EFFECT OF PERIOPERATIVE FLUID MANAGEMENT AND
ANAESTHETIC TECHNIQUE IN POSTOPERATIVE OUTCOME AFTER
RENAL TRANSPLANTATION
K. K. Mubarak1, K. P. Radhika2, K. T. Shafna3
HOW TO CITE THIS ARTICLE:
K. K. Mubarak, K. P. Radhika, K. T. Shafna. “Effect of Perioperative Fluid Management and Anaesthetic Technique in Postoperative Outcome after Renal Transplantation”. Journal of Evidence based Medicine and Healthcare; Volume 2, Issue 37, September 14, 2015; Page: 5881-5889, DOI: 10.18410/jebmh/2015/811
ABSTRACT: BACKGROUND: Renal Transplantation provides near normal life to patients with end stage renal disease. Recent advances in medical management, immunosuppression, anaesthetic and surgical techniques have improved the success after renal transplantation. This study has focused on the effect of perioperative fluid management, anaesthetic technique and complications after renal transplantation. MATERIALS & METHODS: In this retrospective study, we reviewed all the cases (136) of renal transplantation conducted from January 2012 to December 2014 at Government Medical College, Kozhikode. Patients were allocated into two groups, Combined Spinal Epidural Anaesthesia (group CSE) and General Anaesthesia with Epidural Analgesia (group GA+EDB). RESULTS: Of the 136 subjects, 66(48.53%) were of group CSE and 70(51.47%) were of group GA+EDB. Of these, 127 patients received live related grafts (93.4%) and 9 cadaveric grafts (6.6%). Male patients predominated with 115(84.6%) whereas female patients were 21(15.4%). Intravenous fluid infused in Group GA+EDB were 5.2±1.53 Liter and 3.5±0.77 Liter in Group CSE with statistically significant p value of 0.000. Duration of surgery was 255±46.66 minutes in Group GA+EDB and 232±31.79 minutes in Group CSE with a p value 0.001, statistically significant. Average patient recovery time was 84.27±39.63 minutes in Group GA+ EDB and 65.9±20.48 minutes in Group CSE with a statistically significant p value of 0.001. There were three mortality in GA+EDB group, of which two were due to airway related problems and one due to refractory pulmonary oedema. CONCLUSION: Combined spinal epidural anaesthesia is a better choice for renal transplantation surgery than general anaesthesia. Optimal perioperative fluid therapy to maintain hemodynamic stability and graft functioning with vigilant monitoring is the key to success.
KEYWORDS: Renal transplantation, Perioperative fluid management, Anaesthetic technique, Postoperative outcome.
INTRODUCTION: Renal transplantation improves the quality of life and survival of patients suffering from end stage renal disease (ESRD) compared to those maintained on dialysis1.
Increased incidence of kidney failure results in longer waiting list for renal transplant surgery and waiting list deaths.
Our institution is a tertiary referral teaching centre, which has been regularly doing renal transplantation since 1985, where the firstrenal transplant surgery was done in Kerala.
functioning with good urine output, careful positioning and good intra and post-operative analgesia.
General anaesthesia using endotracheal intubation and controlled ventilation with epidural analgesia is the commonly practiced anaesthetic technique. The advantages are airway control, good anaesthetic depth, muscle relaxation, haemodynamic stability and controllable intra and postoperative analgesia. The disadvantages include airway manipulation causing stress response, polypharmacy, delayed excretion of drugs in renal failure leading to respiratory and central nervous system depression. Pulmonary aspiration worsens the complications especially with fluid overload.
The above technique was commonly practiced in our institution. Triple lumen catheter was inserted via internal jugular vein for central venous pressure monitoring and fluid administration. Thirty minutes prior to vascular unclamping after placing the graft, crystalloids were infused to attain a central venous pressure (CVP) of 15-20 cm H2O for perfusion of the graft to produce a
good urine output.
We observed serious perioperative problems in many of these patients, primarily due to airway problems and fluid overload, causing soft tissue edema of the head and neck and pulmonary oedema, often requiring tracheal intubation and ventilatory support. Tracheal reintubation was difficult in many cases due to the soft tissue edema, and there was even mortality, primarily attributable to the airway problems.
Since the major risk was airway problems and due to fluid over load, we reconsidered the anaesthetic management, regarding the airway and fluid management. Avoiding airway manipulation and preventing fluid overload were the options. This prompted us to consider regional anaesthesia using a combined spinal and epidural technique with optimum fluid therapy to maintain euvolemia and adequate graft functioning to produce a satisfactory urine output.
Regional anaesthetic techniques (sub-arachnoid, epidural and combined spinal epidural blocks) have been successfully used for renal transplant surgeries. The feared complications are coagulopathy leading to bleeding, epidural haematoma and haemodynamic instability leading to impaired graft functioning. Awake anxious patients may need heavy sedation or even supplementary general anesthesia. Regional anaesthesia has the advantages of avoiding airway manipulation and its related problems like hemodynamic response to tracheal intubation and pulmonary aspiration. Polypharmacy can be avoided in these patients, who are already having impaired kidney function.
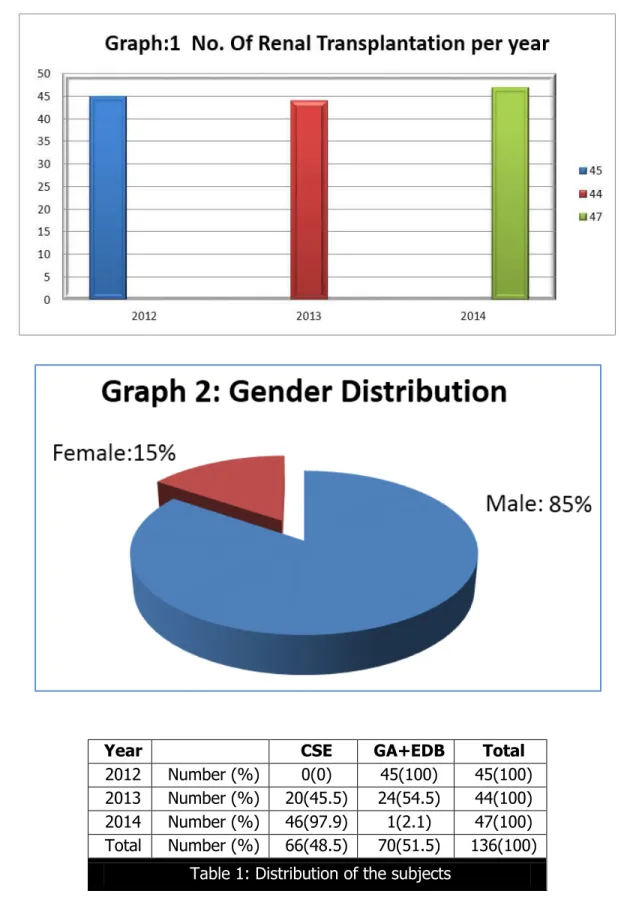
MATERIALS AND METHODS: In this retrospective study all the patients who had undergone renal transplantation over a period of three years from January 2012 to December 2014 were studied with regard to perioperative fluid management, anaesthetic technique and postoperative outcome. We had obtained approval from the institutional research committee for this study.
Patients were allocated into two groups according to the anaesthetic technique used. They were, 1. Combined Spinal Epidural Anaesthesia (Group CSE).
2. General Anaesthesia using endotracheal intubation and controlled ventilation with Epidural Analgesia (Group GA+EDB).
Premedication was given with ranitidine hydrochloride 150 mg orally, morphine 0.1 mg/kg and promethazine 0.25 mg/kg intravenously one hour before surgery. Peripheral venous access was secured in the forearm without arteiovenous fistula and intravenous fluid started. Preinduction monitors used were electrocardiogram, non-invasive blood pressure, and pulse oximeter. Central venous cannula and urinary catheter were later inserted. End tidal CO2 and temperature were also
monitored in group GA+EDB. Central venous catheter was inserted in the arm vein opposite to arteriovenous fistula in group CSE and right internal jugular vein in group GA+EDB.
General Anesthesia: After preoxygenation, fentanyl (2µg/kg) and thiopentone sodium (5mg/kg) was given intravenously. Tracheal intubation was done with suxamethonium (1.5mg/kg), connected to capnometer and bilateral air entry confirmed by auscultation. Anaesthesia was maintained with nitrous oxide, oxygen and Isoflurane. Muscle relaxation was maintained with atracurium (0.5mg/kg) and at the end of the procedure, reversed with neostigmine (0.05 µg/ kg) and glycopyrrolate (8 µ gram/kg) intravenously, ensuring return of muscle power and protective reflexes. Post-operative analgesia was provided via lumbar epidural catheter which was inserted and tested before the induction of general anaesthesia with 0.125% bupivacaine using an elastometric pump.
Combined Spinal Epidural Anesthesia: Before taking up, contraindication for regional anaesthesia like coagulopathy, neuropathy, and cardiorespiratiory compromise were ruled out and heparin free preoperative haemodialysis ensured. Epidural space was identified by the loss of resistance technique using 16G Tuohy needle in the L2-L3 interspace and catheter was introduced.
Test dose of 3ml 2% lignocaine with 1 in 2,00,000 adrenaline was given to rule out intrathecal and intravascular placement. Subarachnoid punctue was performed in the L3- L4 interspace with 23
gauge spinal needle and 3 ml of 0.5% bupivacaine heavy with 60 µg buprenorphine was given.
RESULTS: A total of 136 patients underwent renal transplantation during the study period. Of this, 66(48.53%) were of group CSE and 70(51.47%) were of group GA+EDB. Of these, 127 patients received live related grafts (93.4%) and 9 received cadaveric grafts (6.6%).
Male patients were more with 115(84.6%) and female patients were only 21(15.4%). The causes of End Stage Renal Disease were chronic glomerulonephritis (17.6%), IGA nephropathy (11%), diabetic nephropathy (4.4%), chronic interstitial nephritis (0.7%), polycystic kidney diseases (0.7%), obstructive uropathy, IGA (6.6%), repeat renal transplant (0.7%) and other diseases (57.6%).
were rheumatic heart disease with mitral regurgitation 2.9%, mitral regurgitation, pulmonary regurgitation, coronary artery disease and bicuspid aortic valve, 0.7% each. 2.9% patients had left ventricular hypertrophy, 0.7% each had pulmonary oedema, pericardial effusion and global hypokinesia in echocardiography. Other diseases associated were epilepsy in 5.9%, bronchial asthma, hepatitis, hypothyroidism and eczema of 0.7% each. All the patients were on immunusupressant therapy.
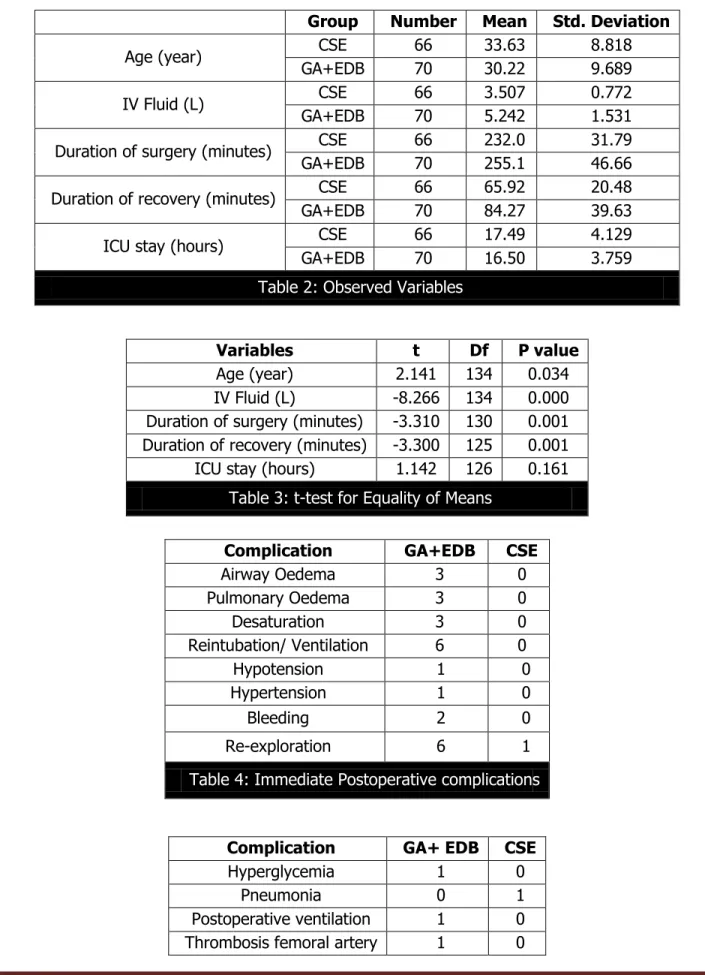
Age was comparable in both the groups (table 1). In Group GA+EDB the mean age was 30.22±9.68, while it was 33.63±8.81 in Group CSE. Central venous cannulation was done via internal jugular vein in Group GA+EDB, and long arm vein in Group CSE. It was via internal jugular vein In 70 patients, long arm vein in 62 patients and subclavian route in 4 patients.
Intravenous fluids administered were crystalloids (Normal Saline and Ringer lactate). No colloids or blood were transfused intraoperatively. All patients received Mannitol 0.5g/kg and Furosemide 1 to 1.5mg/kg before the release of vascular anastamosis. Total fluid infused in Group GA+EDB was 5.2±1.53 Liter and 3.5±0.77 Liter in Group CSE with p value 0.000 which was statistically significant (table 2&3).
Duration of Surgery: The time between entry and exit from operation theatre was 255±46.66 minutes in Group GA+EDB and 232±31.79 in Group CSE with a p value 0.001, which was statistically significant (table 2&3).
Average patient recovery time was 84.27±39.63 minutes in Group GA+ EDB and 65.9±20.48 in Group CSE with a p value 0.001, which was statistically significant (table 2 & 3). Immediate complications (table 4)
In the GA+EDB group, intraoperatively two patients developed tachycardia and five patients had hypotension. One patient developed pulmonary oedema. 131 patients (96.3%) had adequate urine output whereas five (3.7%) patients developed oliguria. Four patients in the group required post-operative ventilation, and the remaining were extubated in the operation theatre.
General anaesthesia was supplemented in four patients of the CSE group due to pain and discomfort during the procedure and in two patients due to inadequate muscle relaxation.
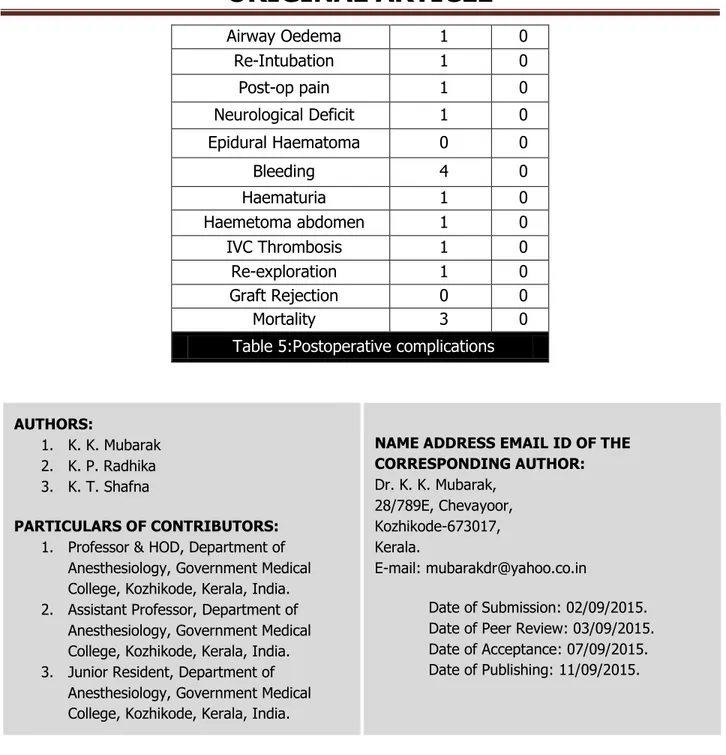
ICU complications (table 5)
All patients were transferred to post kidney transplant unit from the immediate recovery room. Epidural analgesia provided good pain relief in 135 cases. One patient required additional analgesia with intravenous fentanyl. There were three cases of mortality in the GA+EDB group, of which two were due to airway related problems and one due to refractory pulmonary oedema.
DISCUSSION: Renal transplantation is the preferred treatment for patients with ESRD. The first description of anesthesia for renal transplantation was in 1960s under spinal anaesthesia. Earlier transplants were done under spinal anaesthesia and some centers in the United states still perform neuraxial blockade for renal transplantation.2 Case series of successful renal transplantation done
under combined spinal epidural in high risk patients with dilated cardiomyopathy is reported in the literature.3
technique for renal transplant surgery. Since we found serious postoperative morbidity and even mortality, primarily attributable to airway problems and fluid overload, we opted for combined spinal epidural technique, avoiding airway manipulation and optimal fluid therapy for graft functioning, to produce a satisfactory urine output. This has the advantage of providing dense block and muscle relaxation initially by the subarachnoid block, which can be extended with the epidural both for intraoperative and postoperative analgesia3. Low dose of subarachnoid heavy
bupivacaine with buprenorphine was given to attain stable haemodynamics with reduced requirement for intravenous fluids and vasoconstrictors. Central venous access was changed from internal jugular to a peripherally inserted one through brachial vein.
In this study, a statistically significant reduction in the duration of surgery and recovery time was found in the CSE group. Airway problems and fliud overload was more in the GA+EDB group. Re-exploration was required in 8.57% in the GA+EDB group, while only 1.5% had the same in the CSE group.
We observed higher postoperative morbidity and mortality in group GA+EDB. Major problems were airway problems, fluid overload, due to soft tissue edema, arterial de saturation, delayed recovery resulted in reintubation and postoperative ventilator support.
Fluid management is controversial in perioperative medicine and organ transplantation. Goal directed therapy is commonly practiced in transplant medicine.4 Problems of fluid therapy are
contracted intra vascular volume due to preoperative dialysis which makes them prone for hypovolemia causing impaired graft function. Overzealous fluid administration compromise cardiac function leading to decreased graft perfusion and may lead to increased morbidity. Hypovolemia impairs renal perfusion whereas hypervolemia adversely affect cardiac contractility, also reducing renal perfusion in patients with coronary artery disease and left ventricular dysfunction.5 Though
crystalloid solutions are commonly used, colloids may be used in severe hypovolemia. Balanced crystalloids should be alternated with normal saline to prevent hyperchloremic acidosis.
Patients should be adequately hydrated, because renal function is mainly dependent on renal perfusion. Too much crystalloids cause tissue oedema due to redistribution into the interstitial space, which can cause soft tissue oedema causing airway problems and pulmonary oedema.
Peri operative fluid management must ensure restoration and maintenance of intra vascular fluid volume. We assessed the intraoperative volume status by clinical methods including haemodynamic parameters, urine output and the trend in CVP values, rather than a single value. Volume expansion to a target CVP of 10-15mmHg is considered optimal for good renal perfusion and postoperative graft functioning.6 CVP declines in the late intraoperative and immediate
postoperative period even with vigorous fluid resuscitation. The etiology is unclear but may be due to increased vascular permeability.7,8 Invasive blood pressure monitoring is not needed
routinely and the artery may be needed later for creation of arterio venous fistula or a vascular graft.
Average volume of crystalloids infused intra operatively in group GA (5.2±1.5 litre) was higher and was similar to other studies.4,9 In this group some patients developed complications
The combined spinal epidural anaesthesia did not produce major haemodynamic changes in any of the patients, which is the most feared complication of this technique compromising the renal perfusion. The possible mechanisms may be reduced circulating catecholamines, gradual and controlled venous filling prior to graft perfusion.10 The duration of the procedure was less in
group CSE compared to group GA. We found early recovery in group CSE compared to group GA. Total ICU stay was comparable in both the groups. None of our patients developed hemodynamic instability or epidural haematoma, which was the feared complication of the technique.
Careful patient selection, preoperative optimization, proper anaesthetic technique, vigilant monitoring, optimal fluid management and good postoperative care are the keys to a successful renal transplantation surgery.
CONCLUSION: Combined spinal epidural anaesthesia with optimum fluid therapy is an acceptable and good technique for renal transplantation. In this study, we found that this technique, by avoiding airway manipulation and overzealous fluid therapy targeted at a high CVP could significantly improve the postoperative outcome in renal transplant surgery. There was significant reduction of complications like airway problems, postoperative ventilation, duration of the procedure and recovery room stay by selecting this technique. Further large prospective studies are required to put this into a common clinical practice.
REFERENCES:
1. Wolfe RA, Ashby VB, Milford EL, Ojo AO Ettengar RE, Agoda LY et al. Comparison of mortality in all patients on dialysis, patients on dialysis awaiting transplantation, and recipients of a first cadaveric transplant. N Engl J Med 1999; 341: 1725-30.
2. B. S. Martinez, I. Gasanova, and A. O. Adesanya, “Anesthesia for kidney transplantation—a
review,” Journal of Anesthesia and Clinical Research, vol. 4, no. 1, pp. 1–6, 2013.
3. Divya Srivastava, Tanmay Tiwari, Sandeep Sahu et al Anaesthetic Management of Renal Transplant Surgery in Patients of Dilated Cardiomyopathy with Ejection Fraction Less than 40% Anaesthesiology Research and practice, vol. 2014 Article ID 525969, 5 pages
4. Anand Jain, Vaibhavi Baxi, and D Dasgupta Renal Transplantation –Anesthetic experience of 350 cases: Indian J Anesth.2009 Jun; 53 (3): 306-311.
5. Yasser Haggag and Imran Ahmad Guy’s and St Thomas NHS FoundationTrust UK.
www.intechopen.com.
6. Lemmens HJ. Kidney transplantation: recent developments and recommendations for anesthetic management. 2004; 22: 651-62.
7. Thomson HS Lokkegaard H Munck O Influence of normal central venous pressure on onset of function in renal allografts Scand J Urol Nephrol 1987 21: 143-145.
8. Hestin D Mertes PM, Hubert J, Claudon Mejat E, et al Relationship between blood pressure and rennin,angiotensin11 and atrial natriuretic factor after renal transplantation. Clin Nephrol 1997 48: 98-103.
9. O’ Malley CMN, Frumento RJ, Hardy MA et al. A randomized double blind comparison of
10.Sahajananda H, Jyothy, Punithavathy Renal transplantation with and without epidural analgesia – a review of 6 years of experience. Indian J Anesth.2006; 50 (3): 187-192.
Year CSE GA+EDB Total
2012 Number (%) 0(0) 45(100) 45(100)
2013 Number (%) 20(45.5) 24(54.5) 44(100)
2014 Number (%) 46(97.9) 1(2.1) 47(100)
Total Number (%) 66(48.5) 70(51.5) 136(100)
Group Number Mean Std. Deviation
Age (year) CSE 66 33.63 8.818
GA+EDB 70 30.22 9.689
IV Fluid (L) CSE 66 3.507 0.772
GA+EDB 70 5.242 1.531
Duration of surgery (minutes) CSE 66 232.0 31.79
GA+EDB 70 255.1 46.66
Duration of recovery (minutes) CSE 66 65.92 20.48
GA+EDB 70 84.27 39.63
ICU stay (hours) CSE 66 17.49 4.129
GA+EDB 70 16.50 3.759
Table 2: Observed Variables
Variables t Df P value
Age (year) 2.141 134 0.034
IV Fluid (L) -8.266 134 0.000
Duration of surgery (minutes) -3.310 130 0.001 Duration of recovery (minutes) -3.300 125 0.001
ICU stay (hours) 1.142 126 0.161
Table 3: t-test for Equality of Means
Complication GA+EDB CSE
Airway Oedema 3 0
Pulmonary Oedema 3 0
Desaturation 3 0
Reintubation/ Ventilation 6 0
Hypotension 1 0
Hypertension 1 0
Bleeding 2 0
Re-exploration 6 1
Table 4: Immediate Postoperative complications
Complication GA+ EDB CSE
Hyperglycemia 1 0
Pneumonia 0 1
Postoperative ventilation 1 0
Airway Oedema 1 0
Re-Intubation 1 0
Post-op pain 1 0
Neurological Deficit 1 0
Epidural Haematoma 0 0
Bleeding 4 0
Haematuria 1 0
Haemetoma abdomen 1 0
IVC Thrombosis 1 0
Re-exploration 1 0
Graft Rejection 0 0
Mortality 3 0
Table 5:Postoperative complications
NAME ADDRESS EMAIL ID OF THE CORRESPONDING AUTHOR: Dr. K. K. Mubarak,
28/789E, Chevayoor, Kozhikode-673017, Kerala.
E-mail: mubarakdr@yahoo.co.in
Date of Submission: 02/09/2015. Date of Peer Review: 03/09/2015. Date of Acceptance: 07/09/2015. Date of Publishing: 11/09/2015. AUTHORS:
1. K. K. Mubarak 2. K. P. Radhika 3. K. T. Shafna
PARTICULARS OF CONTRIBUTORS: 1. Professor & HOD, Department of
Anesthesiology, Government Medical College, Kozhikode, Kerala, India. 2. Assistant Professor, Department of
Anesthesiology, Government Medical College, Kozhikode, Kerala, India. 3. Junior Resident, Department of