www.bjorl.org
Brazilian
Journal
of
OTORHINOLARYNGOLOGY
ORIGINAL
ARTICLE
Human
Papillomavirus
and
students
in
Brazil:
an
assessment
of
knowledge
of
a
common
infection
---
preliminary
report
夽
João
Cesar
Frizzo
Burlamaqui
a,
Ana
Carolina
Cassanti
a,
Gabriela
Bastos
Borim
a,
Edward
Damrose
b,
Luisa
Lina
Villa
c,
Leonardo
Silva
a,∗aFaculdadedeCiênciasMédicasdaSantaCasadeSãoPaulo,SãoPaulo,SP,Brazil bStanfordUniversity,California,USA
cUniversidadedeSãoPaulo(USP),FaculdadedeMedicina,DepartamentodeRadiologiaeOncologia,SãoPaulo,SP,Brazil
Received23January2016;accepted2February2016 Availableonline22April2016
KEYWORDS
Brazil; Viruses;
Sexualbehavior; Policy
Abstract
Introduction:HumanPapillomavirus(HPV)infectionisthemostprevalentsexuallytransmitted diseaseworldwide.Oneofthebarrierstotheimplementationofpreventionprogramsagainst thediseaseisthelimitedknowledgepossessedbymostpopulationsregardingthevirusandits possibleconsequences.
Objective:ThepurposeofthisstudywastoevaluatetheknowledgeofBraziliancollegestudents ontransmission,clinicalmanifestations,anddiseasescorrelatedwithHPV,highlightingthepoor knowledgeofaverycommoninfection.
Methods:Atotalof194studentsansweredaquestionnaireabouttransmission,clinicalfeatures andthepossibleconsequencesofpersistentHPVinfection.Thequestionnairewasself-applied underthesupervisionoftheauthors.
Results:TheclinicalmanifestationsofHPVinfectionwerenotcleartomoststudents.Incorrect assumptionsoftheclinicalmanifestationsofHPVinfectionincluded:bleeding(25%),pain(37%) andrashes(22%).TwelvepercentofrespondentsdidnotrecognizewartsasanHPV-related disease.Regardingpotentialconsequencesofpersistentinfection,studentsdidnotrecognizea relationshipbetweenHPVandlaryngealcarcinoma(80.9%),pharyngealcarcinoma(78.9%),anal carcinoma(73.2%),vulvarcarcinoma(65.4%)andvaginalcarcinoma(54.6%).Largeportionsof thepopulationevaluatedwereunawareofmodesofHPVtransmissionbeyondgenitalcontact.
夽 Pleasecitethisarticleas:BurlamaquiJC,CassantiAC,BorimGB,DamroseE,VillaLL,SilvaL.HumanPapillomavirusandstudentsin
Brazil:anassessmentofknowledgeofacommoninfection-preliminaryreport.BrazJOtorhinolaryngol.2017;83:120---5.
∗Correspondingauthor.
E-mail:leosilva@uol.com.br(L.Silva).
PeerReviewundertheresponsibilityofAssociac¸ãoBrasileiradeOtorrinolaringologiaeCirurgiaCérvico-Facial.
http://dx.doi.org/10.1016/j.bjorl.2016.02.006
Conclusion: KnowledgeofHPVby thepopulationevaluated inthisstudy ispartialand frag-mented.Lackofknowledgemaycontributetothefurtherspreadofthedisease.Publichealth policiesforeducationandguidanceofthepopulationshouldbeimplementedinBrazil. © 2017 Associac¸˜ao Brasileira de Otorrinolaringologia e Cirurgia C´ervico-Facial. Published by Elsevier Editora Ltda. This is an open access article under the CC BY license (http://
creativecommons.org/licenses/by/4.0/).
PALAVRAS-CHAVE
Brasil; Vírus;
Comportamento sexual;
Política
HPVeestudantesnoBrasil:avaliac¸ãodoconhecimentodeumainfecc¸ão comum---relatopreliminar
Resumo
Introduc¸ão: Ainfecc¸ãopelopapilomavírushumano(HPV)éadoenc¸asexualmentetransmissível maisprevalenteemtodoomundo.Umadasbarreirasparaaimplementac¸ãodeprogramasde prevenc¸ãocontraadoenc¸aéoconhecimentolimitadodamaioriadaspopulac¸õessobreovírus esuaspossíveisconsequências.
Objetivo: Oobjetivo desteestudo foi avaliaroconhecimento dosestudantes universitários brasileirossobreatransmissão,manifestac¸õesclínicasedoenc¸ascorrelacionadascomoHPV, comdestaqueparaopoucoconhecimentodeumainfecc¸ãomuitocomum.
Método: Umtotalde194estudantesrespondeuaumquestionáriosobreatransmissão, carac-terísticasclínicaseaspossíveisconsequênciasdainfecc¸ãopersistentepeloHPV.Oquestionário foiautoaplicado,sobasupervisãodosautores.
Resultados: Asmanifestac¸õesclínicasdainfecc¸ãopeloHPVnãoeramclarasparaamaioriados estudantes.Assuposic¸õesincorretasdasmanifestac¸õesclínicasdainfecc¸ãopeloHPVincluíam: hemorragia (25%),dor(37%) eerupc¸õescutâneas(22%)— 12%dosentrevistados não recon-heciamasverrugascomoumadoenc¸arelacionadaaoHPV.Quantoàspotenciaisconsequências dainfecc¸ãopersistente,osalunosnãoreconheciamumarelac¸ãoentreHPVecâncerdelaringe (80,9%),carcinomadafaringe(78,9%),carcinomaanal(73,2%),carcinomavulvar(65,4%)e car-cinoma vaginal(54,6%). Grandesporc¸ões dapopulac¸ãoavaliada desconheciamos modosde transmissãodoHPValémdocontatogenital.
Conclusão:OconhecimentodeHPVpelapopulac¸ãoavaliadanesteestudoéparciale fragmen-tado.Afaltadeconhecimentopodecontribuirparaapropagac¸ãodadoenc¸a.Políticaspúblicas desaúdeparaaeducac¸ãoeorientac¸ãodapopulac¸ãodevemserimplementadasnoBrasil. © 2017 Associac¸˜ao Brasileira de Otorrinolaringologia e Cirurgia C´ervico-Facial. Publicado por Elsevier Editora Ltda. Este ´e um artigo Open Access sob uma licenc¸a CC BY (http://
creativecommons.org/licenses/by/4.0/).
Introduction
HumanPapillomavirus(HPV)istheetiologicalagentofthe mostcommonviralinfectionofthegenitaltractworldwide. The virus is also related to a wide range of disorders in children and adults of both genders. The clinical impact ofHPV-relateddiseaseencompassesarangeofbenignand malignantdisorders.1
HPVinfectionisthemostprevalentsexuallytransmitted diseaseworldwide,withover14millionnewcasesreported intheUnitedStatesin2008.Takingintoaccountallinfected individuals,itisestimatedthatabout79millionAmericans wereinfectedwithHPVin2008.2
The human papillomavirusis aDNA virus of the Papil-lomaviridaefamily.HPVinfectsskinandmucosa.Basedon differencesinthegenomicsequenceofL1,thegene encod-ingthemajorcapsidprotein,morethan190typesofHPV havebeenidentifiedbymolecularanalysis.3
HPV is classified into high- and low-risk types accord-ingtotheirpotentialtoinducecancerininfectedtissues.1 Although sexual contact is the most widely accepted
mode of transmission, other forms of contamination are described in the literature.4 Vertical transmission (infec-tion of infants by passage through a contaminated birth canal) is 231 times higher in women with vaginal/vulvar condyloma than in women without clinically evident dis-ease.TransmissionofHPVthroughsubclinicalinfectionmay alsobeanimportantmodeofinfection,perhapsthe high-est risk factor when studying maternal-fetal transmission rate.5
TheclinicalmanifestationsofHPV-relateddiseasesvary dependingupon theHPV typeandthesite ofinoculation, but the wart is considered the classic primary lesion of infection.6
Whilepersistentinfectioninthecervixbyhigh-riskHPV (16and18)haslongbeenconsideredthecausativefactorin cervicalanduterinecancer, ithasbeenonlyrecently rec-ognizedthatthissame processaccountsforcancer ofthe anus,penis,vagina,vulvaandoropharynx.7,8
Consideringthe high prevalence of HPV-associated dis-ease and its potential for recurrence and malignant conversion,costsrelatedtodiagnosis andtreatment have amajorimpactonhealthsystemsworldwide.Forexample, in2003alonethe UnitedStatesspent$418million dollars for the treatment of HPV-related diseases, excluding the amountsspentoncervicaldisease.10
In 2012, the Italian health system spent 528.6 million Euros for the treatment of HPV-related diseases (cervical cancer,vulvarcancer, vagina,anus,penis,headandneck, genitalwartsandrespiratorypapillomatosis).11
Inadditiontotheextremelyhighcostsforhealthsystems worldwide,HPV-related diseases are associated withhigh ratesofmorbidityandmortality.12
Aswithothersexuallytransmitteddiseases,prevention remainsthebestoptionforcontrollingHPV-relateddiseases, particularlysince thereis nocurative treatment.9 Among thedifferentformsofpreventionavailableforHPV-related diseases,vaccination hasdemonstrated cost-effectiveness inseveralprogramsaroundtheworld.9
However,oneof thebarriers tothe implementationof theseprogramsisthelimitedknowledgepossessedbymost populations13---16 regardingthevirus anditspossible conse-quences.
Studies in different partsof the world have identified thatthereisnotaproperunderstandingofthetopicwhen consideringsexuallyactiveyoungpeople.17---19
Positively, countriesthat have implemented immuniza-tion programs have observed that vaccination campaigns have contributed to increasing levels of awareness of the issue. These campaigns, however, have been primarily focused on cervical cancer, while the infor-mation provided about other HPV-related diseases is limited.20
Although the scientific literature provides strong evi-denceabouttherelationshipbetweeninfectionbyhigh-risk HPV and the development of oropharyngeal cancer pop-ular knowledge regarding this tumor is inadequate or inexistent.21
In a study of 2.126 American adultsevaluating overall knowledgeofhead andneckcancers,lessthan1%of par-ticipantsrecognizedHPVinfectionasapossibleriskfactor forcancerofthemouthandpharynx.22
Interestingly, thereis a 10-folddifferencein the rates of oral infection (4%) andgenital infection (40%)in men. Despite relatively low infection rates, development of benignandmalignantlesionsintheheadandneckis increas-ingatanalarmingrate.23
Sexualbehaviorhasbeenrelatedtotheincreasingrate oforalHPVinfection,butthereisnoconsensusinthe litera-tureonthesubject.Riskfactorsmayincludethenumberof lifetimesexualpartnersandtheincreasingpracticeoforal sex.24,25
Subclinicalinfectionmayfacilitatedisseminationof dis-easetouninfectedpartners.Condomuseshouldalwaysbe encouraged but may not provide total protection against HPVinfectionbecausethevirusmaybeshedfromsitesnot protectedbythecondom.26
The purposeof thisstudy wastoevaluate thelevel of knowledgeofcollege studentsonissuesinvolved in trans-mission ofthe virus, clinical manifestations andpotential consequencesofpersistentHPVinfections,identifyinggaps
in knowledge and thus contributing to educational cam-paigns.
Methods
This cross-sectionalstudy wasapprovedbythe Ethicsand ResearchCommittee(CAAE:20424413.4.0000.5479).Three hundred students of the first two years of the schools of Medicine, Nursing and Speech-Language Pathology and Audiologywereinvitedtoparticipateinthisstudy.The ques-tionnairewasself-appliedandthesubjectswereorganized intogroupsinordertominimizeinterferencewiththe cur-riculumofeachofthecolleges.Theauthorssupervisedthe completionof the questionnaires.Each questionnairewas identified only by number for the purpose of maintaining theanonymityofeachparticipant.
Results
Ofthe300studentsinvitedtoparticipateinthestudy,194 agreed to participate and fully completed the question-naires.Noquestionnairewasexcluded.
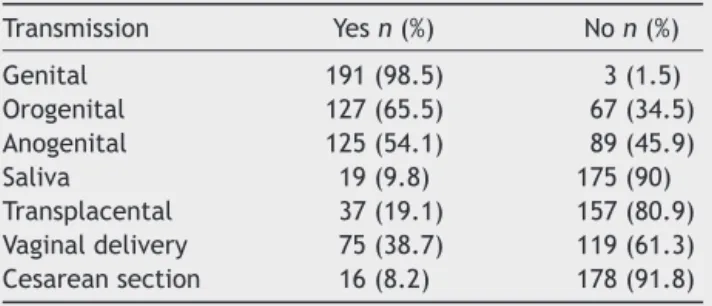
Mostofthesubjects(92.8%)correctlyindicatedthatthe greaterthenumberofsexualpartnersthehighertheriskof HPVinfection.Resultsregardingtransmissionaredisplayed in Table1.Mostrespondentsrecognizedgenitaltogenital contact as a common mode of transmission, but knowl-edge regarding other modes of transmission was limited. Mostrespondentsunderestimatedtheriskofmaternal-fetal transmission.
Regarding protective measures, 51% of participants stated thatcondomsprovide total protectionagainst HPV infectionduringsexualintercourse,12.4%couldnotanswer thisquestionand36.6%reportedthatsuchprotectionwould notbefullyeffective.Whenaskediftheycouldinfecttheir partners even when asymptomatic 88.7% of respondents answeredpositively,2.2%negativelyand8.8%didnotknow. Regarding developmentof malignancy, the risk of cer-vicalandpenile cancerwasmostreadilyrecognized,with muchlowerappreciationforcanceratothersites(Table2). Uncertaintyregarding cancerrisk in theseother siteswas alsoevident.
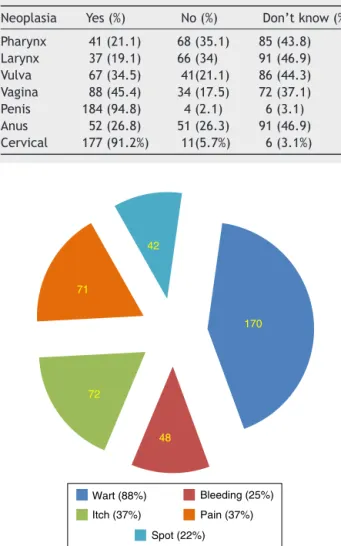
Regarding signs and symptoms of HPV infection, par-ticipants reported warts to be the main symptom (88%). Symptoms suchasbleeding(25%), itching(37%), andspot (22%)wereincorrectlyidentifiedaspartofroutine sympto-matology(Fig.1).
Table1 AnswersaboutthemodesoftransmissionofHPV.
Transmission Yesn(%) Non(%)
Genital 191(98.5) 3(1.5)
Orogenital 127(65.5) 67(34.5)
Anogenital 125(54.1) 89(45.9)
Saliva 19(9.8) 175(90)
Table2 Proportionofresponsesabouttheparticipationof HPVinthepathogenesisofcancerindifferentanatomical sites.
Neoplasia Yes(%) No(%) Don’tknow(%)
Pharynx 41(21.1) 68(35.1) 85(43.8) Larynx 37(19.1) 66(34) 91(46.9) Vulva 67(34.5) 41(21.1) 86(44.3) Vagina 88(45.4) 34(17.5) 72(37.1) Penis 184(94.8) 4(2.1) 6(3.1) Anus 52(26.8) 51(26.3) 91(46.9) Cervical 177(91.2%) 11(5.7%) 6(3.1%)
170
48 72
71
42
Wart (88%) Bleeding (25%)
Itch (37%) Pain (37%)
Spot (22%)
Figure1 SignsandsymptomsofHPVinfectioninaccordance withtheunderstandingofthesurveyedparticipants.
Discussion
AccordingtotheUnitedStatesCentersforDiseaseControl, 49%of HPV infectionsoccur inpeoplebetween 15and 24 yearsofage,withsignificanttreatment-relatedcosts.27
Lowsocioeconomicandeducationalstatusiscorrelated withapoorprognosisinHPV-relateddiseases,suchas Recur-rentRespiratoryPapillomatosis,aswellaswithlowratesof adherencetoinfectionpreventionprograms.28
InBrazil,44.9%ofthepopulationoverage15haseither noeducationor incompleteelementary schooleducation, while19%haveincompletemiddleschooleducation.29
Itisimportanttoconsiderthatalthoughtheeducational levelofthestudygroupwashigherthanthatofthegeneral population,theparticipantshadnoformaleducationinHPV oritsrelateddiseases.Thus,theknowledgeofthisgroupis representativeoftheirpeers.Ourresultsshowgood knowl-edgeofrespondentsonsomeissues,butinotherimportant areasthisknowledgeispartialandfragmented.
The vast majority of the subjects in the study (92.8%) indicated thatthegreaterthe numberofsexualpartners, thegreater therisk ofHPVinfection. Thisresultwasalso
observedinotherstudies.25,30Genitaltogenitaltransmission wasreadilyrecognizedasasignificantfactorforHPV infec-tion.Unfortunately,alternativeformsoftransmissionsuch asorogenital andanogenitalwererecognizedbylessthan halfoftherespondents,animportantdeficitin understand-ingwhat areconsidered tobe safesexual practices. This dataisparticularlytroublingwhenconsideringthepossible consequencesofpersistentinfectionsinthesesites (malig-nanttransformation)anddeservesspecialattentionforthe formulationoffutureeducationalhealthpolicies.24,30
The subjectsinthis workbelong toanage withahigh number of sexual partners and low frequency of condom use.31
Ourresultsindicatethatthemajority(63.4%)of respon-dentsfeelfullyprotectedagainstHPVinfectionwhenusing condoms.Alternativeclinicalpresentationsofviralinfection (RRPandcancer)werenotrecognizedbytheassessed pop-ulation,afactthatshouldalsobeconsideredinprevention programs.
Thevast majorityofrespondentsdidnotrecognizethe possibilityoftransplacentaltransmissionofthevirusoreven iftransmissioncanoccurduringvaginalchildbirth.Whenwe considertheageandyearsofreproductivelifeofthestudied population,inadequateunderstandingofHPVinthisgroup representsaseriousanddangerousknowledgegap.
With respect to HPV-related disease, cervical cancer wasmostreadilyrecognizedbystudyparticipants(91.23%). Unfortunately,therewaspoorrecognitionoftheassociation ofinfectionwithothercancers.Thesedataareconsistent withtheepidemiological datathat hasbeen presented in recentyearsinrelationtosuchdiseases.25,32
Whileeducationaleffortshavebeensuccessfulin estab-lishing recognition of the relationship between HPV and cervical cancer, more aggressive efforts must be made to firmly establish this same recognition with other can-cers.Ourdata indicatethat 88.7% of respondents readily recognized the potential for spreading the disease when asymptomatic. Most respondents recognized the wart as theclassicsymptomof infection,a rategreaterthanthat obtainedbyotherauthors,33 buttheyincorrectlyidentified othersignsandsymptomsascomponentsofactiveinfection (Fig.1).Self-examinationmaybecriticaltorecognitionof activeinfection,andshouldbeencouraged.Earlydetection ofactiveinfectionisimportantaslatediagnosisisassociated withhighercomplicationrates.23,34
However,theinabilitytocorrectlyidentifysignsofactive infection,asdemonstratedinthisstudy,representsacritical barrierthatmustbeovercomeforthesuccessful implemen-tationofaself-examinationprogram.
Taking into account the potential severity and costs related to HPV-associated diseases, the role of preven-tionis unquestionable. However,for individual protective measures to be effective it is necessary that a minimum level of knowledge on the subject is achieved by the population.
However,ithasbeenobservedbyotherauthorsthatan increase in knowledge of the problem is not reflected in awarenessoftheimportanceofthepreventivemeasuresto beadopted.Theseauthorsrecommendedthatinformation shouldbedirectandaccompaniedbyargumentsthatcannot bemisinterpreted.35
Thefactsthatoursamplewasnotrepresentativeofthe entireBrazilianpopulationaswellasthelimitingof recruit-menttoonlyoneuniversityarepotentiallimitationsofthis study.Nevertheless,webelievethatthisworkcanprovide usefulinformationforpolicyguidanceforthepopulation.
Knowledge gaps about HPV infection and its potential consequences can decrease the efficiency and scope of prevention programs. Although vaccination programs are alreadyinplaceforalargeportionofthepopulation they should be supplemented with information for the entire population.Otherwise,theefficacyofvaccinationprograms maybecompromised.Itisessentialtopromoteeducational campaignsabouttherisksoftransmission,formsof protec-tionandconsequencesof HPV-relateddiseases inorderto minimizetheindividualmorbidityandtominimizecoststo thehealthsystem.Publichealthpoliciesforeducationand guidanceofthepopulationshouldbeimplementedinBrazil.
Conclusion
KnowledgeofHPVbythepopulationevaluatedinthisstudy ispartialandfragmented.Lackofknowledgemaycontribute to the further spread of the disease. Public health poli-cies for education andguidance of the population should beimplementedinBrazil.
Conflicts
of
interest
Theauthorsdeclarenoconflictsofinterest.
References
1.VenkatesanNN,PineHS,UnderbrinkMP.Recurrentrespiratory papillomatosis.OrthopClinNorthAm.2012;45:671-ix. 2.Owusu-Edusei K Jr, Chesson HW, Gift TL, Tao G, Mahajan
R, OcfemiaMC, etal. The estimateddirectmedical costof selectedsexuallytransmittedinfectionsintheUnitedStates, 2008.SexTransmDis.2013;40:197---201.
3.DoorbarJ,QuintW,BanksL,BravoIG,StolerM,BrokerTR,etal. Thebiologyandlife-cycleofhumanpapillomaviruses.Vaccine. 2012;30:55---70.
4.AndersonTA,SchickV,HerbenickD,DodgeB,FortenberryJD. Astudyofhumanpapillomavirusonvaginallyinsertedsextoys, beforeand aftercleaning,amongwomenwhohavesex with womenandmen.SexTransmInfect.2014;90:529---31. 5.Skoczy´nskiM,Go´zdzicka-JózefiakA,Kwa´sniewskaA.Risk
fac-torsoftheverticaltransmissionofhumanpapillomavirusin newborns from singleton pregnancy --- preliminary report. J MaternFetalNeonatalMed.2014;27:239---42.
6.Tschandl P, Rosendahl C,Kittler H. Cutaneoushuman papil-lomavirus infection: manifestationsanddiagnosis. CurrProbl Dermatol.2014;45:92---7.
7.Gillison ML, Koch WM, Capone RB. Evidence for a causal association between human papillomavirus and a subset of head and neck cancers. JNatl Cancer Inst.2000;92:709---20 http://jnci.oxfordjournals.org/content/92/9/709.long
8.CoglianoV,BaanR,StraifK,GrosseY,SecretanB,ElGhissassi F.Carcinogenicity ofhuman papillomaviruses.Lancet Oncol. 2005;6:204.
9.BurgerEA,SyS,NygårdM,KristiansenIS,KimJJ.Preventionof HPV-relatedcancersinNorway:cost-effectivenessofexpanding theHPVvaccinationprogramtoincludepre-adolescentboys. PLOSONE.2014;9:e89974.
10.Hu D,GoldieS. Theeconomic burdenofnoncervicalhuman papillomavirus disease in the United States. Am J Obstet Gynecol.2008;198:e1---7.
11.BaioG,CaponeA,MarcellusiA,MenniniFS,FavatoG.Economic burdenofhumanpapillomavirus-relateddiseasesinItaly.PLoS One.2012;7:e49699.
12.Gillison ML, Koch WM, Shah KV. Human papillomavirus in headandnecksquamouscell carcinoma:are someheadand neckcancersasexuallytransmitteddisease?CurrOpinOncol. 1999;11:191---9.
13.Trad M,ReardonRF, CaraveoD. Understanding HPVand the future implications ofcontracting the virus.Radiol Technol. 2013;84:457---66.
14.Barras V, Jacot-Guillarmod M. Human papillomavirus: what do young people really know about it. Rev Med Suisse. 2014;10:1297---301.
15.Chau J, Kibria F,Landi M, Reilly M, Medeiros T, Johnson H, et al. HPV knowledge and vaccine acceptance in an unin-suredHispanicpopulationinProvidenceRI.RIMedJ.2014;97: 35---9.
16.Kester LM, Shedd-Steele RB, Dotson-Roberts CA, Smith J, ZimetGD.Theeffects ofabriefeducationalinterventionon humanpapillomavirusknowledgeandintentiontoinitiateHPV vaccination in 18---26 year old young adults. Gynecol Oncol. 2014;132:S9---12.
17.Lenselink CH, Schmeink CE, Melchers WJ, Massuger LF, Hendriks JC, vanHamont D,et al. Young adultsand accep-tance of the human papillomavirus vaccine. Public Health. 2008;122:1295---301.
18.KielyM,SauvageauC,DubéE,DeceuninckG,DeWalsP.Human papillomavirus: knowledge, beliefs and behavior of Quebec women.CanJPublicHealth.2011;102:303---7.
19.BlödtS,HolmbergC,Müller-NordhornJ,RieckmannN.Human Papillomavirusawareness,knowledgeandvaccineacceptance: a survey among18---25 year old maleand femalevocational school students in Berlin, Germany. Eur J Public Health. 2012;22:808---13.
20.HiltonS,SmithE.Ithoughtcancerwasoneofthoserandom things.Ididn’tknowcancercouldbecaught.:adolescentgirls’ understandingsandexperiencesoftheHPVprogrammeinthe UK.Vaccine.2011;29:4409---15.
21.´SnieturaM,JaworskaM,PigłowskiW,Goraj-Zaj˛acA,Wo´zniakG, LangeD.High-riskHPVDNAstatusandp16(INK4a)expression asprognosticmarkersinpatientswithsquamouscellcancerof oralcavityandoropharynx.PolJPathol.2010;61:133---9. 22.Luryi AL, Yarbrough WG, Niccolai LM, Roser S, Reed SG,
NathanCA,etal.Publicawarenessofheadandneckcancers: a cross-sectional survey. JAMA Otolaryngol Head Neck Surg. 2014;140:639---46.
23.Assi R, Reddy V, Einarsdottir H, Longo WE. Anorectal human papillomavirus: current concepts. Yale J Biol Med. 2014;87:537---47.
24.BadoualC,TartourE,RousselH,BatsAS,PavieJ,PernotS,etal. HPV(HumanPapillomaVirus)implicationinothercancersthan gynaecological.RevMedIntern.2015;5:23---5.
26.deMartinoM,Haitel A,Wrba F,Schatzl G,KlatteT, Waldert M.High-riskhumanpapillomavirusinfectionoftheforeskinin asymptomaticboys.Urology.2013;81:869---72.
27.Centers for Disease Control and Prevention. Incidence, prevalence, and cost of sexually transmitted infections in the United States; 2013 http://www.cdc.gov/std/stats/sti-estimates-fact-sheet-feb-2013.pdf[accessed03.05.15]. 28.ChandoS, Tiro JA, HarrisTR, Kobrin S, Breen N. Effects of
socioeconomicstatusandhealthcareaccessonlowlevelsof humanpapillomavirusvaccinationamongSpanish-speaking His-panicsinCalifornia.AmJPublicHealth.2013;103:270---2. 29.IBGE --- Instituto Brasileiro de Geografia e Estatística; 2015
http://saladeimprensa.ibge.gov.br/noticias?view=noticia&id= 1&busca=1&idnoticia=2125[accessed04.06.15].
30.KreimerAR,BrennanP,LangKuhsKA,WaterboerT,CliffordG, FranceschiS,etal.Humanpapillomavirusantibodiesandfuture riskofanogenitalcancer:a nestedcase-controlstudyinthe Europeanprospective investigationintocancer and nutrition study.JClinOncol.2015;33:877---84.
31.FontenotHB,Fantasia HC,CharykA, SutherlandMA. Human papillomavirus (HPV) risk factors, vaccination patterns, and vaccineperceptionsamongasampleofmalecollegestudents. JAmCollHealth.2014;62:186---92.
32.LillsundeLarssonG, HeleniusG, SorbeB, KarlssonMG.Viral load, integration and methylation of E2BS3 and 4 inhuman papillomavirus(HPV) 16-positivevaginaland vulvar carcino-mas.PLOSONE.2014;9:e112839.
33.Capogrosso P, Ventimiglia E, Matloob R, Colicchia M, Serino A, Castagna G, et al. Awareness and knowledge of human papillomavirus-related diseases are still dramatically insuffi-cientintheeraofhigh-coveragevaccinationprograms.World JUrol.2015;33:873---80.
34.SilvaL,Gonc¸alvesCP,FernandesAMF,DamroseEJ,CostaHO. Laryngealpapillomatosisinchildren:theimpactoflate recog-nitionoverevolution.JMedVirol.2015;87:1413---7.