www.revportcardiol.org
Revista
Portuguesa
de
Cardiologia
Portuguese
Journal
of
Cardiology
REVIEW
ARTICLE
A
2018
overview
of
diuretic
resistance
in
heart
failure
Sofia
Isabel
Jardim
a,∗,
Luís
Ramos
dos
Santos
b,
Inês
Araújo
c,d,
Filipa
Marques
c,d,
Patrícia
Branco
e,
Augusta
Gaspar
e,
Cândida
Fonseca
c,daUnidadeFuncionalMedicina1.2,HospitaldeSãoJosé,CentroHospitalardeLisboaCentral,Lisbon,Portugal bServic¸odeMedicinaInterna,HospitalCentraldoFunchal,Funchal,Portugal
cUnidadedeInsuficiênciaCardíaca,Servic¸odeMedicinaIII,HospitalSãoFranciscoXavier,Lisbon,Portugal dNOVAMedicalSchool,FaculdadedeCiênciasMédicas,UniversidadeNovadeLisboa,Lisbon,Portugal eServic¸odeNefrologia,HospitaldeSantaCruz,CentroHospitalardeLisboaOcidental,Lisbon,Portugal
KEYWORDS Heartfailure; Diureticresistance; Loopdiuretic; Sequentialnephron blockade; Ultrafiltration
Abstract Heart failureisadisease with highdirect andindirect costs.Current treatment includesdrugsthatalterdiseaseprogressionanddrugsthattoimprovesymptoms.Loopdiuretics arethecornerstoneofcongestionreliefforacutemanagement,aswellasforchronic stabiliza-tion.Inheartfailurepatients,maximaldiureticresponseisreducedbymanyindividualfactors. Diureticresistanceisdefinedasfailuretoachieveeffectivecongestionreliefdespite appropri-ateorescalatingdiureticdoses.Itscausesincludeimpaireddeliveryofthediuretictoitsluminal siteofaction,neurohormonalactivation,tubularcompensatoryadaptationanddrug interac-tions.Severalstrategiescanbeemployedtoaiddecongestionofpatientswithimpaireddiuretic response.Theseincludesaltrestriction,ahighereffectivesingledoseorhigherdosefrequency ofloopdiuretics,continuousinfusionofdiureticsand/orsequentialnephronblockadethrough asynergisticcombinationoftwoormorediureticsfromdifferentclasses.Ultrafiltrationhas alsobeenfoundtobeanothereffectiveandsafetherapeuticoptionandshouldbeconsidered inpatientswithrefractorydiureticresistance.Overall,thereisalackofhigh-qualityclinical datatoguidethechoiceoftreatmentstrategyandtherapyshouldbetailoredonacase-by-case basis.
©2018SociedadePortuguesadeCardiologia.PublishedbyElsevier Espa˜na,S.L.U.Thisisan openaccessarticleundertheCCBY-NC-NDlicense( http://creativecommons.org/licenses/by-nc-nd/4.0/). PALAVRAS-CHAVE Insuficiência cardíaca; Resistênciaaos diuréticos; Diuréticosdeansa;
Aresistênciaaosdiuréticosnainsuficiênciacardíacarevisitadaem2018
Resumo A insuficiênciacardíaca éumadoenc¸acomcustos diretoseindiretoselevados. A terapêuticaatualincluifármacosquealteramaprogressãodadoenc¸aefármacosquemelhoram asintomatologia.Osdiuréticosdeansaconstituemapedrabasilarnoalíviodacongestãoquer naabordagemagudaquernaestabilizac¸ãocrónica.Nosdoentescominsuficiênciacardíaca,a respostadiuréticamáximaencontra-sediminuídadevidoamúltiplosfatores.Aresistênciaaos
∗Correspondingauthor.
E-mailaddress:sofiaisabeljardim@gmail.com(S.I.Jardim).
https://doi.org/10.1016/j.repc.2018.03.014
0870-2551/©2018SociedadePortuguesadeCardiologia.PublishedbyElsevierEspa˜na,S.L.U.ThisisanopenaccessarticleundertheCC BY-NC-NDlicense(http://creativecommons.org/licenses/by-nc-nd/4.0/).
Bloqueiosequencial donefrónio; Ultrafiltrac¸ão
diuréticosédefinidacomoaausênciadealívioeficazdacongestãoapesardedosesapropriadas oucrescentesdediuréticos.Ascausasderesistênciaaosdiuréticosincluemocompromissoda entregadediuréticonoseulocaldeac¸ão,aativac¸ãoneuro-hormonal,aadaptac¸ão compen-satóriatubulareinterac¸õesmedicamentosas.Podemserimplementadasváriasestratégiaspara diminuiracongestãoemdoentescomrespostadiuréticainsuficiente.Essasestratégiasincluem restric¸ãosalina,aumentodadoseoufrequênciadosdiuréticosdeansa,infusãocontínuade diuréticose/oubloqueiosequencialdonefrónioatravésdacombinac¸ãodedoisoumais diuréti-cosdediferentesclassesecomefeitossinérgicos.Aultrafiltrac¸ãotem-sereveladoumaoutra estratégiaseguraeeficazedeveserconsideradaemdoentescomresistênciaaosdiuréticos refratária.Verifica-seglobalmenteumaescassezdedadosclínicosdeelevadaqualidadepara guiaraescolhadaestratégiaterapêuticapeloqueaabordagemdeveseradequadacasoacaso. ©2018SociedadePortuguesadeCardiologia.PublicadoporElsevierEspa˜na,S.L.U.Este ´eum artigoOpen Accesssobumalicenc¸aCCBY-NC-ND( http://creativecommons.org/licenses/by-nc-nd/4.0/).
Abbreviations
ATOMIC-HF AcuteTreatment withOmecamtiv Mecar-bil to Increase Contractility in Acute Heart Failure
BNP B-typenatriureticpeptide
BLAST-AHF Biasedligand ofthe angiotensinIItype 1 receptorinpatientswithacuteheartfailure CARRESS-HF Cardiorenal Rescue Study in Acute
DecompensatedHeartFailure CKD Chronickidneydisease
CUORE Continuous Ultrafiltration for Congestive HeartFailure
DOSE DiureticOptimizationStrategiesEvaluation DAD-HF II Dopamine in Acute Decompensated Heart
FailureII
RELAX-AHF-2 Efficacy,SafetyandTolerabilityof Sere-laxin When Added to Standard Therapy in AcuteHeartFailure
RELAX-AHF Efficacy and Safety of Relaxin for the TreatmentofAcuteHeartFailure
TRUE-AHF Efficacy and Safety of Ularitide for the Treatment of Acute Decompensated Heart Failure
EVEREST EfficacyofVasopressinAntagonism inHeart FailureOutcomeStudywithTolvaptan EPICA Epidemiologia da Insuficiência Cardiaca e
Aprendizagem HF Heartfailure
NT-proBNP N-terminalpro---BNP
NSAID Nonsteroidalanti-inflammatorydrug
PROTECT Placebo-Controlled Randomized Study of theSelectiveAdenosineA1Receptor Antago-nistRolofyllineforPatientsHospitalizedwith AcuteDecompensatedHeartFailureand Vol-umeOverloadtoAssessTreatmentEffect on CongestionandRenalFunction
REVIVE Randomized Multicenter Evaluationof Intra-venousLevosimendanEfficacy
RAPID-CHF Relief for Acutely Fluid-Overloaded Patients With Decompensated Congestive HeartFailure
ROSE RenalOptimizationStrategiesEvaluation RAA Renin-angiotensin-aldosterone
REWORD-HF Reverse Worsening Renal Function in DecompensatedHeartFailure
UF Ultrafiltration
UNLOAD Ultrafiltration versus Intravenous Diuretics forPatientsHospitalizedforAcute Decompen-satedCongestiveHeartFailure
ULTRADISCO Ultrafiltrationvs.Diureticsin Decompen-satedHeartFailure
Introduction
The incidenceof heartfailure(HF)is 1%amongAmerican patientsover65yearsofage.1,2Portuguesefiguresfromthe
2002EpidemiologiadaInsuficiênciaCardiacae Aprendiza-gem (EPICA) study concluded that the overall prevalence of HF is 4.4%, peaking at 16% in those over 80 years of age.3 It continues to be the primary discharge diagnosis
among elderly American patients.4 Hospitalization for HF
constitutes an ominous sign, with half of patients read-mitted in thesubsequent sixmonths anda mortalityrate of 25-35%atthe endofthe firstyear.4,5 Consequently,HF
is ahighburden diseasewithelevated directandindirect costs.1
Currenttreatmentincludesdrugsthatalterdisease pro-gressionsuchasangiotensinconvertingenzymeinhibitors, angiotensinII receptor blockersor, morerecently, sacubi-tril/valsartan,beta-blockersandmineralocorticoidreceptor antagonists --- in HF withreduced ejection fraction--- and drugsusedtoimprovesymptomssuchasdiuretics,namely loop diuretics.6---8 Loop diuretics are the cornerstone of
congestion relief and are widely used for acute man-agement (up to 90% of patients) as well as for chronic stabilization.2,5,8---10
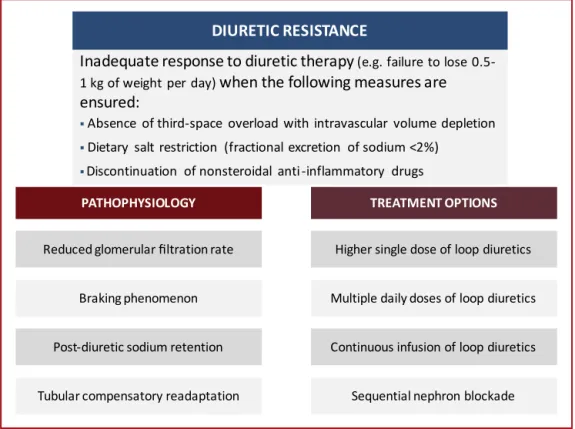
Figure1 Pathophysiology-basedapproachtodiureticresistance.
Despitethefactthatdiureticsthemselvesarenotlinked toincreasedsurvival,6,8diureticefficacyhasbeenshownto
prolongevent-freesurvival,regardlessofglomerular filtra-tionrate.5,11---13
In this review, we discussthe underlying pathophysio-logyof diureticresistance in HFpatients, while providing severalcurrentlyavailableevidence-basedpharmacological andnon-pharmacologicalstrategiestoovercomethis prob-lem(Figure1).Theaimofthisarticleistosummarizethe existingdataandhighlightrecentresearchonthesubject, providinganup-to-dateandpracticalapproachtodiuretic resistance.
Diuretic
resistance
---
defining
the
problem
There is ample variation in the definition of diuretic-resistant patients.13 The general definition refers to the
failuretoachieveeffectivecongestionreliefdespite appro-priateorescalatingdosesofdiuretics.14,15
Someearlyreportsestimatedtheprevalenceofdiuretic resistancetobe20-30%amongHFpatients.16,17However,the
lackofa formaldefinitionmakesitimpossible toproperly assessthenumbers.9,13,15
Recent data link furosemide-equivalent doses of loop diuretics (for intravenous diuretics, 1 mg of bumetanide, 20mgoftorsemideand40mgoffurosemide11)tochanges
inseveralparameterssuchasweightloss,urineoutputor natriuresisasmeanstodiagnosediureticresistance.13These
studiesaresummarizedinTable1.
Depending onthestudy,poordiureticresponsemaybe defined as: a weight change of 0 to 2.7 kgper 40 mgof furosemide (or equivalent)18; a urinary diuretic response
<1400 ml per 40 mg of furosemide (or equivalent)18;
a fractional excretion of sodium at baseline <0.2%19;
a urinary sodium concentration and urinary furosemide concentrationratio(bothobtainedfromspoturinesamples) <2mmol/mg12;and/orlowerchloridelevelsatbaseline(97
to103mEq/l).20 However,thecorrelationbetween
differ-entmetricsremainspoorandthereisnocut-offtoestablish actualdiureticresistance.13Prospectivetrialsareneededto
properlyvalidatethesemetrics.21
Predictorsofdiureticresistance,ontheotherhand,are morefirmlyestablished betweenstudies and include:low systemicbloodpressure,elevatedbloodureanitrogen,HF ofischemic originanddiabetes.5,11,18,22These studiesalso
foundthatdiureticresistance isan independentpredictor ofworsein-hospitaloutcomesfor HF,early post-discharge mortalityandincreasedHFrehospitalization.
Pharmacokinetics
&
pharmacodynamics
of
loop
diuretics
The relationship between loopdiuretic concentrationand natriuresis can be illustrated through an S-shaped dose-responsecurve,14whichmeansthataminimalconcentration
mustbereached atthesiteofactionbeforeanyresponse isnoted.8 Anormaldose-responserelationship canbe
dis-tortedbyavarietyofclinicalconditions.InHFpatients,the curveisshifteddownwardsandtotheright,whichtranslates intoadecreasedmaximaldiureticresponse.8Furthermore,
duringhospitalization,diureticresponseisaffectedbymany individualfactors14including,butnotlimitedto,renal
Table1 Relationshipbetweendiureticefficacyandclinicaloutcomesinheartfailure.
Author(year) Metric Findingsinpatientswithlowdiureticefficacy Testanietal.(2014)11 Netfluidloss Higherall-causemortalityafter5years(Penn
Cohort)/180days(EvaluationStudyofCongestiveHeart FailureandPulmonaryArteryCatheterization
EffectivenessCohort)
Valenteetal.(2014)5 Weightloss Higherheartfailurereadmissionsafter60days
Higherdeath,heartfailureorrenal-related readmissionsafter60days
Higherall-causemortalityafter180days Voorsetal.(2014)22 Weightloss Higherdeath,heartfailureorrenal-related
readmissionsafter60days
Neutraleffectonall-causemortalityafter180days Singhetal.(2014)12 Urinarysodium
Furosemideconcentration
Higherdeath,transplantationorheartfailure readmissionafter5months
terMaatenetal.(2015)18 Weightloss
Urineoutput
Higherdeathorheartfailurereadmissionafter30days Verbruggeetal.(2015)10 Natriuresis Higherdeathorheartfailurereadmissionafter188days
Kumaretal.(2015)19 Fractionalsodiumexcretion Higherall-causemortalityafter30days
TerMaatenetal.(2016)20 Chloridelevels Highermortalitythrough180days
Aronsonetal.(2016)56 Netfluidloss
Urineoutput
Higherall-causemortalityafter6months
AdaptedfromVerbruggeFH,MullensW&TangWH(2016).13
higher dose of diuretics is needed to achieve the same degreeofnatriuresis.8
Pathophysiology
of
diuretic
resistance
Thepathophysiology ofdiuretic resistanceiscomplexand severalcauses maybe involved (Table2).15 Itstems from
multiplefactors,includingreduceddeliveryofthediuretic toitsluminalsiteofaction,neurohormonalactivation, tubu-larcompensatoryadaptationanddruginteractions.15
Reduceddeliveryofthediuretictoitssiteofaction
Reduceddeliveryofthediuretictoitssiteofactionisclosely relatedtoitsdecreasedbioavailability.
In HF patients, increased peripheral and bowel wall edemaleadstoreducedabsorptionofthediuretic,witha moremarkedeffectwhenoralfurosemideisused.21
HF itself as well as concurrent chronic kidney disease (CKD)(urate andothercompetingorganicacids) maylead to decreased glomerular filtration rate, which in turns leadstoimpairedsecretionofdiuretics(namelyfurosemide) by theorganic acid transporter into the proximal tubule. Reducedglomerular filtration rate can, therefore, reduce delivery or reduce active secretion of loop diuretics into their site of action.23 Moreover, CKD has been proposed
asacontributingfactor tothedevelopmentofHFoverall, regardlessofleftventricularejectionfraction.CKDleadsto volumeretention,alteredcalcium---phosphatemetabolism, hyperparathyroidism,vitaminDdeficiency,anemia,andthe accumulationofuremictoxins.24 Renaldysfunctioncaused
byintra-abdominalhypertensionandcardiorenalsyndrome arealsoplausiblemechanismsofdiureticresistancethrough venous congestion.9,25 Intra-abdominal hypertension relief
improves renal perfusion, renal filtration and diuresis. It
is usuallypresent in up to60%of acutely decompensated HFpatients.25 It isvery importanttoemphasize theneed
to detect third-space overload as opposed to intravascu-laroverloadbecauseboththekidneysanddiuretictherapy can only act in vascular overload. Persistent diuretic use in patients who are already suffering from intravascular volume depletion further activates the renin-angiotensin-aldosterone (RAA) axis and makes diuretic resistance dependent onrenal blood flow. Urinary sodium and chlo-ride measurements may indicate when vascular volume has been optimized because they decrease as euvolemia approaches.13 These may serve as more reliable markers
ofdecongestionasopposedtotheclinicalsignsand symp-toms traditionally used to guide decongestive therapy.26
Clinicalsignsandsymptomslack sensitivityandspecificity butdoraisetheneedforfurtherclinicalevaluation. Natri-ureticpeptidesarehelpfulfor diagnosisandprognosisbut lackthepowertoproperlymonitorvolumestatus.26Newer
approaches pointtoquantitativebloodvolumeanalysisas means todifferentiate hypervolemia profiles. Appropriate profilingofvolumeoverload inHF,accordingtoblood vol-ume, has therapeutic implications and may aid patients with diuretic resistance, redirecting them toother forms ofdecongestion.26
Another mechanism of diuretic activity impairment involvesincreasedre-absorptionofsodiumandchloridein theproximaltubule,leadingtodecreaseddeliveryofthese substrates tothe distal areas of the nephron where loop diuretics act. This mechanism causes diuretic resistance through decreased substrate availability to the sodium-potassium-chloridecotransportsystem.13
Albuminlevelsalsocorrelatetodiureticactionbecause they are high affinity albumin-binding molecules (>90%).9
Hypoalbuminemia increases the drug distribution volume andprevents suitablekidney delivery.Onthe other hand,
Table2 Causesofdiureticresistance.
Incorrectdiagnosis
Venousedema Lymphaticedema
Thirdspaceoverloadwithintravascularvolumedepletion
Nonadherencetorecommendedsodiumand/orfluid restriction
Poordiureticdeliverytothenephronlumen
Nonadherence
Dosetoolowortooinfrequent
Poorabsorption(example:edematousgut) Hypoalbuminemiaandnephroticsyndrome Hepaticcirrhosis
Reduceddiureticsecretion
Tubularuptakeofdiureticimpairedbyuremictoxins Decreasedkidneybloodflow
Decreasedfunctionalkidneymass
Insufficientkidneyresponsetodrug
Lowglomerularfiltrationrate
Decreasedeffectiveintravascularvolumedespiteelevated totalextracellularfluidvolume
Activationoftherenin-angiotensin-aldosteroneaxisand renalsympatheticnerves
Increasedsodiumdeliveryandabsorptionindistaltubular segments
Compensatoryretentionofsodiumaftertheeffective periodofthediuretic
Nephronadaptation(hypertrophyandhyperplasiaofdistal tubularcells)
Useofnonsteroidalanti-inflammatorydrugs
AdaptedfromHoornEJ&EllisonDH(2017).36
high levels of albuminuria decrease loop diuretic deliv-ery.Increasedurinealbuminbindstodiuretics,preventing their ligation to the sodium-potassium-chloride receptors andthusimpairingtheiraction.9
Neurohormonalactivation
Neurohormonal activation is strongly related to RAA axis upregulation. Loop diuretics can activate the RAA axis throughavarietyofmechanisms.15Theyinducerenin
secre-tion through the direct blockade of the macula densa sodium-potassium-chloridecotransportsystem,thusleading toincreasedreninandaldosteroneinavolume-independent pathway.8 Furthermore, diuretics induce renal
prostacy-clin production, which increases renin secretion. Finally, diuretics inducevolumecontraction, thusactivating renin secretionthroughvascularstimulation.8RAAaxisactivation
eventually leads toincreasedsodium reabsorption, prom-ptingthe onsetof post-diuretic sodiumretention and the braking phenomenon.15 Post-diuretic sodium retention is
oneoftheprocessesthroughwhichdiureticresistancemay be established and it arises as soon as the concentration ofdiureticinthetubularfluiddropsbelowthetherapeutic threshold.15Anegativenetsodiumbalanceinthe24hours
betweennatriuresisandpost-diureticsodiumretentionmay not be achieved in the event of dietary noncompliance,
rendering the diuretic effect insignificant.15 The braking
phenomenon,ontheotherhand,isdefinedasthedecrease indiuresisvolumeaftermultiplesame-doseadministrations ofdiuretic.This islinkedtoRAAaxis activationand com-pensatorychangesinthenephron.9
Tubularcompensatoryreadaptation
Tubular readaptation is another mechanism that helps explainreduced diuretic response.21 Owing to the
above-mentionedactivationoftheRAAaxis,aswellasthebraking phenomenon,proximaltubularreabsorptionarises,leading toincreasedsodiumuptake in thisareaofthe nephron.21
Simultaneously,the chronic use of loop diuretics --- which inhibit sodium uptake in the loop of Henle --- leads to increased sodium delivery to the distal tubular system, resulting in compensatory hyperplasia and hypertrophy.9
Thismeansthatthepatientwouldretainmoresodiumand thuswaterthanadiuretic-naïvepatient.13,21Thisresistance
mechanism can be overcome using a sequential nephron blockadewiththiazidediuretics.9
Druginteractions
Somedrugs, such asnonsteroidal anti-inflammatorydrugs (NSAIDs),canreducetheeffectofdiuretics.21
NSAIDs may cause diuretic resistance in a number of ways, particularly: decreased prostaglandin synthesis, decreasedrenalvasodilation, increasedrenalreabsorption inareas ofthe nephronother than theloopof Henleand hypertension.9 Evidence regarding the effect of low-dose
aspirin (<1 mg/kg/day) on diuretic response in particu-lar is more scarce and controversial. A previous study reported that chronic low-dose aspirin could profoundly affect platelet prostaglandin production without affect-ing diuretic-stimulated renal prostacyclin production or plasmareninactivity.27However,morerecently,Jhundetal.
demonstrated that the venodilation that occurs follow-ing furosemide administration could be inhibited by both high and low dose-aspirin.28 Furthermore, Hall noted an
important reduction in the need for diuretics when daily aspirin administration was stopped.29 There is also some
evidence that aspirin, even at a low dose, may neutral-izethefavorableeffectsofangiotensin-convertingenzyme inhibitorsbyblockingprostaglandinproductionand enhanc-ingthevasoconstrictorpotentialofendothelin.30Inpatients
withHF, aspirin should beavoided wherever possible and other antithrombotic agents that respect the integrity of prostaglandinmetabolismshouldbeconsidered.
Treatment
options
for
diuretic
resistance
Overall, there is a lack of high-quality clinical data to guidethechoiceoftreatmentstrategytoovercomediuretic resistance.31 Several strategies can be employed to aid
decongestion in patients with acute HF manifesting an impaired diuretic response. These include diuretic and nondiureticstrategies(Table3).21
Before considering the following treatment options, othercausesofapparentdiureticresistance,suchas third-spaceoverload withintravascular volumedepletion, must beruledout.
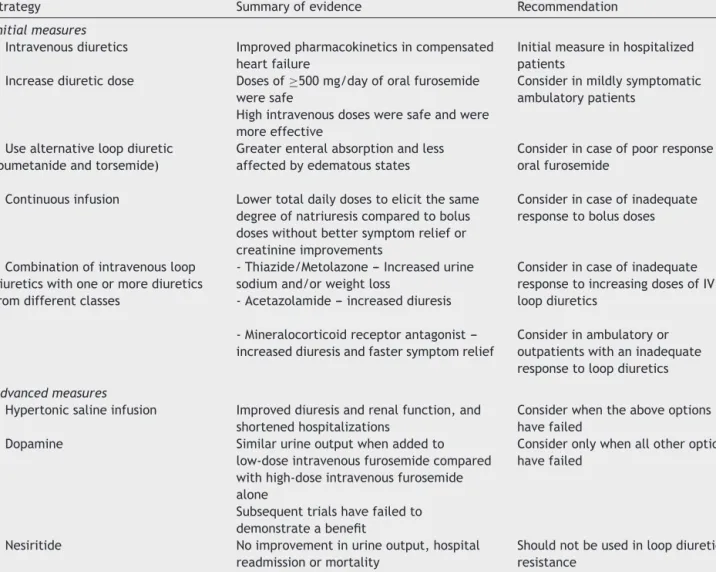
Table3 Strategiesfortreatingdiureticresistance.
Strategy Summaryofevidence Recommendation
Initialmeasures
Intravenousdiuretics Improvedpharmacokineticsincompensated heartfailure
Initialmeasureinhospitalized patients
Increasediureticdose Dosesof≥500mg/dayoforalfurosemide weresafe
Highintravenousdosesweresafeandwere moreeffective
Considerinmildlysymptomatic ambulatorypatients
Usealternativeloopdiuretic (bumetanideandtorsemide)
Greaterenteralabsorptionandless affectedbyedematousstates
Considerincaseofpoorresponseto oralfurosemide
Continuousinfusion Lowertotaldailydosestoelicitthesame degreeofnatriuresiscomparedtobolus doseswithoutbettersymptomreliefor creatinineimprovements
Considerincaseofinadequate responsetobolusdoses
Combinationofintravenousloop diureticswithoneormorediuretics fromdifferentclasses
-Thiazide/Metolazone---Increasedurine sodiumand/orweightloss
-Acetazolamide---increaseddiuresis
Considerincaseofinadequate responsetoincreasingdosesofIV loopdiuretics
-Mineralocorticoidreceptorantagonist ---increaseddiuresisandfastersymptomrelief
Considerinambulatoryor outpatientswithaninadequate responsetoloopdiuretics
Advancedmeasures
Hypertonicsalineinfusion Improveddiuresisandrenalfunction,and shortenedhospitalizations
Considerwhentheaboveoptions havefailed
Dopamine Similarurineoutputwhenaddedto low-doseintravenousfurosemidecompared withhigh-doseintravenousfurosemide alone
Subsequenttrialshavefailedto demonstrateabenefit
Consideronlywhenallotheroptions havefailed
Nesiritide Noimprovementinurineoutput,hospital readmissionormortality
Shouldnotbeusedinloopdiuretic resistance
AdaptedfromBowman,Nawarskas&Anderson(2016).31
Saltrestriction
Dietarysodiumrestrictionisakeydeterminantofdiuretic efficacy.Whendietarysodiumintakeis high,post-diuretic sodiumretentioncompensatesalmostentirelyforthe loop-diuretic-inducedsodiumloss. Conversely, ifsodiumintake isrestricted, post-diuretic sodiumretentionis minimized, resultingin a negative fluid and sodium balance.32 Thus,
restricting sodium intake to less than 100 mEq/day mit-igates the effect of post-diuretic sodium retention and helps achieve a negative sodium balance. A 24-hour uri-nary sodium excretion of more than 100 mEq/day or a fractional excretion of sodium value >2% indicates non-compliance with sodium restriction and rules out true diureticresistance.15
Discontinueconcomitantuseofnonsteroidal anti-inflammatorydrugs
Concomitant use of NSAIDs is a major cause of diuretic failure and discontinuing them can significantly improve diureticeffectiveness.15
Establishtheeffectivesingledose
Diuretics have a dose-response curve and the effect only beginsoncethediureticlevelreachesatherapeutic thresh-oldwithintherenaltubularlumen.InconditionssuchasCKD and cardiorenal syndrome, thedose-response curve shifts downwards and towards the right. This means that these patientsneedhigherdosesofloopdiureticstoachievethe therapeuticdruglevelatthesiteofaction.Diureticdoses belowsaidthresholdareineffective, soahighereffective singleloopdiureticdoseisneededratherthanadministering aninadequatedosemorefrequently.15
Increasedosefrequencyofloopdiuretics
Because most loop diuretics are short acting, increasing thedosefrequencycanhelpovercomepost-diureticsodium retentionandrestorediureticresponse.15
Diureticsubstitution
Gastrointestinal absorption and the bioavailability of dif-ferent diuretics belonging to the same class can vary
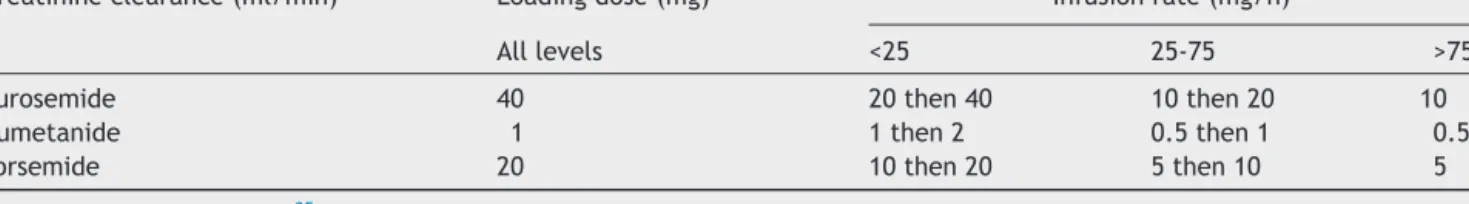
Table4 Dosageregimensforcontinuousintravenousdiureticadministration.
Creatinineclearance(ml/min) Loadingdose(mg) Infusionrate(mg/h)
Alllevels <25 25-75 >75
Furosemide 40 20then40 10then20 10
Bumetanide 1 1then2 0.5then1 0.5
Torsemide 20 10then20 5then10 5
AdaptedfromBrater(2011).35
considerably and this could be a factor behind a poor response. Furosemide has a bioavailability of about 50%, whereastorsemideandbumetanidehavealmostcomplete absorption(80-100%).Attimes, replacingfurosemidewith comparable doses of bumetanide or torsemide can be enoughtoimprovediuresis.15
Intravenousdiuretics
Sometimes, administering diuretics intravenously instead of orally is all that is needed to improve diuresis. Oral absorption may be altered in the presence of gastroin-testinaledema,gastroparesisanddelayedgastricemptying. Drug concentration at the site of diuretic action in the tubule lumen maybe inadequate,due todecompensated HF,renalhypoperfusionorimpairedsecretionasaresultof hypoalbuminemia.32
Compared to bolus doses, continuous diuretic infusion maybemoreeffectiveinimprovingdiuresis.Itmaydecrease fluctuations in intravascular volume, resulting in a more gradual and relatively constant hourly urine output and limitingtheeffectofpost-diureticsodiumretention.Some studies found that furosemide administered as a contin-uous infusion was more effective than intermittent bolus doses, since significantly less furosemide was required to producethesamediuresisandduetotheeliminationof a diuretic-free interval (during which compensatory sodium retention occurs).Said studiesfound nosignificant differ-encesinadverseeffectsandnochangeinserumcreatinine orhospitalmortality.33,34 Otherstudies reportedthatboth
regimenswereequallyeffectiveinachievinganegativefluid balance.32 In the Diuretic OptimizationStrategies
Evalua-tion(DOSE) trial, there wereno significant differencesin patients’ global symptom assessment or in the change in renal function between the two strategies.2 Despite the
conflicting evidence, pharmacodynamic concepts support the improved efficacy of continuous infusion of all loop diuretics except ethacrynic acid. A bolus dose of a loop diuretic should be administered before initiating a con-tinuous infusion or when the infusion rate is increasedin ordertodecrease thetime for thedrug’s onsetof action (Table4).32,35
Sequentialnephronblockade
Asequential sodiumuptake blockadeindifferentnephron segments by means of a combination of two or more diureticsfromdifferentclassesmayproduceanadditiveor synergisticmechanismofactionanddiureticresponse,and
canbeaneffectiveapproachinresistantcases(Table5).15
For edematous disorders other than liver cirrhosis and ascites,the evidence for specific diureticcombinations is less clear.36 The use of a loop diuretic and a thiazide or
thiazide-like diuretic withor without a potassium-sparing agentis most common in practice.15 Nevertheless, in the
absenceof evidenceonthe comparative efficaciesof the variousdiureticcombinations,choosingastrategyshouldbe basedonpatient-specificfactorsandthesideeffectprofiles ofthedifferentcombinations.31
Thiazide diuretics inhibit sodium reabsorption in the distal convoluted tubule and can thus counteract com-pensatory distal tubular hypertrophy.31 Metolazone and
hydrochlorothiazidearethetwothiazidesmost commonly used in combination with furosemide, although there is noclear evidence that one is superior to the other, nei-ther in terms of their efficacy in increasing diuresis nor theirsafety withregard torenal functionand electrolyte abnormalities.32,37,38 When initiating combination therapy,
thiazides should beadministered before intravenous loop diureticstoallowenoughtimeforthefullblockadeofthe distalnephron.32 Casestudiesand smallobservational
tri-als reported effective diuresis in 75-90% of patients who received thiazide diuretics in addition to loop diuretic therapy.31However,onedrawbackofthiazide-typediuretics
isthattheylimit thekidneys’capacitytoproducediluted urineandthusfreewaterclearanceandtheyshould there-forebeavoidedinhypotonichyponatremia.13
There isa paucity of data regardingspecific mineralo-corticoid receptor antagonists use in acute HF and the combination of spironolactoneand loop diuretics has not been shown to be synergistic. Nevertheless, said drugs
Table5 Combinationdiuretictherapy.
Toaneffectiveormaximalsafedoseofaloopdiureticadd: Distalconvolutedtubulediuretics
Metolazone2.5-10mgperosdaily(durationorfrequency adjustedbasedonthetargetweight)
Hydrochlorothiazide(orequivalent)25-100mgperosdaily Chlorothiazide500-1000mgintravenously
Proximaltubulediuretics
Acetazolamide250-375mgdailyorupto500mg intravenously
Potassium-sparingdiuretics
Spironolactone100-200mgdaily Amiloride5-10mgdaily
exhibitmildbuteffectivenatriureticeffectsandminimize potassiumwastingbyloopdiuretics.8,13 Moreover,
spirono-lactoneoreplerenonearerecommendedinallsymptomatic patients(despitetreatmentwithanangiotensin-converting enzymeinhibitorandabeta-blocker)withHFandareduced ejection fraction in order to reduce mortality and HF hospitalization.31Therefore,theremaybeastrongrationale
tocontinue andevenincrease dosingofthesedrugswhen theglomerularfiltrationrateisstableandserumpotassium levelsarelessthan5.5mEq/l.8,13
Whilethe diureticand natriureticcapacityof acetazo-lamideispooronitsown,itcouldwellbeaveryefficient booster of diuretic efficacy. The combination of acetazo-lamideandaloopdiureticcanbeveryeffective,blocking more than 90% of sodium reabsorption in the nephron. Moreover,it reduces renin releasewith potentially favor-ableeffectsonneurohormonalactivation. However,there are currently no data on the benefits of acetazolamide asadd-ontherapy andlong-termuse cancausemetabolic acidosis.13,15
Combination therapy is associated with a significant increaseinadverseeffectssuchaselectrolyteimbalances, dehydrationandrenalimpairment.Itrequirescareful mon-itoringandisbestreservedfortheoccasionalpatientwith highresistancetoloopdiuretics.15,32
Managementofintra-abdominalpressure
Intra-abdominalhypertensionisdefinedasasustained intra-abdominalpressure of12mmHgor above.Splanchnicand interstitialcongestionmaycauseelevatedintra-abdominal pressureintheabsenceofascitesinacutedecompensated HF. In such patients, a rise in intra-abdominal pressure increasesrenalvenouspressure,therebyreducingthe tran-srenal perfusion gradient and renal perfusion. Elevated intra-abdominalpressurealsocausesincreasedrenal inter-stitial pressure that opposes net filtration pressure. Both contribute to renal impairment and diuretic resistance. When intravenous loop diuretic therapy fails, measuring intra-abdominal pressure is an inexpensiveand minimally invasiveprocedurethatrulesoutadiureticresistancecause. Ifintra-abdominalhypertensionorabdominalcompartment syndrome(definedasasustainedintra-abdominalpressure of>20mmHgwhichisassociatedwithneworgan dysfunc-tion)isidentified,areductioninintra-abdominalpressure by mobilizing third-space fluid can be achieved through acombination of diuretics, vasodilatorsand/or inotropes. Abundantascitescanbemanagedwithparacentesis, ultra-sound or computer tomography guidance if needed. In certain patients, ultrafiltration (UF) may be appropriate. Thetherapeutic aimis toachievean abdominalperfusion pressure (calculated asthe mean arterial pressure minus the intra-abdominal pressure) of over 60 mmHg (with an intra-abdominalpressureof 5to7mmHg),whichsignifies afavorableoutcome(improvementinrenalperfusion,renal filtrationanddiuresis).25
Infusionwithalbumin
Simultaneous infusion of a diuretic and albumin could slightlyimprovediureticresistance.Ameta-analysisofeight
randomizedclinicaltrialsofadultswithhypoalbuminemia, comparingtheco-administrationofloopdiureticsand albu-minversus loopdiureticsalone,foundtransient effectsof modestclinicalsignificancewiththeformerstrategy.39
How-ever,thisinterventionshouldonlybeconsideredinseverely hypoalbuminemicpatients whenthe approachesdiscussed abovehavefailed.15
Renal-dosedopamine
Lowdosesofdopamine(<3g/kg/min)selectivelyworkon peripheraldopaminergicreceptorsresultinginvasodilation intherenal,coronary,splanchnicandcerebralcirculations. TworecenttrialsofdopamineinacuteHF---theDopaminein AcuteDecompensatedHeartFailureII(DAD-HFII)trialand theRenalOptimizationStrategiesEvaluation(ROSE)trial ---haveshownnoaddedbenefitwiththeadditionofdopamine tostandard therapywithhigh-dosediuretics.Thus,onthe basisofcurrentdata,dopaminehasnorolein nonhypoten-sivepatients withacuteHF. Intheabsenceofcardiogenic shock,however,theroleoflow-dosedopamineinacuteHF withhypotensionmeritsfurtherstudy.21,31
Alternativepharmacologicaltherapies
Hypertonicsalineworksosmoticallytopullfreewaterfrom theinterstitialfluidintotherenalvasculature.Inaddition toincreasingrenalbloodflow,itimprovessodiumdelivery totheloopofHenle,thusrestoringsomeoftheloop diuret-ics’ effect.Several studies have reportedbetter diuresis, improved renal function and shorter hospital stays when hypertonicsalineisaddedtoloopdiuretictherapy.31
NesiritideisasyntheticB-typenatriureticpeptide(BNP) approved by the Food andDrug Administration for symp-tomaticreliefduetoitsfavorableeffectsonhemodynamics, dyspneaand renalfunction.However,both theROSEtrial and ter Maaten et al. (2015) found no additive effect of usinglow-dosenesiritideaddedtodiuretictherapyinterms of decongestionor improved renalfunction. Experimental researchhasshown thatrenaldelivery of BNPhad signifi-cantlygreater beneficialeffectsthan systemicdelivery.It couldbe thata highersystemicdose is needed; however, theusagethereofwouldincreasetheincidenceofadverse effectssuchashypotension.18,40
Furthermore,itisworthnotingthatHFtrialsonnesiritide anddopaminehavenotbeenspecifictopatientsexhibiting aresistancetoloopdiuretics.31
Vasopressin-2-receptorantagonistsmaypromote aquare-sisbyblockingtheeffectsofvasopressinonthevasopressin 2 receptors located in the collecting ducts, thus blocking there-absorptionoffreewater.Thispromoteswater clear-ance without affecting sodiumbalance. Inthe Efficacy of VasopressinAntagonisminHeartFailureOutcomeStudywith Tolvaptan(EVEREST)trial,tolvaptanatadoseof30mgonce dailyforaminimumof60dayshadnoeffectontotal mor-talityorHFhospitalizationwhencomparedtoplacebo.21,41
Adenosineantagonistscanpotentiallyincrease glomeru-lar filtration and enhance the diuretic effect of diuretic drugs.However,thePlacebo-Controlled RandomizedStudy of the Selective Adenosine A1 Receptor Antagonist Rolo-fyllineforPatientsHospitalizedwithAcuteDecompensated
Heart Failure and Volume Overload to Assess Treatment Effect on Congestion and Renal Function (PROTECT) trial did not report any beneficial effects on congestion or renalfunctionandwasassociatedwithanincreasedriskof seizures.21,42
Glucocorticoidsmaypromotediuresisandprotectrenal functioninpatientswithacuteHF.Liuetal.reportedthe effects of prednisolone in 13 congestiveHF patients with significant volume overload and diuretic resistance who hadfailedtorespondtoaconventionalsequentialnephron blockade treatment strategy. They reported an improve-ment in diuresis,clinical status and renalfunction.43 The
sameauthorlaterreviewedtheavailableevidenceand con-cluded that the short-term use of glucocorticoids, when added to maximum conventional therapy, can potentiate renal responsiveness to diuretic therapy in patients with HF.44 However, larger randomized double-blind
placebo-controlledstudiesarewarrantedtodemonstratetheirsafety and efficacy in such patients. The proposed mechanism of action of glucocorticoids includes increasedexpression of natriuretic peptide receptor-A in the kidney and the hypothalamus,whichappeartobereducedinpatientswith HF,alsoincreasingrenalbloodflowthroughdilatationofthe renalvasculature via increased renalprostaglandin,nitric oxideanddopamineproduction.21,43,44
Levosimendan was studied in patients presenting with acute HF in the Randomized Multicenter Evaluation of IntravenousLevosimendanEfficacy(REVIVE)studies.These showed that levosimendan improved renal function and diureticresponseinsuchpatients.However,therewasalso anincreasedriskofarrhythmiaandhypotension.21
Ularitide, a human endogenous natriuretic peptide expressedinthekidney,whichinducesnatriuresisand diure-sisbybindingtoaspecificnatriureticpeptidereceptor,was investigatedin patientswithacuteHFin theEfficacy and SafetyofUlaritidefor theTreatment ofAcute Decompen-satedHeartFailure(TRUE-AHF)trial.Packeretal.reported favorable physiological effects (greater reductions in sys-tolic blood pressure and in levels of N-terminal pro---BNP [NT-proBNP] than the placebo group, without affecting cardiac troponin levels). However, short-term treatment neither affected the initial 48-hour clinical course nor reducedlong-termcardiovascularmortality.21,45
IntheEfficacyandSafetyofRelaxinfortheTreatmentof AcuteHeartFailure(RELAX-AHF)trial, serelaxin,ahuman recombinantformofthevasodilatorrelaxin,showedno sig-nificanteffectondiureticresponse,butdidhavebeneficial effectsinpreventingorgandamageinpatientswithacute HFwhowerediuretic-resistant.21,46TheEfficacy,Safetyand
Tolerabilityof SerelaxinWhen AddedtoStandard Therapy in AHF (RELAX-AHF-2)trial wasdesigned toconfirm sere-laxin’seffectontheseclinicaloutcomesbutitdidnotmeet eitherofitsprimaryendpoints.Therewasnodifferencein cardiovascularmortalityat180daysandthetrendfor reduc-ing worseningHFthrough day fivewithserelaxin was not statisticallysignificant.47
Thereareseveralotheragentsunderinvestigation,which could play a role in aiding decongestion of patients pre-senting with acute HF, such as omecamtiv mecarbil and TRV027.21
Omecamtivmecarbilisaselectivecardiacmyosin activa-torthatincreasesmyocardialfunctioninhealthyvolunteers
andinpatientswithchronicHF.Itseffectsonpatientswith acuteHFwereevaluatedintheAcuteTreatmentwith Ome-camtiv Mecarbil to Increase Contractility in Acute Heart Failure(ATOMIC-HF)trial.Thisstudyshowedthat omecam-tivmecarbilmayimprovedyspneascoreswhenhigherdoses wereused in comparison to placebo; however, it did not significantlyimproveoveralldyspneascores---the primary endpointofthestudy.48
TRV027 is a novel ligand of the angiotensin II type 1 receptor, selectively antagonizing the negative effects of angiotensin II, while preserving the potential pro-contractility effects of angiotensin II type 1 receptor stimulation. Its safety and efficacy were assessed in the BiasedligandoftheangiotensinIItype1receptorinpatients withacuteheartfailure(BLAST-AHF)trialand,althoughwell tolerated,TRV027 did notimprove clinical status through 30-dayfollow-upcomparedtoplacebo.49
Further studiesare needed toevaluate the safetyand efficacy of these drug candidates in a larger group of patientswithacuteHF.
Ultrafiltration
UFis very effective at removing plasma fluid from blood across a semipermeable membrane that allows small moleculestopassthroughalongitspressuregradienttothe ultrafiltratefluid.21
Smallstudies suggest thatUF improves pulmonary and peripheraledema,lungfunctionandhemodynamicswithout adverseeffectsonrenalfunction.Thefluidremovalrateis reevaluatedusingclinicalassessmentandserialhematocrit measurementstoensureappropriatevascularcompartment refill.21
The recent development of veno-venousperipheral UF haspositionedthistechniqueasapotentialalternative to loopdiureticsinacuteHF.21
The Relief for Acutely Fluid-Overloaded Patients With DecompensatedCongestiveHeartFailure(RAPID-CHF)trial, a multicenter randomized controlled trial involving forty patients,found that UFwas feasible, well-tolerated, and resultedinsignificantweightlossandfluidremoval.50
Favorable outcomes were also reported in the Ultra-filtration versus Intravenous Diuretics for Patients Hospi-talizedforAcuteDecompensated CongestiveHeartFailure (UNLOAD)trial.This prospective,randomized,multicenter trialinvolving200patients,found thatUFsafelyproduces greater weight and fluid loss than intravenous diuretics, reduces90-dayresourceutilizationforHFandisaneffective alternativetherapy.51
IntheUltrafiltration vs.DiureticsinDecompensatedHF (ULTRADISCO)study,aprospective,randomized,open-label, single-centerstudy whichincluded30 patients,theuseof UFwasassociatedwithgreaterhemodynamicstabilityand withagreaterreductioninplasmalevelsofNT-proBNPand aldosteronecomparedtodiureticinfusion.52
In the Continuous Ultrafiltration for Congestive Heart Failure(CUORE)trial,UFasafirst-linetreatmentinpatients withsevere congestive HF wasassociated withprolonged clinicalstabilizationandgreaterfreedomfrom rehospital-ization for congestive HF compared to standard medical therapyalone.53
The CardiorenalRescue Studyin AcuteDecompensated Heart Failure (CARRESS-HF), however, found a stepped pharmacologic-therapyalgorithm tobesuperior toUF for thepreservationofrenalfunctionat96hours,witha simi-laramountofweightlossseenwiththetwoapproachesand ahigherrateofadverseeventsobservedwithUF.54
Results of the Reverse Worsening Renal Function in Decompensated Heart Failure (REWORD-HF) study (which endedinApril 2017)arestillpendingandwillhelp deter-minewhetherfluidremovalby UFis superiortodifferent pharmacologicalapproachesinacutelyrelievingcongestion andpreventingfurtherdeteriorationinrenalfunctionand whetheritresultsinlongeradmission-freesurvival90days afterenrolmentinpatientswithdecompensatedHFand car-diorenalsyndrome.
Sevenrandomizedcontrolledtrials,includingseveralof thosementionedabove,weresubmittedforameta-analysis. UF was found to be an effective and safe therapeu-tic strategy, resulting in greater weight loss and fluid removal without affecting renal function, mortality or rehospitalization.55
The2016EuropeanSocietyofCardiologyguidelinesstate that thereis no evidence favoring UF over loop diuretics asfirst-line therapyinpatients withacuteHF. Theformer shouldthus beconfinedtopatientswhofailtorespondto diuretic-basedstrategies.
Conclusion
Diureticresistancehas emergedasan independentfactor behindworseHFpatientoutcomes,namelyin-hospital wors-ening,earlypost-dischargemortalityandrehospitalizations. While several mechanisms help to explain their reduced responsetodiuretics, the definitionof the problemitself remains elusive. More recent evidence is leaningtowards thecoupling of parameterssuch asweight lossand urine outputtodiureticdose,butseveralchallengesremain. Non-pharmacologicalmeasuresandafewmedicaloptions,such ascontinuousinfusion ofdiureticsandsequential nephron blockade,maybeusedtoovercomediureticresistance. Nev-ertheless,disease progressionmay warrant more invasive methodsfor fluidremoval.Therapymustbe tailoredona case-by-casebasis.
Conflicts
of
interest
Theauthorshavenoconflictsofinteresttodeclare.
References
1.IyengarS,AbrahamWT.Diureticresistanceinheartfailure.Curr HeartFailRep.2006;3:41---5.
2.Felker GM, Lee KL, Bull DA, et al. Diuretic strategies in patientswithacutedecompensatedheartfailure.NEnglJMed. 2011;364:797---805.
3.CeiaF,FonsecaC,MotaT,etal.Prevalence ofchronic heart failureinSouthwesternEurope:theEPICAstudy.EurJHeart Fail.2002;4:531---9.
4.Jentzer JC, Dewald TA, Hernandez AF. Combination of loop diureticswith thiazide-typediuretics inheart failure.JACC. 2010;56:1527---34.
5.ValenteMA,VoorsAA,DammanK,etal.Diureticresponsein acuteheartfailure:clinicalcharacteristicsandprognostic sig-nificance.EurHeartJ.2014;35:1284---93.
6.Bruyne LKM. Mechanisms and management of diuretic resistance in congestive heart failure. Postgrad Med J. 2003;79:268---71.
7.SicaDA,DeedwaniaPC. Diureticresistance andstrategiesto overcomeresistanceinpatientswithcongestiveheartfailure. CongestHearFail.2002;8:80---5.
8.EllisonDH.Diuretictherapyandresistanceincongestiveheart failure.Cardiology.2001;96:132---43.
9.CoxZL,LenihanDJ.Loopdiureticresistanceinheartfailure: resistanceetiology-basedstrategiestorestoringdiuretic effi-cacy.JCardFail.2014;20:611---22.
10.VerbruggeFH,DupontM,BertrandPB,etal.Determinantsand impactofthenatriureticresponsetodiuretictherapyinheart failure withreduced ejection fraction and volumeoverload. ActaCardiol.2015;70:265---73.
11.Testani JM,Brisco MA, Turner JM,et al. Loop diuretic effi-ciency: a metric of diuretic responsiveness with prognostic importanceinacutedecompensatedheartfailure.CircHeart Fail.2014;7:261---70.
12.SinghD,ShresthaK,TestaniJM,etal.Insufficientnatriuretic responseto continuous intravenous furosemide is associated withpoorlong-termoutcomesinacutedecompensatedheart failure.JCardFail.2014;20:392---9.
13.VerbruggeFH,MullensW,TangWH.Managementofcardio-renal syndromeanddiureticresistance.CurrTreatOptionsCardiovasc Med.2016;18:11.
14.VaduganathanM,KumarV,VoorsAA,etal.Unsolvedchallenges indiuretictherapyforacuteheartfailure:afocusondiuretic response.ExpertRevCardiovascTher.2015;13:1075---8.
15.IqbalJ,JavaidMM.Diureticresistanceanditsmanagement.Br JHospMed(Lond).2014;75:C103---7.
16.NeubergGW,MillerAB,O’ConnorCM,etal.Diureticresistance predictsmortalityinpatientswithadvancedheartfailure.Am HeartJ.2002;144:31---8.
17.FonarowGC.TheAcuteDecompensatedHeartFailureNational Registry(ADHERE):opportunitiestoimprove careofpatients hospitalizedwithacutedecompensatedheartfailure.Rev Car-diovascMed.2003;4Suppl.7:S21---30.
18.terMaatenJM,DunningAM,ValenteMA,etal.Diureticresponse inacuteheartfailure-ananalysisfromASCEND-HF.AmHeartJ. 2015;170:313---21.
19.Kumar D, BagarhattaR. Fractional excretionof sodium and itsassociationwithprognosisofdecompensatedheartfailure patients.JClinDiagnRes.2015;9:OC01---3.
20.TerMaatenJM,DammanK,HanbergJS,etal.Hypochloremia, diureticresistance,andoutcomeinpatientswithacuteheart failure.CircHeartFail.2016;9.
21.VazirA,CowieMR.Decongestion:diureticsandothertherapies forhospitalizedheartfailure.IndianHeartJ.2016;68Suppl. 1:S61---8.
22.VoorsAA,DavisonBA,TeerlinkJR,etal.Diureticresponsein patientswithacute decompensatedheartfailure: character-isticsandclinicaloutcome-ananalysisfromRELAX-AHF.EurJ HeartFail.2014;16:1230---40.
23.de Silva R, Nikitin NP, Witte KK, et al. Incidence of renal dysfunctionover6monthsinpatientswithchronicheart fail-uredueto left ventricularsystolicdysfunction: contributing factors and relationship to prognosis. EurHeart J. 2006;27: 569---81.
24.NayorM,LarsonMG,WangN,etal.Theassociationofchronic kidneydisease and microalbuminuriawithheartfailure with preserved vs. reduced ejection fraction. Eur J Heart Fail. 2017;19:615---23.
25.Nguyen VQ, Gadiraju TV, Patel H, et al. Intra-abdominal hypertension: an important consideration for diuretic
resistanceinacutedecompensatedheartfailure.ClinCardiol. 2016;39:37---40.
26.MillerWL.Fluidvolumeoverloadandcongestioninheart fail-ure: timeto reconsider pathophysiology and howvolume is assessed.CircHeartFail.2016;9:e002922.
27.WilsonTW,McCauleyFA,WellsHDJ.Effectsoflow-doseaspirin onresponsestofurosemide.ClinPharmacol.1986;26:100---5.
28.JhundPS,DavieAP,McMurrayJJ.Aspirininhibitstheacute ven-odilatorresponsetofurosemideinpatientswithchronicheart failure.JAmCollCardiol.2001;37:1234---8.
29.HallD.Controversiesinheartfailure.Arebeneficialeffectsof angiotensin-convertingenzymeinhibitorsattenuatedbyaspirin inpatientswithheartfailure?CardiolClin.2001;19:597---603.
30.Cleland JG, John J, Houghton T. Does aspirin attenuate the effect of angiotensin-converting enzyme inhibitors in hypertensionor heart failure?Curr OpinNephrol Hypertens. 2001;10:625---31.
31.BowmanBN,NawarskasJJ,AndersonJR.Treatingdiuretic resis-tance:anoverview.CardiolRev.2016;24:256---60.
32.AsareK.Managementofloopdiureticresistanceintheintensive careunit.AmJHealth-SystPharm.2009;66:1635---40.
33.LahavM,RegevA,Ra’ananiP,etal.Intermittentadministration offurosemidevscontinuousinfusionprecededbyaloadingdose forcongestiveheartfailure.Chest.1992;102:725---31.
34.DormansTP,vanMeyelJJ,GerlagPG,etal.Diureticefficacy ofhighdosefurosemideinsevereheartfailure:bolusinjection versuscontinuousinfusion.JAmCollCardiol.1996;28:376---82.
35.BraterC.Updatein diuretic therapy:clinicalpharmacology. SeminNephrol.2011;31:483---94.
36.HoornEJ, Ellison DH. Diuretic resistance. Am J Kidney Dis. 2017;69:136---42.
37.MoranvilleMP,ChoiS,HoggJ,etal.Comparisonofmetolazone versus chlorothiazide in acute decompensated heart failure withdiureticresistance.CardiovascTher.2015;33:42---9.
38.ShulenbergerCE,JiangA,DevabhakthuniS,etal.Efficacyand safety of intravenous chlorothiazide versus oral metolazone inpatientswithacutedecompensatedheartfailureand loop diureticresistance.Pharmacotherapy.2016;36:852---60.
39.Kitsios GD,Mascari P, Ettunsi R, et al. Co-administration of furosemidewithalbuminforovercomingdiureticresistancein patientswithhypoalbuminemia:ameta-analysis.JCritCare. 2014;29:253---9.
40.WanSH,StevensSR,BorlaugBA,etal.Differentialresponseto low-dosedopamineorlow-dosenesiritideinacuteheart fail-urewithreducedorpreservedejectionfraction:resultsfrom theROSEAHFTrial(RenalOptimizationStrategiesEvaluationin AcuteHeartFailure).CircHeartFail.2016;9.
41.CavalcanteJL,KhanS,GheorghiadeM.EVERESTstudy:efficacy ofvasopressinantagonisminheartfailureoutcomestudywith tolvaptan.ExpertRevCardiovascTher.2008;6:1331---8.
42.VoorsAA,DittrichHC,MassieBM,etal.Effectsofthe adeno-sine A1 receptor antagonist rolofylline on renal function in patientswithacuteheartfailureandrenaldysfunction:results fromPROTECT (Placebo-ControlledRandomized Studyofthe
Selective Adenosine A1 Receptor Antagonist Rolofylline for PatientsHospitalizedwithAcuteDecompensatedHeartFailure andVolumeOverloadtoAssessTreatmentEffectonCongestion andRenalFunction).JAmCollCardiol.2011;57:1899---907.
43.LiuC,LiuG,ZhouC,etal.Potentdiureticeffectsofprednisone inheartfailurepatientswithrefractorydiureticresistance.Can JCardiol.2007;23:865---8.
44.LiuC,LiuK.Effectsofglucocorticoidsinpotentiatingdiuresis inheartfailurepatientswithdiureticresistance.JCardFail. 2014;20:625---9.
45.PackerM,O’ConnorC,McMurrayJJ,etal.Effectofularitideon cardiovascularmortalityinacuteheartfailure.NEnglJMed. 2017;376:1956---64.
46.Teerlink JR, Cotter G, Davison BA, et al. Serelaxin, recom-binanthumanrelaxin-2,for treatmentofacuteheartfailure (RELAX-AHF):arandomised,placebo-controlledtrial.Lancet. 2013;381:29---39.
47.TeerlinkJR,VoorsAA,PonikowskiP,etal.Serelaxininaddition tostandardtherapyinacuteheartfailure:rationaleanddesign oftheRELAX-AHF-2study.EurJHeartFail.2017;19:800---9.
48.Teerlink JR, Felker GM, McMurray JJV, et al. Acute treat-ment with omecamtiv mecarbil to increase contractility in acuteheartfailure:theATOMIC-AHFstudy.JAmCollCardiol. 2016;67:1444---55.
49.Pang PS, Butler J, Collins SP, et al. Biased ligand of the angiotensin II type 1 receptor in patients with acute heart failure:arandomized,double-blind,placebo-controlled,phase IIB, dose ranging trial (BLAST-AHF). Eur Heart J. 2017;38: 2364---73.
50.Bart BA,Boyle A,BankAJ, etal. Ultrafiltrationversususual careforhospitalizedpatientswithheartfailure:theRelieffor Acutely Fluid-Overloaded Patients withDecompensated Con-gestive Heart Failure (RAPID-CHF) trial. J Am Coll Cardiol. 2005;46:2043---6.
51.Costanzo MR, Guglin ME, Saltzberg MT, et al. Ultrafiltra-tion versus intravenous diuretics for patients hospitalized for acute decompensated heart failure. J Am Coll Cardiol. 2007;49:675---83.
52.GiglioliC,LandiD,CecchiE,etal.EffectsofULTRAfiltrationvs, DIureticSonclinical,biohumoralandhaemodynamicvariables inpatientswithdeCOmpensatedheartfailure:theULTRADISCO study.EurJHeartFail.2011;13:337---46.
53.MarenziG,MuratoriM,CosentinoER,etal.Continuous ultra-filtrationforcongestiveheartfailure:theCUOREtrial.JCard Fail.2014;20:9---17.
54.BartBA,GoldsmithSR,LeeKL,etal.Ultrafiltrationin decom-pensatedheartfailurewithcardiorenalsyndrome.NEnglJMed. 2012;367:2296---304.
55.Cheng Z,Wang L, GuY, et al. Efficacyand safetyof ultra-filtration indecompensatedheartfailure patientswithrenal insufficiency.IntHeartJ.2015;56:319---23.
56.AronsonD,BurgerAJ.Diureticresponse:clinicaland hemody-namicpredictorsandrelationtoclinicaloutcome.JCardFail. 2016;22:193---200.