REVISTA
BRASILEIRA
DE
ANESTESIOLOGIA
OfficialPublicationoftheBrazilianSocietyofAnesthesiologywww.sba.com.br
SCIENTIFIC
ARTICLE
Ultrasound
guidance
improves
the
success
rate
of
axillary
plexus
block:
a
meta-analysis
Qin
Qin
a,
Debao
Yang
b,
Hong
Xie
a,
Liyuan
Zhang
c,
Chen
Wang
a,∗aDepartmentofAnesthesiologyandCriticalCare,TheSecondAffiliateHospitalofSoochowUniversity,Suzhou,JiangsuProvince,
People’sRepublicofChina
bDepartmentofNeurosurgery,KowloonHospital,ShanghaiJiaotongUniversitySchoolofMedicine,Suzhou,JiangsuProvince,
People’sRepublicofChina
cDepartmentofRadiotherapy,TheSecondAffiliateHospitalofSoochowUniversity,Suzhou,JiangsuProvince,People’sRepublic
ofChina
Received8December2014;accepted27January2015 Availableonline1October2015
KEYWORDS
Meta-analysis; Brachialplexusblock; Ultrasonography
Abstract
Objective: Toevaluatethevalue ofreal-timeultrasound(US)guidancefor axillarybrachial plexusblock(AXB)throughthesuccessrateandtheonsettime.
Methods:The meta-analysis was carried outin the Anesthesiology Departmentof the Sec-ond AffiliatedHospitalofSoochow University, Suzhou,Jiangsu Province,China. A literature searchofMedline,EMBASE,Cochranedatabasefromtheyears2004to2014wasperformed. Theliteraturesearcheswerecarriedoutusingmedicalsubjectheadingsandfree-textword: ‘‘axilla’’, ‘‘axillary’’,‘‘brachialplexus’’,‘‘ultrasonography’’,‘‘ultrasound’’,‘‘ultrasonics’’. Twodifferentreviewerscarriedoutthesearchandevaluatedstudiesindependently.
Results:Sevenrandomizedcontrolledtrials,onecohortstudyandthreeretrospectivestudies were included.Atotal of2042patientswereidentified.1157patientsunderwent AXBusing US guidance (USgroup)and thecontrolled group included885patients (246patients using traditionalapproach(TRAD)and639patientsusingnervestimulation(NS)).Ouranalysisshowed thatthesuccessratewashigherintheUSgroupcomparedtothecontrolledgroup(90.64%vs. 82.21%,p<0.00001).Theaveragetimetoperformtheblockandtheonsetofsensorytimewere shorterintheUSgroupthanthecontrolledgroup.
Conclusion: Thepresentstudydemonstratedthatthereal-timeultrasoundguidanceforaxillary brachialplexusblockimprovesthesuccessrateandreducethemeantimetoonsetofanesthesia andthetimeofblockperformance.
© 2015SociedadeBrasileirade Anestesiologia.Publishedby ElsevierEditoraLtda.Allrights reserved.
∗Correspondingauthor.
E-mail:doubleqq@126.com(C.Wang). http://dx.doi.org/10.1016/j.bjane.2015.01.002
PALAVRAS-CHAVE
Metanálise; Bloqueiodoplexo braquial;
Ultrassonografia
Orientac¸ãoporultrassommelhoraataxadesucessodobloqueiodoplexoaxilar:uma metanálise
Resumo
Objetivo:Avaliarovalordaorientac¸ãoporultrassonografia(US)emtemporealparabloqueio doplexobraquialporviaaxilar(BPBA)pelataxadesucessoetempodelatência.
Métodos: UmametanálisefoirealizadanoDepartamentodeAnestesiologiadoSegundoHospital AfiliadodaUniversidadedeSoochow,Suzhou,provínciadeJiangsu,China.Fizemosumapesquisa bibliográficanasbasesdedadosMedline,EMBASAeCochranede2004a2014.Apesquisafoi realizadausandotítulosdeassuntosmédicosepalavrasdetextolivre:axilla,axillary,brachial plexus,ultrasonography,ultrasound,ultrasonics.Doisrevisoresdiferentesfizeramapesquisa eavaliaramosestudosdeformaindependente.
Resultados: Seteestudosclínicosrandômicos,umestudodecoorteetrêsestudosretrospectivos foramincluídos.Foiidentificadoumtotalde2.042pacientes,dosquais1.157foramsubmetidos ao BPBAguiadoporultrassom(grupoUS);ogrupocontroleincluiu885pacientes,dos quais 246 foramsubmetidos àabordagem tradicional (TRAD) e639 àestimulac¸ãodo nervo(EN). Nossaanálisemostrou quea taxadesucesso foimaior nogrupoUS em comparac¸ãocomo grupocontrole(90,64%vs.82,21%,p<0,00001).Asmédiasdotemponecessáriopararealizaro bloqueioedotempodelatênciaforammaiscurtasnogrupoUSquenogrupocontrole. Conclusão:Opresenteestudodemonstrouqueaorientac¸ãoporultrassomemtemporealpara obloqueiodoplexobraquialporviaaxilarmelhoraataxadesucessoereduzamédiadotempo deiníciodaanestesiaedotempodeexecuc¸ãodobloqueio.
©2015SociedadeBrasileiradeAnestesiologia.PublicadoporElsevierEditoraLtda.Todosos direitosreservados.
Introduction
Inrecentyears,thepeoplepaidmoreandmoreattentions onthelocalanesthesia,especiallyonperipheralnerveblock technique.1,2 The traditional nerve block needs the help
of anatomical landmarks, the arterial pulse, needling of abnormalsensationornervestimulator,but,withtherapid developmentoftechnologyofultrasounddevice,underthe guidance of ultrasound nerve block anesthesia as a new fieldofanultrasonicapplicationsaregraduallybeingretired by the attention, ultrasonic technology is a fundamental change in theway nerveblock. Brachial plexus block are themostcommonmethodsusedinperipheralnerveblock. Peripheral nerve stimulation may have a high degree of accuracy and reliability for the axillary nerve block, but sometimes cause failure or incomplete block, even when tookmultiplestimulationandinjection.3,4
Anesthesiologistshavebeenabletoobservethebrachial plexus and the surrounding structures through the ultra-soundguidedpuncture.5Soanesthesiologistscanpuncture
intothe targetperipheralnerveaccuratelywithreal-time ultrasound.Theinjectionprocessandthediffusionrangeof localanestheticscanalsobeobservedbyultrasonography. Thetechnologyensuredthelocalanestheticevenlyspread toperipheral nerve,make localanestheticsfullyinfiltrate thenerve,significantlyimprovethesuccessrateandreduce thecomplications.
Methods
Searchstrategy
The meta-analysis was carried out in the Anesthesiology Department of the Second Affiliated Hospital of Soochow
University, Suzhou, Jiangsu Province, China. A literature search of Medline, EMBASE, Cochrane database from the years2004to2014wasperformed.Theliteraturesearches were carried out using medical subject headings and free-text word: ‘‘axilla’’, ‘‘axillary’’, ‘‘brachial plexus’’, ‘‘ultrasonography’’,‘‘ultrasound’’,‘‘ultrasonics’’.Two dif-ferent reviewers carried out the search and evaluated studiesindependently.
Inclusioncriterion
All randomized, non-randomized controlled clinical trials, which compared ultrasound-guided AXB with traditional approachorperipheralnervestimulationincluded.
Exclusioncriterion
Abstracts,letters,casereports,comments,andconference proceedings werenot included in the review.We exclude studieswithsmall-sizedgroup(<40patients).
Datecollection
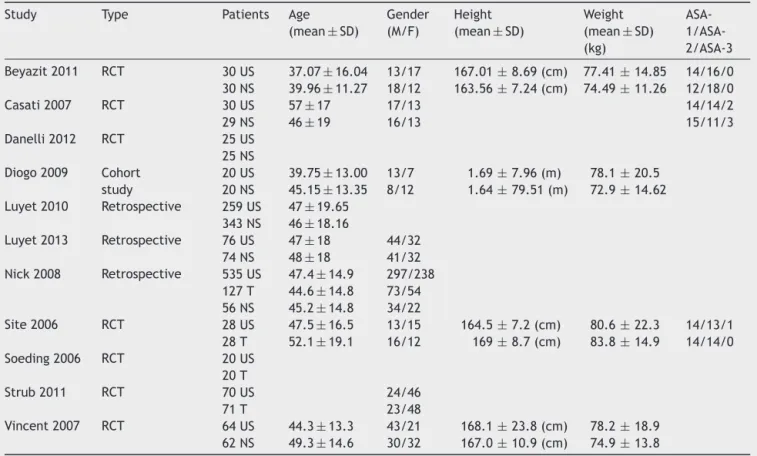
Table1 Summaryofpublishedinformationfromcontrolledstudies.RCT,randomizedcontrolledtrials.
Study Type Patients Age (mean±SD)
Gender (M/F)
Height (mean±SD)
Weight (mean±SD) (kg)
ASA- 1/ASA-2/ASA-3
Beyazit2011 RCT 30US 37.07±16.04 13/17 167.01±8.69(cm) 77.41±14.85 14/16/0 30NS 39.96±11.27 18/12 163.56±7.24(cm) 74.49±11.26 12/18/0
Casati2007 RCT 30US 57±17 17/13 14/14/2
29NS 46±19 16/13 15/11/3
Danelli2012 RCT 25US 25NS Diogo2009 Cohort
study
20US 39.75±13.00 13/7 1.69±7.96(m) 78.1±20.5 20NS 45.15±13.35 8/12 1.64±79.51(m) 72.9±14.62 Luyet2010 Retrospective 259US 47±19.65
343NS 46±18.16
Luyet2013 Retrospective 76US 47±18 44/32 74NS 48±18 41/32 Nick2008 Retrospective 535US 47.4±14.9 297/238
127T 44.6±14.8 73/54 56NS 45.2±14.8 34/22
Site2006 RCT 28US 47.5±16.5 13/15 164.5±7.2(cm) 80.6±22.3 14/13/1 28T 52.1±19.1 16/12 169±8.7(cm) 83.8±14.9 14/14/0 Soeding2006 RCT 20US
20T
Strub2011 RCT 70US 24/46
71T 23/48
Vincent2007 RCT 64US 44.3±13.3 43/21 168.1±23.8(cm) 78.2±18.9 62NS 49.3±14.6 30/32 167.0±10.9(cm) 74.9±13.8
Statisticalanalysis
We used Review Manager 5.2 toconduct the review. The Mantel---Haenszelmethodwasusedforthestatistical analy-sisofthesuccessrate,themeantimetoonsetofanesthesia and the time of block performance. Dichotomous data were analyzed for odds ratio (OR) and 95% effectiveness confidence interval. p≤0.05 was considered statistically significant.
Results
Sevenrandomized controlledtrials, onecohort study and three retrospective studies were included (Table 1).4,6---15
Our analysis showed that the success rate was higher in the US group compared to the controlled group (90.64% vs.82.21%,total1992patients;Heterogeneity:Chi2=15.17;
p<0.00001;I2=47%;OR:0.50;95%CI[0.38,0.65])(Fig.1).
The average time to perform the block is shorter in the
The control group
The control group
0.01 0.1 1 10 100
Study or Subgroup
Total (95% CI) Total events
Test for overall effect: Z=4.98 (P<.00001) Heterogeneity: Chi2=15.17, df=8 (P=.06); I2=47%
707 1026
860 1132 100.0% 0.50 [0.38, 0.65]
Beyazit 2011 Casati 2007 Diogo 2009 Luyet 2010 Luyet 2013 Nick 2008 Site 2006 Soeding 2005 Strub 2011 Vincent 2007
26 29 19 274 69 148 20 18 51 53
30 29 20 343 74 183 28 20 71 62
30 30 19 230 66 490 28 19 52 62
30 30 20 259 76 535 28 20 70 64
3.1%
0.7% 36.6% 3.1% 33.1% 5.8% 1.3% 10.2% 6.1%
0.10 [0.00, 1.88] Not estimable 1.00 [0.06, 17.18] 0.50 [0.31, 0.80] 2.09 [0.68, 6.44] 0.39 [0.24, 0.63] 0.04 [0.00, 0.78] 0.47 [0.04, 5.69] 0.88 [0.42, 1.86] 0.19 [0.04, 0.92]
The US group
The US group
Weight Total
Total Events Events
Odds ratio M-H, Fixed, 95% CI
Odds ratio M-H, Fixed, 95% CI
The control group
The control group
–100 –50 0 50 100
Study or Subgroup
Total (95% CI)
Test for overall effect: Z=9.83 (P<.00001)
Heterogeneity: Chi2=167.57, df=6 (P<.00001); I2=96%
689 1017 100.0% 3.88 [3.11, 4.65]
Beyazit 2011 Danelli 2012 Luyet 2010 Luyet 2013 Nick 2008 Site 2006 Vincent 2007 6.4 8 35 20.1 40.1 11.1 11.2 3.9 5 13 9 27.3 5.7 4.2 30 25 343 74 127 28 62 7.3 5 22 21.7 30.6 7.9 9.3 2.6 3 8 11.4 14.2 3.9 4 30 25 259 76 535 28 64 21.1% 11.4% 21.0% 5.5% 2.5% 9.1% 29.1%
–0.90 [–2.58, 0.78] 3.00 [0.71, 5.29] 13.00 [11.31, 14.69] –1.60 [–4.88, 1.68] 9.50 [4.60, 14.40] 3.20 [0.64, 5.76] 1.90 [0.47, 3.33]
The US group
The US group
SD Total Weight Mean
SD Mean Total
Mean difference IV. Fixed, 95% CI
Mean difference IV. Fixed, 95% CI
Figure2 AnalysisofcontrolledstudiesforperformancetimeofAXB:withoutultrasoundguidancevs.ultrasoundguidanceinthe patientswithAXB.95%CI,95%confidenceinterval;M-H,Mantel---Haenszel;df,degreesoffreedom;OR,oddsratio;US,ultrasound.
The control group
The control group
–100 –50 0 50 100
Study or Subgroup
Casati 2007 Danelli 2012 18 18 6 7 29 25 14 15 6 9 30 25 68.1% 31.9%
4.00 [0.94, 7.06] 3.00 [–1.47, 7.47]
Total (95% CI)
Test for overall effect: Z=2.86 (P=.004) Heterogeneity: Chi2=0.13, df=1 (P=.72); I2=0%
54 55 100.0% 3.68 [1.15, 6.21] The US group
The US group
SD Total Weight Mean
SD Mean Total
Mean difference IV. Fixed, 95% CI
Mean difference IV. Fixed, 95% CI
Figure3 AnalysisofcontrolledstudiesforonsettimeofAXB:withoutultrasoundguidancevs.ultrasoundguidanceinthepatients withAXB.95%CI,95%confidenceinterval;M-H,Mantel---Haenszel;df,degreesoffreedom;OR,oddsratio;US,ultrasound.
US group than the controlled group (total 1706 patients; Heterogeneity:Chi2=167.57,p<0.00001;I2=96%;OR:3.88;
95%CI[3.11, 4.65])(Fig.2).The onsetof sensorytimeis alsoshorterintheUSgroupthanthecontrolledgroup(total 109patients; Heterogeneity:Chi2=0.13, p=0.004;I2=0%;
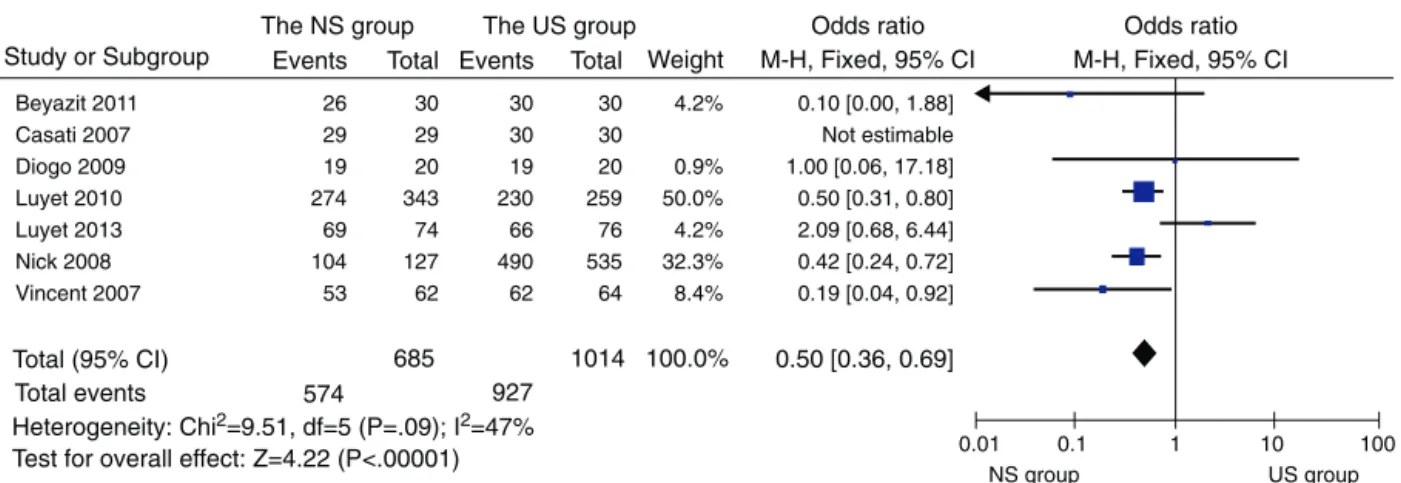
OR:3.68;95%CI[1.15,6.21])(Fig.3).Thedataanalysisof subgroup showed that the success rate washigher in the US group compared to the NS group (91.42% vs. 83.80%, total1699patients;Heterogeneity:Chi2=9.51,p<0.0001;
I2=47%;OR:0.50;95%CI[0.36,0.69])(Fig.4).
Discussion
Axillarybrachialplexusblockis applicabletooperationof elbow and on the lower part of elbow, can prevent the tourniquetpain,alsocanincreasethebloodflowofupper limb.16---18Axillarybrachialplexuscanblockincludingmedian
nerve,ulnar nerve,musculocutaneous nerve,radialnerve and all terminal branch. Musculocutaneous nerve is usu-ally issued from axillary Fasciculus lateralis, so the AXB is often incomplete. The nerve stimulatorand ultrasound
The NS group
NS group
0.01 0.1 1 10 100
Study or Subgroup
Total (95% CI) Total events
Test for overall effect: Z=4.22 (P<.00001) Heterogeneity: Chi2=9.51, df=5 (P=.09); I2=47%
574 927
685 1014 100.0% 0.50 [0.36, 0.69]
Beyazit 2011 Casati 2007 Diogo 2009 Luyet 2010 Luyet 2013 Nick 2008 Vincent 2007 26 29 19 274 69 104 53 30 29 20 343 74 127 62 30 30 19 230 66 490 62 30 30 20 259 76 535 64 4.2% 0.9% 50.0% 4.2% 32.3% 8.4%
0.10 [0.00, 1.88] Not estimable 1.00 [0.06, 17.18] 0.50 [0.31, 0.80] 2.09 [0.68, 6.44] 0.42 [0.24, 0.72] 0.19 [0.04, 0.92]
The US group
US group Weight Total Total Events Events Odds ratio M-H, Fixed, 95% CI
Odds ratio M-H, Fixed, 95% CI
guided axillary brachialplexus block significantly improve thesuccessrate.
Although the nervestimulator could be able tolocate thetargetnerve,but becausetheinjectionoflocal anes-theticnervehadnoideatoguaranteeencasedcompletely, sothenervestimulatorblockhas10---15% failurerate.19,20
Ultrasonic monitoring can ensure that after the injection ofdrug,thenervebundlewassurroundingandinfiltrating, therebyimprovingtheaxillarybrachialplexusblocksuccess rate.However,thedifferentlevelsof anesthesiaoperator maynotfullybeabletodistinguisheachnerveinultrasound images.Especiallytheradialnerveweredifficulttolocate, andisoftenconfusedwithaxillaryarteryofposteriorwall.21
The depth of insertion of the needle and the dura-tion of axillary block placemen may affect the pain intensity.4,13,22,23PatientswhogetAXBwithultrasound(US)
guidancewerelesspainfulandmorecomfortablethanthe patientsgetAXBwithneurostimulation.24 Itwassuggested
thatultrasoundrequestedlessnumberofneedlepassesthan neurostimualtion.7
In conclusion,ultrasound guidancefor axillary brachial plexusblockimprovedthesuccess rateanddecreased the performancetimeand onsettime.Thevisualization tech-nologygreatlyreducedthepossibilityofoccurrenceoferror, suchasperforatingvesselsandlocalanestheticspoisoning andimprovedthesafety.Soitistheidealoptionforupper limboperation.
Conflicts
of
interest
Theauthorsdeclarenoconflictsofinterest.
Acknowledgements
ThisworkissupportedbyGrantNo.SZD0613(toDr.Wang) from the Technology Bureau of Suzhou, China. Dr. Wang alsoreceivedsupportfromtheRevitalizingtheKeyTalent’s SubsidyProjectinScienceandEducation(JiangsuProvince, China).
References
1.GritsenkoK,KhelemskyY,KayeAD,etal.Multimodaltherapy inperioperative analgesia. Best PractRes ClinAnaesthesiol. 2014;28:59---79.
2.LiuSS, StrodtbeckWM, RichmanJM,et al. Acomparison of regionalversusgeneralanesthesiaforambulatoryanesthesia: ameta-analysisofrandomizedcontrolledtrials.AnesthAnalg. 2005;101:1634---42.
3.RodríguezJ,TaboadaM,DelRíoS,etal.Acomparisonoffour stimulation patternsin axillaryblock. Reg Anesth Pain Med. 2005;30:324---8.
4.ChanVW,PerlasA, McCartneyCJ,etal.Ultrasoundguidance improvessuccessrateofaxillarybrachialplexusblock.CanJ Anaesth.2007;54:176---82.
5.RanganathA,SrinivasanKK,IohomG.Ultrasoundguidedaxillary brachialplexusblock.MedUltrason.2014;16:246---51. 6.ZencirciB.Comparisonofnervestimulatorandultrasonography
asthetechniquesappliedfor brachial plexusanesthesia.Int ArchMed.2011;21:1---4.
7.CasatiA, Danelli G, Baciarello M, et al.A prospective, ran-domizedcomparisonbetweenultrasoundandnervestimulation guidanceformultipleinjectionaxillarybrachialplexusblock. Anesthesiology.2007;106:992---6.
8.Danelli G, Bonarelli S, Tognú A, et al. Prospective random-ized comparison of ultrasound-guided and neurostimulation techniques for continuousinterscalene brachial plexus block in patients undergoing coracoacromial ligament repair. Br J Anaesth.2012;108:1006---10.
9.Conceic¸ão DB, Helayel PE, de Oliveira Filho GR. A compar-ativestudybetween ultrasoundand neurostimulationguided axillarybrachial plexusblock. Rev BrasAnestesiol. 2009;59: 585---91.
10.LuyetC,SchüpferG,WipfliM,etal.Differentlearningcurves foraxillarybrachialplexusblock:ultrasoundguidanceversus nervestimulation.AnesthesiolResPract.2010:1---7.
11.LuyetC,ConstantinescuM,WaltenspülM,etal.Transitionfrom nerve stimulator to sonographically guided axillary brachial plexus anesthesiain handsurgery: blockqualityand patient satisfaction during the transition period. J Ultrasound Med. 2013;32:779---86.
12.LoN,BrullR, PerlasA,etal.Evolutionofultrasoundguided axillarybrachialplexusblockade:retrospectiveanalysisof662 blocks.CanJAnaesth.2008;55:408---13.
13.Sites BD, Beach ML, Spence BC, et al. Ultrasound guidance improvesthesuccessrateofaperivascularaxillaryplexusblock. ActaAnaesthesiolScand.2006;50:678---84.
14.SoedingPE,ShaS,RoyseCE,etal.Arandomizedtrialof ultra-soundguidedbrachialplexusanaesthesiainupperlimbsurgery. AnaesthIntensiveCare.2005;33:719---25.
15.Strub B.Whatbenefits doesultrasound-guided axillaryblock for brachial plexus anaesthesia offer over the conventional blindapproachinhandsurgery.TheJournalofHandSurgery. 2011;36:778---86.
16.LoMonteAI,DamianoG,MularoA,etal.Comparisonbetween localandregionalanesthesiainarteriovenousfistulacreation. JVaseAccess.2011;12:331---5.
17.lskandar H, Wakim N, Benard A, et al. The effects of interscalene brachialPlexus blockonhumeral arterialblood flow: a Doppler Ultrasound study. Anesth Analg. 2005;101: 279---81.
18.ShemeshD,OlshaO,OrkinD,etal.Sympathectomylikeeffects ofbrachialplexusblockinarteriovenousaccesssurgery. Ultra-soundMedBiol.2006;32:817---22.
19.AbrahamsMS,AzizMF,FuRF,etal.Ultrasoundguidance com-pared with electrical neurostimulation for peripheral nerve block: asystematic reviewand meta-analysis ofrandomized controlledtrials.BrJAnaesth.2009;102:408---17.
20.Liu FC, Liou JT, Tsai YF. Efficacy of ultrasound guided axil-lary brachial plexus block: a comparative study with nerve stimulator-guidedmethod.ChangGungMed.2005;28:396---402. 21.Marhofer P, Chan VW. Ultrasound guided regional anesthe-sia: current concepts and future trends. Pulesth Analg. 2007;104:1265---9.
22.Koscielniak-NielsenZJ,RasmussenH,NielsenPT.Patients’ per-ceptionofpainduringaxillaryandhumeralblocksusingmultiple nervestimulations.RegAnesthPainMed.2004;29:328---32. 23.Schwemmer U, Schleppers A, Markus C, et al. Operative
management in axillary brachial plexus blocks: comparison of ultrasound and nerve stimulation. Anaesthesist. 2006;55: 451---6.