www.revportcardiol.org
Revista
Portuguesa
de
Cardiologia
Portuguese
Journal
of
Cardiology
ORIGINAL
ARTICLE
Cardiovascular
risk
in
HIV-infected
individuals:
A
comparison
of
three
risk
prediction
algorithms
Sara
Policarpo
a,b,∗,
Teresa
Rodrigues
c,
Ana
Catarina
Moreira
d,
Emília
Valadas
eaServic¸odeDietéticaeNutric¸ão,HospitaldeSantaMaria,Lisboa,Portugal
bUniversidadedeLisboa,FaculdadedeMedicina,LaboratóriodeNutric¸ão,Lisboa,Portugal cUniversidadedeLisboa,FaculdadedeMedicina,LaboratóriodeBiomatemática,Lisboa,Portugal
dEscolaSuperiordeTecnologiadaSaúdedeLisboa,InstitutoPolitécnicodeLisboa,PortugalH&TRC---CentrodeInvestigac¸ão
emSaúdeeTecnologia,Portugal
eUniversidadedeLisboa,FaculdadedeMedicina,ClinicaUniversitáriadeDoenc¸asInfecciosas,Lisboa,Portugal
Received27December2017;accepted21October2018 Availableonline12September2019
KEYWORDS Cardiovascularrisk; Metabolicsyndrome; HIV/Acquired immunodeficiency syndrome; Portugal Abstract
Introduction:Cardiovascular(CV)riskisknowntobeincreasedinHIV-infectedindividuals.Our aimwastoassessCVriskinHIV-infectedadults.
Methods:CVriskwasestimatedforeachpatientusingthreedifferentriskalgorithms:SCORE, theFraminghamriskscore(FRS),andDAD.Patientswereclassifiedasatlow,moderateorhigh CVrisk.Clinicalandanthropometricdatawerecollected.
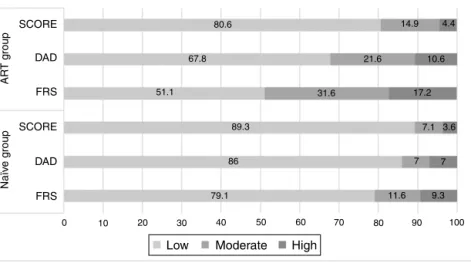
Results:Weincluded571HIV-infectedindividuals,mostlymale(67.1%;n=383).Patientswere dividedintotwogroupsaccordingtoantiretroviraltherapy(ART):naïve(7.5%;n=43)orunder ART(92.5%;n=528).ThemeantimesinceHIVdiagnosiswas6.7±6.5yearsinthenaivegroupand 13.3±6.1yearsintheARTgroup.Metabolicsyndrome(MS)wasidentifiedin33.9%(n=179)and 16.3%(n=7)ofparticipantsintheARTandnaïvegroups,respectively.MSwasassociatedwithART (OR=2.7;p=0.018).Triglycerides≥150mg/dl(OR=13.643,p<0.001)wasoneofthemajorfactors contributingtoMS.Overall,highCVriskwasfoundin4.4%(n=23)ofpatientswhentheSCORE toolwasused,in20.5%(n=117)usingtheFRS,andin10.3%(n=59)usingtheDADscore.The observed agreement between the FRS and SCORE was 55.4% (k=0.183, p<0.001), between the FRS andDAD 70.5% (k=0.465,p<0.001), and between SCORE and DAD 72.3% (k=0.347, p<0.001).
Conclusion: On thebasisofthethree algorithms, wedetected ahigh rateofhighCV risk, particularlyinpatientsunderART.TheFRSwasthealgorithmthatclassifiedmostpatientsin thehighCVriskcategory(20.5%).Inaddition,ahighprevalenceofMSwasidentifiedinthis patientgroup.
©2019PublishedbyElsevierEspa˜na,S.L.U.onbehalfofSociedadePortuguesadeCardiologia.
∗Correspondingauthor.
E-mailaddress:sara.policarpo@chln.min-saude.pt(S.Policarpo).
https://doi.org/10.1016/j.repc.2019.08.002
0870-2551/©2019PublishedbyElsevierEspa˜na,S.L.U.onbehalfofSociedadePortuguesadeCardiologia.
This is an open access article under CC BY-NC-ND license. (http://creativecommons.org/licenses/by-nc-nd/4.0/)
This is an open access article under CC BY-NC-ND license (http://creativecommons.org/licenses/by-nc-nd/4.0/)
PALAVRAS-CHAVE
Riscodedoenc¸a cardiovascular;
Síndromemetabólica;
VIH/SIDA; Portugal
RiscocardiovasculareminfetadosporVIH:comparac¸ãodetrêsferramentasde avaliac¸ão
Resumo
Introduc¸ão:Oriscocardiovascular(RCV)podeestaraumentadoemindivíduoscominfec¸ãopor VírusImunodeficiênciaHumana(VIH).OobjetivodestetrabalhofoiavaliaroRCVemadultos infetadosporVIH.
Métodos: ORCV foiestimadoutilizando trêsalgoritmosdiferentes,Score,FraminghamRisk Score(FRSs-CVD)eDAD;osparticipantesforamclassificadosapresentandoRCVbaixo,moderado ouelevado.Recolheram-sedadosclínicoseantropométricos.
Resultados: Incluíram-se571indivíduos,maioritariamentedogéneromasculino(67,1%;n=383). Dividiram-seosparticipantesem doisgrupos,come semterapêutica antirretroviral(cTAR): naïve(7,5%;n=43)versuscTAR(92,5%;n=528).Otempomédiodesdeodiagnósticodainfec¸ão porVIHfoi6,7±6,5anosnogruponaïvee13,3±6,1anosnogrupocART.Asíndromemetabólica (SM)foiidentificadaem33,9%(n=179)eem16,3%(n=7)dosparticipantes,respetivamenteno grupocARTenogruponaïve.Verificou-seumRCVelevadoem4,4%(n=23)dosparticipantes,com recursoàferramentaScore,em20,5%(n=117)utilizandoaFRSseem10,3%dosparticipantes (n=59)utilizando aferramenta DAD.A concordânciaobservadaentreFRSs eScorefoi55,4% (k=0,183;p<0,001), entreFRSs e DAD70,5% (k=0,465;p<0,001)e entreScore eDAD 72,3% (k=0,347;p<0,001).
Conclusão:Comrecursoaosalgoritmosutilizados,identificou-seumapresenc¸asignificativade elevado RCV, sendo a ferramenta FRSs-CVD a que classificou mais indivíduos na categoria deRCVelevado(20,5%),esimultaneamenteverificou-seumaprevalênciaelevadadeSM. ©2019PublicadoporElsevierEspa˜na,S.L.U.emnomedeSociedadePortuguesadeCardiologia. Este ´e um artigo Open Access sobuma licenc¸a CC BY-NC-ND(http://creativecommons.org/ licenses/by-nc-nd/4.0/).
Introduction
InEuropean countries in recent years,cardiovascular
dis-ease(CVD)hasbeenidentifiedasamajorcauseofmortality
inhumanimmunodeficiencyvirus(HIV)-infectedindividuals,
accountingfor15%ofalldeathsinthispopulation.1---3In
Por-tugal,CVDisthemajorcauseofdeathoverall,butmortality
fromCVDinthegeneralpopulationis stilllowerthanthat
reportedintheHIVpopulation.Also,themeanageofdeath
inpatientswithHIVinPortugalissignificantlylowerthanin
thegeneralpopulation(52vs.81years).4
Cardiovascular (CV) risk in theHIV-infected population
hasbeenshowntobehigh,anestimated50%higherthanin
uninfectedindividuals,althoughsomeofthedataarestill
controversial.6---11 Traditionalrisk factors such assmoking,
which are particularly prevalent in this population,
con-tributetothisincreasedrisk.1,2,6,11---16Otherfactorsinclude
substance abuse6 and changes in lipid profile1,8,12,15,17
andglucosemetabolism, withincreased insulinresistance
and/orimpairedinsulinsecretion.8,18HIVinfectionitself,as
wellasinflammation andantiretroviraltherapy (ART),are
furthercontributingfactorsinthispopulation.11
Overall,obesityandhigherwaistcircumference(WC)are
knowncauses ofincreasedCVrisk, andinsulinresistance,
changes in lipid profile and increased WC19,20 have been
associatedwithHIVinfectionandtreatment.19,20
While increased WC is the key factor for defining the
presenceof metabolic syndrome (MS)in the non-infected
population,19 in HIV-infected individuals MS is better
identified by increased triglycerides (TG) and decreased
high-density lipoprotein cholesterol (HDL-C). It should be
alsonotedthatcardiovasculareventsoccuratmuchyounger
agesintheHIVpopulation.20
AsinthegeneralEuropeanpopulation,obesityisonthe
riseamongHIV-infectedindividuals.17---24InPortugal,obesity
andCVDarehighlyprevalentandcardiovasculareventsare
oneoftheleadingcausesofdeath.5
Cardiovascularriskpredictionalgorithmsweredeveloped
innon-HIV-infectedpopulationsandmaynotaccurately
pre-dict riskfor HIV-infectedindividuals,sincetheetiology of
CVD inthispopulation maybedifferent.The Framingham
riskscore(FRS)calculatesCVDriskandpredictsfuture
coro-nary heart disease events at 10 years. However, the FRS
may wrongly estimate the risk in populations other than
theUSpopulation,andtheEuropeanSociety ofCardiology
accordinglydevelopedandrecommendstheuseofthe
Sys-tematic CoronaryRisk Evaluation (SCORE) tool25 to assess
CVDriskinthegeneralpopulation.TheDataCollectionon
AdverseEvents ofAnti-HIVDrugs(DAD) groupdevelopeda
CVD risk equation specificallydesigned for the HIV
popu-lation, which includes exposure toHIV treatment (use of
indinavir,lopinavir/ritonavirandabacavir),aswellas
tradi-tionalCVriskfactors.26
This study aims to estimate the risk of CVD in
HIV-infected adults, to assess the agreement between the
FRS, SCOREandDAD algorithms,tostudy therelationship
between CV risk and MS in HIV-infected individuals, and
to compare the prevalence of traditional cardiovascular
factorswiththenon-infectedpopulation.Giventheburden
identificationofpatientsathighCVriskcouldleadtomore
tailoredlifestylecounselingandmoreaggressivetreatment
ofcomorbidities.27---29
Methods
Across-sectionalstudywascarriedoutat theDepartment
ofInfectiousDiseases,SantaMariaUniversityHospital,
Lis-bon, Portugal, from December 2013 to May 2014. During
the study period, at least five consecutive HIV-infected
adultswere interviewedper day, randomly selected from
thescheduledappointmentsofthatday. Weaimedto
col-lectasampleofmorethan490patientstoensurethatthe
studypopulation wasrepresentative.Ages rangedfrom18
to65years,andtheinterviewwasperformedonthesame
dayasthehospitalappointment.Exclusioncriteriaincluded
pregnancy, hospitalization in the previous three months,
presenceofopportunisticinfections,kidneyorliverfailure,
institutionalization,residenceoutsidePortugal,orinability
tounderstandandsigntheinformedconsentform.Patients
withknownCVD(coronaryarterydisease,myocardial
infarc-tion,angina,ischemicstroke,hemorrhagicstroke,transient
ischemic attack, peripheral arterial disease and/or heart
failure)werealsoexcluded.Demographicinformation(age,
gender,race),clinicaldata(smokingstatus,familyhistoryof
cardiovascularevents,diagnosisofdiabetesand/or
hyper-tension,timeofHIVdiagnosis),totaltimeandtypeofART,
antihypertensiveorlipid-loweringtherapy,laboratory
mark-ers (CD4+lymphocytecount andviral load,blood glucose,
totalcholesterol,HDL-C,LDLcholesterol,TG)andsystolic
anddiastolicblood pressure(SBPandDBP)werecollected
frommedicalrecords.
CVrisk wasestimated foreach patientusingthree
dif-ferentrisk algorithms: SCOREandthe FRS30,31 for 10-year
riskestimation,andtheDADriskequationforfive-yearrisk
estimation.32
SCORE estimates the risk over a 10-year period of a
firstfatalatheroscleroticevent(suchasmyocardial
infarc-tion, cerebrovascular disease, or other occlusive arterial
disease,andincludingsuddencardiacdeath).Thealgorithm
includesgender,age,totalcholesterol,SBPandsmoking
sta-tus.TheFRSestimates absoluteriskovera10-yearperiod
of cardiovascular events (defined as coronary artery
dis-ease,myocardialinfarction,coronaryinsufficiency,angina,
ischemic stroke, hemorrhagic stroke, transient ischemic
attack, peripheral arterial disease, or heart failure). The
adapted algorithm,developedonthe basisof theoriginal
FraminghamscaletobeapplicableinHIV,encompasses
gen-der,age,smokingstatus,presenceofdiabetes,presenceof
leftventricular hypertrophy, totalcholesterol, HDL-C and
SBP. DAD estimates the risk of developing coronaryheart
diseaseandmyocardialinfarctionwithinafive-yearperiod.
The algorithmincludesthefollowing factors:gender, age,
SBP,smokinghabits,familyhistoryofCVD,presenceof
dia-betes,totalcholesterol,HDL-C,andexposure toARTwith
indinavir,lopinavirandabacavir.
IndividualswereclassifiedaspresentinglowCVriskwith
SCORE<4%,FRS<10%orDAD<5%;moderatetohighCVrisk
with SCORE 5-10%, FRS 10-20% or DAD 5-10%; or high CV
risk withSCOREor DAD ≥10%and FRS ≥20%.The original
algorithm for each tool was used and individual risk was
determinedusingIBMSPSS®.
Multivariate logistic regression analysis was performed
usingall factors significantly (p<0.1) associated withhigh
CVrisk(age,gender,smokingstatus,familyhistoryofCVD,
bloodglucose,totalcholesterol,LDL,HDL-C,TG,bodymass
index[BMI],WCandART).
Weight and height were measured with participants
wearinglightclothesandbarefoot,usingacalibratedscale.
These parameters were used to calculate BMI.33 WC was
measuredhalfway betweenthelowest point ofthecostal
margin and the top of the iliac crest. Male patients with
WC≥94cmandfemalepatientswithWC≥80cmwere
con-sideredtohave high WC.34 MS wasdefined inaccordance
withthestandardsoftheInternationalDiabetesFederation,
bythepresenceofatleastthreeofthefollowingcriteria:
increasedWC, TG≥150 mg/dl, HDL-C<40 mg/dlfor men
and <50 mg/dl for women, SBP ≥130 mmHg and/or DBP
≥85mmHgandfastingbloodglucose≥100mg/dl.
Pharma-cologicaltherapyforanyoftheseconditionswasconsidered
analternativecriterion.34
Statistical
analysis
Demographicandclinicalvariableswereanalyzedbyoverall
groupandbygender.Continuousvariablesweresummarized
asmeanandstandarddeviationandcategoricalvariablesas
frequencyandpercentage.Thechi-squaretestwasusedto
determine the independence of categorical variables and
theStudent’s ttest or analysis ofvariance, withmultiple
comparisonsadjustedwiththeBonferronicorrection,were
usedforcontinuousvariables.Unadjustedandadjustedodds
ratios(OR)andthecorresponding95%confidenceintervals
(CI)andp-valueswerereportedforeachanalysis.The
for-wardstepwisemethodwasusedforthemultivariatelogistic
regressionanalysis.Themodel’sgoodnessoffitwasassessed
by the Hosmer-Lemeshow test (at least 80% of expected
valueswere≥5).Thesignificancelevelwassetat5%.All
sta-tisticalanalyseswereperformedwithIBMSPSS® software,
version22.0.
ThestudywasapprovedbytheEthicsCommitteeofSanta
Maria Hospital and authorized by the hospital’s Board of
Directors.Allsubjectsprovidedwritteninformedconsent.
Results
Fromthe 3000HIV-infectedadultpatientsfollowed inthe
DepartmentofInfectiousDiseases,719 wererecruitedfor
participation during the study period. Thirty-five did not
consenttoparticipateand113didnotmeettheeligibility
criteria.
Overall, 571 patients were included. Most were male
(n=383; 67.1%) and Caucasian (n=524; 91.3%). Mean age
was46.4±8.9 years; time since HIV diagnosis was 12.8±
6.4 years and only 12 patients had been diagnosed in
theprevious year. Mostpatients(92.5%) hadbeen onART
for 10.4±6.1years.Patientswith aCD4+count >500/mm3
at the time of the study had a longer mean time since
HIV diagnosis than patients with a CD4+count <200/mm3
(13.2±6.2vs. 10.4±7.0 years;p=0.026) and had been on
Table1 Characteristicsofthestudypopulation,overallandbyage.
Overall Age>40years(n=445) Age≤40years(n=126) pb
FamilyhistoryofCVD 52.9(302) 55.3(246) 44.4(56) 0.031 Currentsmoker 53.1(303) 51.9(231) 57.1(72) >0.05 SBP,mmHga 132.4±16.2(86-199) 133.5±16.5 128.1±14.2 0.004 DBP,mmHga 78.2±11.1(52-118) 78.8±11.1 76.0±10.7 0.014 HBP 19.6(112) 24.0(107) 4.0(5) <0.001 Bloodglucose,mg/dla 95.4±20.9(56-300) 96.9±22.0 90.1±15.1 0.001 Diabetes 5.1(29) 6.1(27) 1.6(2) 0.040 TC,mg/dla 191.2±40.7(94-347) 196.6±40.1 172.3±33.9 <0.001 TC≥200mg/dl 38.0(217) 44.0(196) 16.7(21) <0.001 HDL-C,mg/dla 50.9±15.3(22-131) 51.8±15.9 47.8±12.6 0.01 HDL-C<40(M)or<50(F)mg/dl 27.5(157) 26.7(119) 30.2(38) >0.05
HIVdiagnosis,years 12.8±6.4(0-29) 13.9±6.1 8.7±5.6 <0.001
CD4+count,/mm3
Mean 688.7±346.8(22-2269) 702.6±357 639.3±301 >0.05
<200 5.1(29) 5.8(26) 2.4(3) >0.05
200-499 17.9(162) 26.7(119) 34.1(43)
≥500 66.7(380) 67.4(300) 63.5(80)
Viralload(<50copies) 83.9(474) 87.5(384) 71.4(90) <0.001
ART,years 10.4±6.1 11.7±5.8 6.0±4.9 <0.001 Weight,kga 70.8±14.3(39.6-122.1) 71.1±14.4 69.5±13.8 >0.05 BMI,kg/m2a 24.7±4.5(15.4-43.3) 24.9±4.5 23.7±4.1 0.004 Underweight 4.9(28) 3.8(17) 8.7(11) 0.006 Normalweight 54.8(313) 52.6(234) 62.7(79) Pre-obesity 28.9(165) 31.0(138) 21.4(27) Obesity 11.4(65) 12.6(56) 7.1(9) WC,cma 88.5±12.8(60.1-129.0) 90.1±12.7 83.1±11.4 <0.001 WCabovecut-off 41.9(239) 46.7(207) 25.4(32) <0.001
ART:antiretroviraltherapy;BMI:bodymassindex;DBP:diastolicbloodpressure;F:female;HBP:highbloodpressure;M:male;SBP: systolicbloodpressure;TC:totalcholesterol;WC:waistcircumference.
aMean±standarddeviation(minimum-maximum)or%(n). b chi-squareorStudent’sttest.
(11.0±5.9 vs. 8.2±7.0 years; p=0.002). Male participants
presented higher blood glucose and SBP levels. Although
more than half of the participants had normal weight as
definedbyBMI(n=313;54.8%),40.3%(n=230)presentedBMI
≥25kg/m2,whichindicatesexcessweight.Femalepatients
presented a higher prevalence of WC above the defined
cut-off(35.2%vs.36.3%inmales;p<0.001).Regarding
tra-ditionalCVriskfactors,52.9%(n=302)hadafamilyhistory
ofcardiovascularevents,53.1%(n=303) weresmokersand
5.1%(n=29) werediabetic.Almostonethird hadahistory
ofsubstanceabuse(n=166,29.1%).Table1presentspatient
characteristicsandprevalenceofCVDriskfactors.No
signif-icantdifferenceswerefoundbetweengenders,apartfrom
higherHDL-Cinfemalepatients(58.0±16.7mg/dlvs.47.5±
13.3mg/dlinmalepatients;p<0.001)andhigherSBPinmale
patients(134.2±15.4mmHgvs.128.8±17.1mmHginfemale
patients;p<0.001).
Metabolic
syndrome
Of the 571 individuals assessed, 186 (32.6%) had
clini-calcriteriafor MS. Those withMSwere mostlyCaucasian
(n=172; 92.5%) and were older (48.7±8.5 vs. 44.4±
8.8years;p<0.001),hadHIVinfectionforlonger(13.7±6.3
vs.12.4±6.4years;p=0.019)andwereexposedtoARTfor
longer(11.6±5.9vs.9.8±6.2years;p<0.001)than
partici-pantswithout MS. An association wasfound between ART
andthepresenceofMS(OR=2.6[95%CI:1.1-6.0];p=0.018).
IntheMSgroup,96.2%(n=179)wereunderART.
TG≥150mg/dlandahighWCwerefoundtobethemajor
diagnosticfactorsofMS(OR=13.6[95%CI:8.9-20.7];p<0.001
andOR=13.1[95%CI:8.5-20.1];p<0.001,respectively).
Regardinganthropometricparameters,participantswith
MS had higher mean weight (79.5±13.3 vs. 66.5±12.8
kg; p<0.001) and a higher BMI (27.5±4.2 vs. 23.3±
3.9kg/m2,p<0.001)thanparticipantswithoutMS.
Cardiovascular
risk
assessment
Overall,CVrisk showedwidevariationandcalculatedrisk
variedaccordingtothealgorithmused.AhighCVriskwas
found in 4.4% (n=23) of patients when the SCORE tool
was used,in 20.5% (n=117) when FRS wasapplied and in
10.3%(n=59)ofpatientsusingtheDADscore.Patientsunder
ART(n=528)hadasignificantlyhigherCVriskthanART-naïve
patients(n=43)withallthreetoolsused(Figure1).Forthis
reason,furtheranalysiswasperformed intwogroups: the
AR T g roup Naïv e g roup SCORE DAD DAD FRS FRS 0 10 20 30 40 79.1 86 89.3 51.1 67.8 80.6 31.6 17.2 7.1 3.6 7 7 11.6 9.3 10.6 14.9 4.4 21.6 50 60 70 80 90 100 SCORE
Low Moderate High
Figure1 Cardiovascularriskinthestudy populationestimatedbytheSystematicCoronaryRiskEvaluation(SCORE),theData CollectiononAdverseEventsofAnti-HIVDrugs(DAD)riskequationandtheFraminghamriskscore(FRS).ART:antiretroviraltherapy.
Table2 Characteristicsofthestudypopulationbytreatmentgroup.
ARTgroup(n=528) Naïvegroup(n=43) pb
Age,years 47.0±8.5 39.9±11.7 <0.001 FamilyhistoryofCVD 52.3(276) 60.5(26) 0.381 Currentsmoker 53.4(282) 48.8(21) 0.563 SBP,mmHga 132.5±16.5 131.7±11.7 0.564 DBP,mmHga 78.1±11.3 78.6±8.1 0.779 HBP 20.6(109) 7.0(3) 0.003 Bloodglucose,mg/dla 95.9±21.2 90.1±14.3 0.081 Diabetes 5.1(27) 4.7(2) 0.894 TC,mg/dla 191.7±41.3 184.8±31.7 0.289 TC≥200mg/dl 39.2(207) 23.3(10) 0.038 TG,mg/dla 144.0±93.6 118.2±70.7 0.077 TG≥150mg/dl 35.8(189) 25.6(11) 0.177 HDL-C,mg/dla 51.3±15.6 46.3±10.4 0.039 HDL-C<40(M)or<50(F)mg/dl 26.3(139) 41.9(18) 0.028
HIVdiagnosis,years 13.3±6.1 6.7±6.6 <0.001
CD4+count,/mm3
Mean 697.4±348.1 581.1±315.4 0.034
<200 4.4(23) 14.0(6) 0.018
200-499 28.2(149) 30.2(13)
≥500 67.4(356) 55.8(24)
Viralload<50copies 89.5(469) 12.2(5) 0.001
Weight,kga 70.8±14.4 69.8±13.4 0.664 BMI,kg/m2a 24.7±4.4 24.3±5.2 0.582 Underweight 4.2(22) 14(6) 0.202 Normalweight 54.9(290) 53.5(23) Pre-obesity 29.7(157) 18.6(8) Obesity 11.2(59) 14.0(6) WC,cma 88.9±12.9 83.6±10.8 0.009 WCabovecut-off 43.3(228) 25.6(11) 0.023
ART:antiretroviraltherapy;BMI:bodymassindex;DBP:diastolicbloodpressure;F:female;HBP:highbloodpressure;M:male;SBP: systolicbloodpressure;TC:totalcholesterol;WC:waistcircumference.
a Mean±standarddeviation(minimum-maximum)or%(n). b chi-squareorStudent’sttest.
Moderate to very high
Metabolic syndrome
SCORE
Low Low Moderate to very high Low Moderate to very high
DAD FRS 100% 80% 60% 40% 20% 0% 89% 66% 11% 34% 76% 51% 24% 49% 62% 30% 38% 70% No Yes
Figure2 PrevalenceofmetabolicsyndromeinthestudypopulationaccordingtocardiovascularriskasestimatedbytheSystematic CoronaryRiskEvaluation(SCORE),theDataCollectiononAdverseEventsofAnti-HIVDrugs(DAD)riskequationandtheFramingham riskscore(FRS).
Among the 528 patients on ART, almost half (47.2%,
n=249)wereonaprotease inhibitor-basedregimen.Naïve
participants(n=43)wereyounger,hadashortertimesince
HIV diagnosis, had a lower mean CD4+count than the
ARTgroup andwere mostlyin thecategory of CD4+count
<200/mm3. Table 2 presents patient characteristics and
comparisonbytreatmentgroup.
RegardingCVriskfactors,therewerenosignificant
dif-ferences in cholesterol (total or LDL) or smoking status
betweentheART groupandthe naïvegroup.A trendwas
foundfornaïvepatientstopresentlowerTGandblood
glu-coselevels,although this wasnotstatistically significant.
NaïvepatientshadasmallermeanWCthantheARTgroup
(p=0.009).
ThepresenceofMSwasassociatedwithincreasedCVrisk
intheARTgroupwhenallthreetoolswereused(p<0.001)
(Figure 2). In the naïve group the same association was
found, although without statistical significance (data not
shown).
Independentlyofthetoolused,increasedmeanBMIand
WCwerestronglyassociatedwithhigherCVrisk(Figure3).
TheobservedagreementbetweentheFRSandSCOREwas
55.4% (k=0.183, p<0.001),while between FRS and DAD it
CV risk algorithm SCORE (10-year risk) DAD (5-year risk) FRS (10-year risk) BMI WC 5.00 4.00 3.00 2.00 1.00
Figure3 Oddsratiosand95%confidenceintervalsassociated withincreasedbodymassindex(BMI)andwaistcircumference (WC)accordingtocardiovascularriskscore(Systematic Coro-naryRiskEvaluation (SCORE),theDataCollectiononAdverse EventsofAnti-HIVDrugs(DAD)riskequationandthe Framing-hamriskscore(FRS).
was70.5%(k=0.465,p<0.001)andbetweenSCOREandDAD,
72.3%(k=0.347,p<0.001),whichrepresentsfairtomoderate
agreement.35 The observed agreement between the
algo-rithmsdidnotimprovesignificantlywhenonlypatientsaged
over40yearswereanalyzed(datanotshown).
In the final logistic regression model, the factors that
were stillassociatedwithhigherCV riskdiffered
depend-ing on the tool used.When SCORE wasused, the factors
associatedwithhigherCVriskwereolderage(OR=14.4[95%
CI:6.8-30.7];p<0.001)andincreasedTG(OR=2.5[95%CI:
1.5-4.1];p<0.001).UsingtheDADestimator,theassociated
factors were age (OR=21.4 [95% CI: 12.3-37.1]; p<0.001),
increasedTG(OR=3.8[95%CI:2.4-6.0];p<0.001),and
smok-ing(OR=3.8[95%CI:2.2-6.2];p<0.001).UsingtheFRS,the
factors were age (OR=20.6 [95% CI: 12.2-34.8]; p<0.001),
increasedTG(OR=3.9[95%CI:2.5-6.2];p<0.001)and
smok-ing(OR=5.5[95%CI:3.3-9.4];p<0.001).Interestingly,after
applyinglogisticregressiontoourdata,ARTwasonly
associ-atedwithincreasedCVriskwhentheFRSwasused(OR=3.2
[95%CI:1.2-8.5];p=0.002).
Discussion
The present study was conducted in a population of
HIV-infected individuals in Lisbon, mainly composed
of adult Caucasian males. In this sample, traditional CV
risk factors15,26,36---40 were associated with higher CV risk,
in agreementwithprevious studies. However,we found a
much higher prevalence of smoking (53.1%) compared to
thegeneralpopulationinPortugal(20%).41Interestingly,the
prevalenceoflowHDL-C(27.5%)foundinourstudywasless
than in other studies (37.2-36.3%),probably becauseof a
largeproportionofblackpatientsinourstudy(8.7%).
As expected,older patientshad higherCV risk
regard-lessofARTstatus.43Theinclusionofyoungerpatients(<30
years)inthisstudymeanscautionshouldbeexercisedwhen
interpretingthedataonCVrisk,sinceforsomealgorithms,
theriskismostlyrelative.However,dataonmortalityfrom
CVD in the HIV population indicate that evenat younger
ages,thesepatients present non-negligible cardiovascular
mortality,andthiswastheprimaryreasontoincludethese
patientsintheanalysis.44Inaddition,previousstudieshave
reportedtheapplicationofthesealgorithmstoyoungerHIV
IncreasedTGwasthemajorfactorassociatedwithMS.
LowHDL-C,identifiedinpreviousstudiesasthesecondmost
commonfactorassociatedwithMS,waslessstrongly
associ-atedthanincreasedWC.36UnlikeMalobertietal.,45 inthis
study we found that patients with MS presented a longer
meantimesinceHIVdiagnosisandlongerexposuretoART.
The prevalence of MSwas lowerin thisstudy than in the
generalnon-infectedPortuguesepopulation(43.1%).46
The useandclinicalbenefitsofCVriskalgorithmshave
beenmuchdiscussedinrecentyearsanddebatecontinuesas
towhichalgorithmisthemostaccuratefortheHIV-infected
population.Inourstudy,theprevalenceofpatients
classi-fiedasmoderatetohighCVriskusingtheSCOREtoolwas
lower than that found by others39 in which patients with
a knownhistoryof CVD werealso included. However,the
prevalenceinthisstudywashigherthanthatfoundinother
studies,whichcouldbeduetodifferencesinpatients’age.42
Usingthe DAD algorithm,theprevalence of infected
indi-viduals onART with high CV risk wasmuch higher in our
study(10.6vs.2.1%),38whichcouldbeexplainedbythefact
thatourpatientswereonaverage10yearsolderandwere
moreoftensmokers.Finally,usingtheFRS,theprevalence
ofmoderatetohighCVrisk(46.8%)wasmuchhigherthan
thatreportedinotherstudies(6-23.4%).14,38,39,42Again,the
differencesfoundcouldbeduetothehigherprevalenceof
hypertriglyceridemiaandsmokingandolderageinourstudy.
Comparingmoderatetohigh CVrisk bygender,the
preva-lencefoundwassimilartootherstudies,10,16,47highlighting
the increased CV risk seen in males, which is consistent
withdata onuninfected patients. Apart fromSCORE, the
algorithmsshowedthathigherCVriskwasassociatedwith
durationofARTexposure,asreportedbyothers.48Although
somestudies48,49describeahigherincidenceofCVDin
HIV-infectedpatientswithlowerCD4+lymphocytecounts,inthis
study therewere morepatients inthehigher CVrisk
cat-egories witha CD4+count over 500/mm3 than <200/mm3,
whichmaybeduetolongerARTexposureandhencemore
alterationsinlipidprofile.50
Overall,ourresultsindicatethattheDADandFRStools
appear to be more sensitive in detecting high CV risk
patients. Of note, we found that anthropometric
param-eters, although not contributing directly to the CV risk
algorithms, werepositivelyassociatedwithcardiovascular
risk, suggestingthat anynewtooldeveloped toassess CV
risk shouldinclude anthropometricparameters.Given the
resultsofthedifferenttoolsusedinthisstudy,a
longitudi-nal studyis necessarytodetermine theaccuracyof these
estimations.
Regardless of the algorithmused,measuringCV riskin
HIV-infectedpatientsshouldbeconsideredapriority,since
ourresultsdemonstratethatthereisahighprevalenceof
at-riskpatients.DeterminationofCVrisk,usingtoolstailored
tothispopulation,shouldbeseenasroutineforallpatients.
Portugal has a well-established HIV control program, and
prevention has been the primary focus. However, with
the increased survival rate witnessed in the HIV-infected
populationwithART,guidelinesshouldalsoincorporate
rec-ommendations to tackle unhealthy lifestyles, as already
seenforsmoking,particularlypromotionofhealthierdietary
habitsandexercisetoamelioratetheburdenofobesityand
CVD.
Disclosures
Nofinancialsupport.
Conflicts
of
interest
Theauthorshavenoconflictsofinteresttodeclare.
Acknowledgments
We would like to thank the patients participating in our
study,as well as the hospital staffat the Department of
InfectiousDiseases,for theirsupportduring the
investiga-tion.
Partiallypresentedatthe12thInternationalCongresson
DrugTherapy in HIV Infection, November 2014, Glasgow,
Scotland(PP195)andatthe36thCongressoftheEuropean
Society for Clinical Nutrition and Metabolism, September
2014,Geneva,Switzerland(SUN-PP219).
References
1.Boccara F. Cardiovascular complications and atherosclerotic manifestations in the HIV-infected population: type, inci-dence and associated risk factors. AIDS. 2008;22 Suppl. 3: S19---26.
2.PalellaFJJr,PhairJP.CardiovasculardiseaseinHIVinfection. CurrOpinHIVAIDS.2011;6:266---71.
3.BavingerC,BendavidE,NiehausK,etal.Riskofcardiovascular diseasefromantiretroviraltherapyforHIV:asystematicreview. PLOSONE.2013;8:e59551.
4.INSA.Infec¸ãoVIH/SIDA:asituac¸ãoemPortugala31de dezem-brode2016.Documenton◦148;2017.
5.DGS.PortugalDoenc¸as Cérebro-Cardiovascularesem números --- 2015. Programa Nacional para as Doenc¸as Cérebro-Cardiovasculares;2016.
6.EscárcegaRO, FrancoJJ,ManiBC,et al.Cardiovascular dis-ease inpatientswithchronic humanimmunodeficiency virus infection.IntJCardiol.2014;175:1---7.
7.IslamFM,WuJ,JanssonJ,etal.Relativeriskofcardiovascular diseaseamongpeoplelivingwithHIV:asystematicreviewand meta-analysis.HIVMed.2012;13:453---68.
8.KaminDS,GrinspoonSK.CardiovasculardiseaseinHIV-positive patients.AIDS.2005;19:641---52.
9.Triant VA. Cardiovascular disease and HIV infection. Curr HIV/AIDSRep.2013;10:199---206.
10.LakeJE,WohlD,ScherzerR,etal.Regionalfatdepositionand cardiovascularriskinHIVinfection:theFRAMstudy.AIDSCare. 2011;23:929---38.
11.ShahbazS,ManicardiM,GuaraldiG,etal.Cardiovascular dis-easeinhumanimmunodeficiencyvirusinfectedpatients:atrue orperceivedrisk?WorldJCardiol.2015;7:633---44.
12.HemkensLG,BucherHC.HIVinfectionandcardiovascular dis-ease.EurHeartJ.2014;35:1373---81.
13.FedeleF,BrunoN,ManconeM.Cardiovascularriskfactorsand HIVdisease.AIDSRev.2011;13:119---29.
14.De Socio GV, Parruti G, Quirino T, et al. Identifying HIV patientswithanunfavorablecardiovascularriskprofileinthe clinical practice: results from the SIMONE study. J Infect. 2008;57:33---40.
15.ReinschN,NeuhausK,EsserS,etal.AreHIVpatients under-treated? Cardiovascular risk factors in HIV: results of the HIV-HEARTstudy.EurJPreventCardiol.2012;19:267---74.
16.ShahmaneshM,SchultzeA,BurnsF,etal.Thecardiovascular riskmanagementforpeoplelivingwithHIVinEurope:howwell arewedoing?AIDS.2016;30:2505---18.
17.Mankal PK, Kotler DP. From wasting to obesity, changes in nutritionalconcernsinHIV/AIDS.EndocrinolMetabClinNAm. 2014;43:647---63.
18.Willig AL, Overton ET. Metabolic consequences of HIV: pathogenicinsights.CurrHIV/AIDSRep.2014;11:35---44. 19.WormSW,LundgrenJD. ThemetabolicsyndromeinHIV.Best
practice&research.ClinEndocrinolMetab.2011;25:479---86. 20.JarrettOD,WankeCA,RuthazerR,etal.Metabolicsyndrome
predictsall-causemortalityinpersonswithhuman immunode-ficiencyvirus.AIDSPatCareSTDs.2013;27:266---71.
21.TateT, WilligAL,WilligJH,etal. HIVinfectionandobesity: wheredidallthewastinggo?AntivirTherapy.2012;17:1281---9. 22.Crum-CianfloneN,TejidorR, MedinaS, etal.Obesityamong patients withHIV: thelatestepidemic. AIDS Pat CareSTDs. 2008;22:925---30.
23.LakeJE,CurrierJS.MetabolicdiseaseinHIVinfection.Lancet InfectDis.2013;13:964---75.
24.KimDJ,WestfallAO,ChamotE,etal.Multimorbiditypatterns inHIV-infectedpatients:theroleofobesityinchronicdisease clustering.JAcquirImmuneDeficSyndr.2012;61:600---5. 25.PiepoliMF,HoesAW, AgewallS,etal.2016 European
Guide-linesoncardiovasculardiseasepreventioninclinicalpractice: TheSixthJointTaskForceoftheEuropeanSocietyof Cardiol-ogyandOtherSocietiesonCardiovascularDiseasePreventionin ClinicalPractice(constitutedbyrepresentativesof10societies and byinvitedexperts) Developedwiththespecial contribu-tionoftheEuropeanAssociationforCardiovascularPrevention &Rehabilitation(EACPR).EurHeartJ.2016;37:2315---81. 26.Friis-MollerN,WeberR,ReissP,etal.Cardiovasculardiseaserisk
factorsinHIVpatients---associationwithantiretroviraltherapy. ResultsfromtheDADstudy.AIDS.2003;17:1179---93.
27.CooneyMT,DudinaA,D’AgostinoR,etal.Cardiovascular risk-estimationsystemsinprimaryprevention:dotheydiffer?Do theymakeadifference? Canweseethefuture?Circulation. 2010;122:300---10.
28.Authors/TaskForceM,PiepoliMF,HoesAW,etal.2016 Euro-peanGuidelinesoncardiovasculardiseasepreventioninclinical practice:TheSixthJointTaskForceoftheEuropeanSocietyof CardiologyandOtherSocietiesonCardiovascularDisease Pre-ventioninClinicalPractice(constitutedbyrepresentativesof 10societiesandbyinvitedexperts):developedwiththe spe-cialcontributionoftheEuropeanAssociationforCardiovascular Prevention & Rehabilitation (EACPR). Eur J Prevent Cardiol. 2016;23:NP1---96.
29.Ladapo JA,RichardsAK, DeWittCM,et al.Disparitiesinthe qualityofcardiovascularcarebetweenHIV-infectedversus HIV-uninfectedadultsintheUnitedStates:across-sectionalstudy. JAmHeartAssoc.2017;6.
30.D’AgostinoRBSr.Cardiovascularriskestimationin2012:lessons learnedandapplicability totheHIV population.JInfectDis. 2012;205Suppl.3:S362---7.
31.DeWitS,BattegayM,D’ArminioMonforteA,etal.European AIDSClinicalSocietySecondStandardofCareMeetingBrussels 16-17November2016:asummary.HIVMed.2018;19:77---80. 32.Friis-MollerN,ThiebautR,ReissP,etal.Predictingtheriskof
cardiovasculardiseaseinHIV-infectedpatients:thedata collec-tiononadverseeffectsofanti-HIVdrugsstudy.EurJCardiovasc PrevRehabilit:OffJEurSocCardiolWorkingGroupsEpidemiol PreventCardiacRehabilitExercPhysiol.2010;17:491---501. 33.WHOExpertCommitteeonPhysicalStatus:theuseand
inter-pretation of anthropometry. Physical status: the use and
interpretationofanthropometry:reportofaWHOExpert Com-mittee,x.Geneva:WorldHealthOrganization;1995.p.452. 34.Alberti KG, Eckel RH, Grundy SM, et al. Harmonizing the
metabolic syndrome:ajoint interim statementofthe Inter-nationalDiabetesFederationTaskForceonEpidemiologyand Prevention;NationalHeartLung,and BloodInstitute; Ameri-canHeartAssociation;World HeartFederation;International AtherosclerosisSociety;and InternationalAssociationfor the StudyofObesity.Circulation.2009;120:1640---5.
35.LandisJR,KochGG.Themeasurementofobserveragreement forcategoricaldata.Biometrics.1977;33:159---74.
36.SignoriniDJ,MonteiroMC,AndradeMdeF,etal.Whatshould weknowaboutmetabolicsyndromeandlipodystrophyinAIDS? RevAssocMedBrasil.2012;58:70---5.
37.SmithCJ,LevyI,SabinCA,etal.Cardiovasculardiseaserisk fac-torsandantiretroviraltherapyinanHIV-positiveUKpopulation. HIVMed.2004;5:88---92.
38.NeryMW,Martelli CM,Silveira EA, etal. Cardiovascular risk assessment: a comparison of the FraminghamPROCAM, and DADequationsinHIV-infectedpersons.ScientificWorldJournal. 2013;2013:969281.
39.Knobel H,Jerico C,MonteroM, et al.Global cardiovascular riskinpatientswithHIVinfection:concordanceanddifferences in estimates according to three risk equations (Framing-ham SCORE, and PROCAM). AIDS Pat Care STDs. 2007;21: 452---7.
40.GlassTR,UngsedhapandC,WolbersM,etal.Prevalenceofrisk factorsforcardiovasculardiseaseinHIV-infectedpatientsover time:theSwissHIVCohortStudy.HIVMed.2006;7:404---10. 41.DGS.ProgramaNacionalparaaPrevenc¸ãoeControlodo
Tabag-ismo2017;2017.
42.Masia M, Perez-Cachafeiro S, Leyes M, et al. Cardiovascu-lar risk in human immunodeficiency virus-infected patients in Spain CoRIS cohort, 2011. Enferm Infec Microbiol Clin. 2012;30:517---27.
43.HsuePY,DeeksSG,HuntPW.Immunologicbasisof cardiovascu-lardiseaseinHIV-infectedadults.JInfectDis.2012;205Suppl. 3:S375---82.
44.Croxford S, Kitching A, Desai S, et al. Mortality and causes of deathin people diagnosed with HIV in the era of highly activeantiretroviraltherapycomparedwiththegeneral pop-ulation:ananalysisofanationalobservationalcohort.Lancet PublHealth.2017;2:e35---46.
45.MalobertiA,GiannattasioC,DozioD,etal.Metabolicsyndrome in human immunodeficiency virus-positive subjects: preva-lence,phenotype,andrelatedalterationsinarterialstructure andfunction.MetabSyndrRelDisord.2013;11:403---11. 46.RaposoL, SeveroM, BarrosH, et al.The prevalence ofthe
metabolicsyndromeinPortugal:thePORMETSstudy.BMCPubl Health.2017;17:555.
47.AboudM,ElgalibA,PomeroyL,etal.Cardiovascularrisk eval-uation and antiretroviral therapy effects in an HIV cohort: implicationsforclinicalmanagement:theCREATE1study.IntJ ClinPract.2010;64:1252---9.
48.LichtensteinKA,ArmonC,BuchaczK, etal. LowCD4+Tcell countisariskfactorforcardiovasculardiseaseeventsinthe HIVoutpatientstudy.ClininfectDis:OffPubl Infect DisSoc Am.2010;51:435---47.
49.GrinspoonS,CarrA. Cardiovascularriskand body-fat abnor-malities in HIV-infected adults. N Engl J Med. 2005;352: 48---62.
50.HesterEK.HIVmedications:anupdateandreviewofmetabolic complications.NutrClinPract:OffPublAmSocParentEnteral Nutr.2012;27:51---64.