0104-0014/$ - see front matter © 2013 Sociedade Brasileira de Anestesiologia. Published by Elsevier Editora Ltda. All rights reserved. doi: 10.1016/j.bjane.2012.08.004
Oficial Publication of the Brazilian Society of Anesthesiology www.sba.com.br
Revista
BRasileiRa de
anestesiologia
* Corresponding author.
E-mail: meltem72_3@hotmail.com (M.T. Aydogmus).
SCIENTIFIC ARTICLE
Comparison of laryngeal mask airway supreme and laryngeal mask
airway proseal for laryngopharyngeal trauma and postoperative
morbidity in children
Meltem Turkay Aydogmus*, Birsen Eksıoglu, Sibel Oba, Oya Ünsal,
Hacer Sebnem Yeltepe Türk, Sıtkı Nadir Sınıkoglu, Aslıhan Tug
Department of Anesthesiology and Reanimation, Sisli Etfal Training and Research Hospital, Istanbul, Turkey
Received 16 July 2012; accepted 23 August 2012
KEYWORDS
Laryngeal mask airway supreme;
Laryngeal mask airway proseal
Abstract
Background and objectives: Laryngeal mask airway (LMA), which has been used frequently in airway management, can cause laryngopharyngeal injury and morbidity. In this trial, we compare the macroscopic changes on laryngopharyngeal structures and the postoperative laryngopharyngeal morbidity by using LMA supreme with LMA proseal in children.
Methods: We divided patients into two groups. We inserted size three LMA proseal into the first group and size three LMA supreme into the second group. Before LMA insertion and after LMA removal, we performed direct laryngoscopy on the patients. We compared hyperemia, mucosal injury and blood staining on LMA removal, as well as insertion time, rate of success in gastric tube insertion on the first attempt, nausea, vomiting, and sore throat between the two groups.
Results: We recorded no significant differences between the two groups for mean operation time, sex, age, weight, rate of success in gastric tube insertion on first attempt, nausea, vomiting, sore throat and mucosal injury. Mean insertion time for the LMA proseal group was significantly longer than the LMA supreme group (p = 0.0001). The ratio of blood staining on LMA removal was significantly higher in the LMA proseal group than the LMA supreme group (p = 0.034). The patients with blood staining on LMA removal exhibited significantly more mucosal hyperemia and injury than the patients with clear LMA (p = 0.0001, p = 0.020). Conclusion: LMA supreme insertion is faster and easier than LMA proseal and causes less laryngopharyngeal injury than LMA proseal in children.
Introduction
Supraglottic airway devices have been used for airway management in modern anaesthesia. LMA, which was designed
by Dr Archie Brain (UK) in 1981, has been successfully used as
an airway device in both predicted and unpredicted airway difficulties.1,2 Since the first LMA model, new generation LMA
models have been developed.3 LMA supreme was designed
in 2007 to combine the desirable features of ILMA and LMA proseal. It is made of latex-free medical grade polyvinyl chloride (PVC) for single use. Elliptical and anatomically shaped, it facilitates easy insertion, without placing fingers in the patients’ mouths or requiring an introducer tool. It has a gastric access using a lubricated gastric tube up to size 16 F.4,5 The rigid anatomic shape of ILMA facilitates
easy insertion of the device without the need for placing fingers in the patient’s mouth, but does not offer gastric access. LMA proseal is flexible and requires placing fingers in the patient’s mouth or an introducer tool for insertion. Several studies have macroscopically investigated the trauma in the laryngopharyngeal structures caused by LMA classic and LMA proseal in adults,6 but no study has so far
investigated the trauma caused by supreme LMA in children. The primary objective was to compare laryngopharyngeal trauma and macroscopic changes related to LMA proseal with LMA supreme in children. The secondary aim was to compare postoperative laryngopharyngeal morbidity and complications due to LMA proseal with LMA supreme.
Methods
After obtaining the Ethics Committee’s approval and patients’ parents’ written informed consent, the study was conducted according to the Declaration of Helsinki. This prospective and randomized study was performed in 80 patients over a period of eight months. For this study, we selected a group of ASA I patients who were scheduled for minor pelvic or genitourinary operations and weighed between 30-50 kg. Exclusion criteria included patients who had gastroesophageal reflux, risk of aspiration, an airway infection in the last six weeks and known or predicted airway. Thirty minutes before the operation, patients were interned to the premedication unit. We performed intravenous (iv) catheterisation on these patients with a
22-gauge iv catheter, and started 0.9% NaCl fluid infusion. We gave preoperative 0.05 mg•kg-1 iv midazolam as
premedication. We monitored non-invasive systemic artery pressure, ECG and pulse oximetry of the patients interned in the operation room. We divided patients into two groups randomly. We performed randomisation using a sealed envelope method. We performed anesthesia induction
with 2 mg•kg-1 propofol and 1 µg•kg-1 fentanyl. We did not
use neuromuscular blocking agents. After induction and before LMA insertion, an anesthetist with more than five years experience smoothly performed direct laryngoscopy. We used a size three blade for direct laryngoscopy. We excluded the patients who had hyperemia and infection findings in direct laryngoscopy from this trial. Another anesthetist - also with more than five years experience - inserted lubricated LMA, The anesthetist who performed
the direct laryngoscopy did not see the inserted LMA’s type. We used a size three LMA proseal (Laryngeal Mask Company Limited, Le Rocher, Victoria, Mahe, Seychelles) on the first group and size three LMA supreme (Laryngeal Mask Company Limited, Le Rocher, Victoria, Mahe, Seychelles) on the second group. LMA proseal was inserted by finger. We used neither an introducer tool nor fingers in LMA supreme insertion. We included in the trial the patients into whom the LMA had been inserted on the first attempt. We excluded repeated attempts from the trial. We connected the LMA to a circle breathing system. We maintained anaesthesia
with 2% sevoflurane and 40% medical air/O2 mixture. We performed controlled ventilation on the patients as 10
mL•kg-1 tidal volume, 12•min-1 ventilation rate and 1:2
for inspiratory:expiratory rate. We monitored LMA cuff
pressure for lower than 60 cmH2O by using a cuff pressure
monitor (Endotest; Rüsch, Kernen, Germany) and controlled every 10 minutes. After the operation, when spontaneous respiration occurred in deep anaesthesia, the anesthetist who had inserted it removed the LMA. We recorded blood staining on LMA removal. The anaesthetist who performed the direct laryngoscopy before LMA insertion inspected the laryngopharyngeal structures again in direct laryngoscopy. We recorded the presence of hyperemia and mucosal injury numerically as below:
Hyperemia present in oropharynx: 1 No hyperemia in oropharynx: 0 Mucosal injury present: 1 No mucosal injury: 0
Blood staining on LMA removal: 1 No blood on LMA removal: 0
We recorded LMA insertion time, success in inserting the gastric tube on the first attempt, presence of nausea, vomiting, laryngospasm and sore throat in the first hour postoperatively.
Results
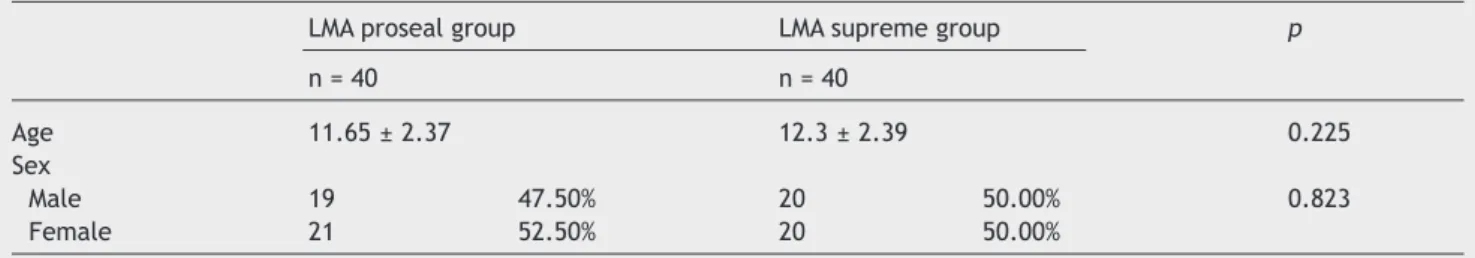
The distribution of sex (p = 0.823) and mean age (p = 0.225) (Table 1) between the LMA proseal and LMA supreme groups were similar. There was no significant difference between groups for mean weight and operation time (p
= 0.933, p = 0.882). We found mean insertion time of the LMA proseal group to be significantly longer than the LMA supreme group (p = 0.0001) (Table 2). We recorded no significant differences between the two groups for incidence of nausea (p = 0.723), vomiting (p = 0.723), sore throat (p = 0.456) and rate of success in inserting the gastric tube on first attempt (p = 0.360) (Table 3). There was no difference between groups according to the mucosal hyperemia (p = 0.366) and mucosal injury (p = 0.090). Rate
of blood staining on removal of the LMA proseal group was significantly higher than the LMA supreme group’s rate (p = 0.034) (Table 4). We found incidence of mucosal hyperemia
in 12 (92.3%) of the patients with blood staining on LMA
removal, significantly more than the patients with clear
LMA 22 (32.8%) (p = 0.0001) (Table 5). The patients with
significantly more than the patients with clear LMA 3 (4.5%)
(p = 0.020) (Table 5).
We calculated the sample sizes with the assumption of at
least of 30% possible difference between any two groups.
Therefore, we allocated 40 patients into each group in
order to obtain an alpha error of 5% and statistical power of 80%.
Statistical analyses
In this study, statistical analyses were performed with the NCSS (Number Cruncher Statistical System) 2007 Statistical Software (Utah, USA) program. For the evaluation of obtained data, along with descriptive statistical methods (mean, standard deviation), an independent t-test was used for comparison
Table 1 The distribution of sex and age in groups.
LMA proseal group LMA supreme group p
n = 40 n = 40
Age 11.65 ± 2.37 12.3 ± 2.39 0.225
Sex
Male 19 47.50% 20 50.00% 0.823
Female 21 52.50% 20 50.00%
LMA, laryngeal mask airway.
Table 2 Mean weight, operation time and laryngeal mask airway insertion time of groups.
LMA proseal group LMA supreme group p
n = 40 n = 40
Weight 39.88 ± 6.75 40 ± 6.45 0.933
Operation time 48.63 ± 14.76 48.13 ± 15.39 0.882
LMA insertion time 17.18 ± 1.88 12.03 ± 1.67 0.0001*
LMA, laryngeal mask airway.
* p < 0.05 (mean ± standard deviation).
Table 3 Incidence of nausea, vomiting, coughing, sore throat and ratio of success in gastric tube insertion on irst attempt among groups.
LMA proseal group LMA supreme group p
n = 40 n = 40
Nausea
Absent 35 87.50% 36 90.00% 0.723
Present 5 12.50% 4 10.00%
Vomiting
Absent 35 87.50% 36 90.00% 0.723
Present 5 12.50% 4 10.00%
Sore throat
Absent 35 87.50% 37 92.50% 0.456
Present 5 12.50% 3 7.50%
Gastric tube insertion
Absent 30 76.90% 34 85.00% 0.360
Present 9 23.10% 6 15.00%
Present 4 10.00% 5 12.50%
between the two groups and a chi-square test was used for comparison of qualitative parameters. We considered results statistically significant when p value was less 0.05.
Discussion
Theoretically, when the cuff pressure is higher than the pharyngeal mucosal capillary perfusion pressure of the LMA-inserted patients, mucosal blood flow reduces and direct tissue trauma occurs. The same happens in the tracheal tube-inserted patients.6 In the histopathologic studies performed
on dogs by Martin et al.,7 the authors reported that high LMA
cuff pressure caused minor changes to the laryngopharyngeal mucosa. These minor laryngopharyngeal injuries may explain the patients’ complaints of sore throat, hoarseness and disphagia. Increased LMA cuff pressures cause a powerful compression of the laryngopharyngeal structures, resulting in injuries of the lingual, hypoglossal, recurrent nerves and lingual artery compression. Therefore, they recommended maintaining LMA cuff pressure lower than 60 cmH2O to
reduce the possibility of these complications.6,7 Seet et al.8
reported that an intracuff pressure lower than 44 mmHg reduced laryngopharyngeal morbidity. In our study, the cuff pressures were monitored in both groups and maintained at
lower than 60 cmH2O by controlling them every 10 minutes.
Although the mucosal hyperemia was seen with direct laryngoscopy more frequently in the LMA proseal group, we found no significant difference between the two groups in our study. We obtained the histopathologic evidences in animal studies which investigated the effects of long-term use of LMA proseal’s on laryngopharyngeal mucosa. Although we found minor mucosal changes, we observed no mucosal injury in the use of LMA proseal over nine hours on pigs. However, we did observe mucosal injuries when using LMA proseal’s over 12 hours.9 In our study, the longest operation time was 80 minutes in the LMA supreme group
and 90 minutes in the LMA proseal group. None of these
complications occurred in either group.
The incidence of sore throat ranged from 5.8% up to 34% for the LMA and it was 10% for the LMA proseal.6 Chia et
al.10 suggested the importance of using larger air volume
and larger size LMA as factors that cause postoperative laryngopharyngeal morbidity. Grady et al.11 demonstrated
that sore throat incidence was higher when using large size LMA. In our study, we planned to avoid the possible differences of morbidity by using size three LMA in both groups. Soar throat incidence during the first hour
postoperatively was 12.5% in the LMA proseal group and 7.5%
in the LMA supreme group, an insignificant difference.
Table 5 Comparison of the blood staining on laryngeal mask airway removal with mucosal hyperemia and mucosal injury.
Blood on LMA (–) Blood on LMA (+) p
n = 67 n = 13
Mucosal hyperemia
Absent 45 67.20% 1 7.70% 0.0001*
Present 22 32.80% 12 92.30%
Mucosal injury
Absent 64 95.50% 10 76.90% 0.020*
Present 3 4.50% 3 23.10%
LMA, laryngeal mask airway. * p < 0.05.
Table 4 Rates of mucosal hyperemia, mucosal injury and blood staining on laryngeal mask airway removal among the groups.
LMA proseal group LMA supreme group p
n = 40 n = 40
Mucosal hyperemia
Absent 21 52.50% 25 62.50% 0.366
Present 19 47.50% 15 37.50%
Blood staining on LMA removal
Absent 30 75.00% 37 92.50% 0.034*
Present 10 25.00% 3 7.50%
Mucosal injury
Absent 35 87.50% 39 97.50% 0.090
Present 5 12.50% 1 2.50%
Timmermann et al.12,13 reported that the LMA supreme
was easy to insert, provided optimal laryngeal view and caused low airway morbidity according to their fiberoptic bronchoscopy performed study. Tan et al.14 suggested that
the mean insertion time was 15 seconds (12-18 seconds) for LMA supreme in their study. In this study, incidence of
blood staining on LMA removal was 7%. A controlled and
randomized study like ours was conducted by Jagannathan et al.15 In this study, the authors recorded insertion time,
easiness of insertion, possibility of gastric tube insertion and complications of LMA supreme size two with LMA proseal size two. There was no statistically significant difference between parameters compared in both groups. The LMA supreme’s mean insertion time was significantly shorter than the LMA proseal’s in our study. The shortest and the longest
insertion times were 9 seconds and 16 seconds, respectively,
for the LMA supreme, and 15 seconds and 21 seconds, respectively, for the LMA proseal. Although we did not find macroscopic bleeding in any patient’s direct laryngoscopy, the incidence of blood staining on removal of the LMA
proseal group (25%) was significantly higher than in the LMA supreme group (7.5%). The presence of mucosal hyperemia
and mucosal injury in the patients with blood staining on LMA removal was significantly higher than the patients with clear LMA. According to these data, the anatomic shape of LMA supreme, which is facilitating easy insertion, results in lower rates of laryngopharyngeal injury.
Eschertzhuber et al.16 reported that the rate of LMA insertion success on the first attempt was 92% for LMA proseal and 95% for LMA supreme in their study. The rate
of gastric tube insertion success on the first attempt was
91% in LMA proseal and 92% in LMA supreme in the same
study. We included only the LMA-inserted patients in the first attempt in our study because repeated attempts could induce laryngopharyngeal trauma. In our study, the rate of gastric tube insertion success in the first attempt was
91% in the LMA proseal group and 92% in the LMA supreme
group. Incidences of coughing, nausea and vomiting were similar in both groups.
In conclusion, it was easier and faster to determine the LMA supreme insertion than the LMA proseal in children. Although both had similar postoperative complications, the LMA supreme caused less laryngopharyngeal injury than the LMA proseal. The LMA supreme could be used safely in elective surgery.
Limitations of the study
Direct laryngoscopy has the possibility of inducing postoperative morbidity. But in our study, there would not be any difference in morbidity rates because we performed direct laryngoscopy in all of the patients. Significant results in this study (such as LMA insertion time or blood staining on LMA removal) were objective findings. Also there was no significant difference between two groups in postoperative complications.
Conlicts of interest
The authors declare no conflicts of interest.
References
1. Singh M, Bharti R, Kapoor D. Repair of damaged supraglottic airway devices: A novel method. Scand J Trauma Resusc Emerg Med. 2010;17:18-33.
2. Sharma V, Verghese C, McKenna PJ. Prospective audit on the use of the LMA-Supreme for airway management of adult patients undergoing elective orthopaedic surgery in prone position. Br J Anaesth. 2010;105:228-32.
3. Ali A, Canturk S, Turkmen A, et al. Comparison of the laryngeal mask airway Supreme and laryngeal mask airway Classic in adults. Eur J Anaesthesiol. 2009;26:1010-4.
4. Verghese C, Ramaswamy B. LMA-Supreme-a new single-use LMA with gastric access: a report on its clinical eficacy. Br J Anaesth. 2008;101:405-10.
5. Seet E, Rajeev S, Firoz T, et al. Safety and eficacy of laryngeal mask airway Supreme versus laryngeal mask airway ProSeal: a randomized controlled trial. Eur J Anaesthesiol. 2010;27:602-7.
6. Tekin M, Kati I, Tomak Y, et al. Comparison of the effects of room air and N2O + O2 used for ProSeal LMA cuff inlation on cuff pressure and oropharyngeal structure. J Anesth. 2008; 22:467-70.
7. Martins RH, Braz JR, Defaveri J, et al. Effect of high laryngeal mask airway intracuff pressure on the laryngopharyngeal mucosa of dogs. Laryngoscope. 2000;110:645-50.
8. Seet E, Yousaf F, Gupta S, et al. Use of manometry for laryngeal mask airway reduces postoperative pharyngolaryngeal adverse events: a prospective, randomized trial. Anesthesiology. 2010; 12:652-7.
9. Brimacombe J, Richardson C, Keller C, et al. Mechanical closure of the vocal cords with the laryngeal mask airway ProSeal. Br J Anaesth. 2002;88:296-7.
10. Chia YY, Lee SW, Liu K. Propofol causes less postoperative pharyngeal morbidity than thiopental after the use of a laryngeal mask airway. Anesth Analg. 2008;106:123-6.
11. Grady DM, McHardy F, Wong J, et al. Pharyngolaryngeal morbidity with the laryngeal mask airway in spontaneously breathing patients: does size matter? Anesthesiology. 2001;94: 760-6.
12. Timmermann A, Cremer S, Eich C, et al. Prospective clinical and iberoptic evaluation of the Supreme laryngeal mask airway. Anesthesiology. 2009;110:262-5.
13. Timmermann A, Cremer S, Heuer J, et al. Laryngeal mask LMA Supreme. Application by medical personnel inexperienced in airway management. Anaesthesist. 2008;57:970-5.
14. Tan BH, Chen EG, Liu EH. An evaluation of the laryngeal mask airway supreme’ in 100 patients. Anaesth Intensive Care. 2010; 8:550-4.
15. Jagannathan N, Sohn LE, Sawardaker A, et al. A randomised comparison of the LMA Supreme™ and LMA ProSeal™ in children. Anaesthesia. 2012;67:632-9.