ABSTRACT
BACKGROUND AND OBJECTIVES: Adequate nutritional
intervention promotes wellbeing, symptoms control and im-proved quality of life for patients and their families. his study aimed at evaluating whether nutrition may or may not improve quality of life of patients under palliative care.
CONTENTS: his is an integrative review using Pubmed, Sci-elo and Medline databases. Guiding question was: “Is nutritional therapy able to improve quality of life of patients under palliative care?” Six articles met pre-established inclusion criteria. Nutri-tionists were professionals most orienting nutritional therapy, in addition to explaining nutritional strategies to minimize diet-related discomforts. Adequate therapy should respect dietary and cultural preferences, thus assuring better quality of life.
CONCLUSION: Nutritional approach during palliative care should respect patients and their families’ decisions and bioethics principles. Nutritional interventions should give more importance to counseling and support, instead of focusing just on matching nutritional needs. Nutritionists should orient patients and their families about nutri-tional therapy, in addition to giving further explanations to prolong survival, decrease weight loss and improve quality of life.
Keywords: Bioethics, Nutritional therapy, Nutritionist, Pallia-tive care, Quality of life.
RESUMO
JUSTIFICATIVA E OBJETIVOS: A intervenção nutricional adequada promove bem-estar, controle de sintomas e melhora da qualidade de vida dos pacientes e de seus familiares. O objetivo deste estudo foi veriicar se a nutrição pode ou não melhorar a qualidade de vida do paciente em cuidados paliativos.
CONTEÚDO: Trata-se de uma revisão integrativa, utilizando
Nutrition, quality of life and palliative care: integrative review
Nutrição, qualidade de vida e cuidados paliativos: uma revisão integrativa
Suelyne Rodrigues de Morais1, Alane Nogueira Bezerra2, Natália Sales de Carvalho3, Ana Carolina Cavalcante Viana1
1. Hospital Universitário Walter Cantídio, Residência em Assistência em Transplantes, For-taleza, CE, Brasil.
2. Hospital Universitário Walter Cantídio, Residência em Assistência em Diabetes. For-taleza, CE, Brasil.
3. Universidade de Fortaleza. Fortaleza, CE, Brasil. Submitted in August 20, 2015.
Accepted for publication in April 11, 2016. Conlict of interests: none – Sponsoring sources: none.
Correspondence to: Suelyne Rodrigues de Morais
Rua Capitão Francisco Pedro, 1290 - Rodolfo Teóilo 60430-370 Fortaleza, CE, Brasil.
E-mail: suelyne_rodrigues@hotmail.com
© Sociedade Brasileira para o Estudo da Dor
as bases de dados Pubmed, Scielo e Medline. A pergunta nortea-dora foi “A terapia nutricional é capaz de melhorar a qualidade de vida dos pacientes em cuidados paliativos?”. Seis artigos se en-quadravam nos critérios de inclusão pré-estabelecidos. O cionista foi o proissional que mais orientou sobre a terapia nutri-cional em uso, além de fornecer esclarecimentos sobre estratégias nutricionais para redução de desconfortos ligados à alimentação. A terapia adequada deve respeitar as preferências alimentares e culturais, garantindo, assim, melhor qualidade de vida.
CONCLUSÃO: A conduta nutricional em cuidados paliati-vos deve respeitar as decisões do paciente e de sua família e os princípios bioéticos. As intervenções nutricionais devem dar maior importância à prestação de aconselhamento e de apoio, ao invés de centrar apenas na adequação das necessidades nu-tricionais. O nutricionista deve orientar o paciente e sua família sobre a terapia nutricional em uso, além de fornecer orientações e esclarecimentos, a im de prolongar a sobrevida, reduzir a perda de peso e melhorar a qualidade de vida.
Descritores: Bioética, Cuidados paliativos, Nutricionista, Quali-dade de vida, Terapia nutricional.
INTRODUCTION
he World Health Organization (WHO) has published in 1990 a deinition of palliative care (PC) and this concept was updat-ed in 2002 being internationally acceptupdat-ed: “Palliative care is an approach that improves the quality of life of patients and their families facing the problem associated with life-threatening ill-ness, through the prevention and relief of sufering by means of early identiication and impeccable assessment and treatment of pain and other problems, physical, psychosocial and spiritual”1.
In palliative care, when cure is no longer possible, therapeutic strategy should be based on maintaining patients’ autonomy preserving the most from their normal lives or helping people enjoy their vitality within their limits2. Observing that
qual-ity of life (QL) is individuals’ perception of their position in life, in the context of the culture and value system within they live, and also considering objectives, expectations, patterns and interests, one may state that PC aims at reaching the best pos-sible QL for patients and their families, without delaying or hastening death, which should be respected for being a consti-tutive element of the natural process of life3. So, PC should be
an alternative for the assistance to patients without therapeutic possibilities of cure to be human, fair and beneicial2.
important thing for PC is to preserve patients’ dignity and to provide comfort and wellbeing, which may be reached by means of minor and simple actions, such as basic hygiene, ad-equate attention, comfortable furniture and diet4. It is critical
to use resources preventing nutritional and gastrointestinal manifestations, such as anorexia, nausea, vomiting, wasting, malnutrition and dehydration, in addition to relieving their repercussions and extensions, if already installed5.
PC should respect patients’ desires and should supply the most possible comfort by means of indicated therapies to minimize distress, but there are controversies whether food could contrib-ute to this process. In general, these patients have some nutri-tional impairment, but not always this recovery is reached by means of nutritional therapy. Nutritional, caloric, protein and water requirements should be established according to patients’ acceptance, tolerance and symptoms, aiming at promoting com-fort and better QL and not only assuring adequate nutrients ingestion, preventing in some cases unnecessary invasive nutri-tional interventions, such as introduction of enteral nutrinutri-tional therapy (ENT) or parenteral nutritional therapy (PNT)6.
his study aimed at observing whether nutritional orientation may improve QL of PC patients by means, considering that an adequate nutritional intervention promotes wellbeing, symp-toms control and better QL of patients and their families.
CONTENTS
his is an integrative review consisting of six stages, where the irst stage is to decide the hypothesis or question of the study.
hen, a sample of scientiic articles to be reviewed is selected, followed by categorization and evaluation of such studies. In-terpretation of results and presentation of the review or of the summary of the knowledge are the last steps of this process7.
Articles were selected using Pubmed, Scielo and Medline da-tabases, by means of the following keywords: bioethics ( bioé-tica); palliative care (cuidados paliativos); nutrition (nutrição); nutritionist (nutricionista).
he following question was developed to guide the study: “Is nutritional therapy able to improve quality of life of patients under palliative care?”, complying with the following inclu-sion criteria: mentioning PC patients’ nutrition, being in-dexed in databases, being published in Portuguese or English between 2005 and 2015 and being available in full. Exclusion criteria were all articles of restricted access and literature re-views.
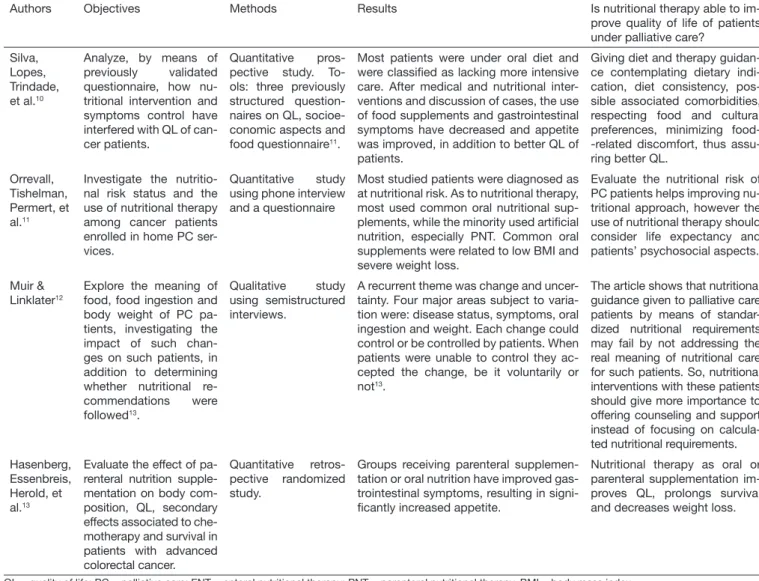
Articles were selected by reading titles and respective abstracts aiming at checking the matching of the study to the guiding question. At the end of the search, 16 studies were found, however 10 studies were excluded because nutritionist was mentioned by there were no results on nutritional guidance. So, only six have met pre-established inclusion criteria, of which four are quantitative studies and two are qualitative studies. For data extraction identiication, characteristics of study methods, evaluation of methodological rigor, studied interventions and results were investigated. Data and discus-sion were presented in descriptive form, making possible the application of this review to nutrition practice in PC. Includ-ed articles are shown in table 1.
Table 1. Information on articles included in the integrative review according to the guiding question. Fortaleza, 2015
Authors Objectives Methods Results Is nutritional therapy able to im-prove quality of life of patients under palliative care?
Schirmer, Ferrari & Trindade8
Evaluate the evolution of oral mucositis in cancer patients assisted by the PC service, after medi-cal and nutritional inter-vention and guidance, in addition to evaluating how mucositis severity interferes with patients’ food ingestion.
Qualitative prospecti-ve study using inter-views and previously structured question-naire.
Before intervention, mucositis grade I was present in more than half the patients and almost half of them ingested solid food. Few individuals had mucositis grade IV where all ingested liquid food. After inter-vention, more than half the patients had no mucositis and no restrictions to diet consistency. Oral complaints, such as xe-rostomia dysgeusia, appetite loss, anore-xia and candidiasis were decreased.
Nutritional guidance, such as mouth washing with chamomile tea, avoiding very acid, dry, hard or spicy food, restrict salt, avoid very hot food or preparations may help improving mucositis, thus assuring better QL.
Loyolla, Pessini, Bottoni, et al.9
Analyze, from bioethics point of view, the use of nutritional therapy for cancer patients under PC, observing vision and participation of patients and their families in the decision to use such therapy
Qualitative study with semistructured ques-tionnaire.
Most patients and caregivers were in-formed about indicated ENT by the nu-tritionist. When asked about what is and what is the purpose of TNE, most have answered that it served to fortify and feed patients. With regard to the choice by pa-tients or caregivers to start or not TNE, answer was yes for many, but some were in doubt and thought that this should be a physician’s decision. As to ENT being a basic care that should always be provided, answers have varied from replacement by other if not bringing beneits or cannot be withdrawn because it is patient’s right.
ENT is considered a basic care by patients and/or caregivers and is patient’s right, which shall be replaced but never with-drawn if not bringing beneit to patients. Although nutritionist was the professional more ex-plaining about ENT, patients and caregivers feel they are unable to decide about using ENT.
Table 1. Information on articles included in the integrative review according to the guiding question. Fortaleza, 2015 – continuation
Authors Objectives Methods Results Is nutritional therapy able to im-prove quality of life of patients under palliative care?
Silva, Lopes, Trindade, et al.10
Analyze, by means of previously validated questionnaire, how nu-tritional intervention and symptoms control have interfered with QL of can-cer patients.
Quantitative pros-pective study. To-ols: three previously structured question-naires on QL, socioe-conomic aspects and food questionnaire11.
Most patients were under oral diet and were classiied as lacking more intensive care. After medical and nutritional inter-ventions and discussion of cases, the use of food supplements and gastrointestinal symptoms have decreased and appetite was improved, in addition to better QL of patients.
Giving diet and therapy guidan-ce contemplating dietary indi-cation, diet consistency, pos-sible associated comorbidities, respecting food and cultural preferences, minimizing food--related discomfort, thus assu-ring better QL.
Orrevall, Tishelman, Permert, et al.11
Investigate the nutritio-nal risk status and the use of nutritional therapy among cancer patients enrolled in home PC ser-vices.
Quantitative study using phone interview and a questionnaire
Most studied patients were diagnosed as at nutritional risk. As to nutritional therapy, most used common oral nutritional sup-plements, while the minority used artiicial nutrition, especially PNT. Common oral supplements were related to low BMI and severe weight loss.
Evaluate the nutritional risk of PC patients helps improving nu-tritional approach, however the use of nutritional therapy should consider life expectancy and patients’ psychosocial aspects.
Muir & Linklater12
Explore the meaning of food, food ingestion and body weight of PC pa-tients, investigating the impact of such chan-ges on such patients, in addition to determining whether nutritional re-commendations were followed13.
Qualitative study using semistructured interviews.
A recurrent theme was change and uncer-tainty. Four major areas subject to varia-tion were: disease status, symptoms, oral ingestion and weight. Each change could control or be controlled by patients. When patients were unable to control they ac-cepted the change, be it voluntarily or not13.
The article shows that nutritional guidance given to palliative care patients by means of standar-dized nutritional requirements may fail by not addressing the real meaning of nutritional care for such patients. So, nutritional interventions with these patients should give more importance to offering counseling and support instead of focusing on calcula-ted nutritional requirements. Hasenberg,
Essenbreis, Herold, et al.13
Evaluate the effect of pa-renteral nutrition supple-mentation on body com-position, QL, secondary effects associated to che-motherapy and survival in patients with advanced colorectal cancer.
Quantitative retros-pective randomized study.
Groups receiving parenteral supplemen-tation or oral nutrition have improved gas-trointestinal symptoms, resulting in signi-icantly increased appetite.
Nutritional therapy as oral or parenteral supplementation im-proves QL, prolongs survival and decreases weight loss.
QL = quality of life; PC = palliative care; ENT = enteral nutritional therapy; PNT = parenteral nutritional therapy. BMI = body mass index.
DISCUSSION
Untreated mucositis may interfere with nutritional status and even interfere with the choice of anti-cancer therapy, in addi-tion to impairing patients’ QL14. According to Schirmer,
Fer-rari and Trindade8, nutritional therapy may prevent severe oral
mucositis8. According to Boligon and Huth15,
supplementa-tion with 20g/day glutamine for head and neck cancer pa-tients under anti-cancer therapy has helped the maintenance of nutritional status and has prevented mucositis, especially grades III and IV. In case of moderate to severe mucositis, enteral nutrition with nasogastric/nasoenteric probe, or even parenteral nutrition, should be indicated in cases of weight loss above 5%. So, medical and nutritional care is needed to contribute to anti-cancer therapy maintenance, as well as to patients’ weight maintenance and hydration16.
Multiprofessional action is mandatory for the eicient man-agement of PC patients, helping improving complications, QL and their autonomy9. his should be achieved by means
of better interaction among professionals, considering the in-dividualized choice of pharmacological and dietary therapy, in addition to minimizing drug-related adverse efects10.
Loyolla et al.9 have observed that patients and caregivers were
informed about nutritional therapy and knew how to deine its function and importance. However, it was observed that information given by professionals was not enough or was not clear for most patients and caregivers. his transfers ENT responsibility to the physician aiming at assuring patients’ beneit. In addition, physician, patient and caregiver relation-ship still follows the old paternalist pattern, an asymmetric relationship where the only decision-maker on therapy is the physician.
According to Cardoso et al.17 the multiprofessional team
nu-tritional requirements. Dietary prescription should, above all, ofer pleasure and comfort to patients, in addition to respecting their will2. So, it is clear that patients’ autonomy, while being
conscious and able to decide, should be respected, otherwise, family should determine what is best9.
Silva et al.10 have shown that nutritional and medical
inter-ventions have indirectly relected on socialization and have al-lowed patients’ participation in meals together with relatives and friends, in addition to implying comfort and self-care. his has shown that nutritional aspects are not only those related to nutritional status, but also those related to family relations, pleasure, wellbeing and autonomy. Seredynskyj et al.18 have observed that autonomy should be preserved for the
maintenance of better patients’ health status. In addition, si-multaneous medical and nutritional intervention has also re-sulted in improved symptoms such as appetite loss, dysgeusia, oral candidiasis, mucositis, nausea and constipation, similarly to Durval et al.19 indings, who have shown improved
wast-ing, thus contributing to better QL. When strategies to favor food ingestion are obtained, results portray patients’ clinical and social approach, improving their life condition10.
Orrevall et al.11 have observed that more than two thirds of
patients were at nutritional risk, which was associated to pre-cancer low body mass index (BMI). However, an association between pre-cancer BMI indicating overweight and nutri-tional risk was also found, being indicated that nutrinutri-tional problems may not be easily identiied without nutritional tracking, even after severe weight loss. his study has shown the need for a structured approach to early identify and evalu-ate cancer patients on nutritional risk. However, any evalua-tion tool which may generate physical or emoevalua-tional discom-fort should not be used in this stage.
Incurable cancer is associated to high prevalence of nutri-tional problems and weight loss, leading to physical and psychological impairment. Nutritional implications should be identiied and treated as early as possible during disease progression, however, in later stages, nutritional therapy is still controversial20.
Nutritional therapy is part of integral oncological support and may signiicantly contribute to improve QL21. However,
ENT or PNT should only be started in individuals with bet-ter life expectance and/or if there are psychosocial aspects fa-voring such process, to assure better life condition to patients, sparing those with no indication from unnecessary interven-tions22.
Muir and Linklater12 have observed the testimony of patients,
allowing a broad understanding of their concerns. For them, food goes beyond nutritional objectives; it is relected on mo-tivation, control along disease progression, care and compas-sion exprescompas-sions, and death acceptance. Health worsening may be often identiied by not being able to eat22.
With regard to meaning, foods are physical substances neces-sary as energy source to feed the body and continue to ight against disease, which is source of frustration and anxiety, in addition to showing the sensation of patients’ care and
inter-est. Changes in food ingestion have followed the trend of de-cline, characterized by decreased appetite, oral ingestion and weight loss. Decreased consumption has induced physical and psychological changes in such patients. As to weight, loss was fearsome and stressing because death process was com-ing close. So, most of them have felt that weight monitorcom-ing could be noxious or even useless12.
Malnutrition is mentioned by studied patients not only as physical malnutrition, but also as psychological and socio-logical malnutrition. Weight loss may be identiied by many as symbol of disease progression, loss of control of their own body and physical and emotional weakness, and may also represent the proximity of death. Many times it is related to weakness, fatigue and decreased QL23. Nutritional care
strate-gies with holistic approach should be developed to meet the broad meanings that food or eating may have, because already deined protocols and standards may not meet individual re-quirements and even overload patients with unfeasible tar-gets, such as weight gain and adequate nutritional ingestion12.
So, sensitivity and creativity will make the diference during nutritional evaluation and guidance22. Aiming at improving
QL, the real meaning of PC nutritional care should be ad-dressed, especially by means of assuring patients’ counseling and support12.
Hasenberg et al.13 have observed that early nutritional therapy
may maintain body composition, improve life condition and even prolong survival of cancer patients under PC13. It is
nec-essary to stress that unintentional weight loss and changes in body composition are related to unfavorable clinical evo-lution, psychological, socioeconomic and QL impairment21.
his article has observed the efects of parenteral and oral nutrition supplementation. Group receiving PNT and oral nutrition have stabilized albumin levels, in addition to im-proving gastrointestinal symptoms related to chemotherapy, thus improving QL. Patients receiving oral supplementation have reported improved symptoms, such as early satiation, constipation, nausea, vomiting, abdominal pain and diarrhea, resulting in signiicant appetite improvement in this group13.
So, nutritional intervention has positively impacted clinical and social aspects, improving individuals’ life condition. Anti-cancer therapies may produce additional symptoms, negatively afecting nutritional status, depending on treat-ment type and duration, dose and individual patients’ re-sponse21. Nutritional therapy helps decreasing
treatment-re-lated symptoms and disease evolution, as well as weight loss, prolonging survival and improving QL13.
In light of the above, dietary approach should, above all, ofer pleasure and comfort, respecting patients and their families’ autonomy. So, together with other therapeutic measures, it may contribute to promote QL of patients without clinical possibilities of cure.
CONCLUSION
beneicence, non malfeasance and justice. Nutritional therapy may prolong survival, decrease weight loss and improve QL of PC patients, by means of decreasing adverse efects of treat-ments and/or diseases. Considering the importance of this article, there is need for further nutrition studies involving PC patients, not only in the oncologic area, but also in all diferent situations involving this theme.
REFERENCES
1. World Health Organization. National cancer control programmes: policies and mana-gerial guidelines. 2nd ed. Genebra. 2002.
2. Corrêa PH, Shibuya E. Administração da terapia nutricional em cuidados paliativos. Rev Bras Cancerol. 2007;53(3):317-23.
3. World Health Organization. WHO deinitions of palliative care. 2015. Acesso em 24 de julho de 2015. Disponível em: < http://www.who.int/cancer/palliative/deini-tion/en >.
4. Nordon DG, Moreno MS, Figueiredo MT, Figueiredo MG. Palliative care in alzheimer’s disease. Rev Fac Ciênc Méd Sorocaba. 2010;12(2):1-3.
5. Sociedad Española de Cuidados Paliativos. Guia de cuidados paliativos. 2008. Acesso em 24 de julho de 2015. Disponível em: <http://www.secpal.com/guiacp/index.php>. 6. Instituto Nacional de Câncer (Brasil). Consenso Nacional de Nutrição Oncológica.
Rio de Janeiro: INCA; 2009. Disponível em: <http://www.asbran.org.br/arquivos/ consenso_nutricao_oncologia.pdf>
7. Beyea SC, Nicoll LH. Writing an integrative review. AORN J. 1998;67(4):877-80. 8. Schirmer EM, Ferrari A, Trindade LC. Evolução da mucosite oral após intervenção
nutricional em pacientes oncológicos no serviço de cuidados paliativos. Rev Dor. 2012;13(2):141-6
9. Loyolla VC, Pessini L, Bottoni A, Serrano, SC, Teodoro AL, Bottoni A. Terapia nu-tricional enteral em pacientes oncológicos sob cuidados paliativos: uma análise da bioética. Saúde, Ética & Justiça. 2011;16(1):47-59.
10. Silva PB, Lopes M, Trindade LC, Yamanouchi CN. Controle dos sintomas e
interven-ção nutricional. Fatores que interferem na qualidade de vida de pacientes oncológicos em cuidados paliativos. Rev Dor. 2010;11(4):282-8.
11. Orrevall Y, Tishelman C, Permert J, Cederholm T. Nutritional support and risk sta-tus among cancer patients in palliative home care services. Support Care Cancer. 2009;17(2):153-61.
12. Muir CI, Linklater GT. A qualitative analysis of the nutritional requirements of pallia-tive care patients. J Hum Nutr Diet. 2011;24(5):470-8.
13. Hasenberg T, Essenbreis M, Herold A, Post S, Shang E. Early supplementation of pa-renteral nutrition is capable of improving quality of life, chemotherapy-related toxicity and body composition in patients with advanced colorectal carcinoma undergoing palliative treatment: results from a prospective, randomized clinical trial. Colorectal Dis. 2010;12(10):e190-e9.
14. Wong PC, Dodd MJ, Miaskowski C, Paul SM, Bank KA, Shiba GH, et al. Mucositis pain induced by radiation therapy: prevalence, severity, and use of self-care behaviors. J Pain Symptom Manage. 2006;32(1):27-37.
15. Boligon CS, Huth A. O impacto do uso de glutamina em pacientes com tumores de cabeça e pescoço em tratamento radioterápico e quimioterápico. Rev Bras Cancerol. 2011;57(1):31-8.
16. Stone R, Fliedner MC, Smiet AC. Management of oral mucositis in patients with cancer. Eur J Oncol Nurs. 2005;9( Suppl 1):S24-32.
17. Cardoso DH, Muniz RM, Schwartz E, Arrieira IC. Cuidados paliativos na assistên-cia hospitalar: a vivênassistên-cia de uma equipe multiproissional. Texto Contexto Enferm. 2013;22(4):1134-41.
18. Seredynskyj FL, Rodrigues RA, Diniz MA, Fhon JR. Percepção do autocuidado de idosos em tratamento paliativo. Rev Eletr Enf. 2014;16(2):286-96.
19. Durval PA, Vargas BL, Fripp JC, Arrieira IC, Lazzeri B, Destri K, Assunção MC. Caquexia em pacientes oncológicos internados em um programa de internação domi-ciliar interdisciplinar. Rev Bras Cancerol. 2010;56(2):207-12.
20. Bozzetti, F. Home total parenteral nutrition in incurable cancer patients: a therapy, a basic humane care or something in between? Clin Nutr. 2003;22(2):109-11. 21. Marín Caro MM, Laviano A, Pichard C, Gómez Candela C. Relación entre la
in-tervención nutricional y la calidad de vida en el paciente con cáncer. Nutr Hosp. 2007;22(3):337-50.
22. Benarroz MD, Faillace GB, Barbosa LA. Bioética e nutrição em cuidados paliativos oncológicos em adultos. Cad Saúde Pública. 2009;25(9):1875-82.