REVISTA
BRASILEIRA
DE
ANESTESIOLOGIA
PublicaçãoOficialdaSociedadeBrasileiradeAnestesiologiawww.sba.com.br
SCIENTIFIC
ARTICLE
Effect
of
gabapentin
pretreatment
on
myoclonus
after
etomidate:
a
randomized,
double-blind,
placebo-controlled
study
Mensure
Yılmaz
C
¸akirgöz
a,∗, ˙Ismail
Demirel
b,
Esra
Duran
c,
Ays
¸e
Belin
Özer
b,
Volkan
Hancı
d,
Ülkü
Aygen
Türkmen
a,
Ahmet
Aydın
b,
Ays
¸ın
Ersoy
a,
Aslıhan
Büyükyıldırım
aaOkmeydanıTrainingandResearchHospital,DepartmentofAnesthesiologyandReanimation,S¸is¸li, ˙Istanbul,Turkey bFıratUniversity,SchoolofMedicine,DepartmentofAnesthesiologyandReanimation,Elazı˘g,Turkey
c¸ehitS KamilStateHospital,Gaziantep,Turkey
dDokuzEylülUniversity,SchoolofMedicine,DepartmentofAnesthesiologyandReanimation, ˙Izmir,Turkey
Received13August2014;accepted11November2014 Availableonline20October2015
KEYWORDS
Etomidate;
Injectionpain;
Myoclonus; Gabapentin
Abstract
Aim:Toevaluatetheeffectsofthreedifferentdosesofgabapentinpretreatmentonthe inci-denceandseverityofmyoclonicmovementslinkedtoetomidateinjection.
Method: Onehunderedpatients,between18and60yearsofageandriskcategoryAmerican SocietyofAnesthesiologistsI---II,withplannedelectivesurgeryundergeneralanestheticwere includedinthestudy.Thepatientswererandomlydividedintofourgroupsand2hbeforethe operationweregivenoralcapsulesofplacebo(GroupP,n=25),400mggabapentin(GroupG400,
n=25),800mggabapentin(GroupG800,n=25)or1200mggabapentin(GroupG1200,n=25). Sideeffectsbeforetheoperationwererecorded.Afterpreoxygenationforanesthesiainduction 0.3mgkg−1etomidatewasadministeredfor10s.Asingleanesthetistwithnoknowledgeofthe
studymedicationevaluatedsedationandmyoclonicmovementsonascalebetween0and3. Twominutesafterinduction,2gkg−1fentanyland0.8mgkg−1rocuroniumwereadministered
fortrachealintubation.
Results:Demographicdataweresimilar.IncidenceandseverityofmyoclonusinGroupG1200 andGroupG800weresignificantlylowerthaninGroupP;sedationincidenceandlevelwere appreciablyhighercomparedtoGroupPandGroupG400.Whiletherewasnodifferenceinthe
∗Correspondingauthor.
E-mail:drmensure@gmail.com(M.YılmazC¸akirgöz).
http://dx.doi.org/10.1016/j.bjane.2014.11.014
incidenceofmyoclonusbetweenGroupPandGroupG400,theseverityofmyoclonusinGroup G400waslowerthanintheplacebogroup.Inthetwo-hourperiodbeforeinductionotherthan sedationnoneofthesideeffectsrelatedtogabapentinwereobservedinanypatient.
Conclusion: Pretreatment with 800mg and 1200mg gabapentin 2h before the operation increasedthelevelofsedationandreducedtheincidenceandseverityofmyoclonicmovements duetoetomidate.
©2015SociedadeBrasileiradeAnestesiologia.Publishedby ElsevierEditoraLtda.Thisisan openaccessarticleundertheCCBY-NC-NDlicense( http://creativecommons.org/licenses/by-nc-nd/4.0/).
PALAVRAS-CHAVE
Etomidato;
Doràinjec¸ão;
Mioclonia; Gabapentina
Efeitodopré-tratamentocomgabapentinasobreamiocloniaapósetomidato:um
estudorandômico,duplo-cegoecontroladoporplacebo
Resumo
Objetivo: Avaliarosefeitosdetrêsdosesdiferentesdegabapentinacomopré-tratamentosobre aincidênciaegravidadedosmovimentosmioclônicosassociadosàinjec¸ãodeetomidato.
Método: Cempacientes,comidadesentre18-60anos,estadofísicoASAI-II,programadospara cirurgiaeletivasobanestesiageralforamincluídosnoestudo.Ospacientesforam randomica-mentedivididosemquatrogrupose,2horasantesdaoperac¸ão,receberamcápsulasoraisde placebo(GrupoP,n=25),400mgdegabapentina(GrupoG400,n=25),800mgdegabapentina (GrupoG800,n=25)ou1200mgdegabapentina(GrupoG1200,n=25).Osefeitoscolaterais antesdacirurgiaforamregistados.Apóspré-oxigenac¸ãoparaainduc¸ãodaanestesia,etomidate (0,3mg.kg−1)foiadministradopor10segundos.Umúnicoanestesista,cegoparaamedicac¸ão
doestudo,avaliouasedac¸ãoeosmovimentosmioclônicosusandoumaescalade0a3.Dois minutosapósainduc¸ão,fentanil(2gr.kg−1)erocurônio(0,8mg.kg−1)foramadministrados
paraaintubac¸ãotraqueal.
Resultados: Osdadosdemográficosforamsemelhantes.Aincidênciaegravidadedamioclonia nosgrupos G1200e G800foramsignificativamentemenores quenoGrupoP;aincidênciae oníveldesedac¸ãoforamconsideravelmentemaiorescomparadosaoGrupoPeGrupoG400. Enquantonãohouvediferenc¸anaincidênciademiocloniaentreosgruposPeG400,agravidade damioclonia noGrupo G400foi menorque nogrupoplacebo. Noperíodo de2horasantes dainduc¸ão,nenhumdos efeitoscolaterais relacionadosàgabapentina,exceto sedac¸ão,foi observadoemqualquerpaciente.
Conclusão:Opré-tratamentocom800mge1200mgdegabapentina2horasantesdaoperac¸ão aumentouoníveldesedac¸ãoereduziuaincidênciaegravidadedosmovimentosmioclônicos associadosaoetomidato.
©2015SociedadeBrasileiradeAnestesiologia.PublicadoporElsevierEditoraLtda.Este ´eum artigo OpenAccess sobumalicenc¸aCCBY-NC-ND( http://creativecommons.org/licenses/by-nc-nd/4.0/).
Introduction
Etomidate,aderivativeofimidazole,isapopularhypnotic agentchosenforpatientswithcardiovascularinstabilitydue tominimalcardiovascularsideeffectsandextremelystable hemodynamicprofile.Myoclonusandinjectionpainaretwo disagreeablesideeffectsofanesthesiainductionwith eto-midate.Asmanysideeffectsduetoetomidatearethought tobelinkedtothesolventpropyleneglycol,alipid formula-tionwasdeveloped.Whilethisnewformulationprevented injectionpain,venousirritationandhemolysis, myoclonus incidencewasnotaffectedbythesolvent.1
Theformationofmyoclonusduringanesthesiainduction with etomidate has clinical importance in select groups of patients. Myoclonus can increase the risk of regurgi-tation and aspiration in patients with full stomach, asit
increasesintraocularpressureitmaycausevitreousprolapse inpatientswithopen eyeinjuries,andasmyocardial oxy-genconsumption increasesduringmyoclonusitmaycause problemsinpatientswithlimitedcardiovascularreserves.2
Finallymyoclonushasbeenobservedtoberesponsiblefor hypoxemia attacks during spontaneous respiration when etomidateisadministeredforsedation.2,3Despitethe
vari-etyofmedicationsthatreduce theincidenceandseverity of myoclonic movements after etomidate administration, themechanismis notclear. Doenickeetal.reportedthat myoclonus after treatment with etomidate was a phe-nomenonofsubcorticaldisinhibition,likethephenomenon ofrestlesslegsduringnormalhumansleep,andisnot gen-eratedbyanepilepticfocus.1,4
withantinociceptive,analgesic andantihyperalgesic prop-erties.Themostwidespreaduseofgabapentin,outsideof epilepsy,isfor neuropathic pain.5 Alsogabapentinand its
analogshavebeeneffectiveinthetreatmentofmotion dis-orders such as periodic leg movements in sleep, restless leg syndrome,essential tremorand acquired nystagmus.6
Recentlymanyclinicalstudiesevaluatingthepotentialrole ofgabapentininthepreoperativeperiodforavarietyofaims havebeenpublished.5Howeverthoughmyoclonuslinkedto
etomidate hassimilar pathophysiology andEEG results as restlessleg syndromewhichhasbeen successfullytreated bygabapentin,nostudieswerefoundongabapentin’seffect onmyoclonuslinked toetomidate.The hypothesis ofthis study is that pretreatment with three different doses of oral gabapentin will reduce the incidence and severity of myoclonic movements linked to etomidate in a dose-dependentfashion.
To test this hypothesis the aim was to complete a prospective, randomized, double-blind and placebo-controlledstudy toresearchtheeffectsofthreedifferent dosesoforalgabapentinpretreatmentontheincidenceand severityofmyoclonicmovementslinkedtoetomidate.
Methods
ThisstudywascompletedwithpermissionofFiratUniversity MedicalFacultyPharmaceuticalResearchEthicsCommittee (Head: Prof. Mehmet Tokdemir, dated 12.07.2012, deci-sionn◦ 07) between July 2012 andDecember 2012in the
operatingtheatersof FiratUniversity MedicalFacultyand OkmeydaniEducationalandResearchHospitalafterpatients signedaninformedconsentform.One-hunderedpatientsin I---IIriskgroup,accordingtotheAmericanSocietyof Anes-thesiologists(ASA)classificationofphysicalcondition,who weretoundergoelective surgicalintervention under gen-eralanesthesiabetweentheagesof18---60wereincludedin thestudy.
Patients considered have airway management diffi-culties, cardiac disease, diabetes mellitus, history of neuromusculardisease,impairedrenalstatus,liverfailure, COPDand asthma, hiatalhernia and symptomatic gastro-esophageal reflux, gastrointestinal dysfunction affecting absorptionoforaltreatments,historyofallergicreactionto thestudydrugs,pregnancy,lactatingfemalepatients,drug oralcoholaddiction,andpatientswithahistoryofchronic opioid, tricyclic antidepressant, benzodiazepine anticon-vulsant, clonidine, beta blocker, systemic and/or topical steroidusewerenotincludedinthestudy.
No patient received any premedication. The patients wererandomly assignedusing a computer-generated ran-domnumberstabletooneofthefollowingfourtreatment groups: 1--- Group Preceived an oral placebo;2 --- Group G400 received gabapentin 400mg, po; 3 --- Group G800 received gabapentin 800mg, po; and 4 --- Group G1200 received gabapentin 1200mg, po. The study medication capsuleswere put in numberedenvelopes containing two placebo capsules (Group P), one gabapentin 400mg with oneplacebocapsule(GroupG400),twogabapentin400mg capsules(GroupG800),ortwogabapentin600mgcapsules (GroupG1200).Twohoursbeforetheoperationstudy med-icationswere administeredwitha smallamount of water
by an anesthetist not included in the study. The study drugswerepreparedbythepharmacyinordertomaintain double-blind conditions,and an appropriatecode number was assigned. Patients and the anesthetist in charge of patientmanagementanddatacollectionwereunaware of thegroups.Beforebeingtakentotheoperatingroomside effects developing in the patients, such as nausea, vom-iting, dizziness, headache, confusion, weakness, fatigue, nystagmus,skinrash,drowsiness,peripheraledema,vision disorders etc., were evaluated and recorded by an anes-thetist blind to the contents of the study drugs and not includedinthestudy.
Afterpatients were transferred tothe operating table preoxygenation was begun with 6Lmin−1 oxygen
admin-istered through a mask and non-invasive blood pressure, electrocardiogram, and pulse oxymetry monitoring was applied. A vein was opened in the back of the left hand with a 20G cannula and infusion of 0.9% NaCl solution wasstarted.Afterpreoxygenationforanesthesiainduction 0.3mgkg−1etomidatewasadministeredfor10s.Afterthe
eyelashreflexwaslostafterinductionthepatientwas man-uallyadministered100%O2 througha maskuntilendtidal
CO2(ETCO2)was35---40mmHg.Twominutesafterinduction
2gkg−1fentanyland0.8mgkg−1rocuroniumweregivenfor
trachealintubation.Afterendotrachealintubation anesthe-siawasmaintainedwith30%oxygen,70%nitrousoxidewith 2%sevoflourane.
Sedationandmyoclonicmovementswereevaluatedand recorded on a 0---3 scale by an anesthetist blind to the studiedmedication.Evaluationofsedationwascompleted beforeinductionwithetomidatewasbegun;sedationlevel wasevaluatedas0=none/awake(alert),1=slight(drowsy but responds tonamesaid innormal voice),2=moderate (respondstoloudvoiceand/orrepeatedcalls)and3=deep (responds when prodded lightly or shaken).2 Myoclonic
movementswereevaluatedinthe2minperiodafter induc-tion;myoclonicseveritywasevaluatedaccordingto0=no myoclonus,1=slightmyoclonus(slightfasciculationofface and/ordistalupperand/orlowerextremities),2=moderate myoclonus(definitemovementsoffaceand/orextremities) and 3=severe myoclonus (movements of extremities and trunk).7
Heartrate(HR),meanarterialpressure(MAP)and periph-eraloxygensaturationwererecordedbeforeinduction(base value), immediatelybefore intubationand inthe 1st,3rd and5thminutesaftertrachealintubation.Attheendofthe studyperiod,anesthesiamanagementwastransferredtothe anesthesiateamresponsiblefor theoperatingtheaterand awareofthemedicationsadministeredtothepatient.
Statistical
method
Table1 Demographiccharacteristicsofpatients.
GroupP(n=25) GroupG400(n=25) GroupG800(n=25) GroupG1200(n=25)
Age(years) 35.5±12.4 34.9±6.2 36.1±9.4 35.8±12.4
BMI(kg/m2) 24.0±3.6 23.8±3.0 23.9±4.8 23.6±3.3
Gender(male/female) 13/12 12/13 14/11 12/13
ASAphysicalstatus(I/II) 11/14 12/13 13/12 14/11
Dataaregivenasnumberofpatientsormean±standarddeviation.ASA---AmericanSocietyofAnesthesiologists.
distributed data.Significancewasaccepted asp<0.05. In
the placebo group the incidence of myoclonus wasabout
70%, assuming ˛=0.05, and 1−ˇ=0.80, and with a
pre-dictedaverage reductionof myoclonusincidenceof 40%8;
for the study at least 22 patients were required in each group.Workingfromthisdata,inthestudy25patientswas includedineachgroup.
Results
Intermsofdemographicdatatherewasnosignificant sta-tisticaldifferencebetweenthegroups(p>0.05)(Table1). Inthetwohourperiodbeforeinductionotherthansedation noneofthesideeffectsrelatedtogabapentinwereobserved inanypatient.
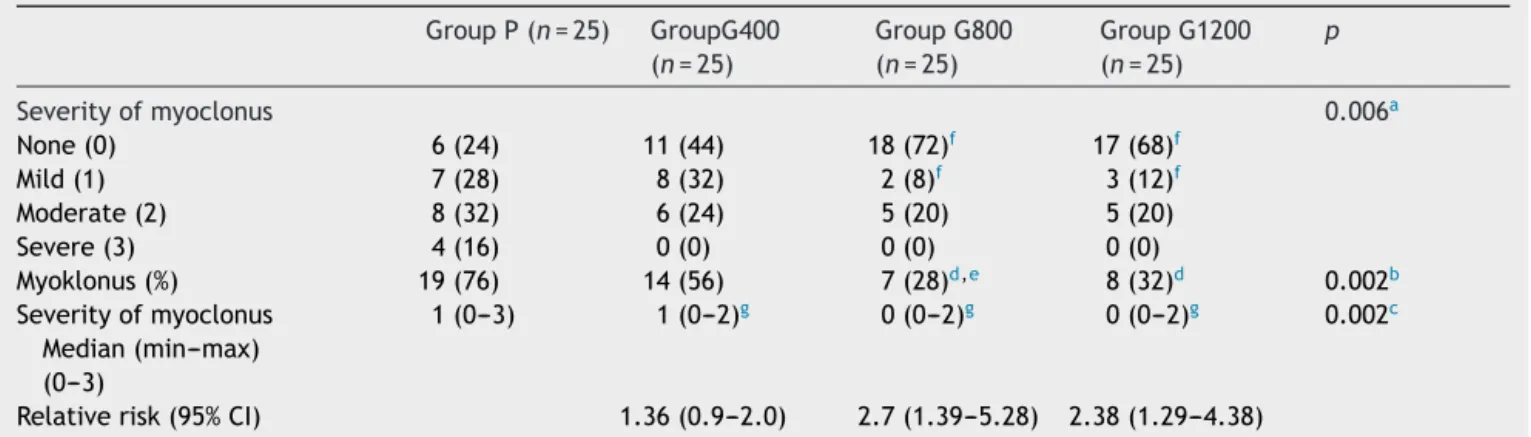
There was a significant difference in the incidence, severityandmedian valuesofmyoclonus linkedto etomi-date between the groups (p=0.002 Chi-square, p=0.006 FisherExacttest,KruskalWallisp=0.002respectively).The myoclonus severity levels in the G1200 and G800 groups weresignificantlylowerthaninGroupP(p=0.006,p=0.003 Fisher Exacttest).The myoclonus incidenceinG1200 and G800 was significantly lower than in Group P (p=001, p=0.002 Chi-square), and in Group G800 the incidence wassignificantly lowerthanin Group G400 (p=0.045 Chi-square).Comparedtotheplacebogroup,inG800therewas
2.71timesandinG1200therewas2.38timeslessmyoclonus observed(Table2).
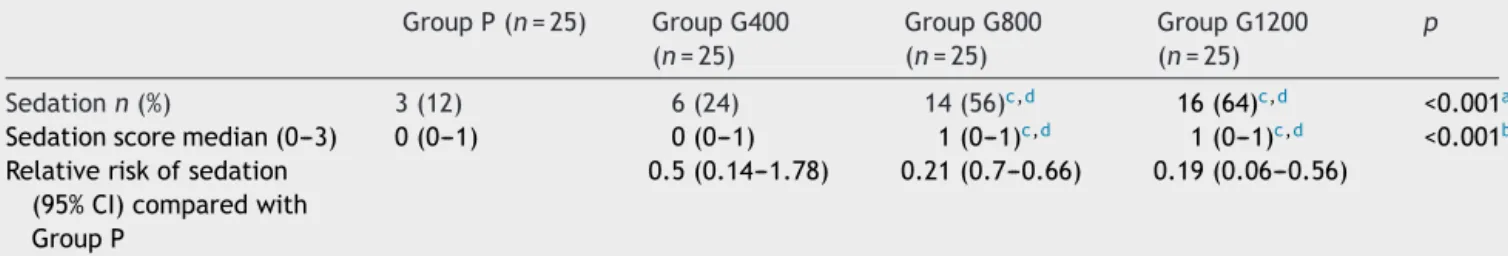
Thefrequency,intensitiesandmedianvaluesofsedation between the groups were statistically significantly differ-ent(p<0.01).Thefrequencyandintensitiesofperioperative sedationinGroupG1200andG800weresignificantlyhigher than in Group P and G400 (p=0.001, p=0.001, p=0.04, p=0.021respectively)(Table3).Comparedtotheplacebo group,inG800therewas4.76timesandinG1200therewas 5.26timesmoresedationobserved(Table2).
The mean arterial blood pressure and the heart rate weresimilaramongthegroups at allmeasurementtimes. Nobradycardiaorhypotensionwasobservedinanypatient. Peripheraloxygensaturation inthefourgroupsduringthe studyperiodwasabove≥97% andtherewasnosignificant differenceobservedbetweenthegroups.
Discussion
Inthis study,while 800mg and1200mgof gabapentin 2h beforetheoperationreducedthefrequencyandseverityof myoclonicmovementslinked toanesthesiainduction with etomidate, it was determined that it also increased the preoperativesedationlevel.
Preventingmyoclonusrelatedtoetomidate isclinically important.Etomidateis frequentlyusedasitallowsearly
Table2 Numberofpatients(%)andseverityofmyoclonusafterinjectionofetomidate. GroupP(n=25) GroupG400
(n=25)
GroupG800 (n=25)
GroupG1200 (n=25)
p
Severityofmyoclonus 0.006a
None(0) 6(24) 11(44) 18(72)f 17(68)f
Mild(1) 7(28) 8(32) 2(8)f 3(12)f
Moderate(2) 8(32) 6(24) 5(20) 5(20)
Severe(3) 4(16) 0(0) 0(0) 0(0)
Myoklonus(%) 19(76) 14(56) 7(28)d,e 8(32)d 0.002b
Severityofmyoclonus Median(min---max) (0---3)
1(0---3) 1(0---2)g 0(0---2)g 0(0---2)g 0.002c
Relativerisk(95%CI) 1.36(0.9---2.0) 2.7(1.39---5.28) 2.38(1.29---4.38)
GroupP,placebogroup;GroupG400,Gabapentin400mg;GroupG800,Gabapentin800mg;GroupG1200,Gabapentin1200mg. a Fisherexacttest.
b Chi-squaretest.
c KruskalWallistest.Comparisonsforincidenceofmyoclonus. d p<0.01comparedwithgroupP.
Table3 Comparisonoffrequencyandintensitiesofsedationbetweeninfourgroups. GroupP(n=25) GroupG400
(n=25)
GroupG800 (n=25)
GroupG1200 (n=25)
p
Sedationn(%) 3(12) 6(24) 14(56)c,d 16(64)c,d <0.001a
Sedationscoremedian(0---3) 0(0---1) 0(0---1) 1(0---1)c,d 1(0---1)c,d <0.001b
Relativeriskofsedation (95%CI)comparedwith GroupP
0.5(0.14---1.78) 0.21(0.7---0.66) 0.19(0.06---0.56)
GroupP,placebogroup;GroupG400,Gabapentin400mg;GroupG800,Gabapentin800mg;GroupG1200,Gabapentin1200mg. Frequencyofsedation.
aChi-squaretestp<0.001.
Intensitiesofsedationwithfourgroups
b Fisher-exacttest/KruskalWallistestp<0.001. c p<0.002comparedwithgroupP.
d p<0.05comparedwithgroup400.
recoveryandstablehemodynamicsininterventions requir-ing short-term anesthesia like elective cardioversion.7 In
the absence of neuromuscular blocker agents when used forinduction myoclonusisobserved in50---80% ofpatients withoutpremedication,while theincidenceisreportedas 20---45% when used for sedation of patients.1,9 Reported
cases are generally mostly minor myoclonic events of short/briefdurationortremor.Howeverafewpatientshave myocloniceventscharacterizedasserious,describedas gen-eralizedrigidityandstiffnessandlastingseveralminutes.In additionduringmyoclonus ECG electrodes weredisplaced andoxygensaturationfallsarefrequentlyreportedonpulse oxymetry.Inthissituationitshouldbenotedthatmyoclonic events may be large enough to delay evaluation of mon-itoringand success of intervention in patients.3 However
especiallyfor shortdurationinterventionsthe medication given toprevent myoclonus due to etomidate should not disruptthepositivehemodynamicandearlyrecovery prop-ertiesofetomidate.2Inourstudyatthedosesofgabapentin
used no effect on respiration or consciousness after the intervention wasexpected, soin thisstudy therewas no postoperativerecordkept.
In our study, similar to previous studies, observed myoclonicactivityat76%intheplacebogroup.Itisknown that in more than half of cases myoclonus due to etomi-datestartsafterthe1stminute1sotheobservationperiod
inthis studywasfixed at 2min. To denotethe difference betweenhand-armpullmovementsduetopainofthe etomi-dateinjectionandmyoclonus,movementduringintravenous etomidateadministration wasaccepted asinjection pain, whilemovement inthe2minafterthe injectionwasfully finishedwereacceptedasmyoclonus.Itisknownfrom previ-ousstudiesthatslowinjectionspeed,withaeffectsimilarto primingdoseofetomidate,reducedmyoclonusincidence.1
Inthisstudyetomidatewasinjectedover10s.Itisthought thatthisallowedustocapturethetruerateofmyoclonus.
The neurologic mechanism of myoclonic activity after etomidate is not clear and one possibility is that it may beaformofseizureactivity.Anothertheoryisthatits ini-tial causemay bedue to differencesin local brain blood floworinreceptoraffinitiesintheCNSasynchronoustothe effectof etomidate, together witha possible subcortical
disinhibition developingdue toquicksuppressionof corti-calinhibition linkedtoearlierandlowerdosesdepressing theexcitatorycircuitsofinhibitorpathways.1,10Disruption
ofGABAneuronsmakespathwaysrelatedtoskeletalmuscle controlmoresensitivetospontaneousnervetransmissions, which causesmyoclonicmusclemovements.7 Choi etal.11
showed that rocuronium premedication blocked the neu-romuscular junctiontransmission and definitively reduced myoclonusduetoetomidate.
StructurallyananticonvulsantGABAanalog,afterusefor neuropathicpainsyndromes,inthe1990sgabapentinbegan tobeusedsuccessfullytotreatrestlesslegsyndrome.12The
experimentalevidencefromstudiestodateindicatea dis-inhibitionroleinRLSpathogenesisatsupraspinallevels.6In
anelectroencephalogram(EEG)studybyDoenickeetal.1on
EEGepileptic activitywasnot encountered,asmyoclonus linked to etomidate, similar to restless leg syndrome, is linked to subcortical disinhibition theyreported that low doses with etomidate administration reduced myoclonus, supportingthesubcorticaldisinhibitiontheory.Inaddition, afterpremedicationwithbenzodiazepansandopioids,with knownlimitingeffectsonsubcorticalstructures,the reduc-tioninmyoclonuslinkedtoetomidatesupportsthetheory ofdisinhibitionofsubcorticalstructures.1,4Whilethe
effec-tive mechanism of gabapentin is not definitely known, it increasesnon-synapticGABAreleaseandsynthesisfromglial structuresinthe wholebrainindose-linked fashion. Link-agewithhighaffinityfor␣2␦subunitsofvoltagesensitive calcium channels, reductionin the releaseof monoamine neurotransmitters,inhibitionofvoltageactivesodium chan-nelsandincreaseinserotoninconcentrationareamongthe othereffectsprovenforgabapentin.13Inthisstudywhilethe
Gabapentin is a medication with low incidence of side effects and little interaction withother medications whichiswelltolerated.Non-epilepticfocalandmulti-focal myoclonus is among the side effects of long-term treat-mentwithgabapentinandpregabalin,suchasforepilepsy, neuropathic pain and restless leg syndrome, though the incidenceislessthanforotheranticonvulsants.13 Recently
reportsofmyoclonusrelatedtogabapentin(GBP)usebeen case studies or been formed of small patient series. In available case studies, frequently a clinical tableau of myoclonusafewdaysaftergabapentindoseincreasefrom stable dose in cases with a history of serious neurologic and/or systemic disease and polytherapy administration, which quicklyresolves withindays afterstopping. In pre-marketing studies of 1486 patients using gabapentin for epilepsyamyoclonusrateof0.1%wasreported.14 Contrary
tothis Asconap et al. wheninquiring about myoclonusin patientsreceivinggabapentintreatmentfound12.5%of104 patientshadobservedmyoclonus.Thishighincidencemay bepartlyexplainedbyquestioningspecificallyformyoclonic situations.Inthepatientpopulationlateperiodrenal fail-urewhichinterfereswiththemedicationsrenalexcretion, chronic static encephalopathy, mental retardation or dif-fuse braindamage mayberisk factors for myoclonusdue togabapentin.This relationship is knownfromthe devel-opmentof choreoathetosis andother movement disorders during use of gabapentin and other antiepileptic medi-cations. The role of other possible risk factors, such as polytherapy and refractory seizures is not clear.14 The
anti-epileptic effective mechanism of gabapentin, similar to its induction mechanism for myoclonus, is not fully understood. Myoclonus linked togabapentin is thoughtto form in the serotonergic neurotransmitter system linked tomyoclonus.15 Inaddition,in posthypoxicanimal models
a dose-linked antimyoclonic effect of gabapentin was found.16Inordertomoreclearlyunderstandtherelationship
between gabapentin and myoclonus more advanced stud-iesonthepathophysiologyofmyoclonusandtheeffective mechanismofgabapentinareneeded.
Intheperoperativeperiodthemostfrequentlyreported side effects of single-dose or short-term gabapentin administration are dizziness (16%), sedation (23%), nau-sea/retching/vomiting (19---25%), somnolence, urinary retention, and lightheadedness.6 After preoperative
gabapentin administration studies on the presence of a sedation effect in the preoperative period has a mixed structure. Inthe literaturefor a varietyof surgerytypes, 600 or 1200mg gabapentin in the preoperative period 1---2hafteradministrationinthelimitednumberofstudies evaluatingthesedationlevel,17---20whilesomereportno
sta-tisticaldifferenceinsedationlevelbetweenplacebogroup andgabapentingroup,Clarkeetal.21 inastudyevaluating
the effectof 1200mg gabapentin 2h beforeoperation on high-anxiety levels reported observing a significant level of sedation in the gabapentin group compared to the placebogroup.Togetherwiththis,gabapentin’s structural analog pregabalin is reported to increase sedation in a dose-linked fashionin thepreoperative period.22,23 In this
study inthe 2hour periodbeforetheoperation similarto previous studies,17---21 noside effectslinkedto gabapentin
such as nausea and vomiting, dizziness, lightheadedness, somnolence,peripheraledema, andvisualdisturbancesor
headache were observed. Comparing the frequency and intensities of sedation in the groups in the preoperative period,adefinitefrequencyandintensitiesofsedationwas identified in Group G800 and Group G1200 compared to theplaceboandG400group (p=0.001,p=0.001,p=0.04, p=0.021respectively).Theresultsofthisstudyaresimilar tothatofClarkeetal.21 inthatincreasingdoseincreased
sedationlevels.
In our study the primarylimitation is that thepatient groupwasyoungerandmorehealthythanthepatientgroup towhometomidateismostfrequentlyadministeredin clin-ical practice. Generalizations should not be made from this study for high-risk and/or geriatric patients who use antidepressants,hypnoticorantihypertensivemedications, includinggabapentin,whomayshowincreasedsensitivityto medication.Forsimilarfutureresearchmoreadvanced stud-iesareneededtofirstlyidentifytheoptimaldoseforthese types of patients and possible side effects. In the period beforesurgery,concernsrelatedtoanesthesiaandsurgery areknowntocauseanxietyin60---80%ofpatients.24,25Stress
andanxietyarewidelyacceptedtodelaygastricemptying.26
Asitisthoughtthatabsorptionoforallyadministered med-icationandpeakplasmaconcentrationvaluesareaffected byanxiety,27anotherlimitationofoutstudyisthatto
stan-dardizepatientsbasalanxietylevelsandgabapentinserum levelswerenotexamined.
In conclusion in this study, 800mg and 1200mg gabapentinoraladministration2hbeforeoperationreduced thefrequency and severityof myoclonicmovements dur-inganesthesiainductionwithetomidateandincreasedthe sedation level before the operation. It is concluded that thelowest effectivedose of 800mg gabapentinshouldbe consideredtopreventmyoclonuslinkedtoetomidate. How-everthesedativepropertiesofgabapentinandpossibilityof delayingpostoperativerecoveryincasesofelective ambu-latorysurgeryshouldbenoted.
Conflicts
of
interest
Theauthorsdeclarenoconflictsofinterest.
References
1.DoenickeAW,RoizenMF,KuglerJ,etal.Reducingmyoclonus afteretomidate.Anesthesiology.1999;90:113---9.
2.Guler A,Satilmis T,Akinci SB,et al.Magnesium sulfate pre-treatmentreducesmyoclonusafteretomidate.AnesthAnalg. 2005;101:705---9.
3.AissaouiY,BelyamaniL,ElWaliA,etal.Preventionofmyoclonus afteretomidateusingaprimingdose.AnnFrAnesthReanim. 2006;25:1041---5.
4.Yang J, Uchida I. Mechanisms of etomidate potentiation of GABAAreceptor-gatedcurrentsinculturedpostnatal hippocam-palneurons.Neuroscience.1996;73:69.
5.Tiippana EM, Hamunen K, Kontinen VK, et al. Do surgical patients benefit from perioperative gabapentin/pregabalin? A systematic review of efficacy and safety. Anesth Analg. 2007;104:1545---56.
7.HuterL,SchreiberT,GugelM,etal.Low-doseintravenous mida-zolam reducesetomidate-induced myoclonus: a prospective, randomizedstudyinpatientsundergoingelectivecardioversion. AnesthAnalg.2007;105:1298---302.
8.HueterL,Schwarzkopf K,SimonM,etal. Pretreatmentwith sufentanilreducesmyoclonusafteretomidate.Acta Anaesthe-siolScand.2003;47:482---4.
9.Hullander RM,LeiversD, WinglerK. Acomparison of propo-fol and etomidatefor cardioversion.Anesth Analg. 1993;77: 690---4.
10.ReddyRV,MoorthySS,DierdofSF,etal.Excitatoryeffectsand electroencephalogrphic correlationof etomidate,thiopental, methohexitalandpropofol.AnesthAnalg.1993;77:1008---11.
11.Choi JM,Choi IC, Jeong YB, et al. Pretreatment of rocuro-niumreducedthefrequencyandseverityofetomidateinduced myoclonus.JClinAnesth.2008;20:601---4.
12.Happe S, Klösch G, Saletu B, et al. Treatment of idio-pathicrestlesslegssyndrome(RLS)withgabapentin.Neurology. 2001;57:1717---9.
13.RoseMS,KamPC.Gabapentin:pharmacologyanditsuseinpain management.Anaesthesia.2002;57:451---62.
14.Asconap´eJ,DiedrichA,DellabadiaJ.Myoclonusassociatedwith theuseofgabapentin.Epilepsia.2000;41:479---81.
15.Reeves AL, So EL, Sharbrough FW, et al. Movement dis-orders associated with the use of gabapentin. Epilepsia. 1996;37:988---90.
16.KanthasamyAG,VuTQ,YunRJ,etal.Antimyocloniceffectof gabapentininaposthypoxicanimalmodelofmyoclonus.EurJ ClinPharmacol.1996;297:219---24.
17.MenigauxC,AdamF,GulgnardB,etal.Preoperativegabapentin decreasesanxietyandimprovesearlyfunctionalrecoveryfrom kneesurgery.AnesthAnalg.2005;100:1394---9.
18.AdamF,BordenaveL,SesslerDI,etal.Effectsofasingle 1200-mgpreoperativedose ofgabapentinonanxietyand memory. AnnFrAnesthReanim.2012;31:223---7.
19.TiraultM,FoucanL,DebaeneB,etal.Gabapentin premedica-tion:assessmentofpreoperativeanxiolysisandpostoperative patientsatisfaction.ActaAnaesthesiolBelg.2010;61:203---9.
20.Yoon JS, Jeon HJ, Cho SS, et al. Effect of pretreat-ment with gabapentin on withdrawal movement associated withintravenous rocuroniuminjection.KoreanJAnesthesiol. 2011;61:367---71.
21.ClarkeH,KirkhamKR,OrserBA,etal.Gabapentinreduces pre-operative anxiety and pain catastrophizingin highly anxious patientspriortomajorsurgery:ablindedrandomized placebo-controlledtrial.CanJAnaesth.2013;60:432---43.
22.NuttD,MandelF,BaldinettiF.Earlyonsetanxiolyticefficacy afterasingledose ofpregabalin:double-blind,placebo-and active-comparatorcontrolledevaluationusingadentalanxiety model.JPsychopharmacol.2009;23:867---73.
23.White PF, Tufanogullari B, Taylor J, et al. The effects of pregabalinonpreoperativeanxietyandsedationlevels:a dose-rangingstudy.AnesthAnalg.2009;108:1140---5.
24.ElBakryAEA,HatimM.Theeffectofgabapentinpremedication onpainandanxiety duringcataractsurgeryunderperibulbar block.EgyptJAnaesth.2012;28:43---7.
25.Caumo W, Schmidt AP,Schneider CN, et al. Risk factors for postoperativeanxietyinadults.Anaesthesia.2001;56:720---8.
26.KallarSK,EverettLL.Potentialrisksandpreventivemeasures for pulmonary aspiration:newconceptspreoperative fasting guidelines.AnesthAnalg.1993;77:171---82.