www.rpped.com.br
REVISTA
PAULISTA
DE
PEDIATRIA
ORIGINAL
ARTICLE
Mortality
in
the
first
24h
of
very
low
birth
weight
preterm
infants
in
the
Northeast
of
Brazil
Eveline
Campos
Monteiro
de
Castro
a,∗,
Álvaro
Jorge
Madeiro
Leite
b,
Ruth
Guinsburg
aaEscolaPaulistadeMedicina,UniversidadeFederaldeSãoPaulo(EPM-Unifesp),SãoPaulo,SP,Brazil
bUniversidadeFederaldoCeará(UFC),Fortaleza,CE,Brazil
Received27February2015;accepted21May2015 Availableonline4January2016
KEYWORDS
Pretermnewborn; Verylow-birthweight newborn;
Neonatalmortality; Earlyneonatal mortality
Abstract
Objective: Toevaluatefactorsassociatedwithneonataldeathwithin24hoursafterbirthin verylowbirthweightpretermnewborns.
Methods: Prospective cohortoflivebirths with gestationalage of230/7---316/7 weeks,birth
weightof500---1499gwithoutmalformations,in19publicmaternityhospitalsinninecapitals innortheasternBrazilfromJulytoDecember2007.The19hospitalswereassessedinrelation tophysicalresources,equipment,humanresourcesandaimingatqualityincareinitiatives. Hospital,maternalandneonatalcharacteristics,neonatalmorbidity,neonatalproceduresand interventionswerecomparedbetweenpretermnewbornsthatdiedorsurvivedupto24hours oflife.Thevariables associatedwithdeathwithin24 hoursafter birthwere determinedby logisticregression.
Results: Of the627 newborns enrolled inthe study,179 (29%) diedwithin 168hours after birth,ofwhich59(33%)upto24hoursand97(54%)upto48hoursafterbirth.Thevariables associatedwithdeath<24hwere:weight<1000g(2.94;1.32---6.53),5thminuteApgar<7(7.17; 3.46---14.88),malegender(2.99;1.39---6.47).Abetterhospitalstructurewasaprotectivefactor forearlyneonataldeath(oddsratio:0.34;95%confidenceinterval:0.17---0.71).
Conclusions: ThehighneonatalmortalityonthefirstdayoflifeincapitalcitiesofNortheast Brazilisassociatedwithbiologicalvariablessuchasweightandgenderofthenewborn,aswell aslowvitalityatbirthandaworseinfrastructureofthehospitalwherethebirthoccurred. ©2015SociedadedePediatriadeSãoPaulo.PublishedbyElsevierEditoraLtda.Thisisanopen accessarticleundertheCCBYlicense(https://creativecommons.org/licenses/by/4.0/).
∗Correspondingauthor.
E-mail:evelinecamposmc@gmail.com(E.C.M.Castro).
http://dx.doi.org/10.1016/j.rppede.2015.12.008
PALAVRAS-CHAVE
Recém-nascido pré-termo; Recém-nascidode muitobaixopeso; Mortalidade neonatal;
Mortalidadeneonatal precoce
Mortalidadecom24horasdevidaderecém-nascidospré-termodemuitobaixopeso
daRegiãoNordestedoBrasil
Resumo
Objetivo: Avaliarosfatoresassociadosao óbitoneonatalaté24horasapósonascimentode recém-nascidospré-termodemuitobaixopeso.
Métodos: Coorteprospectivadosnascidosvivoscomidadegestacionalde230/7---316/7semanas,
pesoaonascerde500---1.499gsemmalformac¸õesem19maternidadespúblicasdenovecapitais naRegiãoNordestedoBrasil dejulhoadezembrode2007. Os19 hospitaisforamavaliados comrelac¸ãoaosrecursosfísicos,equipamentos,recursos humanoseiniciativasdebuscade qualidadenoatendimento.Ascaracterísticashospitalares,maternaseneonatais,amorbidade neonatal, osprocedimentoseasintervenc¸õesneonataisforamcomparadosentreos recém-nascidos pré-termoquemorreram ou sobreviveramaté24horas.As variáveisassociadas ao óbitoaté24horasapósonascimentoforamdeterminadasporregressãologística.
Resultados: Dos627recém-nascidosincluídos noestudo,179(29%) morreramaté168horas devida, dosquais59 (33%)até24horase97(54%)até48 horas.Asvariáveis associadasao óbito<24hforam:peso<1.000g(2,94;1,32---6,53),Apgar5◦minuto<7(7,17;3,46---14,88),sexo
masculino(2,99;1,39---6,47).Amelhorestruturahospitalarfoifatordeprotec¸ãoparaoóbito neonatalprecoce(OddsRatio0,34;IntervalodeConfianc¸a95%0,17---0,71).
Conclusões: AelevadamortalidadeneonatalnoprimeirodiadevidanascapitaisdoNordeste brasileiroassocia-seavariáveisbiológicas,comoopesoeosexodorecém-nascido,assimcomo àbaixavitalidadeaonascereàpiorinfraestruturadohospitalnoqualopartoocorreu. ©2015SociedadedePediatriadeSãoPaulo.PublicadoporElsevierEditoraLtda.Esteéumartigo OpenAccesssobalicençaCCBY(https://creativecommons.org/licenses/by/4.0/deed.pt).
Introduction
Neonatal mortalityhas acquired increasing importanceas themostsignificantcauseofinfantmortality.Ofallneonatal deaths,3/4happeninthefirstweekoflife.Thefirstdayof lifehasthehighestriskofdeathandaccountsfor25---45%of alldeaths.1
TheneonatalmortalityrateremainshighinBrazil;itwas of 10:1000 live births in 2011, which is 2.5 times higher than that in the United States and Canada and about 10 timeshigherthanthatofJapaninthesameyear.2Ofthese deaths,inBrazil,26%happenonthefirstdayoflife----values underestimatedduetosparsedata.3IntheNortheastregion, earlyneonatalmortalityraterelatedtodeathsfrombirth up tosix days old is twice higher than that of the South Region.3Thehighnumberofdeathsinthefirstweekoflife inBrazil,moreconcentratedonthefirstday,isrelatedtothe careprovidedtopregnantwomenandnewbornsduringthe antepartum,intrapartum, andpostpartum period.Actions aimedatimprovingsuchassistancehavebeenrecommended toreducetheearlyneonataldeaths.4
In recent years, the prevalence of preterm births in Brazilisgrowing,firstduetotheincreaseduseofassisted reproductiontechniques,andsecond duetothequalityof prenatalcare and significant increasein the frequencyof earlyterminationsofpregnancybysurgicaldeliveries.5This findingis of concernbecause prematurityremains oneof theleadingcausesofdeathintheneonatalperiodandits increasedfrequencyhasnullifiedtheimprovementseenin thesurvivaloflowbirthweightnewbornsofwithimproved neonatalcare.5
In additiontothe inequalities in theinternational and regionalscenario, there are differences in neonatal mor-tality in different health institutions. The causes of the differencesarenotclear, evenafteradjustingforpatient characteristics.Hospitalcare playsakeyroleinmortality variationfound between the various centers.This fact is ofimportance,asthe majorityofdeliveries inBrazil take place in health institutions.6 It is suggested that health-carepractices explainthe differencesin clinical outcome ofnewborns, particularlypretermneonates;however,itis difficulttoidentifythecombinationofpracticesconsidered potentially better tomake an impactin reducing neona-talmortality.7Theidentificationofspecificgapsinquality ofcareis astarting pointand cansupportmoreeffective interventionsinreducingneonatalmortality.8
Inthiscontext,theaimofthisstudywastoevaluate fac-torsassociatedwithneonataldeathinthefirst24hofvery lowbirthweightpreterminfantsborninpublichospitalsof capitalcitiesofNortheastBrazil.
Method
Hospital-basedprospective cohort of live birthswith ges-tational age of 230/7 to 316/7 weeks and weighing ≥500
(RENOSPE),aninitiative of theMinistry ofHealth through theTechnicalDepartmentofChildHealth.Theprojectwas approvedbytheEthicsCommitteeoftheMaternitySchool Assis Chateaubriand and UNIFESP and the Data Custodian wasobtainedfromRENOSP2007.
TheresearchdevelopedbyRENOSPEwithdatacollected fromtheNeonatalIntensiveCareUnitevaluated36hospitals intheNortheaststates.Inthisstudy,weincludedonly hos-pitalslocatedinthecapitalcities(29).Ofthose,twowere excludedfornothavingmaternityandeightforhavingless than 20 patients during the collection period. Therefore, 19hospitalswereincludedinninecapitalsoftheBrazilian Northeast.
Theselectedhospitalswereservingonlypatientsofthe UnifiedHealthSystem(SUS).Datacollectionwasperformed prospectivelyinthechartofthenewborn,fromadmission to discharge or death, by a field investigator trained by RENOSPE.Datacollectedincludedhospitalcharacteristics, maternalandneonataldemographics,andclinicalevolution oftheevaluatednewborns.
The19maternityhospitalswereevaluatedusinga ques-tionnaire filled out by health professionals with respect to physical resources, equipment, human resources, and initiativesinsearchofqualityofcare,accordingtothe pre-viously published methodology,9 and two categories were proposed:Level1(L1)forthe13hospitalswithbetter infra-structure and Level 2 (L2) for the six with less qualified infrastructure.
Dataofvariablesrelatedtomaternaldemographic char-acteristics, complications during pregnancy, and use of antenatalcorticosteroidswerecollect----consideredpresent if at least one dose of corticosteroids was given before
delivery----andtypeofdelivery.Theevaluatedneonataldata wererelatedtopatientcharacteristics, proceduresin the delivery room, and the use of positive pressure ventila-tion (PPV) was defined when delivered withbag-mask or trachealtube,andthepresenceofadvancedresuscitation if PPV with heart massage and/or medications. Informa-tionconcerningthenewborn’stemperatureonadmissionto theICU werecollected,considering hypothermia<36◦C,10 respiratory distress syndrome (RDS), according toclinical and radiological criteria, and early sepsis within 72h of life withpositive blood cultures. We collect data on the procedures and interventions for neonatal care, such as the presence of transport incubator between the deliv-ery room and ICU; transfontanellar ultrasound, if there wasanyexaminationonadmission;useof continuous pos-itive airway pressure (CPAP) at any time of admission; use ofconventional mechanicalventilation atany timeof admission;surfactantadministration,regardlessofthetime used;umbilicalcatheterization,definedasintroductionof catheterintothearteryand/orumbilicalvein;useof periph-erally inserted central catheter (PICC) at some time of admission;assessmentofpainatsomepointin hospitaliza-tion,definedbytheapplicationofanypainscalevalidated forthenewborn;useofparenteralnutrition(PN),whenit wasused at anytime of admissionand ifit wasinitiated priortothe24hoflife.Theprimaryoutcomewasdeathup to24hafterbirth.
Statistical analysis initially compared the variables accordingtothepresenceorabsenceofoutcomeusingthe Mann---Whitneyorttest forquantitativevariablesand chi-square or Fisher’s exact test for qualitative variables. To identifyfactorsassociatedwithdeathwithin24hafterbirth,
27,991 live births in the 19 hospitals of the study
1083 newborns with birth weight of 500-1499 g (4%)
456 newborns excluded: - 75 congenital malformations - 21 deaths in the delivery room - 73 referred from other institutions - 24 with gestational age ≥37 weeks - 10 with gestational age <23 weeks - 253 gestational age of 32-366/7 weeks
Gestational age of 23-316/7 weeks Birth weight 500-1499g No malformations
Alagoas (n=40), Bahia (n=126), Ceará (n=158), Maranhão (n=74), Paraíba (n=25), Pernambuco (n=107), Piauí (n=48), Rio Grande do Norte (n=22), and Sergipe (n=27)
627 newborns with:
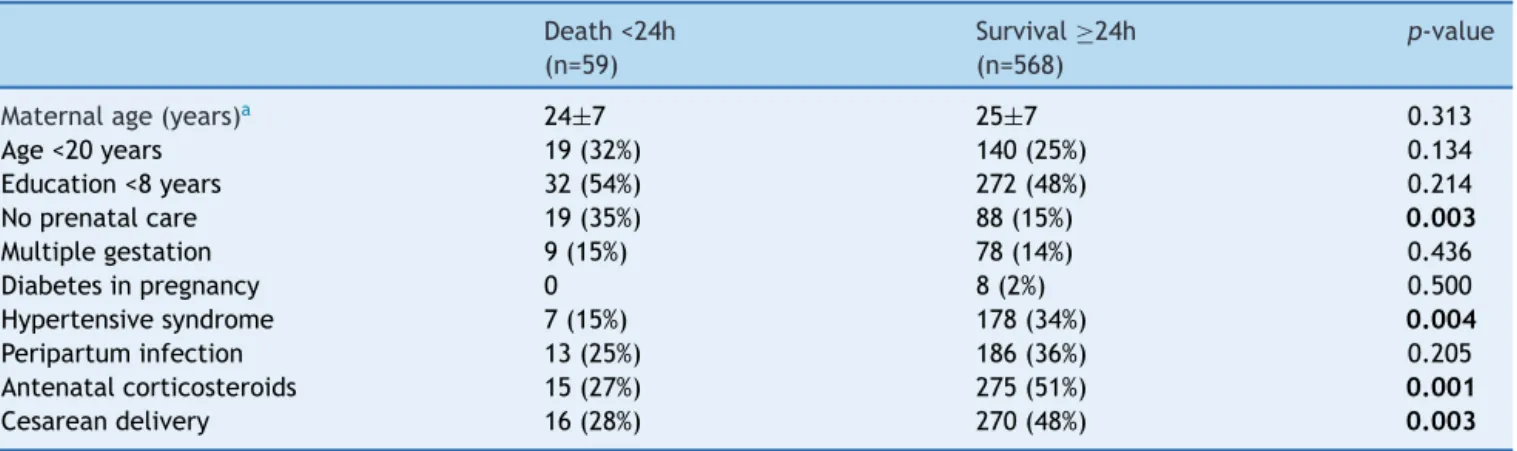
Table1 Maternalvariablesaccordingtothepresenceofneonataldeath24hafter birthofverylow birthweight preterm infantsinthecitycapitalsoftheNortheastregion.
Death<24h (n=59)
Survival≥24h (n=568)
p-value
Maternalage(years)a 24±7 25±7 0.313
Age<20years 19(32%) 140(25%) 0.134
Education<8years 32(54%) 272(48%) 0.214
Noprenatalcare 19(35%) 88(15%) 0.003
Multiplegestation 9(15%) 78(14%) 0.436
Diabetesinpregnancy 0 8(2%) 0.500
Hypertensivesyndrome 7(15%) 178(34%) 0.004
Peripartuminfection 13(25%) 186(36%) 0.205
Antenatalcorticosteroids 15(27%) 275(51%) 0.001
Cesareandelivery 16(28%) 270(48%) 0.003
a Variabledescribedasmean±standarddeviation.
logisticregressionwasperformedwiththebackward step-wise method. The independent factors introduced in the initialmodelwerethosewithp-value<0.20intheunivariate analysisandmaintenanceatp<0.05toremaininthemodel. Theassociationbetweentheindependentvariablesandthe responsevariableswasexpressedasOddsRatio(OR)and95% confidence intervals (95%CI). The final model adjustment wasevaluatedusing theHosmer---Lemeshow test. Statisti-calanalysiswasperformedusingSPSS17.0software(SPSS StatisticsforWindows,Version17.0Armonk,NY:IBMCorp.) andp<0.05wasconsideredsignificant.
Results
Duringthestudyperiod,27,991livebirthsoccurredinthe 19 hospitals included in the study; of those, 1083 were
newborns weighing 500---1499g, representing 4% of total births;456newbornswereexcludedfromthestudyand627 preterminfantswereeligible,withgestationalagebetween 230/7and316/7,weighingbetween500and1499g,without
congenitalmalformations(Fig. 1).Of neonates, 76%were borninthe13Level1hospitals.
Among the 627 newborns in the study, 179 (29%) died before168hoflife;ofwhich,59(33%)within24h.The fol-lowingdistributionof deaths according togestationalage wasobserved: 216infants with23---27 weeks,ofwhich 38 (18%)diedwithin24hand411neonateswith28---31weeks, ofwhich21(5%)diedwithin24h.
Table1showsthedistributionofmaternalcharacteristics accordingtotheoccurrenceofnewborndeathupto24hof life.Table2 shows theneonatalcharacteristics, interven-tionsinthedeliveryroom,andclinicalcomplicationsinthe first24hoflife,accordingtothepresenceofdeathofthe
Table2 Neonatalcharacteristicsaccordingtothepresenceofdeath24hafterthebirthoflowbirthweightpreterminfants inthecitycapitalsoftheNortheastregion.
Death<24h (n=59)
Survival≥24h (n=568)
p-value
BW<1000g 45(76%) 242(43%) <0.001
Birthweight(g)a 854±235 1040±252 <0.001
GA<28weeks 38(64%) 178(31%) <0.001
GA(weeks)a 27±2 28±2 <0.001
Male 40(68%) 278(49%) <0.001
1-minApgar<3 25(45%) 57(10%) <0.001
5-minApgar<7 34(61%) 81(15%) <0.001
UseofPPVinDR 46(82%) 338(60%) <0.001
Advancedresuscitation 11(21%) 26(5%) <0.001
Temp.onadmission(◦C)a 35.3±0.8 35.6±0.7 0.003
Hypothermiaonadmission 41(91%) 429(82%) 0.008
RDS 51(90%) 487(87%) 0.360
EarlysepsisBC+ 2(4%) 32(6%) 0.436
aVariabledescribedasmean±standarddeviation;BW,birthweight;GA,gestationalage;PPV,positivepressureventilation;DR,delivery
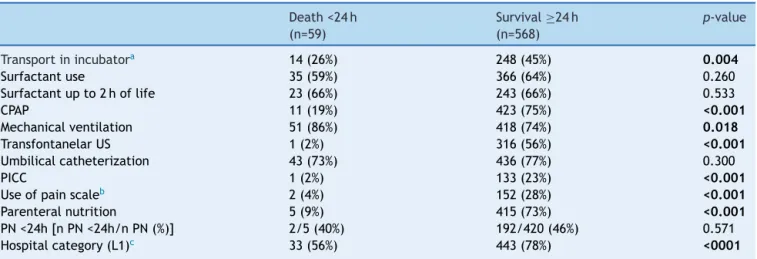
Table3 Procedures andinterventionsfor diagnosticandtherapeuticneonatalcare,accordingtothepresenceofneonatal death24hafterthebirthofverylowbirthweightpreterminfantsinthecitycapitalsoftheNortheastregion.
Death<24h (n=59)
Survival≥24h (n=568)
p-value
Transportinincubatora 14(26%) 248(45%) 0.004
Surfactantuse 35(59%) 366(64%) 0.260
Surfactantupto2hoflife 23(66%) 243(66%) 0.533
CPAP 11(19%) 423(75%) <0.001
Mechanicalventilation 51(86%) 418(74%) 0.018
TransfontanelarUS 1(2%) 316(56%) <0.001
Umbilicalcatheterization 43(73%) 436(77%) 0.300
PICC 1(2%) 133(23%) <0.001
Useofpainscaleb 2(4%) 152(28%) <0.001
Parenteralnutrition 5(9%) 415(73%) <0.001
PN<24h[nPN<24h/nPN(%)] 2/5(40%) 192/420(46%) 0.571
Hospitalcategory(L1)c 33(56%) 443(78%) <0001
aTransportationfromdeliveryroomtotheICUatbirth;HL,hoursoflife;CPAP,continuouspositiveairwaypressurebynasalprongs;
US,ultrasound;PICC,peripherallyinsertedcentralvenouscatheter.
b Useofanyvalidatedratingscaleofpain;PN,parenteralnutrition;PN24,beginningofparenteralnutritioninthefirst24hoflife. c HospitalcategoryL1,whenthehospitalservedmorethan60%oftheitemsdescribedinthemethod.
Table 4 Independent variables associated with the responsevariable‘‘deathwithin24hafterbirthofverylow birthweightpreterminfantsinthecitycapitalsofthe North-eastregion’’:finalmodelofthelogisticregressionanalysis.
OddsRatio Confidence interval96%
HospitalcategoryN1 0.34 0.17---0.71 Birthweight<1000g 2.94 1.32---6.53 5-minApgar<7 7.17 3.46---14.88
Male 2.99 1.39---6.47
Modeladjusted for the presence of prenatal care, cesarean deliveryanduseofantenatalcorticosteroids.
newborninthefirstdayoflife.Table3showsthevariables relatedtoproceduresandinterventionsforneonatalcare, accordingtosurvivalor deathonthefirstdayoflife.Itis noteworthythatofthe19selectedhospitals,13(68%)were inthecategory of hospitalswithbetterinfrastructure(L1 category), and in it the mortality on the first day of life ofthe476attendedVLBWinfantswas7%,whileinthesix hospitalsofL2categoryandinthe151patientsattendedit was17%.
Table 4 shows the results of multivariate analy-sis for death on the first day of life. It is noted that the better infrastructure----L1 hospitals----was a pro-tective factor for the assessed outcome; birth weight <1000g, Apgar score at 5min <7, and male behaved like risk factors. The logistic regression model was adjusted for the variables presence of prenatal care, cesareandelivery,anduseofantenatalcorticosteroids.The Hosmer---Lemeshowtestshowstheproperfitofthemodel, withp=0.712.
Discussion
Thismulticenterstudyshowsthatneonatalmortalityinthe first 24h of life is high in very low birth weight preterm infantsinthecapitalcitiesofnortheasternBrazil,compared withthe more developed regionsof Brazil and developed countries.Of the 627 studiedneonates, 59 (9.4%) died in thefirst24h.Inthestudyofuniversitypublicmaternitiesin theSouthandSoutheastperformedbytheBrazilian Neona-talResearchNetworkin2004,of560newbornsevaluated, excludingdeathsinthedeliveryroom,25(4.5%)diedwithin 24h. Itis noteworthythatpatients weighingbetween 400 and1499gwereincludedinthestudy,whichmayhave con-tributed to increase this percentage.11 Mohamed et al.,12 in a cohort study of neonates with birth weight between 500 and 1499g performed in the United States between 1997and2004,foundthatamongthe91,578infants stud-ied, 4579 (5%) died within 24h. The earlier the death of thenewborn,the moreitis relatedtothe antenatal con-ditions,peripartum,andchildbirthitself.Deathonthefirst dayafterbirthisassociatedwithsocialandeconomic deter-minantsrelatedtothequalityofmaternalhealthcare.13In this line of thought,there wasan attempt tounderstand howthefactorsassociatedwithdeathwithin24hafterbirth behaved.
Amongthefactorsassociatedwithneonataldeathonthe firstday oflife therearethreegroupsof variables:those relatedtothequalityofperinatalcare(hospitalcategory), thoserelatedtoneonatalbiologicalvariables(birthweight andmale),andthosereflectingcareduringlaborand deliv-ery(Apgarscoreat5min).
worsesurvival results.However,Allemanetal.15 reported that the differences in neonatal mortality between the several units cannot be explained only by the diversity of characteristics of patients admitted there, but it may bemore related tothe useof interventions predictiveof survival.Inthissense,itisnotedthatinthisstudythebest hospitalinfrastructureprotectedthenewbornagainstdeath upto24h afterbirth,decreasing thechanceof its occur-rence by 66%. It is noteworthy that, in the absence of a standardizedevaluationmodelforhospitalmaternities asso-ciatedwiththeriskofneonataldeath,aweightedscoreof thecharacteristicsrelatedtohospitalstructurewas estab-lished,inwhichthelessfrequentcharacteristicsweremost valued. According tothis score, it wasseen that mortal-ity on the first day of life of VLBW infants wastwo-fold higherinhospitalswithpoorinfrastructure(L2),compared with those who with better conditions (L1). Among the studied characteristics, more sophisticated technological features,suchasbedsideultrasoundandechocardiography, andthe potentialto reflectonthe medicalpracticeused andlearnfrompossiblemistakesandomissionsthrough clin-icalmeetingswereabsentfrommostinstitutionsclassified asL2.Thatis,althoughallhospitals analyzedwerepublic and linked to SUS, some have invested more in diagnos-tictoolsforprematurepatients,technologydependentfor theirsurvival,andsomehaveinvestedmoreinthetraining of humanresources, fundamental toapplythe technolog-ical resources in this extremely vulnerable population of newborns.
Regarding the biological factors related to neonatal deathwithin 24h after birth, we highlight the extremely lowbirth weightandmale. Among the287infants <1000g analyzedinthisstudy,45(15.7%)diedwithin24h, account-ingfor 76%ofneonates whodiedduring thisperiod.Birth weight<1000gincreasedthreetimestheriskofdeathwithin 24h,comparedtotheweightof1000---1499g.Inthe Amer-icanNeonatalNetwork,amongthe6780extremelowbirth weightpreterminfantsbornbetween1998and2003, mor-tality was 14.3% in the first 24h.16 In a population-based cohortinSãoPaulobetween2000and2001,ofalldeathsup to12hoflife, 86%hadbirthweight<1000g.17 Lee etal.18 proposed a model that includes both gestational age and birth weightin death risk assessment, with an increased riskfor eachdecreaseof 100ginbirthweightandaweek in gestationalage. In thepresent study, inthe 109 VLBW infants between 500 and 749g, mortality in the first 24h was19.3%,while inthe178with750---999gthis valuewas 13.5%. Mohamed et al.12 analyzed the survival of VLBW infants between 1997 and 2004 in the United States. In the18,863newbornsweighingbetween500and749g, mor-tality ratein the firstday of life was19.6%, while in the 17.433weighing750---999gitwas3.1%.Probably,thelower mortalityrateintheweightrangeof500---749gatbirthof theNortheastern maternitiescomparedtothe USreflects alargenumberofinfantswithintrauterinegrowth restric-tionandmoreadvancedgestationalage,whichfavorsthe chance of survival. Indeed, of the 109 infants weighing between 500 and 749g, 26 (24%) had gestational age of 28---31 weeks. It is noteworthy that in the present study, amongthe627newbornswithgestationalageof23weeks
to31 weeks and six days, birth weight between 500 and 1499g,andwithoutbirthdefects,21(3%)diedinthedelivery roomandlosttheopportunityofcareintheintensivecare unit.
Themalegenderisstronglyassociatedwithdeathinthe first 24h of life, with a risk of death three times higher comparedtowomen.Thesamefindingwasseenin-hospital mortality in other studies.19,20 Itabashi et al.21 evaluated 3065extremelowbirthweightJapaneseinfantsandfound a 1.6 higher risk of hospital death in male. Australian research findings suggest that fetal growth and survival aremediatedbysex-specificfunctionsofhumanplacenta, withbetteradaptation andresponsetooxidative stressin female.22
Among the factorsrelated tocare inchildbirth associ-ated with mortality within the first 24h after birth, the Apgarscore<7at5minishighlighted.Inapopulation-based researchintheUnitedStatesperformedbetween2001and 2002, Lee et al.18 evaluated a cohort of 690,933 infants between 24 and 36 weeks of gestation and found asso-ciation between low Apgar scores at 5min and neonatal mortality. In Sweden, between 2000 and 2002, the anal-ysis of 156 preterm infants with 23:24 weeks gestational agealsoidentifiedassociationbetweenlowApgarscoresat 5minandneonatalmortalityinthefirst24hoflife.23 The correlateof lowvitalityatbirth isthe needfor advanced proceduresofneonatalresuscitation,definedasintubation and/or heart massage and/or use of medications in the delivery room. Study of the American Neonatal Research Network, with data from 9565 preterm infants between 22 and 28 weeks, found that 67% received ventilation at birth by tracheal cannula, 8% required cardiopulmonary ressussitation, and 5% medications.24 National data indi-catethat theneed foradvanced resuscitationin verylow birthweightpreterminfantsincreasestwicethechanceof in-hospitaldeathorsurvivalwithbronchopulmonary dyspla-siaand/orsevereintracranialhemorrhage.25 Inthepresent study,itwasfoundastrongassociationof5-minApgarscore <7 with death in the first 24h of life. The risk was 7.2 higherthanthosewith5-minApgarscore=8---10.Propercare duringbirth of preterm infants in the referencehospitals in the Northeastern city capitals is outlined as a priority tomitigatethetransitiondifficultiesfor theextra-uterine life,facilitatethecardiorespiratoryadaptation,andenable clinical stabilityand reducedmortality in the firstday of life.
context,the resultsindicatethatearlyneonatalmortality especiallyinthefirst24his highin verylowbirth weight pretermpatientsinthecitycapitalsoftheNortheastregion comparedtothe moredeveloped regions of Brazil andin developed countries.Our findings revealthe existence of failuresintheintensivecareunitsassessed,withpoor hos-pitalinfrastructureandhighcontributionofextremelylow birth weight and perinatal asphyxia for mortality within the first 24h of life. Overcoming these data requires a governmentpolicy that clearly assigns responsibilities for actionsaimedat improvingthe quality,withpriority sett-ings,selectionanddefinitionsofinterventionsandconstant evaluation.
Funding
RENOSPE(MinistryofHealth,DepartmentofHealthCare,by theDepartmentofStrategicandProgrammaticActionsand theTechnicalDepartmentofChildHealthand Breastfeed-ing).
Conflicts
of
interest
A.J.M.L.coordinates theNorth-NortheastPerinatalHealth Network(RENOSPE).Theauthorsdeclarehavingno relation-shipwithanypersonororganizationthatcouldimproperly influencethestudy.
Acknowledgements
TheauthorsthankDr.AnaCeciliaSucupiraandProf.SL.Dr. ElsaGiugliani,CoordinatorsoftheGeneralCoordinationof ChildHealthandBreastfeedingoftheMinistryofHealthof Brazilduringthestudyperiod,forhelpingtoimplementthe North-NortheastPerinatalHealthNetwork.
References
1.LawnJE,CousensS,ZupanJ,LancetNeonatalSurvivalSteering Team.4millionneonataldeaths:when?Where?Why?Lancet. 2005;365:891---900.
2.United Nations Children’s Fund [página na Internet]. Situac¸ão Mundial da Infância 2013: crianc¸as com defi-ciência.Indicadoresbásicos[acessed14.06.14].Disponívelem: http://www.unicef.org/brazil/pt/PTsowe2013.pdf.
3.Brasil --- Ministério da Saúde. Secretaria de Vigilância em Saúde --- Departamento de Análise de Situac¸ão de Saúde. Brasil 2011: uma análise da situac¸ão de saúde e a vig-ilância da sáude da mulher. Brasília: Ministério da Saúde; 2012.
4.Organizac¸ão Pan-Americana da Saúde. Demografia e saúde: contribuic¸ãoparaaanálisedesituac¸ãoetendências.Brasília: Organizac¸ãoPanAmericanadeSaúde;2009.
5.BarrosFC,VictoraCG,MatijasevichA,SantosIS,HortaBL, Sil-veiraMF,etal.Prematuridade,baixopesoaonascererestric¸ão do crescimento intrauterino em três coortes de nascimen-tosno SuldoBrasil: 1992,1993 e2004. CadSaudePublica. 2008;24:S390---8.
6.Barros AJ, Matijasevich A, Santos IS, Albernaz EP, Victora CG. Neonatal mortality: description and effect of hospital of birth afterrisk adjustment.Rev Saude Publica. 2008;42: 1---9.
7.AmbalavananN,CarloW.Comoevitaroóbitoprecoceem pre-maturos?JPediatr(RioJ).2008;84:283---5.
8.BarrosFC, Diaz-RosselloJL. A qualidadedo atendimento de recém-nascidosdemuitobaixopesonoBrazil.JPediatr (Rio J).2007;83:5---6.
9.De Castro E, Leite Á, de Almeida MF, Guinsburg R. Perina-talfactorsassociatedwithearlyneonataldeathsinverylow birthweightpreterminfantsinNortheastBrazil.BMCPediatr. 2014;14:312.
10.WorldHealthOrganization.Thermalprotectionofthenewborn: apracticalguide.Geneva:WHO;1997.
11.Almeida MF, Guinsburg R, Martinez FE, Procianoy RS, Leone CR, Marba ST, et al. Perinatal factors associated with early deaths of preterm infants born in Brazilian Network on Neonatal Research centers. J Pediatr (Rio J). 2008;84: 300---7.
12.Mohamed MA, Nada A, Aly H. Day-by-day postnatal sur-vival in verylow birth weight infants. Pediatrics. 2010;126: e360---6.
13.Lansky S, Franc¸a E, César CC, Monteiro Neto LC, Leal MC. Mortes perinatais e avaliac¸ão da assistência ao parto em maternidades do Sistema Único de Saúde em Belo Hori-zonte,MinasGerais,Brasil,1999.CadSaudePublica.2006;22: 117---30.
14.Drumond EF, Machado CJ, Franc¸a E. Óbitos neonatais precoces: análise de causas múltiplas de morte pelo métodoGrade ofmembership. Cad Saude Publica. 2007;23: 157---66.
15.AllemanBW,Bell EF,LiL, DagleJM,Smith PB,Ambalavanan N, et al. Individual and center-level factors affecting mor-talityamong extremely lowbirth weight infants. Pediatrics. 2013;132:e175---84.
16.AmbalavananN,CarloWA,BobashevG,MathiasE,LiuB,Poole K,et al. Predictionof deathforextremely lowbirth weight neonates.Pediatrics.2005;116:1367---73.
17.DeAlmeidaMF,AlencarGP,SchoepsD,NovaesHM,Campbell O,RodriguesLC.Sobrevidaefatoresderiscoparamortalidade neonatalemumacoortedenascidosvivosdemuitobaixopeso aonascer,naregiãoSuldomunicípiodeSãoPaulo,Brasil.Cad SaudePublica.2011;27:1088---98.
18.LeeHC,SubehM,GouldJB.LowApgarscoreandmortalityin extremelypretermneonates bornintheUnitedStates. Acta Paediatr.2010;99:1785---9.
19.BallotDE, ChirwaTF,CooperPA.Determinants ofsurvivalin verylowbirthweightneonatesina publicsectorhospital in Johannesburg.BMCPediatr.2010;10:30.
20.KentAL,WrightIM,Abdel-LatifME.Mortalityandadverse neuro-logicoutcomesaregreaterinpretermmaleinfants.Pediatrics. 2012;129:124---31.
21.ItabashiK,HoriuchiT,KusudaS,KabeK,ItaniY,NakamuraT, etal.Mortalityratesforextremelylowbirthweightinfantsborn inJapanin2005.Pediatrics.2009;123:445---50.
22.Clifton VL. Review: sex and the human placenta:mediating differentialstrategiesoffetalgrowthand survival.Placenta. 2010;31Suppl.:S33---9.
23---24 gestational weeks. Acta Paediatr. 2008;97: 551---6.
24.Stoll BJ, Hansen NI, Bell EF, Shankaran S, Laptook AR, Walsh MC, et al. Neonatal outcomes of extremely preterm infantsfromtheNICHDNeonatalResearchNetwork.Pediatrics. 2010;126:443---56.