BrazJOtorhinolaryngol.2017;83(1):94---97
www.bjorl.org
Brazilian
Journal
of
OTORHINOLARYNGOLOGY
ORIGINAL
ARTICLE
Which
features
of
advanced
head
and
neck
basal
cell
carcinoma
are
associated
with
perineural
invasion?
夽
André
Bandiera
de
Oliveira
Santos
∗,
Natália
Martins
Magacho
de
Andrade,
Lenine
Garcia
Brandão,
Claudio
Roberto
Cernea
UniversidadedeSãoPaulo(USP),SãoPaulo,SP,Brazil
Received1November2015;accepted29January2016 Availableonline19April2016
KEYWORDS Perineuralinvasion; Basalcellcarcinoma; Headandneck
Abstract
Introduction:Perineuralinvasionisauniqueroutefortumordissemination.Inbasalcell carci-nomas,theincidenceislow,butincreasesinadvancedcases.Itsimportanceisrecognizedbut notfullyunderstood.
Objective:Tocompareheadandneckbasalcellcarcinomaswithandwithoutperineural inva-sion.
Methods:Aretrospectivemedicalchartreviewofmultidisciplinarysurgeriesforbasalcell car-cinomas thatrequired a headand necksurgeryspecialist in atertiary referral center was performed.Clinical-demographicsandhistopathologicalfeatureswereanalyzed.
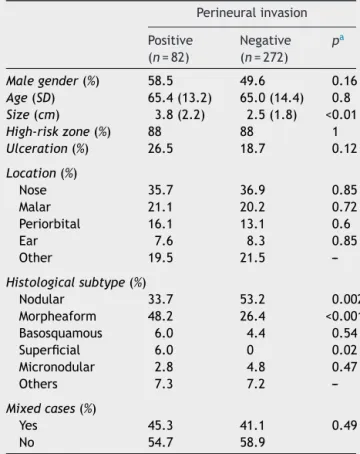
Results:Of354cases,perineuralinvasionwaspresentin23.1%.Largertumorsandmorpheaform subtypewerestatisticallyrelatedtoperineuralinvasion.Nodularandsuperficialsubtypeswere lessfrequentinpositivecases.Nosignificantdifferencewasfoundingender,age,ulceration, location,andmixedhistology.
Conclusion:Inthisseriesofselectedpatientswithbasalcellcarcinomassubmittedtomajor resections, perineural invasion was clearly related to morpheaform subtype and to larger tumors.Otherclassically associatedfeatures,suchaslocationinhigh-riskmaskzoneofthe face,malegenderandmixedhistology,werenotsostronglylinkedtoperineuralinvasion. © 2016 Associac¸˜ao Brasileira de Otorrinolaringologia e Cirurgia C´ervico-Facial. Published by Elsevier Editora Ltda. This is an open access article under the CC BY license (http:// creativecommons.org/licenses/by/4.0/).
夽
Pleasecitethisarticleas:SantosAB, AndradeNM, BrandãoLG,CerneaCR. Whichfeaturesof advancedhead andneckbasalcell carcinomaareassociatedwithperineuralinvasion?BrazJOtorhinolaryngol.2017;83:94---7.
∗Correspondingauthor.
E-mail:andrebandiera@yahoo.com.br(A.B.Santos).
PeerReviewundertheresponsibilityofAssociac¸ãoBrasileiradeOtorrinolaringologiaeCirurgiaCérvico-Facial. http://dx.doi.org/10.1016/j.bjorl.2016.01.009
Perineuralinvasioninbasalcellcarcinomas 95
PALAVRAS-CHAVE Carcinoma
basocelular; Invasãoperineural; Cabec¸aepescoc¸o
Quaiscaracterísticasdoscarcinomasbasocelularesestãoassociadosainvasão perineural?
Resumo
Introduc¸ão: Ainvasãoperineuraléumaviaindependentededisseminac¸ãotumoral.Em carci-nomasbasocelulares,aincidênciaébaixa,masaumentaemcasosavanc¸ados.Suaimportância éreconhecidamasnãocompletamentecompreendida.
Objetivo: Compararoscarcinomasbasocelularescomeseminvasãoperineural.
Método: Estudoretrospectivoderevisãodeprontuáriosdepacientessubmetidosacirurgiasde grandeporte,conduzida porequipesmultidisciplinaresemcentroterciáriodereferênciade câncer.Característicasdemográficasehistopatológicasforamanalisadas.
Resultados: De 354 casos; 23,1% apresentaram invasão perineural. Tumores com dimensão maioresubtipoesclerodermiformeforamsignificativamentemaisassociadosainvasão perineu-ral.Ossubtiposnodularesuperficialforammenosfrequentesemcasospositivos.Nãohouve diferenc¸arelacionadaasexo,idade,ulcerac¸ão,localizac¸ãoehistologiamista.
Conclusão:Nessasériedecasosselecionadosdecarcinomasbasocelularessubmetidosagrandes ressecc¸ões,ainvasãoperineuralfoiclaramenterelacionada aosubtipoesclerodermiformee tumores demaiordimensão. Outros fatores classicamenteassociados,como localizac¸ãoem zona de alto risco, sexo masculinoehistologia mistanão apresentaram essa associac¸ãode modosignificativo.
© 2016 Associac¸˜ao Brasileira de Otorrinolaringologia e Cirurgia C´ervico-Facial. Publicado por Elsevier Editora Ltda. Este ´e um artigo Open Access sob uma licenc¸a CC BY (http:// creativecommons.org/licenses/by/4.0/).
Introduction
Perineural invasion was recently recognized as a unique route of tumor spread, regardless of the lymphatic and hematogenic pathways.1 In addition, TNM staging system
included skullbase perineural invasionasa T4prognostic factorfornon-melanomaskincancer.2
Theincidenceofperineuralinvasioninbasalcell carcino-masreportedintheliteratureisusuallyunder1%,anditis generallyassociatedwithadvancedcases.3,4Incraniofacial
resections,ratesmayreach50%.5
The relationshipbetween clinicpathological character-isticsandperineuralinvasionisnotfullyunderstood.Most patients do not present with any specific symptoms, but paresthesia or pain may occur when there is gross nerve involvement.6 Skin tumors with perineural invasion were
more frequently found in male gender, in the high-risk mask zoneof theface,in largerandrecurrentlesions,as well as in aggressive subtypes such as morpheaform and basosquamous.7
Majorresectionsforbasalcellcarcinomasareoften per-formedbyamultidisciplinaryteamthatincludesaheadand neck surgery specialist. In this setting, incidence of per-ineuralinvasionisexpectedtobehigh.Thisarticlereports the18-yearexperienceofheadandnecksurgeryin a ter-tiary care referral center in São Paulo, Brazil, comparing advancedbasalcellcarcinomaswithandwithoutperineural invasion.
Methods
Themedicalchartsfrompatientssubmittedtosurgerywith head and neck surgery specialists in this institution from 1994 to2012 werereviewed. Routineevaluation included
CTscanpriortosurgery.Inallcases,generalanesthesiawas required; tumors were excised withappropriate margins, asconfirmedbyfrozensection.Reconstructionwasplanned withlocal flaps, skin grafts, or muscular or microsurgical freeflaps.
Dataon gender, age, histologicalsubtype of basal cell carcinoma, location, size, and perineural invasion were reviewed. Cases with tumors located in areas other than head and neck were excluded, aswell assmaller lesions excisedunderlocalanesthesia.
Locationwasclinicallydefinedasthecenterofthetumor, accordingtoninesubsites:scalp,frontal,ear,periorbital, nose, malar, nasolabial fold, lip, and cervical. We also classifiedtheriskassessmentareasaccordingtoNCCN rec-ommendationsforskinneoplasm,whichclassifieshighand moderate risk areas for head and neck topography.2 Size
wasmeasured after theresectionby grossanalysis ofthe specimen.
Basal cell carcinomas showing histological perineural invasion were compared with negatives cases. Statistical analysiswasperformedwithMinitab16forWindows(Minitab Inc.;StateCollege,PA,UnitedStates).Thechi-squaredtest wasused for qualitative data. Parametric variables were comparedwithStudentt-test. Statistical significance was settop<0.05.Thestudyprotocolconformedtotheethical guidelinesofthe1975DeclarationofHelsinkiasreflectedin theapprovalbytheInstitutionReviewunderNo.0228/14.
Results
96 SantosABetal.
Table 1 Demographic and histopathological features of basalcellcarcinomaswithandwithoutperineuralinvasion.
Perineuralinvasion
Positive (n=82)
Negative (n=272)
pa
Malegender(%) 58.5 49.6 0.16
Age(SD) 65.4(13.2) 65.0(14.4) 0.8
Size(cm) 3.8(2.2) 2.5(1.8) <0.01
High-riskzone(%) 88 88 1
Ulceration(%) 26.5 18.7 0.12
Location(%)
Nose 35.7 36.9 0.85 Malar 21.1 20.2 0.72 Periorbital 16.1 13.1 0.6
Ear 7.6 8.3 0.85
Other 19.5 21.5
---Histologicalsubtype(%)
Nodular 33.7 53.2 0.002 Morpheaform 48.2 26.4 <0.001 Basosquamous 6.0 4.4 0.54 Superficial 6.0 0 0.02 Micronodular 2.8 4.8 0.47 Others 7.3 7.2
---Mixedcases(%)
Yes 45.3 41.1 0.49
No 54.7 58.9
aThechi-squaredtestwasusedforallvariables,exceptage
andsize(Student’st-test).
Discussion
PerineuralinvasionwasdefinedbyBatsakisasthepresence oftumorcells in,around,andthroughthenerves.8 Itwas
onceconsideredasanangiolymphaticinvasiontothenerve sheath,9ahypothesisthatwaslaterrejected,sincethereis
nolymphaticcirculationthere.6Recently,neurotrophinsand
ligand---receptorcomplexes thateffectivelyshowa unique routeof disseminationhavebeen described.Some tumors areespeciallypronetoperineuralinvasionandthereasons arenotcompletelyunderstood.1Inheadandneckmucosal
squamous cell carcinoma, perineural invasion is an inde-pendentprognosticfactor, considered bysome authors to be an indication for postoperative radiotherapy, even in theabsenceoflymphnodemetastasis.10Nevertheless,such
indicationstillremainsacontroversialissueinadvancedskin tumors.11,12
In basal cell carcinomas,perineural invasion, although rare,is animportantprognosticfactor,13 anditisrare.3,14
Therefore, major resections that involve head and neck surgeryspecialistscomprisesaconvenientselectionofcases tostudythisparticularissue.15 Inthepresentstudy,ahigh
incidenceofperineuralinvasionwasobservedamongbasal cellcarcinomasoperatedoninatertiarycarereferral cen-ter,associatedwithmorpheaformcarcinomaandtolarger tumors.
Men are more affected in most series reporting basal cell carcinomas in general,16,17 and also in aggressive
tumorswithperineuralinvasion.7Ourresultsshoweda
non-significanthigherpreponderanceofmen.
Meanageinourseriesissimilartoothers,inwhichno difference was associated with more advanced tumors.18
Therefore, ageis probablynot associatedwith perineural invasion,asstatedbythisandotherstudies.7
Ontheotherhand,largertumorsizewasclearly associ-ated withperineural invasion.Evenin thisselectedseries ofmajorresections,averagesizealmostdoublesintumors withperineuralinvasion.Thisisconsistentwithotherseries ofbasalcellcarcinomas.7
Conversely,largersizewasclearlyassociatedwith per-ineural invasion. Even in this selected series of major resections,theaveragesizealmostdoublesintumorswith perineuralinvasion.Thisisconsistenttootherseriesofbasal cellcarcinomas.7
Acontroversialissueistherelationshipbetween perineu-ralinvasionandlocationontheheadandneck.Atleastin thepresentseries,wefoundnodifferenceeitherregarding riskzonesorspecificlocations.Nasalandmalarlocationsare themostfrequentsitesreported,butunlikeotherstudies,7
wefoundnodifferenceinfrequencyofperineuralinvasionin thedifferentsubsites.Itisnoteworthy,however,thatalmost 90%ofthetumorswerelocatedinthehigh-riskmaskzoneof thefaceinbothgroupswithpositiveandnegativeperineural invasion.
Inthepresentstudy,themostimportantfinding associ-atedwithperineuralinvasionwasthehistologicalsubtype. Nodular basal cell cancer is the most common subtype among all basal cell carcinomas,16 and fortunately it is
less frequentlyassociatedwithperineuralinvasion.In the present series, superficial basal cell carcinoma was very rare, and no case demonstrated perineural invasion, as expected.However,morpheaformsubtype,whichaccounts for only 6% of basal cell carcinomas in general, was the predominantsubtypeinalmost halfoftheperineural pos-itivecasesinthepresentseries.19 Althoughbasosquamous
subtypeisrecognizedasaggressive,20 theincidenceof
per-ineuralinvasionwasnotparticularlyhighamongtumorsof thissubtype.
Thelimitationofthisstudyistheselectionofthecases, based on the referral of patients who needed a head andneck surgeryspecialist fora multidisciplinary surgical approach. However,theactualselection mightbean indi-rectbiasforaggressivetumorsandmajorresections,helping tounderstandthemainfeaturesrelatedtoperineural inva-sion. Accordingto thisseries, perineuralinvasion is more commonlyfoundinlargertumorsandmorpheaformsubtype.
Conclusion
Perineural invasion was clearly related to morpheaform subtypeand tolargertumors.Other classicallyassociated features,suchaslocationinthehigh-riskmaskzoneofthe face,malegender,andmixedhistology,werenotsostrongly linkedtoperineuralinvasion.
Conflicts
of
interest
Perineuralinvasioninbasalcellcarcinomas 97
References
1.Liebig C, Ayala G, Wilks JA, Berger DH, Albo D. Perineu-ral invasion in cancer: a review of the literature. Cancer. 2009;115:3379---91.
2.MillerSJ,AlamM,AndersenJ,BergD,BichakjianCK,BowenG, etal.Basalcellandsquamouscellskincancers.JNatlCompr CancerNetw.2010;8:836---64.
3.Brown CI, PerryAE. Incidence of perineural invasion in his-tologically aggressive types of basal cell carcinoma. Am J Dermatopathol.2000;22:123---5.
4.WallingHW,FoskoSW,GeraminejadPA,WhitakerDC,ArpeyCJ. Aggressivebasalcell carcinoma:presentation, pathogenesis, andmanagement.CancerMetastasisRev.2004;23:389---402. 5.Cernea CR, Ferraz AR, de Castro IV, Sotto MN, Logullo AF,
BacchiCE,etal.Perineuralinvasioninaggressiveskin carcino-masoftheheadandneck.ORLJOtorhinolaryngolRelatSpec. 2009;71:21---6.
6.RatnerD,LoweL,JohnsonTM,FaderDJ.Perineuralspreadof basalcellcarcinomastreatedwithMohsmicrographicsurgery. Cancer.2000;88:1605---13.
7.LeibovitchI,HuilgolSC,SelvaD,RichardsS,PaverR.Basalcell carcinomatreatedwithMohssurgeryinAustraliaIII.Perineural invasion.JAmAcadDermatol.2005;53:458---63.
8.BatsakisJG.Nervesandneurotropiccarcinomas.AnnOtol Rhi-nolLaryngol.1985;94:426---7.
9.FeaselAM,Brown TJ, Bogle MA,Tschen JA,Nelson BR. Per-ineural invasion of cutaneous malignancies. Dermatol Surg. 2001;27:531---42.
10.PfisterDG,AngKK,BrizelDM,BurtnessBA,BussePM,Caudell JJ,etal.Headandneckcancers,Version2.2013.JNatlCompr CancerNetw.2013;11:917---23.
11.Mendenhall WM, Ferlito A, Takes RP, Bradford CR, Corry J, FaganJJ,etal.Cutaneousheadandneckbasalandsquamous
cellcarcinomaswithperineuralinvasion.OralOncol.2012;48: 918---22.
12.GeistDE,Garcia-MolinerM,FitzekMM,ChoH,RogersGS. Per-ineural invasion of cutaneous squamous cell carcinoma and basalcell carcinoma:raisingawareness and optimizing man-agement.DermatolSurg.2008;34:1642---51.
13.BalamuckiCJ, MancusoAA, AmdurRJ,KirwanJM,Morris CG, FlowersFP,et al.Skincarcinomaoftheheadand neckwith perineuralinvasion.AmJOtolaryngol.2012;33:447---54. 14.Bechert CJ, Stern JB. Basal cell carcinoma with
perineu-ral invasion:reexcision perineural invasion? J Cutan Pathol. 2010;37:376---9.
15.AndradeNM,SantosAB,LourencoSV,NetoCF,CerneaCR, Bran-dao LG.Epidemiological and histopathological profileof642 cases ofbasalcell carcinomaof headand necksurgery ina tertiaryinstitution.SaoPaulo:RevBrasCirCabPesc;2011.p. 148---53.
16.BastiaensMT,HoefnagelJJ,BruijnJA,WestendorpRG,Vermeer BJ,BouwesBavinckJN.Differences inage,site distribution, and sex between nodular and superficial basal cell carci-noma indicate differenttypesof tumors. JInvestDermatol. 1998;110:880---4.
17.StaplesMP,ElwoodM,BurtonRC,WilliamsJL,MarksR,Giles GG.Non-melanomaskincancerinAustralia:the2002national surveyandtrendssince1985.MedJAust.2006;184:6---10. 18.Blixt E, Nelsen D, Stratman E. Recurrence rates of
aggres-sivehistologictypesofbasalcell carcinoma aftertreatment withelectrodesiccation andcurettage alone.Dermatol Surg. 2013;39:719---25.
19.ScrivenerY,GrosshansE,CribierB.Variationsofbasalcell carci-nomasaccordingtogender,age,locationandhistopathological subtype.BrJDermatol.2002;147:41---7.