Correspondence to: Slobodan TANASKOVIĆ Institut za kardiovaskularne bolesti „Dedinje” Heroja Milana Tepića 1 11000 Beograd, Srbija drslobex@gmail.com
Коарктација трбушне аорте – приказ прва три
случаја у нашој литератури
Предраг Гајин, Слободан Танасковић, Драгослав Ненезић, Ненад Илијевски, Ђорђе Радак
Институт за кардиоваскуларне болести „Дедиње”, Београд, Србија
UVOD
Sužeweaorteododvajawabrahiocefalič nogstabladobifurkacijenazivasekoark tacija.Koarktacijatrbušneaorte(KTA)je veomaretkooboqeweičinisvega0,52% svihkoarktacija[1,2,3].Uanglosakson skojliteraturiovoteškooboqewepozna tojepodimenimamid dle aor tic syndro me i mid-aor tic dyspla stic syndro me.Premalokali zaciji,možesepodelitinasuprarenalnu (najčešća),interrenalnu,infrarenalnui difuznuformu.Stenozavisceralniharte rijajavqaseu26%slučajeva,multiplere nalnearterijesebeležeu70%,doksekod 84%bolesnikadijagnostikujestenozare nalniharterija[1,4,5,6].
Ovoretkooboqewejeposledicakonge nitalnehipoplazijeilianomalijerazvo ja,alisekaoetiološkifaktoripomiwu ineurofibromatoza[710],zračnaterapi ja,fokalnaateroskleroza[11],nespecifič ni–Takajasuov(Ta kayasu)aortoarteritis [2,1215]ifibromuskularnadisplazija [16].ObjavqenjeislučajKTAizazvanepo stavqewemkateterakrozpupčanuarteri junovorođenčeta[17].KTAseprvenstveno javqakodmladihosoba(prosek20godina) [3],premdasemožeotkritiubilokojem životnomdobu.Dvaglavnasimptomaovog
oboqewasurenovaskularnahipertenzija, odnosnosekundarnesekveledugogodišwe hipertenzije,kaoiintermitentneklau dikacijedowihekstremiteta[1,18].Tre ćisimptom,kojiseređejavqa,jestetrbu šnaangina[1,18,19].
Zlatnistandardmeđudijagnostičkim proceduramajearteriografija[1,18],ko jomseotkrivajumestoiopsegstenozeiza hvaćenostvisceralnihgranaaorte.Neop hodnajezaprocenuizboraendovaskular nogilihirurškogvidalečewa.
PRIKAZI BOLESNIKA
Uperiodu19962007.godineretrospektiv noiprospektivnosuustanovqenatribo lesnikakodkojihjedijagnostikovanaKTA. Analiziranisukliničkisimptomi(in termitentneklaudikacijeisekundarnese kvelearterijskehipertenzije)iznacibo lesti.Odneinvazivnihmetodadijagnosti keprimewenisudoplerultrazvučnapro cenaperiferneishemije(pedobrahijalni indeksi–PBI)iuobičajenomerewearte rijskogpritiska.Odinvazivnihpostupa kaprimewenajearteriografija,naosnovu kojejepostavqanadijagnozaivršenapro cenavrstelečewa.Bolesnicisulečenihi
KRATAK SADRŽAJ
Uvod U kli nič koj prak si do bro je po zna ta kon ge ni tal na ko ark ta ci ja grud ne aor te u ni vou li ga men ta ar te ri o zu ma ili aort nog lu ka. Mno go je re đa ko ark ta ci ja dis tal nog de la grud ne ili tr bu šne aor te (0,5-2%), ko ja je u an glo sak son skoj li te ra tu ri po zna ta pod ime ni ma mid dle aor tic syndro me i mid-aor tic dyspla stic syndro me. To je te ško obo qe we či je le če we zah te va mul ti di sci pli na ran pri stup.
Pri ka zi bo le sni ka U pe ri o du 1996-2007. go di ne na Kli ni ci za va sku lar nu hi rur gi ju In sti tu ta za kar di o va sku lar ne bo le sti „De di we” u Be o gra du le če na su tri bo le sni ka zbog ko ark ta ci je tr bu šne aor te (dve že ne sta re 50 i 55 go di na i če tvo ro go di šwi de čak). Oni su kli nič ki pra će ni 51-118 me se-ci. Bo le sni ci su le če ni hi rur ški baj pa som ve štač kim graf tom i tzv. pač (engl. patch) an gi o pla sti-kom i en do va sku lar no per ku ta nom tran slu mi nal nom an gi o pla sti sti-kom (PTA) sa sten tom ili bez we ga. Kod pe de se to go di šwe bo le sni ce an gi o graf ski na laz je po ka zao zna čaj no su že we su pra re nal nog seg-men ta tr bu šne aor te. Ura đen je to ra ko-ab do mi nal ni baj pas tu bu lar nim da kron skim graf tom preč-ni ka 16 mm. Kod de ča ka je an gi o gra fi jom ta ko đe po tvr đe na ko ark ta ci ja su pra re nal nog de la aor te. U pr vom ak tu pri me we na je „pač” an gi o pla sti ka, a za tim u ne ko li ko na vra ta PTA vi sce ral nih ar te ri ja. Kod pe de set pe to go di šwe bo le sni ce di jag no sti ko va na je ko ark ta ci ja tr bu šne aor te u in fra re nal-nom seg men tu. Ura đe na je PTA uz pri me nu sten ta. Na kon trol nim pre gle di ma sva tri bo le sni ka su bi-la bez simp to ma obo qe wa.
Za kqu čak Ko ark ta ci ja tr bu šne aor te je pa to lo ški en ti tet ko ji se iz u zet no ret ko sre će u va sku lar-noj hi rur gi ji. An gi o gra fi ja je od ve li kog zna ča ja za po sta vqa we di jag no ze i ne po sred nu kon tro lu re-zul ta ta hi rur škog i ne hi rur škog le če wa. Kom bi na ci ja hi rur škog i en do va sku lar nog le če wa je kod na ših bo le sni ka da la vr lo do bre re zul ta te u po sma tra nom pe ri o du.
rurškibajpaspostupkomitzv.pač(engl.patch)angi oplastikomiendovaskularnoperkutanomtranslumi nalnomangioplastikom(PTA)sastentomilibezwe ga.Periodkliničkogpraćewatrajaoje51118meseci.
Prvi bolesnik
Godine1996.naKlinikuzavaskularnuhirurgijuIn stituta„Dediwe”primqenapedesetogodišwažena kojajenekolikogodinaranijeimalaintermitentne klaudikacijeihipertenzivnuencefalopatiju.Tokom kliničkogpregledaustanovqenjeizostanakarterij skihpulzacijauobeprepone.PBIsunaobestrane bili0,61.Arteriogramjeotkriohipoplazijuaorte usuprarenalnomsegmentu(Slika1).
Bolesnicajeoperisanauoktobruistegodine,apo torakofrenolaparotomijiurađenjeaortnoaortni bajpasdakronskimtubularnimgraftomprečnika16 mm.ObeanastomozesukreiranepotipuTL,prok simalnajeformirananazavršnideogrudneaorte (Slika2),adistalnanainfrarenalnisegmenttrbu šneaorte(Slika3).Tokomoperacijejeutvrđenoda
suoberenalnearterijezadovoqavajućegprečnikaida ćeprotokkrozwihbitiodgovarajući,teseodustalo odwihoverekonstrukcije,štoseprehirurškogle čewarazmatralokaomogućnost.
Drugi bolesnik
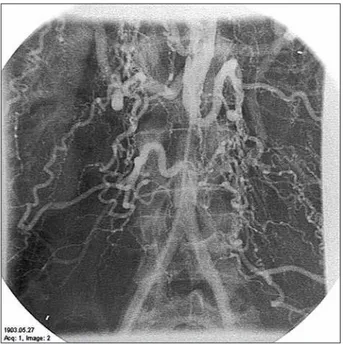
Godine1998.nabolničkolečewejeprimqenčetvo rogodišwidečakkodkojegjeodkliničkihsimpto madominiralahipertenzivnaencefalopatija,adve godineranijepogrešnojelečenpoddijagnozomepi lepsije.Preponskepulzacijebilesujedvapalpabil ne,aPBIsubili0,55naobestrane.Arteriografi jomjepotvrđenadifuznastenozasuprarenalneiin frarenalneaorte,uzpostojaweleveakcesornerenal nearterije(Slika4).
Bolesnikjeoperisanunovembruistegodinetako đeprimenomtorakofrenolaparotomije,uzlevostra numedijalnuvisceralnurotacijupoMetoksu(Mat-tox).Primewenaje„pač”angioplastikasuženogseg mentateflonskomzakrpom(Slika5).Zbogstenozavi sceralnihgranatrbušneaorte,bolesnikujeutrina vrataurađenaPTA:neposrednonakonoperacijeuči Слика 1. Коарктација супрареналне артерије код педесетого ди
шње болеснице
Figure 1. Suprarenal coarctation in a fiftyyearold female patient
Слика 2. Артериограм после аортоаортног бајпаса (проксимална анастомоза)
Figure 2. Arteriography after aortoaortal bypass (proximal ana stomosis)
Слика 3. Артериограм после аортоаортног бајпаса (дистална анастомоза)
Figure 3. Arteriography after aortoaortal bypass (distal anastomosis)
Слика 4. Дифузна форма коарктације трбушне аорте код четворо го дишњег дечака
Слика 5. Артериограм после „пач” ангиопластике трбушне аорте Figure 5. Arteriography after abdominal aorta patch angioplasty
Слика 6. Коарктација инфрареналне артерије код педесетпето го дишње болеснице
Figure 6. Infrarenal coarctation in a fiftyfiveyearold female patient
Слика 7. Артериограм после ПТА и уградње стента Figure 7. Arteriography after PTA and stent placement wenajePTAleverenalneiakcesornerenalnearte
rije,godinudanakasnijegorwemezenteričneidesne renalnearterije,anakondvegodinetrunkusaceli jakusaiponovodesnerenalnearterije.
Treći bolesnik
Uaprilu2003.godinenabolničkolečewejeprimqe napedesetogodišwaženakodkojesuodkliničkih simptomadominiraleintermitentneklaudikacije uznormalnevrednostiarterijskogpritiska.Prepon skihpulzacijanaobestranenijebilo,aPBIjebio 0,66.Arteriogramjepotvrdioprstenastusubokluzi juinfrarenalnogsegmentatrbušneaorte(Slika6).
Umajuistegodinebolesnicajepodvrgnutaleče wuprimenomPTAuzpostavqawestentanamestuko arktacije(Slika7).
DISKUSIJA
Aortnoaortnibajpasjeidealanpostupakzarešava weishemijedowihekstremiteta[1,18,20,21],aade kvatnaregulacijaarterijskogpritiskaprimarni ciqlečewabolesnikasaKTA.Budućidajehiper tenzijadominantansimptom,revaskularizacijabu bregajeizuzetnovažna.Primewujusereimplanta cijarenalniharterija,„pač”plastika,interpozici jaibajpasprocedure(aortorenalni,ilijačnorenal ni,hepatorenalniisplenorenalnibajpas)[4,2225], aponekadjeneophodnainefrektomija[26,27].Sve višeautoraizveštavaouspehuPTA[2831]ipostu pakaugradwestenta[32,33,34]kodKTA,paikodTa kajasuovogarteritisa.
Lečewesvatribolesnikaprikazanauovomradu proteklojebezkomplikacija.Nasvimkontrolama
PBIsubiliufiziološkimgranicama,aobebole snice,kodkojihsuprelečewadijagnostikovanein termitentneklaudikacije,bilesubezsimptomaobo qewa.Kodbolesniceidečakakojisubolovaliodhi pertenzivneencefalopatijevrednostiarterijskog pritiskalakosusekontrolisalemalimdozamabe tablokatora.
LITERATURA
1. Patman RD, Shutze WP. Nonatherosclerotic vascular diseases and conditions. In: Dean RH, Jao JST, Brewster DC, editors. Current Diagnosis and Treatment in Vascular Surgery. Connecticut: Appleton & Lange; 1995. p.17292.
2. Connolly JE, Wilson SE, Lawrence PL, Fujitani RM. Middle aortic syndrome: distal thoracic and abdominal coartation, a disorder with multiple etiologies. J Am Coll Surg. 2002; 194(6):77481. 3. Bates RL, Khourty RT, Rahbar A. An unusual manifestation of congenital abdominal aortic coarctation. J Cardiovasc Surg (Torino). 1987; 28(6):7402.
4. Lillehei CW, Shamberger RC. Staged reconstruction for middle aortic syndrome. J Pediatr Surg. 2001; 36(8):12524.
5. Bartolucci R, Bertoletti GB, Pogany G, Sammarco S, Rabitti G. Coartacion of the abdominal aorta. G Chir. 1999; 20(89):33840. 6. Durand I, Blaysat G, David N, Lacombe M, Tron P. Hypoplasia of
abdominal aorta, rare cause of hypertension in childhood. Arch Pediatr. 1995; 2(12):11736.
7. Criado E, Izguierdo L, Lujan S, Puras E, del Mar Espino M. Abdominal aortic coarctation, renovascular hypertension, and
neurofibtomatosis. Ann Vasc Surg. 2002; 16(3):3637. 8. Welch TJ, McKusick MA. Abdominal coarctation due to
neurofibromatosis. AJR Am J Roentgenol. 1993; 160(6):13134. 9. Zwaan M, Heidbuchel K. Hypertension during neurofibromatosis
with recurring renal artery stenosis and infrarenal aortic coarctation. Rofo Fortschr Geb Rongenstr Neuen Bildgeb Verfahr. 1991; 154(1):1156.
10. Tenschert W, Holdener EE, Haertel MM, Senn H, Vetter W. Secondary hypertension and neurofibromatosis: bilateral renal arterystenosis and coarctation of the abdominal aorta. Klin Wochenschr. 1985; 63(13):5936.
11. Joyce WJ. Uncommon arteriopathies. In: Rutherford RB, editor. Vascular Surgery. Philadelphia: WB Saunders Company; 1995. p.295310.
12. Bahl VK, Chandar S, Taneja K. Selfexpanding wallstent for management of severe abdominal coarctation due to nonspecific aortoarteritis. Indian Heart J. 1997; 49(2):2324.
13. Kashani IA, Skalansky MS, Movahed H, Lucas VW, Rothman A. Successful balloon dilatation of an abdominal coarctation of the aorta in patient with presumed Takayasu’s aortitis. Cathet Cardiovasc Diagn. 1996; 38(4):4069.
14. Akimov OV. Nonspecific aortic arteritis with abdominal aortic coarctation. Arkh Patol. 1995; 57(3):712.
15. Roques X, Bourdeaud’hui A, Choussat A, Riviere J, Laborde N, Hafez A, et al. Coarctation of the abdominal aorta. Ann Vasc Surg. 1988; 2(2):13844.
16. Voung PN, Trinh AC, Lagneau P, Camilleri JP. Coarctation of the abdominal aorta and stenosis of the left ranal artery with hypertension caused by fibrodysplasia. Arch Pathol Lab Med. 1989; 113(7):80911.
17. Adelman RD, Morrell RE. Coarctation of the abdominal aorta and renal renal artery stenosis related to an umbilical artery catheter placement in a neonate. Pediatrics. 2000; 106(3):E36.
18. Terramani TT, Salim A, Hood DB, Rowe VL, Weaver FA.Hypoplasio of the descending thoracic and abdominal aorta: a report of two cases and review of the literature. J Vasc Surg. 2002; 36(4):8448. 19. Le Minh T, Hoang AD, Dupont P, Motte S, el Douaihy M, Ferreira J, et
al. Abdominal aortic coarctation with splanchnic arterial occlusion. Acta Chir Belg. 1999; 99(5):2636.
20. Sinci V, Kalaycioglu S, Aydin H. Transdiaphragmatic graft replacement for coarctation suprarenal abdominal aorta. Int Surg. 1999; 84(2):11821.
21. Abad C, Ninot S, Barriuso C, Mulet J. Coarctation of the abdominal aorta. Surgical treatment. Angiologia. 1989: 41(4):14955. 22. Reihel L, Sandmann W. Coarctation of the thoracoabdominal aorta.
Chirurg. 1998; 69(7):7538.
23. Cohen JR, Birnbaum E. Coarctation of the abdominal aorta. J Vasc Surg. 1988; 8(2):1604.
24. Calabrese E, Malatino L, Petrilo G, Stancanelli B, Stancanelli G. Coarctation of the abdominal aorta and multiple ranal artery stenosis. Case report. Scand J Thorac Cardiovasc Surg. 1988; 22(1):8791.
25. Vascaro PS, Myers JC, Smeald WL. Surgical correction of the abdominal aortic coarctation and hypertension. J Vasc Surg. 1986; 3(4):6438.
26. Bergqvist D, Bergntz SE, Ekberg M, Jonsson K, Takolander R. Coarctation of the abdominal aorta in elderly patients. Acta Med Scand. 1988; 223(3):27580.
27. Boontje AH. Uncommon congenital anomalies of the aorta. J Cardiovasc Surg. 1979; 20(1):338.
28. Adwani S, De Giovanni JV. Percutaneous transluminal ballon angioplasty of abdominal coarctation in an infant. Pediatr Cardiol. 1996; 17(5):3468.
29. Kashani IA, Sklansly MS, Movahed H. Successful balloon dilatation of an abdominal coarctation of the aorta in patient with presumed Takayasu’s aortitis. Cathet Cardiovasc Diagn. 1996; 38(4):4069. 30. Schechter C, Angelini P, Treistman B. Percutaneous balloon catheter
angioplasty of coarctation of the abdominal aorta: report of two cases. Cathet Cardiovasc Diagn. 1985; 11(4):4017.
31. Nanni GS, Hawkins IF, Alexander JA. Percutaneous transluminal angioplasty of an abdominal aortic coarctation. AJR Am J Roentgenol. 1983; 140(6):123941.
32. Guia JM, Castro FJ, Gracian M, Gilabert A, García E. Coarctation of the abdominal aorta. Treatment by stent placement. Rev Esp Cardiol. 2001; 54(11):13325.
33. Eliason JL, Passman MA, Guzman RJ, Naslund TC. Durability of percutaneus angioplasty and stent implantation for the treatment of abdominal aortic coarctation. Vasc Surg. 2001; 35(5):397401. 34. BrzezinskaRajszys G, Qureshi SA, Ksiazyk J, Zubrzycka M, Kosciesza
SUMMARY
Introduction Congenital coarctation of the thoracic aorta at the ligamentum arteriosum or the aortic arch is well recognized. But a much less common variety (0.52.0%) of aortic coarcta tion is located in the distal thoracic aorta or abdominal aorta or both and is often called ”middle aortic syndrome” or ”mid aortic dysplastic syndrome”. This represents serious pathologi cal condition and indicates multidisciplinary therapy approach. Outline of Cases From 1996 to 2007, at the Vascular Surgery Clinic of the Institute for Cardiovascular Diseases „Dedinje”, Belgrade, three patients were treated due to abdominal aorta coarctation, two females aged 55 and 50 and a 4yearold child. The patients were treated surgically (bypass with a prosthetic graft and patch angioplasty) and endovascular percutaneous transluminal angioplasty (PTA) with and without a stent. The followup period was 370 months. In the 50yearold patient, angiography showed severe narrowing of the suprarenal
segment of the abdominal aorta. Thoracoabdominal bypass with a 16 mm dacronic tubular graft was performed. In the 4yearold patient angiography also showed a suprarenal aorta narrowing. In the first act patch angioplasty was performed and after PTA of the visceral arteries was done on several occasions. In the 55yearold patient, after diagnostic angiography, infra renal aorta coarctation was registered. PTA was performed with stent placement. All patients were asymptomatic on control checkups.
Conclusion Abdominal coarctation is a pathological disease which is seldom found in vascular surgery. Angiography is of major importance for setting the diagnosis and for the control of the results of surgical and nonsurgical treatment. The combi nation of surgical and endovascular treatment in our patients showed very good results in the studied period.
keywords: abdominal aorta coarctation; transluminal percu taneus angioplasty; surgical treatment
Abdominal Aorta Coarctation: The First Three Case Reports in Our Literature
Predrag Gajin, Slobodan Tanasković, Dragoslav Nenezić, Nenad Ilijevski, Djordje Radak Institute for Cardiovascular Diseases ”Dedinje”, Belgrade, Serbia