Introduc¸ão: Aespondiliteanquilosante(EA)éumadoenc¸areumáticainflamatóriacrônica caracterizadapelainflamac¸ãodapelveedacolunavertebral,queresultaemumarestric¸ão namobilidadedacolunavertebral.Emdecorrênciadaposturaalteradaedadorinflamatória noturna,osdistúrbiosdosonosãopassíveisdeocorrerempacientescomEA.
Objetivo: Determinarasdiferenc¸asentreospacientescomEAecontrolessaudáveisna qualidadedosono,bemcomoavaliararelac¸ãoentreaqualidadedosonoeaatividadeda doenc¸a.
Método: Paraavaliaraqualidadedosono,55pacientescomEA(40homens,15mulheres, idade média43±1 anos)quepreencheram oscritérios modificadosde NovaYorke55 controlescomparáveis(40homens,15mulheres,idademédia42±9anos)preencheram oquestionárioÍndicedeQualidadedoSonodePittsburgh(PSQI).Aatividadedadoenc¸afoi avaliadapeloBathAnkylosingSpondylitisDiseaseActivityIndex(BASDAI).
Resultados:Aespondiliteanquilosantesecorrelacionousignificativamentecomaqualidade desonoprejudicadadeacordocomosescorestotaisdoPSQI(p=0,001).Foramencontradas diferenc¸assignificativasentreospacientescomEAecontrolessaudáveisnosdomínios doPSQI,incluindo“qualidadesubjetivadosono”(p=0,010),“durac¸ãodosono”(p=0,011), “eficiênciadosonohabitual”(p=0,034),“distúrbiosdosono”(p=0,003)e“disfunc¸ãodiurna” (p=0,009),masnãona“latênciadosono”eno“usodemedicac¸ãoparadormir”.Houveuma correlac¸ãopositivaentreaspontuac¸õesdoBASDAIedoPSQI(r=0,612,p=0,001).
Conclusão: Verificou-sequeosdistúrbiosdosonoforamsignificativamentemaioresem pacientescomEAemcomparac¸ãocomoscontroles.Ospacientescomdoenc¸aativa apre-sentarampiorqualidadedesono.Alémdisso,aatividadedadoenc¸aestevecorrelacionada comapontuac¸ãodamaiorpartedassubescalasdoPSQI.Ainvestigac¸ãodaqualidadedo sonodeveserumaferramentausadanaavaliac¸ãodepacientescomEA.
©2015ElsevierEditoraLtda.Todososdireitosreservados.
Introduction
Ankylosing spondylitis (AS) is a chronic, inflammatory rheumaticdiseasecharacterizedbytheinflammationofthe pelvisandspine, thatresultsin arestrictioninthe mobil-ity of the spine. The prevalence of sleep disorders in AS patientsvaries in arange of54% to 64%,according tothe recentarticles.1–3ASpatientsreportproblemswiththeirsleep
includingdifficultyininitiatingsleep,nighttimepain, morn-ingstiffnessandpoorsleepquality.4Consequently,sleeping
problem has a negative impact on daily life by increas-ingfatigue,painandimpairingpsychologicalhealthonthe affectedpatients.2,5,6
Alteredsleepqualityseemstobemulti-factorialinpatients withAS.Pro-inflammatorycytokines,suchasTNF-␣ andIL-1,
areknowntointerferewiththephysiologicalsleeppattern.7–9
Furthermore,inflammatorypainwhichisthecharacteristic ofthedisease,istypicallyworseatnighttimeandaffectsthe qualityofsleep.Inaddition,spinaldeformitiesthatemerge withthe progressionofthe diseaseinterferewithfinding a comfortablesleepposition.Anotherpossibleexplanationfor sleepdisturbancesmightbeincreasedpain,depressionand fatiqueinpatientswithAS.1,10Thesearecommoncomplaints
thatcaninfluencesleepandviceversa.Restrictedrespiratory functionsarealsocommoninASandmighthaveanadditional negativeimpactonthesleepquality.11
Therehasbeenanincreasingunderstandingofthe impor-tance of sleep disturbances in patients with rheumatic diseases.1,12–15 As for AS, more than half of the patients
reportsleepdisturbances.Fromthe pointofpatients’ qual-ity of life, it is necessary to understand the disrupted components of sleep and their relationship with disease flares.
In addition, sleep problems were suggested to be of higherpriorityfortheimprovementofthepatientswithAS than the patients with other rheumatoid diseases.16
How-ever, there is not any specific questionnaire being used as an assessment tool. Understanding the affected com-ponents of sleep in AS would help us to develop new instruments.
Thereareafewdocumenteddataaboutsleepingproblems inAS.Thesedataaremostlyfromtheprevalencestudiesin whichthesleepqualityassessmentwasnotaprimary end-point. Moreover,thereisalackofevidenceconcerningany differencebetweenASpatientsandhealthypeopleinterms ofsleepquality.
Methods
Thisstudyprotocolwasinacross-sectionaldesign.Fifty-five patients,whomettheModifiedNewYorkCriteriaforASand fifty-fivehealthysubjectswereincludedinthestudy. Exclu-sioncriterionwasanyco-existingdiseaseormedicationthat mayinterferewithsleep.Demographicdata,diseaseduration, treatmentregimens,smokingstatusandexercisehabitwere documentedforeachpatient.Thepresenceofspinalkyphosis onvisualinspectionandserumC-reactiveprotein(CRP)levels werealsorecorded.
Sleepdisturbance
All subjects completed the Pittsburgh Sleep Quality Index (PSQI)questionnairefortheassessmentofsleepquality.PSQI isaself-reportquestionnairethatevaluatessleepqualityover onemonth.17Itconsistsofnineteenquestionswhichfinally
generatesevencomponentscores:“subjectivesleepquality”, “sleeplatency”,“sleepduration”,“habitualsleepefficiency”, “sleepdisturbances”,“useofsleepmedication”and“daytime dysfunction”.Thesenineteenitems areusedforscoring. A totalscoreabove5isassociatedwithapoorsleepquality.In variousdiseases,thePSQIhasbeenusedasanassessment tooltodetectsleepdisturbances.18
Diseaseactivity
Thelevelofdiseaseactivitywasdeterminedineachpatient usingtheBathAnkylosingSpondylitisDiseaseActivityIndex (BASDAI).BASDAIisaself-ratedquestionnairethatconsistsof 6questions(Q)pertainingtothefivemajorsymptomsofAS: fatigue(Q1);spinalpain(Q2);jointpain/swelling(Q3); enthesi-tis(Q4);thedurationofmorningstiffness(Q5)andtheseverity ofmorningstiffness(Q5).19,20
Functionalstatus
Bath Ankylosing Spondylitis Functional Index (BASFI) was used to determine functional status. The BASFI is a self-administeredinventoryconsistingof10questions.Thefirst8 questionsassessthefunctionallimitationsrelatedto anatom-icallimitationsandthelast2questionsanalyzethepatients’ abilitytoperformdailytasks.21,22
Statisticalanalysis
TheKolmogorov–Smirnovtest wasused toassess the nor-mality of numeric variables. The independent sample t
test was used to compare normally distributed numeri-cal variables between two groups and the results were expressed as mean±standard deviation. The comparison of the scores and numerical variables that were non-normallydistributed betweentwogroupswas madebythe Mann–Whitney U-test and the results were expressed as median(25–75percentiles).Thechi-squaretestwasusedfor nominalvariables.TheSpearmantestwasusedfor correla-tionanalysis.Valuesofp<0.05wereconsideredstatistically significant.
Table1–Demographiccharacteristicsofpatientswith ankylosingspondylitis.
n(%)
Diseaseduration(years) 15±9.8
Familyhistory 10(18.9%)
Sleepingpartner 43(81.1%)
Regularexercisehabit 14(26.4%)
Smokinghabit 16(30.2%)
Medication
None 5(9.3%)
NSA˙IDs 16(29.6%)
DMARDs 22(40.7%)
TNF-␣ blokers 11(20.4%)
NSA˙ID, non-steroidal anti-inflammatory drug; DMARD, disease modifyingdrug;TNF-␣,tumornecrosisfactor-␣.
Results
Thebasiccharacteristicsofpatientswhoenrolledinthestudy are showninTable 1. Therewas notanysignificant differ-ence betweenthepatient andcontrolgroups(43±10 years vs42±9years,p=0.604)inage.Therewere40maleand15 femaleparticipantsineachgroup(p=1.000).
Ankylosing spondylitis was associated with a signifi-cantly impaired sleep quality according to the total PSQI scores(p=0.001).Thereweresignificantdifferencesbetween the patients with AS and healthy controls in “subjective sleep quality” (p=0.010),“sleepduration” (p=0.011), “habit-ualsleepefficiency”(p=0.034),“sleepdisturbances”(p=0.003) and “daytime dysfunction” (p=0.009) subscale scores but notinthe“sleeplatency”,“useofsleepmedication”scores (Table2).Significantpositivecorrelationswerefoundbetween BASDAI scoresand the “subjective sleep quality” (r=0.475,
p<0.001), “sleep latency” (r=0.419, p=0.002), “sleep dura-tion”(r=0.354,p=0.009),“habitualsleepefficiency”(r=0.444,
p=0.001),“sleepdisturbances”(r=0.426, p=0.001),“daytime dysfunction” (r=0.445, p=0.001) and the total PSQI scores (r=0.612,p<0.001)ofASpatients(Fig.1).Inaddition,BASDAI scores thatsuggestedactivedisease (≥4)were significantly associated with higher PSQI scores (p<0.001). Themedian PSQIscorewas4(3–6)inpatientswithinactivediseaseand8 (6.8–12)inpatientswithactivedisease.Thedetailedanalysis ofeach BASDAI question revealed thatall questions corre-lated with PSQI scores (r=0.453, p=0.001 for Q1; r=0.516,
p<0.001forQ2;r=0.431,p=0.001forQ3;r=0.378,p=0.005for Q4;r=0.457,p=0.001forQ5andr=0.442,p=0.001forQ6).In addition, serumCRPlevelsofASpatients(n=43)correlated withthesleepduration(r=0.367,p=0.014)andtotalPittsburgh scores(r=0.333,p=0.029).
There wasa significantcorrelation betweenthe levelof fatigue measured using the first item of BASDAI and the “subjectivesleepquality”(r=0.275,p=0.044),“sleepduration” (r=0.404, p=0.002), “sleepdisturbances”(r=0.276,p=0.043), “daytimedysfunction”(r=0.400,p=0.003),andtotalPittsburgh scores(r=0.453,p=0.001).
Table2–ComparisonoftwogroupsinregardsofPittsbughSleepQualityIndex(PSQI)scores.
Ankylosing spondylitis(n=55)
Control (n=55)
p
Age(years) 43±10 42±9 0.604
Gender(male/female) 40/15 40/15 1.000
SubjectiveSleepQuality 1(1–2)a 1(0–1)a 0.010
SleepLatency 1(0–2)a 1(0–2)a 0.181
SleepDuration 1(0–1)a 0(0–1)a 0.011
HabitualSleepEfficiency 0(0–2)a 0(0–0)a 0.034
SleepDisturbances 2(1–2)a 1(1–2)a 0.003
UseofSleepMedication 0(0–0)a 0(0–0)a 0.096
DaytimeDysfunction 1(0–2)a 0(0–1)a 0.009
TotalPSQIscore 7(4–9)a 5(2–7)a 0.001
pvaluesshowthedifferencebetweenankylosingspondylitisandcontrolgroups. a Dataarepresentedasmedian(25–75percentiles).
p=0.017),“sleepdisturbances”(r=0.494,p=0.001),“daytime dysfunction”(r=0.376,p=0.012),and totalPittsburgh scores (r=0.483,p=0.001).
Therewasnostatisticallysignificantcorrelationbetween thesleepqualityandage,gender,diseaseduration,exercise habit,smoking behaviorof thepatients or spinalkyphosis (p>0.05).Therewasnosignificantrelationshipbetweenthe drugsusedandsleepdisturbances.
Discussion
Inthiscross-sectionalcontrolledstudy,ourfindingssuggest thatpatientswithASweresignificantlymoreaffectedbysleep disturbancesthanthehealthyindividuals.Inaddition,there wasasignificantrelationshipbetweenthesleepproblemand diseaseactivityandinflammatorystate.ThetotalPSQIscores increasedwithincreasingscoresofBASDAIandserum CRP levelsinpatientswithAS.
BASDAI
10 8
6 4
2 0
Total PSQI score
20
15
10
5
0
r=0.612 p<0.001
Fig.1–CorrelationoftotalBASDAIscoreswithtotalPSQI scores.
Thefirst question addressedin this study was whether thepatientswithAShadaworsesleepqualitythanhealthy people. In ourstudy,the medianvalue ofPSQIscores was greater in ASpatients than that ofthe healthy subjects (7 and5,respectively).Sinceatotalscoreabove5isassociated withpoorsleepquality,weconcludedthatpatientswithAS haspoorsleepquality.Similartoourstudy,apreviousstudy involving62ASpatientsalsoindicatedapoorsleepqualityin ASpatients,sincethemeanscoreofPSQIwasfoundas5.8.3
Inanotherstudyinvolving11subjectswithASand11healthy volunteers,thesleeppatternwasfoundworseinASpatients.6
Inourstudy,theincidenceofpoorsleepqualityamongthe ASpatientswasfoundas58.1%.Theincidenceofalteredsleep pattern amongthe individuals with AS,has been reported as64.5%byHakkouet al.,54%byWardetal.and54.8%by Günaydınetal.1–3Similarly,DaCostaetal.foundtheincidence
ofsleepproblemsas69%inpatientswithspondyloarthritis.13
Consistentlywiththecurrentliterature,ourresults empha-sizethatapoorsleepqualitymightbeexpectedinmorethan halfofthepatientswithAS.
Thesecondquestion addressedinthisstudy waswhich componentsofsleepqualityhavebeenaffectedinAS.PSQI assesses seven components of sleep. In patients with AS, five of these components were found to be significantly worsecomparedtonormalindividuals.The“Subjectivesleep quality”, “sleep duration”, “sleeps disturbances”, “habitual sleepefficiency”and“daytimedysfunction”weresignificantly impaired. In addition, all PSQI components, except “sleep medication”werefoundtobecorrelatedwithdisease activ-ity.Possibleexplanationsforthereducedsleepdurationand increasedsleepdisturbancesmightbethenocturnalincreases intheinflammation,painand stiffness.Inarecentsurvey, peoplewithrheumaticdiseasesreportedasleepdurationless than 6hper night.23 Althoughthereare considerable
indi-vidualdifferencesinsleepduration,healthyadultssleepan averageof7–8hperday.24Insufficientsleep,nighttime
awak-eningsandlossofsleepefficiencyenhancedepression,fatigue andlifesatisfactioninthesepatients.2,5,10 Inalongitudinal
surveyincluding 175subjects withAS, 54%ofthe patients definedpoorsleepqualityasthemostimportantqualityof life concern.2 In another surveyinvolving 295 AS patients,
thelightofforegoingdata,daytimedysfunctiondetectedby ourstudyshouldnotbesurprising.AsthesymptomsofAS usuallyappearinearlyadulthood,daytimedysfunctiondue tosleepproblemsmayhavesocioeconomicconsequencesfor individualpatientsandforsociety.
Inrespectofsleeplatency,therewasnosignificant differ-encebetweenthegroups,whereasthediseaseactivityscores correlatedwithsleeplatency.Accordingtoapreviousstudy, paininASwasfoundtobecorrelatedwiththedifficultyin gettingtosleep.6Inviewofourfindings,thepreservedsleep
latencyinASpatients mightbeexplainedbythecharacter ofinflammatorypainthatworsenaftermiddleofthenight. Accordingtoourdata,weconcludedthatthemainproblem wasduetomaintainingsleep,notinitiatingit.
Thirdquestionaddressedinthisstudywaswhetherthere wasarelationshipbetweenthedisease-specificvariablesand sleepquality.Itisaclinicallyrelevantquestionbecausethe propermanagementofthediseasecouldimprovesleep qual-ity and health-related quality oflife. We found a positive correlation between the disease activity and sleep distur-bances. According to their BASDAI scores and CRP levels, thepatientswithactivediseasehadworsesleepquality.In detailedanalysis,eachquestionofBASDAIreflectingfatique, spinalpain,jointpain/swelling,enthesitis,thedurationand severityofmorning stiffnessrevealed apositivecorrelation withthePSQIscores.
Although pain and stiffness are the major symptoms of the disease, more than half of the AS patients report fatigue.5,25Therelationshipbetweenfatigueandsleep
qual-ityinASpatientswasreportedpreviously.3,26,27Similarly,in
thepresentstudy,patientsreportinghighlevelsoffatiguehad higherPSQIscoresaswell.Improvingsleepqualitymayhelp todecreasefatigueandpain,whichinturnmayimprovethe functionalityandoverallqualityoflife.Ourresultsindicated thatthepatientswithhigherBASFIscoreshadworsesleep qualityaccordingtoPSQI.Sleepwasassessedbythefourth itemoftheHamiltonAnxietyRatingScaleinapreviousstudy andsimilarlytoourresults,itwasreportedthatthepain inten-sity,diseaseactivityandfunctionalstatushadimpactsonthe sleepquality.1
Theresultsofthisstudyalsosuggestthattheevaluation of the sleep quality should be a part of outcome assess-mentinAS.Inastudy of2138subjectswithinflammatory arthropathies, patients were asked to rank health prob-lems,includingpain,morningstiffness,physicalfunctioning, fatigue,sleep,socialfunctionandemotionalwell-being.The rateofthepatientswhodescribed priorityforthe improve-ment in sleep problems was significantly higher among ASpatientsincomparisontotheother rheumaticdisorder groups.16Thesedataemphasizetheimportanceofthe
assess-mentofsleepproblemsinAS.AnkylosingSpondylitisQuality ofLife (ASQOL)questionnairehasageneralquestionabout sleep,butthisisayes/noquestionandinsufficientto under-standtherealimpact.28Bytheway,wecanconcludethatthe
instrumentsthatassesstheimpactofASonsleepqualityand itsinfluencetodailylifearegenerallylacking.
Certainly,ourstudyhassomelimitations.Thesamplesize wassmallandthestudy designwascross-sectional. There-fore,theresultsofthisstudyneedaconfirmationbyastudy inalongitudinalobservationaldesignwithalargersample
size. Inaddition,wedid notassess the anatomical impair-mentsobjectively,inordertofindouttheirrelationshipwith sleep quality.Aphysicalexaminationconsistingofthoracic expansionandBathAnkylosingSpondylitisMetrologyIndex, couldgivevaluabledata.29However,inthiscontext,wetried
to define a relationship between spinal kyphosis, disease durationandPSQIscores,buttherewasnosignificant rela-tionship.Moreover,smokingbehaviorwasaskedonlytothe patientgroup.Itwasayes/noquestionwhichwasnot ask-ingtheamountofconsumptionandformeraddiction.Further researchesconcerningtheeffectofsmokinghabitonsleep, shouldbeconducted.Finally,wedidnotuseanytooltoassess neitherthequalityoflifenormentalhealthstatus.
Future studies could be designedto findout how sleep problemsinteractdailylife,suchasqualityoflifeormental healthstatusinpatientswithAS.Evaluationofspinal mobil-ity and radiological changes by means ofBath Ankylosing SpondylitisMetrologyIndexandBathAnkylosingSpondylitis Radiology Index as well as the analysis of real inflamma-torystate,byusingmagneticresonanceimagingshouldbe includedinthesestudies.29,30Longtermstudiesinvestigating
howdifferenttherapyregimensimpactsleepqualityandthe polysomnographystudiescouldprovidevaluabledata.
Conclusion
Inthecurrentstudy,wefoundthatsleepdisturbanceswere significantlyhigherinpatientswithAS.Patientswithactive diseasehadworsesleepquality.Inaddition,diseaseactivity wascorrelatedwithmostofthePSQIsubscalescores.Itseems thatthediseaseactivityhasagreaterimpactonsleepquality thantheanatomicalimpairments.Propermanagementofthe diseasecanimprovesleepqualityandhealthrelatedquality oflife.Furthermore,theassessmentofsleepqualityshouldbe usedroutinelyinpatientswithAS.
Conflicts
of
interest
Theauthorsdeclarenoconflictsofinterest.
r
e
f
e
r
e
n
c
e
s
1.HakkouJ,RostomS,MengatM,AissaouiN,BahiriR, Hajjaj-HassouniN.SleepdisturbanceinMoroccanpatients withankylosingspondylitis:prevalenceandrelationships withdisease-specificvariables,psychologicalstatusand qualityoflife.RheumatolInt.2013;33:285–90.
2.WardMM.Health-relatedqualityoflifeinankylosing spondylitis:asurveyof175patients.ArthritisCareRes. 1999;12:247–55.
3.GünaydinR,GökselKaratepeA,Ces¸meliN,KayaT.Fatiguein patientswithankylosingspondylitis:relationshipswith disease-specificvariables,depression,andsleepdisturbance. ClinRheumatol.2009;28:1045–51.
4.AbadVC,SarinasPS,GuilleminaultC.Sleepand rheumatologicdisorders.SleepMedRev.2008;12:211–28.
6. JamiesonAH,AlfordCA,BirdHA,HindmarchI,WrightV.The effectofsleepandnocturnalmovementonstiffness,pain, andpsychomotorperformanceinankylosingspondylitis.Clin ExpRheumatol.1995;13:73–8.
7. KruegerJM,FangJ,TaishiP,ChenZ,KushikataT,GardiJ. Sleep.AphysiologicroleforIL-1betaandTNF-alpha.AnnNY AcadSci.1998;29:856,148–59.
8. ShohamS,DavenneD,CadyAB,DinarelloCA,KruegerJM. Recombinanttumornecrosisfactorandinterleukin1 enhanceslow-wavesleep.AmJPhysiol.1987;253:142–9.
9. KruegerJM,ObálFJ,FangJ,KubotaT,TaishiP.Theroleof cytokinesinphysiologicalsleepregulation.AnnNYAcadSci. 2001;933:211–21.
10.AissaouiN,RostomS,HakkouJ,BerradaGhziouelK,BahiriR, AbouqalR,etal.Fatigueinpatientswithankylosing spondylitis:prevalenceandrelationshipswith
disease-specificvariables,psychologicalstatus,andsleep disturbance.RheumatolInt.2012;32:2117–24.
11.YamamotoJ,OkamotoY,ShibuyaE,NishimuraM,Kawakami Y.Obstructivesleepapneasyndromeinducedbyossification oftheanteriorlongitudinalligamentwithankylosing spondylitis.NihonKokyukiGakkaiZasshi.2000;38:413–6 [Abstract].
12.ChandrasekharaPK,JayachandranNV,RajasekharL,Thomas J,NarsimuluG.Theprevalenceandassociationsofsleep disturbancesinpatientswithsystemiclupuserythematosus. ModRheumatol.2009;19:407–15.
13.DaCostaD,ZummerM,FitzcharlesMA.Determinantsof sleepproblemsinpatientswithspondyloarthropathy. MusculoskeletalCare.2009;7:143–61.
14.Taylor-GjevreRM,GjevreJA,NairB,SkomroR,LimHJ. Hypersomnolenceandsleepdisordersinarheumaticdisease patientpopulation.JClinRheumatol.2010;16:255–61.
15.IrwinMR,OlmsteadR,CarrilloC,SadeghiN,FitzgeraldJD, RanganathVK,etal.Sleeplossexacerbatesfatigue, depression,andpaininrheumatoidarthritis.Sleep. 2012;35:537–43.
16.HeibergT,LieE,VanderHeijdeD,KvienTK.Sleepproblems areofhigherpriorityforimprovementforpatientswith ankylosingspondylitisthanforpatientswithother inflammatoryarthropathies.AnnRheumDis.2011;70:872–3.
17.BuysseDJ,ReynoldsCF3rd,MonkTH,BermanSR,KupferDJ. ThePittsburghSleepQualityIndex:anewinstrumentfor psychiatricpracticeandresearch.PsychiatryRes. 1989;28:193–213.
18.OmachiTA.Measuresofsleepinrheumatologicdiseases: EpworthSleepinessScale(ESS),FunctionalOutcomeofSleep
Questionnaire(FOSQ),InsomniaSeverityIndex(ISI),and PittsburghSleepQualityIndex(PSQI).ArthritisCareRes (Hoboken).2011;63:287–96.
19.GarrettS,JenkinsonT,KennedyLG,WhitelockH,GaisfordP, CalinA.Anewapproachtodefiningdiseasestatusin ankylosingspondylitis:theBathAnkylosingSpondylitis DiseaseActivityIndex.JRheumatol.1994;21:
2286–91.
20.AkkocY,KaratepeAG,AkarS,KirazliY,AkkocN.ATurkish versionoftheBathAnkylosingSpondylitisDiseaseActivity Index:reliabilityandvalidity.RheumatolInt.2005;25: 280–4.
21.CalinA,GarrettS,WhitelockH,KennedyLG,O’HeaJ,Mallorie P,JenkinsonT.Anewapproachtodefiningfunctionalability inankylosingspondylitis:thedevelopmentoftheBath AnkylosingSpondylitisFunctionalIndex.JRheumatol. 1994;21:2281–5.
22.YanikB,GürselYK,KutlayS,AyS,ElhanAH.Adaptationof theBathAnkylosingSpondylitisFunctionalIndextothe Turkishpopulation,itsreliabilityandvalidity:functional assessmentinAS.ClinRheumatol.2005;24:41–7.
23.StipelmanBA,AugustsonE,McNeelT.Therelationship amongsmoking,sleep,andchronicrheumaticconditions commonlyassociatedwithpaininthenationalhealth interviewsurvey.JBehavMed.2012[Epubaheadofprint].
24.FoleyD,Ancoli-IsraelS,BritzP,WalshJ.Sleepdisturbances andchronicdiseaseinolderadults:resultsofthe2003 NationalSleepFoundationSleepinAmericaSurvey.J PsychosomRes.2004;56:497–502.
25.CalinA,EdmundsL,KennedyLG.Fatigueinankylosing spondylitis–whyisitignored?JRheumatol.1993;20:991–5.
26.MissaouiB,RevelM.Fatigueinankylosingspondylitis.Ann ReadaptMedPhys.2006;49:305–8,389–91.
27.MengshoelAM,FørreO.Painandfatigueinpatientswith rheumaticdisorders.ClinRheumatol.1993;12:515–21.
28.DowardLC1,SpoorenbergA,CookSA,WhalleyD,Helliwell PS,KayLJ.DevelopmentoftheASQoL:aqualityoflife instrumentspecifictoankylosingspondylitis.AnnRheum Dis.2003;62:20–6.
29.JenkinsonTR,MalloriePA,WhitelockHC,KennedyLG,Garrett SL,CalinA.Definingspinalmobilityinankylosingspondylitis (AS).TheBathasMetrologyIndex.JRheumatol.
1994;21:1694–8.