r e v b r a s r e u m a t o l . 2014;54(5):393–396
REVISTA
BRASILEIRA
DE
REUMATOLOGIA
ww w . r e u m a t o l o g i a . c o m . b r
Case
report
Acute
myocardial
infarction
as
Eosinophilic
granulomatosis
with
polyangiitis
(formerly
Churg
Strauss
syndrome)
initial
presentation
Wahinuddin
Sulaiman
a,
Ong
Ping
Seung
a,∗,
Sabariah
Mohd
Noor
baDivisionofRheumatology,DepartmentofMedicine,HospitalRajaPermaisuriBainunIpoh,Perak,Malaysia
bDepartmentofPathology,HospitalRajaPermaisuriBainunIpoh,Perak,Malaysia
a
r
t
i
c
l
e
i
n
f
o
Articlehistory:
Received6February2013 Accepted21March2013 Availableonline29August2014
Keywords:
ChurgStrausssyndrome Eosinophilicgranulomatosiswith polyangiitis
Hypereosinophilia Asthma
Myocardialinfarction
a
b
s
t
r
a
c
t
Eosinophilicgranulomatosiswithpolyangiitisisarareprimaryvasculiticdisease character-izedbyhypereosinophilia,lateonsetasthmaandextravasculareosinophilgranulomas.We reportacasepresentedinitiallywithacutemyocardialinfarctionwhichlateronlyproceed with asthma, skin manifestations and peripheral neuropathy. Laboratory parameters showedhypereosinohpiliawithnegativeperinuclearpatternofantineutrophilcytoplasmic autoantibodies(p-ANCA).Skinbiopsyshowedleucocytoclasticvasculitiswitheosinophilic infiltrationwhilecoronaryangiographywasnormal.Thepatient’ssymptomsimprovedwith IVmethylprednisolone,pulsecyclophosphamideandazathioprine.
©2014ElsevierEditoraLtda.Allrightsreserved.
Infarto
agudo
do
miocárdio
como
apresentac¸ão
inicial
de
granulomatose
eosinofílica
com
poliangiite
(anteriormente,
síndrome
de
Churg
Strauss)
Palavras-chave:
SíndromedeChurgStrauss Granulomatoseeosinofílicacom poliangiite
Hipereosinofilia Asma
Infartodomiocárdio
r
e
s
u
m
o
Agranulomatoseeosinofílicacompoliangiiteéumavasculiteprimáriarara,caracterizada porhipereosinofilia,asmadesurgimentotardioegranulomaseosinofílicosextravasculares. Relatamos um caso apresentado inicialmente com infarto do miocárdio e que, ulteri-ormente,teveprosseguimentoapenascomasma,manifestac¸õescutâneaseneuropatia periférica.Os parâmetros laboratoriaisrevelaramhipereosinofiliacomum padrão peri-nuclearnegativodeautoanticorposcitoplásmicosantineutrófilos(p-ANCA).Abiópsiade pele demonstrouvasculite leucocitoclásticacominfiltrac¸ãoeosinofílica, diantede uma
DOIoforiginalarticle:http://dx.doi.org/10.1016/j.rbr.2013.03.002.
∗ Correspondingauthor.
E-mail:ongps@hotmail.com(O.P.Seung). http://dx.doi.org/10.1016/j.rbre.2013.03.002
394
rev bras reumatol.2014;54(5):393–396angiografiacoronárianormal.Ossintomasdopacientemelhoraramcommetilprednisolona IV,pulsoterapiacomciclofosfamidaeazatioprina.
©2014ElsevierEditoraLtda.Todososdireitosreservados.
Introduction
Eosinophilicgranulomatosiswithpolyangitis(EGPA),or previ-ouslybetterknownasChurgStraussSyndrome(CSS),isarare disorderwithanannualincidenceof2.7casespermillion.1It
ischaracterizedbyhypereosinophilia,lateonsetasthmaand extravasculareosinophilgranulomas.Thiswasfirstdescribed byChurgandStrassin1951.2EGPAisvariableinits
manifesta-tions,whichmayrangefromskinlesions,asthma,non-erosive arthritistolifethreateningconditions, suchascardiac dis-ease,severegastrointestinalandperipheralnervoussystem involvement.Cardiacinvolvementisaleadingcauseof mor-tality,accountingfor48%ofdeathsinEGPA.3
The1990AmericanCollegeofRheumatology(ACR) classifi-cationcriteriaforEGPArequiredthepresenceoffourormore ofthefollowingsixcriteriaformakingthediagnosis:asthma, eosinophilia(>10% ofleukocytes bydifferential cell count), mononeuritismultiplexorpolyneuropathy,pulmonary infil-trates(maybetransient,paranasalsinusitisandhistological proof of vasculitis with extravascular eosinophils).4 The
recently published 2012 Revised International Chapel Hill ConsensusConference(CHCC)NomenclatureofVasculitides stated EGPA as an antineutrophil cytoplasmic antibodies (ANCA) associated vasculitides with eosinophil-rich and necrotizinggranulomatousinflammationofteninvolvingthe respiratory tract, and necrotizing vasculitis predominantly affecting small to medium vessels, and associated with asthmaandeosinophilia.5
We report a 50-year-old man presented with inferior myocardial infarction who later developed skin manifes-tations, exacerbation of bronchial asthma and disabling peripheralneuropathy.
Case
report
A50-year-oldmalewaspresentedatouremergency depart-mentwithseverechestpainandshortnessofbreathfor2days. Hispastmedicalhistoryrevealedhypercholesterolemiawith noprevioushospitalizations.The12-leadelectrocardiogram (ECG)showed asinus rhythmand ST-segment elevationin theinferiorleads.Echocardiographyrevealedagoodleft ven-tricularsystolicfunctionwithejectionfractionof78% with noregionalwallmotionabnormality.Laboratoryassessment showedraisedCKMB148U/L(normal<25U/L)andLDH2,047 U/L(normal 200-480U/L).Due tolatepresentation,hewas notthrombolyzed.Hewaspreparedforpercutaneouscardiac intervention(PCI), but herefused. He wasdischarged with medicationsforcoronaryarterydisease.
Two weekslater,hedeveloped multiplepainfulnodular lesionsoverhissolesandhandsassociatedwithintermittent fever.Furtherquestioningrevealedthathehadbeensuffering
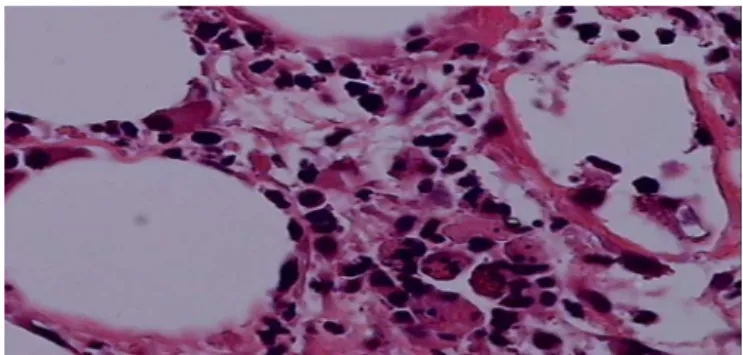
Figure1–Skinbiopsyofthispatientwhichshows lymphocyticandeosinophilicinfiltrationsconsistentwith leukocytoclasticvasculitis.
fromdrycoughfor1yearforwhichhedidnotseekany treat-ment.Therewas noallergicrhinitisorany symptomsthat might suggest asthma.However,hestill experiencedchest discomfortsincedischarged2weeksago.
Chestradiographwasnormal.Repeatedechocardiographs showed global hypokinesia with poor left ventricular sys-tolicfunctionof35%.Laboratoryanalysesshowedanincrease white blood cell count (14,900/L) with predominance of eosinophils(33%),LDH863U/L,raisederythrocyte sedimen-tationrate(52mm/h),CRP(125U/L)andpositiverheumatoid factor. Immunological markers, such as antinuclear anti-body, perinuclear and classic ANCA, extractable nuclear antigenwereallnegative.Askinbiopsywasperformedand showeddenseneutrophilicandlymphocyticinfiltrationswith eosinophilicvasculiticchanges(Fig.1).Heonlyfulfilled2out ofthe6oftheACRclassificationcriteriawithnohistoryof asthmaorsinusits.However,hewasgivenprednisolone60mg (1mg/kg),andhisskinlesionsimproved.Thistimeheagreed onundergoingcoronaryangiography,whichshowedno evi-denceofatheromaoncoronaryluminogram.
Four months later, he presented with exacerbation of bronchialasthmawithnocturnalcough.Therewerenonew skinlesionsorchestpain.Hissymptomsimprovedwith neb-ulizersandashortcourseofprednisolone30mg(0.5mg/kg) for5days.
Duringthefollow-up,6monthslater,hiscomplaintof Ray-naud’sphenomenonandnumbnessoverbothhislowerlimbs withmoreprominentovertherightfoot.Thiswasproceeded with right foot dorsiflexion weakness. Thephysical exam-ination revealed right footdrop, vasculiticlesions over the palmsand anodulewithnecrotizingsurfaceovertheright hand.Laboratoryfindingsshowedraisedwhitecellcounts22.2 witheosionophils(78.8%),ESR32mm/handCRP64U/L. Elec-tromyographyandnerveconductionstudieswereconsistent withsensorimotorpolyneuropathy.
rev bras reumatol.2014;54(5):393–396
395
amlodipine 5mg daily. Afterthe completion ofIV methyl-prednisolone, monthly intravenous cyclophosphamide was administered for6months. Thepatient responded well to thetreatment,withimprovementofthesymptomsAfterthe completionofthepulsecyclophosphamide,hewasaddedon azathioprine25mgdaily.
Throughoutthe 8yearsfollow-up, therewas norelapse afterinitiationoftheimmunosuppressivetreatments. How-ever,thepatientstillexperiencesomeresidualneurological deficitoftherightfoot.Otherwise,thelaboratoryparameters andechocardiographywereallnormal.
Discussion
EGPA is a multisystem vasculitic disorder which involve medium to small sized muscular arteries and veins. It is typically manifested in 3 consecutive phases. The pro-dromal phase consists of allergic manifestations. The second phase involves tissue eosinophilia infiltration and blood eosinophilia. This is followed by vasculitic sys-temicmanifestations.6However,thispatienthadadifferent
sequenceinwhichacutemyocardialinfarctionwastheinitial presentationandasthmaticsymptomsonlyappearedlater.
EGPAmayaffectthemyocardium,valves,coronaryarteries and pericardium. This will lead to structural and func-tional impairment.7 Eosinophils infiltrate the myocardium
and release toxic inflammatory mediators which lead to arrhythmiasandsystolicdysfunction.8Cardiacinvolvement
isthemajorcauseofmortalityinEGPAwithpooroutcomes, butitisfullyreversibleasoccurredinthispatient.9However,
both1990ACRclassificationcriteriaandthenewrevisedCHCC nomenclaturedonotemphasizeoncardiacsymptoms.
Peripheralnerve involvementis the most frequent vas-culitic manifestation of EGPA.10 Most patients responded
wellwithimmunosuppressivetherapy,howeversome resid-ualsymptomsmightpersistasinthiscase.11 Otherorgans
involvementincludescutaneouslesions,lungs(asthma,nasal polyps),kidneyandgastrointestinalinvolvement.
Laboratoryparameterswerenon-specific,whichincluded raisedESR,CRPandeosionophilcounts.
Anti-MPO perinuclear ANCA (p-ANCA) can be found in only30%-40% of patients with EGPA.12 Most patients with
positive ANCA had glomerulonephritis, peripheral neurop-athyandvasculitisinbiopsy.13Itwasnegativeinourpatient.
Indeed,few literatureshad reported that EGPA with heart involvementaremainlyANCAnegative.13,14Persistent
hyper-eosinophilia alone does not exclude other diagnosis such ashypereosinophilicsyndromes. However,thepresencesof otherclinicalmanifestationshelptoreachthediagnosis.
Thefive-factorscorewasdevelopedbytheFrench Vasculi-tis StudyGroup to predict the risk ofdeath inEGPA. This includes,reducedrenalfunction(creatinine>1.58mg/dLor 140moL/L),proteinuria(>1g/24h),gastrointestinal hemor-rhage,infarctionorpancreatitis,involvementofthecentral nervoussystemandcardiomyopathy.Presenceofanyoneof thesehave5-yearmortalityof26%,while2ormorewith46% mortality.15
Currently,thereisnoestablishedprotocol fortreatment ofEGPA.Thetypeoftreatmentmainlybasedontheseverity
of the disease. Minor manifestations, such as asthma or cutaneousmanifestationscanbetreatedwithcorticosteroids alone.Lifethreateningmultisysteminvolvement(acute coro-narysyndrome,severeperipheralpolyneuropathyorsevere gastrointestinal involvement)requiredcombination therapy of glucocorticoids and cyclophosphamide. In this patient, he was given 3 consecutive days of intravenous methyl-prednisolone (500mg/m2)followed bymonthly pulse ofIV cyclophosphamide(750mg/m2)for6months.
Therewasadelayinreachingthediagnosisinthispatient asasthmaticsymptomsonlybecomeapparentafter5months oftheinitialpresentations.Ittookapproximately10months forthe disease toevolve from acutemyocardial infarction, cutaneouslesionsandexacerbationofasthmatoperipheral neuropathy.
Reportsshowthat45%oftherelapsesoccurredduringthe firstyearoftherapy,anditoccureitherverysoonorlongafter theclinicalremission.16 Sofar,therewasnorelapseafter8
yearsoffollowup.
Conclusions
EGPAisamultisystemdisease,andtoobtainthediagnosiscan bechallenging.HighsuspicionforEGPAshouldberaised espe-ciallyinyoungpatientswhopresentedwithacutecoronary syndromewithoutanyriskfactorsassociatedwithhistoryof asthmaandperipheraleosinophiliaofmorethan10%.
Conflicts
of
interest
Theauthorsdeclarenoconflictsofinterest.
r
e
f
e
r
e
n
c
e
s
1.WattsRA,LaneSE,BenthamG,ScottDG.Epidemiologyof systemicvasculitis:aten-yearstudyintheUnitedKingdom. ArthritisRheum.2000;43:414–9.
2.ChurgJ,StraussL.Allergicgranulomatosis,Allergicangiitis, andpolyarteritisnodosa.AmJPathol.1951;27:277–301. 3.LanhamJG,CookeS,DaviesJ,HughesGRV.Endomyocardial
complicationsoftheChurgStrausssyndrome.PostgradMedJ. 1985;61:341.
4.MasiAT,HunderGG,LieJT,MichelBA,BlochDA,ArendWP, etal.TheAmericanCollegeofRheumatology1990Criteriafor theclassificationofChurg-Strausssyndrome(allergic granulomatosisandangiitis).ArthritisRheum. 1990;33:1094–100.
5.JennetteJC,FalkRJ,BaconPA,BasuN,CidMC,FerrarioF,etal. 2012Revisedinternationalchapelhillconsensusconference nomenclatureofvasculitides.ArthritisRheum.2013;65:1–11. 6.LanhamJG,ElkonKB,PuseyCD,HughesGR.Systemic
vasculitiswithasthmaandeosinophilia:aclinicalapproach totheChurg-Strausssyndrome.Medicine.1984;63:65–81. 7.MasiAT,HunderGG,LieJT,MichelBA,BlochDA,ArendWP,
etal.1990criteriafortheclassificationofChurgStrauss syndrome.ArthritisRheum.1990;33:1094.
8.RothenbergME.Eosinophilia.NEngJMed.1998;38:1592–600. 9.GasleyP,FollansbeeW,CoulehanJ.Cardiacmanifestationsof
396
rev bras reumatol.2014;54(5):393–39610.EustaceJA,NadasdyT,ChoiM.TheChurg-Strausssyndrome. JAMSocNephrol.1999;10:2048–55.
11.HatooriN,IchimuraM,NagamatsuM,LiM,YamamotoK, KumazawaK,etal.Clinicopathologicalfeaturesof Churg-StraussSyndromeassociatedneuropathy.Brain. 1999;122:427–39.
12.HelmichB,FlossmannO,GrossWL,BaconP,Cohen-Tervaert JW,GuillevinL,etal.EULARrecommendationforconducting clinicalstatisticand/orclinicaltrialsinsystemicvasculitis: Focusonanti-neutrophilcytoplasmantibody-associated vasculitis.AnnRheum.2007;66:605–17.
13.Sablé-FourtassouR,CohenP,MahrA,PagnouxC,MouthonL, JayneD,etal.Antineutrophilcytoplasmicantibodiesandthe
Churg-Strausssyndrome.AnnInternMed.2005;143: 632–8.
14.WagnerAD,MeyerGP,RihlM,RathmannA,WittkopU, ZeidlerH,etal.Acutecoronarysyndromeassociatedwith Churg-Strausssyndrome.VascularHealthandRisk Management.2007;3:775–9.
15.GuillevinL,LhoteF,GayraudM,CohenP,JarrousseB, LortholaryO,etal.Prognosticfactorsinpolyarteritisnodosa andChurg-Strausssyndrome.Aprospectivestudyin342 patients.Medicine(Baltimore).1996;75:17–28.