Jebmh.com
Case Report
J. Evid. Based Med. Healthc., pISSN- 2349-2562, eISSN- 2349-2570/ Vol. 3/Issue 60/July 28, 2016 Page 3279
A CASE REPORT OF THROMBOTIC ANEURYSM OF EXTERNAL JUGULAR VEIN PRESENTING
AS POSTERIOR NECK SWELLING
Reena Mathur1, Jaya Pamnani2, Shyojiram Burdak3, Divya Bagoria4, Sumitra Choudhary5, Prasanna R6
1Professor & HOD, Department of Radiodiagnosis, JLN Medical College, Ajmer. 23rd Year Resident Doctor, Department of Radiodiagnosis, JLN Medical College, Ajmer. 33rdYear Resident Doctor, Department of Radiodiagnosis, JLN Medical College, Ajmer. 43rd Year Resident Doctor, Department of Radiodiagnosis, JLN Medical College, Ajmer. 53rd Year Resident Doctor, Department of Radiodiagnosis, JLN Medical College, Ajmer. 63rd Year Resident Doctor, Department of Radiodiagnosis, JLN Medical College, Ajmer.
ABSTRACT
Venous aneurysm is rare in occurrence. This report describes a case of thrombotic aneurysm of External Jugular Vein that presented as a mass in posterior triangle of neck. Diagnosis was done using colour Doppler Ultrasound and further confirmed by CT Angiography.
KEYWORDS
External jugular vein (EJV), Aneurysm, Colour Doppler Study and CT Angiography (CTA).
HOW TO CITE THIS ARTICLE: Mathur R, Pamnani J, Burdak S, et al.A case report of thrombotic aneurysm of external jugular vein presenting as posterior neck swelling. J. Evid. Based Med. Healthc. 2016; 3(60), 3279-3281.
DOI: 10.18410/jebmh/2016/709
INTRODUCTION: Venous Aneurysms are a rare entity in Head and Neck due to low pressure prevailing in SVC system. These can be primary (Idiopathic) or secondary (Post Traumatic). Most cases are after long duration catheterisation or after any surgical intervention. Here, it is a case of idiopathic thrombotic aneurysm involving EJV on left side.
CASE REPORT: A 40-year-old married female presented with a neck swelling that she noticed after sudden onset of pain in her left neck region 15 days ago. The swelling was painless at present. No fever existed. There was no increase in size of swelling. Physical examination revealed a soft, round to oval, nontender, non-pulsatile swelling measuring about 2 cm at the left supraclavicular region with no skin changes. Valsalva showed no significant change in size of swelling. On auscultation, bruit was not present and transilluminance was absent. There was no history of obvious trauma. The physical examination of rest of the systems was normal. Laboratory tests, chest radiographs were unremarkable. Her cardiac risk profile was negative for diabetes mellitus, hypertension, and hyperlipidaemia. There was no history of oral contraceptive pills or any hormone replacement therapy. The patient was then sent to the department of radiology for USG neck. Ultrasonography revealed saccular dilatation of external jugular vein with predominantly hyperechoic content within it almost completely occupying the lesion.
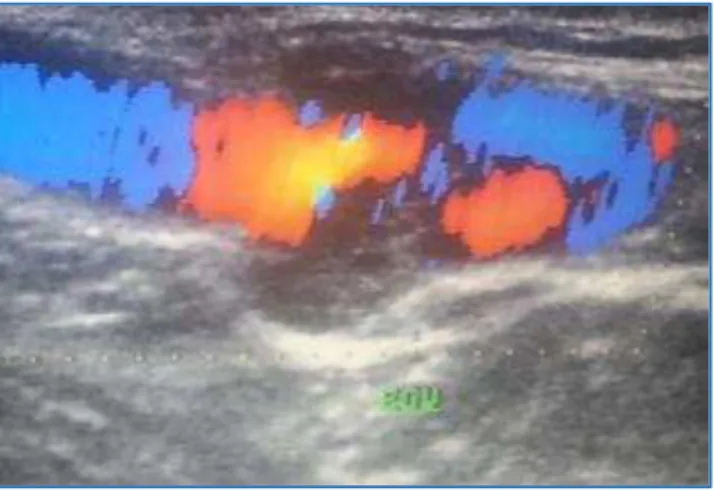
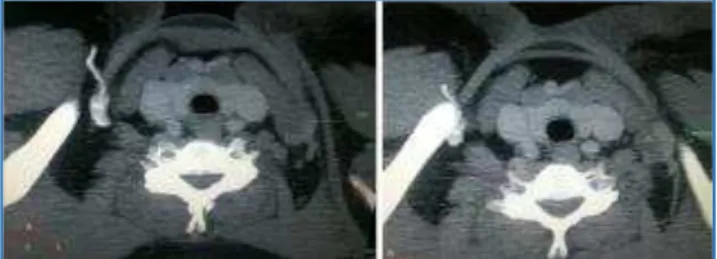
The vein was non-compressible. This was in favour of thrombotic aneurysm. Colour Doppler showed minimally perceptible flow at the site of aneurysm. Internal jugular vein showed normal waveform. CT Angiography was done for further confirmation of diagnosis. CT examination was performed during Valsalva manoeuvre. Arterial and venous structures of the neck were evaluated with post-processed images obtained by Multiplanar Reformation, Volume Rendering techniques and Maximum Intensity Projection (MIP) based on the axial scan. The investigation revealed saccular dilatation of external jugular vein (2.3 x 18 x 19 mm) which showed filling defect with peripheral eccentric patent lumen on contrast study was noted 3.5 cm proximal to its merger with subclavian vein s/o Thrombotic saccular aneurysm of left external jugular vein.
Bilateral internal jugular veins and carotid arteries were patent and normal. Right jugular vein was patent and normal. Brachiocephalic veins and svc appeared normal. No evidence of any atherosclerotic changes were seen in aorta.
Fig. 1: Colour Doppler Image of left EJV in Sagittal Section showing Peripheral Eccentric Colour Filling
Defect at the Site of Focal Dilatation
Financial or Other, Competing Interest: None. Submission 07-07-2016, Peer Review 15-07-2016, Acceptance 25-07-2016, Published 28-07-2016. Corresponding Author:
Dr. Jaya Pamnani, D/o. Mrs. Chaya Pamnani,
Jebmh.com
Case Report
J. Evid. Based Med. Healthc., pISSN- 2349-2562, eISSN- 2349-2570/ Vol. 3/Issue 60/July 28, 2016 Page 3280
Fig. 2: Axial CT Sections showing Dilated EJV with Non-enhancing Lumen and Peripheral Enhancement
Fig. 3: Axial CT Sections showing dilated EJV with Non-enhancing Lumen and Peripheral Enhancement
DISCUSSION: Venous aneurysms (Saccular).[1] and
phlebectasias (Fusiform Focal Dilatation of Vessel).[2]are
rare vascular malformations that occur equally between males and females and do not exhibit any age preponderance. There is no precise size criterion in the literature to differentiate between aneurysm and dilatation of vein. The superficial venous system aneurysms incidence is described around at 0.1%.[3] Superficial venous
aneurysms of the neck (e.g. EJV, facial vein) are extremely rare due to low pressure system of SVC and most commonly involves internal jugular vein.[4] followed by external jugular
vein and very rarely anterior jugular vein. Usual presentation is as asymptomatic subcutaneous insidious swelling and may be associated with pain if thrombosed. Venous aneurysms can be classified as primary and secondary. Primary are spontaneous in occurrence, without any known aetiological factor mostly congenital and are regarded as true aneurysms as the venous wall is intact while secondary are caused by trauma, valvular insufficiency, infection or by an arteriovenous fistula.
Superficial venous aneurysm are not life threatening. Most reported superficial venous aneurysms are asymptomatic but thrombosis and severe pain have been observed due to thrombus formation or mass effect on adjacent structures. The first investigation to be performed is Ultrasonography being a non-invasive technique. The aneurysm appears as well-defined anechoic cystic structure. Colour and Spectral Doppler ultrasound scans show the vascular nature of the lesion and its continuity with the venous system and can differentiate venous aneurysms from arterial aneurysms (If arterial wave form is seen) or A-V fistula (If communication or arterial as well as venous flow is detected). Thrombus, if present, is seen as a lesion of variable echogenicity (As per the age of thrombus) within the lumen. Computed Angiography and MR venography define the size and lesion extent more precisely.
Uncomplicated venous aneurysm enhances during venous phase while if complicated with thrombus the enhancement may be further delayed or may be insignificant, in that case dilatation of vessel wall and its contiguity with the normal vascular lumen establishes the diagnosis.
Complications:
Thrombophlebitis.
Thrombus Formation.
Pulmonary Embolism.
Spontaneous Rupture.
Differential Diagnoses:
Varicose Veins: Veins are tortuous as well as dilated and involve a long segment of the vessel.
Haemangioma: Thrombotic aneurysm may mimic a haemangioma but presence of phleboliths and progressive centripetal filling in during CT establishes the diagnosis.
Lymphocoele: Nonvascular, may show fine septations and is Non-contiguous with the vessel
Arteriovenous Fistulas: Exhibits feeding artery as well as a draining vein on spectral Doppler analysis and early enhancement of vein is noted during CT angiography.
Lymphadenopathy: A large cystic necrotic lymph node can mimic a vessel on grey scale; however, has altered vascularity and vascular contiguity can't be established.
Branchial Cleft Cyst: Nonvascular and occurs at a typical location.
Dermoid Cyst: May show some calcified and fat component.
Treatment: Asymptomatic i.e. silent aneurysms can be managed expectantly with reassurance and regular followup.
Surgery is the definitive treatment.
Indications for surgery:
1. Symptomatic (Pain, Thromboembolism).[5]
2. Enlarging 3. Disfiguring.[6]
Aneurysms should be resected and end-to-end anastomosis or venous continuity with a graft can be established.[7] However, some suggest to perform surgical
resection in all cases to prevent future complications. Superficial venous aneurysms are managed by excision followed by ligation. The surgery is a uniformly successful form of therapy provided satisfactory venous function is achieved.
Jebmh.com
Case Report
J. Evid. Based Med. Healthc., pISSN- 2349-2562, eISSN- 2349-2570/ Vol. 3/Issue 60/July 28, 2016 Page 3281
REFERENCES
1. Schatz IJ, Fine G. Venous aneurysms. N Engl J Med 1962;266:1310-1312.
2. Gerwig WH. Internal jugular phlebectasia. Ann Surg 1952;135(1):130-133.
3. Pascarella L, Al-Tuwaijri M, Bergan JJ, et al. Lower extremity superficial venous aneurysms. Annals of Vascular Surgery 2005;19(1):69-73.
4. Schild H, Berg S, Weber W,
et al
. The venous aneurysm. Aktuelle Radiol1992;2(2):75-80.5. Gabrielli R, Rosati MS, Siani A, et al. Management of symptomatic venous aneurysm. Scientific World Journal 2012;2012:386478.
6. Calligaro KD, Ahmad S, Dandora R, et al. Venous aneurysms: surgical indications and review of the literature. Surgery 1995;117(1):1-6.
7. Ekim H, Kutay V, Tuncer M, et al. Management of
primary venous aneurysms. Saudi Med J
2004;25(3):303-307.