REVISTA
BRASILEIRA
DE
ANESTESIOLOGIA
OfficialPublicationoftheBrazilianSocietyofAnesthesiologywww.sba.com.br
SCIENTIFIC
ARTICLE
Anesthetic
considerations
for
robotic
cystectomy:
a
prospective
study
夽
,
夽夽
Menekse
Oksar
a,∗,
Ziya
Akbulut
b,
Hakan
Ocal
a,
Mevlana
Derya
Balbay
b,
Orhan
Kanbak
aaDepartmentofAnesthesiologyandReanimation,AnkaraAtaturkTrainingandResearchHospital,Ankara,Turkey bDepartmentofUrology,AnkaraAtaturkTrainingandResearchHospital,Ankara,Turkey
Received30July2013;accepted2September2013 Availableonline11November2013
KEYWORDS
Roboticcystectomy; Anesthesia;
Anesthesiologist
Abstract
Backgroundandobjectives: Roboticcystectomyisrapidlybecomingapartofthestandard sur-gicalrepertoireforthetreatmentofprostatecancer.Ouraimwastodescriberespiratoryand hemodynamicchallengesandthecomplicationsobservedinroboticcystectomypatients. Patients:SixteenpatientswhounderwentroboticsurgerybetweenDecember2009and Jan-uary2011wereprospectivelyenrolled.Mainoutcomemeasureswerenon-invasivemonitoring, invasivemonitoringandbloodgasanalysisperformedatsupine(T0),Trendelenburg(T1), Tren-delenburg+pneumoperitoneum (T2), Trendelenburg-before desufflation (T3), Trendelenburg (afterdesufflation)(T4),andsupine(T5)positions.
Results:ThereweresignificantdifferencesbetweenT0−T1andT0−T2withlowerheartrates. The meanarterialpressure value atT1 wassignificantly lowerthanT0.Thecentralvenous pressurevaluewassignificantlyhigheratT1,T2,T3,andT4thanatT0.Therewasnosignificant differenceinthePET-CO2valueatanytimepointcomparedwithT0.Therewerenosignificant differencesinrespiratoryrateatanytimepointcomparedwithT0.ThemeanfvaluesatT3, T4,andT5weresignificantlyhigherthanT0.ThemeanminuteventilationatT4andT5were significantlyhigherthanatT0.ThemeanplateaupressuresandpeakpressuresatT1,T2,T3, T4,andT5weresignificantlyhigherthanthemeanvalueatT0.
Conclusions: Althoughthemajorityofpatientsgenerallytolerateroboticcystectomywelland appreciatethebenefits,anesthesiologistsmustconsiderthechangesinthecardiopulmonary systemthatoccurwhenpatientsareplacedinTrendelenburgposition,andwhen pneumoperi-toneumiscreated.
© 2013SociedadeBrasileirade Anestesiologia.Publishedby ElsevierEditoraLtda.Allrights reserved.
夽 ThestudywasconductedintheDepartmentofAnesthesiologyandReanimationofAnkaraAtaturkTrainingandResearchHospital. 夽夽PresentedinEuroanaesthesiaCongress,Paris,France,9---12June2012.
∗Correspondingauthor.
E-mail:menekseoksar@gmail.com(M.Oksar).
Introduction
Radicalcystectomyremainsthegoldstandardfortreatment of bladder cancer. Since the introduction of laparoscopy, therehasbeenintenseinterestinurologicapplications.The minimallyinvasivebenefitsoflaparoscopicapproacheshave been demonstrated in decreased length of stay, intraop-erativeblood loss,postoperativepainand recovery.Since Sanchezetal.reportedthefirstcaseoflaparoscopic radi-calcystectomyformuscleinvasivebladdercancerin1995, severalauthorshave publishedpromising resultswiththis technique.1,2Theinterestinroboticsisundoubtedlyrelated
totheperceivedbenefits.
Thesearchforminimallyinvasivetechniquesfortreating urothelialmalignancyhasledtothedevelopmentofrobotic cystectomy(RC).3 RCoffersthepromiseof lower
morbid-itysurgerywithpotentiallyequivalentoncologicalcontrol, optimalimagingandmanipulationofthesurgicalarea,and lessbloodlosscomparedwithopenprocedures.4,5However,
theseproceduresarealsoassociatedwithsomechallenges. These drawbacks, which include difficulty of intravenous accessduetothecoveredarmsalongthesideofthebodyto allowtheroboticarmsapproachthepatientduringthe oper-ation,relatively long operatingtime,deep Trendelenburg position,andhighintra-abdominalpressure(IAP),canlead tospecificclinical issuessuch asrespiratoryacidosis,and anaesthesiaandposition relatedcomplications toaddress intheoperatingroom.
RC is rapidly becoming a part of the standard surgi-calrepertoirefor thetreatmentofprostatecancer.Inthe presentstudy,describingtheanaestheticchallengesrelated tothehighIAPcausedbyCO2insufflationanddeep
Trende-lenburgpositioningwasaimedaswellasthemanagement ofthesechallenges,inRCpatients.Additionally,describing thecriteriaforsafedischargefromtheoperatingroomwas thesecondaimofthestudy.
Methods
Studydesign
Ethicalapprovalfromthelocalinstitutionalcommitteeand written informed consent from each consecutive patient wereobtained.Sixteenconsecutivepatientswhounderwent RCbetweenDecember2009andJanuary2011were prospec-tivelyenrolledinthestudy.Sixty-ninepatients underwent roboticurologicalsurgeriesduringthisperiodinour institu-tion(16RC,53roboticprostatectomy).
Non-invasivemonitoring(ECG,pulseoximetry,body tem-perature,andrespiratoryparameters),invasivemonitoring (meanarterial pressure and central venous pressure,and ventilatory parameters) (Infinity Delta patient monitor, DraegerMedicalSystems,Inc.,Telford,PA18969,USA)and blood gas analysis were performed at supine (T0),
Tren-delenburg (T1), Trendelenburg+pneumoperitoneum (T2),
Trendelenburg-beforedesufflation(T3),afive-degree
Tren-delenburg+pneumoperitoneum (T4), and supine (T5)
pos-itions.
After anaesthesia induction with pentobarbital 4---7mg/kg and rocuronium 0.6mg/kg, endotracheal intubation was performed. Anaesthesia was maintained
with remifentanil (50mcg/mL) 1mcg/kg/min in a 0.1mcg/kg/min infusion and with 2% sevoflurane, with additionalbolusesofrocuroniumasneeded.Eachpatient’s lungs were ventilated in volume-controlled ventilation modeusing50%oxygeninairwithasettidalvolume(VT) and/orwithbreathingfrequency(f)toachieveanend-tidal carbon dioxide pressure (PET-CO2) of 25---30%, which was
monitoredwithbloodgasreportstocheckitssuitabilityin parallel.Fluidmanagement wasconsidered in2 intervals, beforeandafterureteralanastomosis.Fluidwasrelatively restricted before ureteral anastomosis in an orthotopic bladder substitutedileal loop casesof the RC group.The second interval included a higher infusion rate to reach 2---3mL/kg/h of the total fluid amount throughout the operation.
Anarterialcatheterwasinsertedintheleftradialartery andcentralvenouscatheterizationwasperformedthrough therightinternaljugularveintomeasurethecentralvenous pressure(CVP).CVPwaszeroedandmeasuredonthe mid-axillary line at the 4th intercostal space in the supine position. The peripheral intravenous access and arterial accesswerelengthenedvialinestobeachievedastheupper extremitiescannotbereachedduetobecoveredalongside the patients bodies. Ondansetron 4mg was administered intravenously,andorogastric tubingwasinsertedwiththe patientinthesupinepositiontosavetheairwayfromgastric contentsanddrainitproperlyduringadeepTrendelendurg position. Silicon pads were usedto supportthe shoulders toavoid abrachialplexus damage duetothe position.In additiontotheextremitiespatientsbodiesarefixedtothe surgical table usingchest beltswhich wereallowed chest expansion duringventilation properly. The intraperitoneal pressurewasadjustedto18mmHg.Cerebralprotectionwas assuredbyadministeringdexamethasonesodiumphosphate 8mgatthebeginningoftheoperation.
Duringextubation,thepatientsweretakenintoareverse Trendelenburg position, and diuretic wasadministered to decreaseupper airwayedema, which mightworsen respi-ratory acidosis after the extubation and be caused by the prolonged use of the deep Trendelenburg position. Extubation was approved after a blood gas analysis con-firmednormocapniaduringminimallyassistedspontaneous breathing and during spontaneous breathing of 10L/min of ventilation on average, in the absence of or with reduced conjunctival, upper airway and tongue oedema, withreversaloftheneuromuscularblockade,andatabody temperatureof35◦Cormore.
Safe extubation was performed in the operating room according toourdischargecriteriaandwasproperly man-aged in RC cases as noted in Table 1. Complications fromdeepTrendelenburgpositioningandanaesthesiawere recordedduringandaftersurgery.Thepatientswere clas-sifiedaccordingtotheirarterialpHlevelsatT5aspH<7.35
andpH>7.35classestodeterminethetypesofacidosisthat developedintraoperatively.
Statisticalanalysis
Table1 Anintegratedchecklistforthesafeextubationand dischargeofroboticcystectomypatientsfromtheoperating room/recoveryroom.
Beforeextubation Adequatebreathing
Reversalofneuromuscularblock
Noorimprovedheadandneckhyperemia Noorimprovedrespiratoryacidosis Noorimprovedtongueedema
Noorimprovedswollenand/orwhiteanddull-appearing tongue
Noorimprovedconjunctivaledema
Normocapniainbloodgasanalysisand10L/minMMVon averageduringspontaneousventilation
Afterextubationintheoperatingroom
Nosnoringduringeitherinspirationorexpiration(or whenthepatientisawake,nosignofbeingaffectedby theneuromuscularblock)
Noloudinspiration(whenthepatientisawake)andno signthatthepatientisaffectedbytheneuromuscular block
Noinspiratorydifficultyordistress(intercostal retraction,supraclavicularretraction,orretractionof thealaenasiduringinspiration)
MMV:meanminuteventilation.
QSquaretestwascarriedouttocomparethenominal varia-bles.
Results
Inthisstudytrendsofcirculatory,respiratoryandmetabolic parameters were recorded during sixteen procedures of roboticcystectomyandanalysedtheeffectsof Trendelen-burgpositionandpneumoperitoneumonthoseparameters. SixteenRCpatients(1female,15males)wereincluded in thestudy.The meanage was66.45±12.73,bodymass index (BMI) was 24.20±3.62, basal metabolic index was
−24.20±3.62, and American Society of Anesthesiologists (ASA)scorewas2.30±0.82forthestudygroup.Asforthe surgical variables, surgical time was 475.00±99.50min., Trendelenburg time was 512.86±105.82min., blood loss was 240.00±54.77mL, total fluids administered was 2533.33±864.58mL. NaHCO3 was administered in 100%
patients, and atropine wasadministrated in 87.5% of the patients.
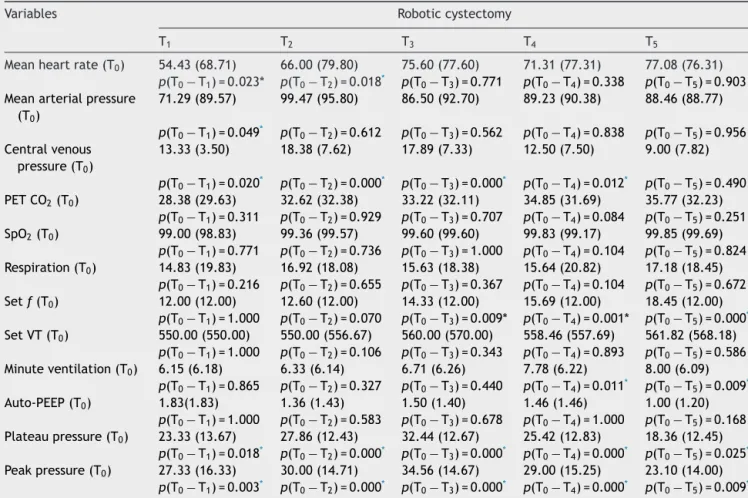
Table 2 shows the differences between the T0 value
and the T1, T2, T3, T4, and T5 values for the
hemody-namicandrespiratorydata,andventilatorysettings.There weresignificantdifferencesbetweenT0−T1(p=0.023)and
T0−T2 (p=0.018)withlowerheartrates. The mean
arte-rialpressure(MAP)valueatT1wassignificantlylowerthan
T0(p=0.023).TheCVPvaluewassignificantlyhigheratT1,
T2,T3,andT4thanatT0 (p=0.020,p=0.0001,p=0.0001,
p=0.012,respectively).Therewasnosignificantdifference inthePET-CO2 valueatanytimepointcomparedwithT0.
Therewerenosignificantdifferencesinrespiratoryrateat any time point compared with T0. The mean f values at
T3,T4,andT5 weresignificantlyhigherthanT0 (p=0.009,
p=0.001,p=0.0001,respectively).The meanminute ven-tilation(MMV)at T4 and T5 weresignificantly higherthan
atT0(p=0.011,p=0.009,respectively).Themeanplateau
pressuresandpeakpressuresatT1,T2,T3,T4,andT5were
significantly higher than the mean value at T0 (p=0.018,
p=0.0001, p=0.0001, p=0.0001, p=0.025, respectively). Nosignificant differencewasobserved in theSPO2 values
andinthepulmonaryend-expiratorypressure(PEEP)values atanytimepointcomparedwithT0(p>0.05).
Patients with a pH<7.35 exhibited significantly higher PaCO2 levels, compared with those with pH>7.35 at T5
(p=0.003).LactatelevelsinpatientswithapH<7.35were significantlylowerwhencomparedwiththosewithpH>7.35 atT5(p=0.002).BEandHCO3levelsatT5didnotshow
sig-nificantdifferencesbetweenpatientswithapH<7.35atT5 andpatientswithapH>7.35atT5(p=0.170,andp=0.340, respectively) (Table 3). There were no significant differ-encesinthesettidalvolume(setVT)orthesetbreathing frequency (set f) at any time point during the operation between the patients with a pH<7.35 and those with a pH>7.35(Table4).
Thesurgicalcomplicationsobservedincludedarthralgia anddigitinjury(6.3%),regurgitation(6.3%),loudinspiration (6.3%),headandneckedema(12.5%),arrhythmia (bradycar-dia)(18.8%),needforICU(31.3%),andconjunctivaledema (43.8%).
Discussion
In the past several years, minimally invasive robotic approachhascometotheforefrontofattentionfor many urologicmalignanciesincludingRCforinvasivebladder can-cer. The surgical robot has been aggressively marketed duringthepast decadewiththepromiseofreducing peri-operativemorbidityandimprovingoncologicandfunctional outcomesin manyorgansites.6,7 Althoughthe
anaesthesi-ologistsneedtobefullyawareof,andpreparedtohandle, thechallengesgeneratedbyadeepTrendelenburgposition andhighIAPinthatpositionrelatedtothisnewtechnology, andmanage the associatedcomplications, data regarding theanaestheticchallengesrelatedwithRCarestilllacking. There are two ways to ventilate the patient during RC, either via pressure-controlled or volume-controlled ventilation.Bothmethodsoffsettheeffectsof pneumoperi-toneumandabnormalpositioningtomaintainthepatient’s respiratory mechanics and hemodynamics within a nor-mal range. Balick-Weber et al. investigated the effects ofpressure-controlledversusvolume-controlledventilation andshowed nohemodynamic benefitof onemethod over the other during open prostatectomy. However, pressure-controlledventilationdecreasedpeakairwaypressureand increased mean airway pressure during the procedure.8
This study was replicated by Choi et al.9 They reported
Table2 Hemodynamicandrespiratorydataandventilatorysettingsinroboticcystectomy.
Variables Roboticcystectomy
T1 T2 T3 T4 T5
Meanheartrate(T0) 54.43(68.71) 66.00(79.80) 75.60(77.60) 71.31(77.31) 77.08(76.31) p(T0−T1)=0.023* p(T0−T2)=0.018* p(T0−T3)=0.771 p(T0−T4)=0.338 p(T0−T5)=0.903
Meanarterialpressure (T0)
71.29(89.57) 99.47(95.80) 86.50(92.70) 89.23(90.38) 88.46(88.77)
p(T0−T1)=0.049* p(T0−T2)=0.612 p(T0−T3)=0.562 p(T0−T4)=0.838 p(T0−T5)=0.956
Centralvenous pressure(T0)
13.33(3.50) 18.38(7.62) 17.89(7.33) 12.50(7.50) 9.00(7.82)
p(T0−T1)=0.020* p(T0−T2)=0.000* p(T0−T3)=0.000* p(T0−T4)=0.012* p(T0−T5)=0.490
PETCO2(T0) 28.38(29.63) 32.62(32.38) 33.22(32.11) 34.85(31.69) 35.77(32.23)
p(T0−T1)=0.311 p(T0−T2)=0.929 p(T0−T3)=0.707 p(T0−T4)=0.084 p(T0−T5)=0.251
SpO2(T0) 99.00(98.83) 99.36(99.57) 99.60(99.60) 99.83(99.17) 99.85(99.69)
p(T0−T1)=0.771 p(T0−T2)=0.736 p(T0−T3)=1.000 p(T0−T4)=0.104 p(T0−T5)=0.824
Respiration(T0) 14.83(19.83) 16.92(18.08) 15.63(18.38) 15.64(20.82) 17.18(18.45)
p(T0−T1)=0.216 p(T0−T2)=0.655 p(T0−T3)=0.367 p(T0−T4)=0.104 p(T0−T5)=0.672
Setf(T0) 12.00(12.00) 12.60(12.00) 14.33(12.00) 15.69(12.00) 18.45(12.00)
p(T0−T1)=1.000 p(T0−T2)=0.070 p(T0−T3)=0.009* p(T0−T4)=0.001* p(T0−T5)=0.000*
SetVT(T0) 550.00(550.00) 550.00(556.67) 560.00(570.00) 558.46(557.69) 561.82(568.18)
p(T0−T1)=1.000 p(T0−T2)=0.106 p(T0−T3)=0.343 p(T0−T4)=0.893 p(T0−T5)=0.586
Minuteventilation(T0) 6.15(6.18) 6.33(6.14) 6.71(6.26) 7.78(6.22) 8.00(6.09)
p(T0−T1)=0.865 p(T0−T2)=0.327 p(T0−T3)=0.440 p(T0−T4)=0.011* p(T0−T5)=0.009*
Auto-PEEP(T0) 1.83(1.83) 1.36(1.43) 1.50(1.40) 1.46(1.46) 1.00(1.20)
p(T0−T1)=1.000 p(T0−T2)=0.583 p(T0−T3)=0.678 p(T0−T4)=1.000 p(T0−T5)=0.168
Plateaupressure(T0) 23.33(13.67) 27.86(12.43) 32.44(12.67) 25.42(12.83) 18.36(12.45)
p(T0−T1)=0.018* p(T0−T2)=0.000* p(T0−T3)=0.000* p(T0−T4)=0.000* p(T0−T5)=0.025*
Peakpressure(T0) 27.33(16.33) 30.00(14.71) 34.56(14.67) 29.00(15.25) 23.10(14.00)
p(T0−T1)=0.003* p(T0−T2)=0.000* p(T0−T3)=0.000* p(T0−T4)=0.000* p(T0−T5)=0.009*
PETCO2:endtidalcarbondioxidepressure;SPO2:saturationofperipheraloxygen;setf:setbreathingfrequency;setVT:settidalvolume. * p<0.05.
adjustments. Accordingly, the observed increases in the PET-CO2 were compensated by increases in the f and
MMV to decrease or prevent further respiratory acido-sis. Also,the plateau pressures and peak pressures were lowered by increasing the f in order toavoid generating auto-PEEP. In the present study, increasing the breathing frequencytoincreasetheMMVwasrequiredduring Trende-lenburgpositioningwithpneumoperitoneum.Furthermore,
theplateaupressurewasmonitoredtoavoidgoingbeyond a 35mmHg limit.In thedeep Trendelenburgposition,the patientstendedtodevelopauto-PEEPandhighintrathoracic pressures, which may have compromised the VT through auto-PEEPand/orareduceddrivingpressure.However,itis unknownwhetherahighIAPinadeepTrendelenburg posi-tionplacedlimitationsonthedrivingpressure,whichmight havecompromisedtheVT.Theeffectsonlungmechanicsof
Table3 ArterialbloodgasreportsbasedacidosisdeterminantsinbothpH<7.35andpH>7.35classesatT5.
Determinants pH<7.35atT5 pH>7.35atT5 p-Value
PaCO2 47.91±5.31 29.63±3.78 0.003
Baseexcess −5.46±2.81 −6.7±2.88 0.170
Lactate 4±1.41 9±1.41 0.002
HCO3 18.65±1.55 19.07±2.18 0.340
Table4 IntraoperativechangesinthesettidalvolumeandsetbreathingfrequencyatpH≥7.35andpH<7.35casesatT5.
pH<7.35atT5 pH≥7.35atT5 p-Value
Settidalvolume 466.14±120.59 543.88±84.17 0.064
deepTrendelenburgpositioningandahighIAPof18mmHg are alsounknown. Therefore,the main clinical challenge in the present study was the choice of ventilation strat-egy tomanage respiratory acidosis. The VT wasadjusted toprovideadequate ventilationwithout exceedingapeak airway pressure of 40cm H2O. As VT wasreduced in the
deep Trendelenburg position, an adjustment to MMV was requiredusingf.Toavoidorminimizeauto-PEEP,the breath-ingfrequency wasadjusted toallow completeexhalation, withaninspiration-to-expirationratio(I/E)of1/2. Respira-toryacidosiswasfurtherminimizedbyreducingthealveolar deadspaceasneeded.Kalmaretal.ventilatedthelungsin volume control mode with an O2/air mixture and a PEEP
of 5cm H2O.The tidalvolumewasadjusted toachieve a
PET-CO2 gradient between 30 and 35mmHg. The PET-CO2
gradient increased from7.95mmHg beforeTrendelenburg positioningto 10.95mmHg after120min of steep Trende-lenburg.PET-CO2andPaCO2werehighlycorrelated.10Inour study,theincreasedPET-CO2mayhavebeenduetotheuse
ofa largeamount of totalCO2during insufflationpriorto
extubation and may have been due to inspiration and/or exhalationdifficulties.Additionally,asanon-invasive, indi-rectmeasurementofPaCO2,PET-CO2isanaccuratemeans
of monitoring PaCO2, and deepTrendelenburg positioning
doesnotdiminishitsusefulness.
Pneumoperitoneum is used in laparoscopic cases for proper visualization of the surgical field. Pressures are typically in the 12---15mmHg range and CO2 is the most
common gas used, although other inert gases have been studied. Pneumoperitoneum has profound effects on the cardiac,renal,pulmonary,andimmunesystems.Theeffects of pneumoperitoneum are attributed to two factors: the IAP itself and CO2 acting as a drug. Peritoneal
insuffla-tion to IAPs greater than 10mm Hg induces significant alterations in hemodynamics.11,12 Meiningeret al.studied
cardiopulmonary effects of steep Trendelenburg position-ing and pneumoperitoneumspecifically relatedto robotic urologic procedures.13,14 MMV was adjusted according to
repeatarterialblood gasanalysistopreventhypercapnia. A significantly elevated arterial CO2 pressure even after
releaseofthepneumoperitoneumisattributedtothe con-siderable amountsof CO2 possiblystored in extravascular
compartmentsofthebodythatareslowlyredistributedand metabolizedorexhaled.15 Although anincreasein arterial
pressureandanunchangedorslightlyincreasedHRare asso-ciatedwiththeseconditions,adropin cardiacoutputhas been reportedduring peritoneal insufflation,whether the patientisplacedinthehead-downorhead-upposition.16---18
Torrielli etal. reported that increasing the IAP to 10mm Hgwasassociatedwithadecreaseinthecardiacindexthat returnedtoitsinitialvalueafter10minof10◦Trendelenburg
positioning.TheyalsoreportedthatelevatedIAPwas asso-ciatedwithincreasesintheMAPandthesystemicvascular resistance,andthesevaluesdidnotreturntonormalafter peritonealexsufflation.16Falabellaetal.demonstratedthat
Trendelenburgpositioningincreasedthestrokevolumeand pneumoperitoneumandsteepTrendelenburgposition signif-icantly increase MAP.19 In the present study, whereas the
MAP increased significantly at the beginning of the Tren-delenburg positioning with pneumoperitoneum, the CVP increased throughout the Trendelenburg positioning. The increases in the CVP values in both deep Trendelenburg
and5◦ Trendelenburgpositioning,withandwithout
pneu-moperitoneum,andthedecreasestobaselineattheendof theoperationin thesupinepositionindicatea close rela-tionshipbetweenCVPvaluesandTrendelenburgpositioning aloneor withIAP. Furthermore, the HRdecreased signifi-cantlyandrequiredintervention.Althoughthemostobvious hemodynamic effects of the RC procedures in our study occurredimmediately afterthepatients weremovedinto theTrendelenburgpositionwithpneumoperitoneum,these measurementscontinuedtobeaffectedtoalesserdegree untiltheendoftheprocedures.
Although the blood gas analyses were used to assess bothrespiratoryand metabolicproblems,the presenceof acidosiswasdeterminedat theendof theoperation(T5).
Increasesin the set VT or the set f reflected respiratory acidosismanagementduringtheoperationatbothpH lev-els.Significantincreasesinthefvalueswereinterpretedto meanthattheMMVhadbeenmaintainedandthatthe PET-CO2 and PaCO2, which had increaseddue tothe reduced
VTduring Trendelenburgpositioningand CO2
pneumoperi-toneum,had decreased.The increasesin theVTand/or f weretheresultofoureffortstomaintaintheMMVandto managerespiratoryacidosis.Eventhoughrespiratory acido-siswasaprobleminourstudygroup,metabolicacidosishad significanteffectonthepHvaluesandrequiredcorrection, whichincludedNaHCO3infusions.Normocarbiaand
mainte-nanceofanadequateMMVwerethemaingoalsintheblood gasmonitoringduringthesurgicalproceduresand extuba-tionassessment.Ourfindingssuggestthatbloodgasanalysis wasnecessaryformonitoringoftheRCpatients.AsthePaO2
andSPO2 did notdecrease tocriticalvalues,none of the
patientsrequiredadditionalinterventiontoenhancePaO2.
Inthepresent study,themetabolic acidosisalonedidnot reachasignificantlevel;however,incombinationwith respi-ratoryacidosisitdecreasedthepHtoacriticallevel,which necessitatedtimely andchallenging management.In addi-tion,thedecreasesinthepHvaluesresultedfrommetabolic eventsthatmayhavebeenduetothelongsurgicaldurations suchasfluidmanagementstrategiesthatincludedthe dilu-tionoftheNaHCO3inlarge-volumeinfusionsandincreases
inthehydrogenionconcentrationsinthevolumerestriction periodduringlengthysurgicalprocedures.HCO3 losscould
havealsoresultedfromilialbowellossduetopouch forma-tionduringthesurgicalprocedures.Noneofthepatientsin ourstudygroupexhibitedhypothermiacausedbyheatloss duetolongsurgerydurationsorinsufflationwithcold CO2
gas,whichmighthaveaddedtothemetabolicacidosis.The greaterNaHCO3useduringsurgeryinthepH>7.35casesat
T5indicatesthatthemetabolicacidosisinourstudywaswell
managed.
Pruthi et al. reported6.1h of surgical timefor cysto-prostatectomyandameanbloodlossof313mL.3Thesame
authorsreportedameanoperatingroomtimeof4.6hforall cystectomycasesandameansurgicalbloodlossof271mL. Priorstudieshave demonstratedthatthereis asignificant learningcurve tothe roboticapproach,whereasafterthe firsttwenty cases a gradual reduction in operative times canbe perceived.20,21 Lowrence etal.22 reporteda mean
demonstrated a significant increase in operative times associated with the robotic approach, the one previous prospective randomized series showed a difference of 4.2 versus 3.5h for the robotic versus the open group respectively.21,24OurRCcaseshadlongersurgicaltimes.In
ourcurrentserieswehaveshownthattheroboticapproach demonstratedasignificantincreaseinoperativetimes.
Ina studyof thetransfusionrequirements in openand robotic-assistedlaparoscopicradicalprostatectomies, Kor-danetal.demonstratedthatroboticsurgerywasassociated withlowerblood lossand asmaller change in hematocrit thantheopenprostatectomygroup.25Ithasbeenreported
that extensive blood loss and blood transfusion require-mentspredictahigherlikelihoodofileusandpostoperative complications in open cystectomy series.26 Boström et al
studiedrisk factorsformortalityandmorbidity relatedto openradicalcystectomyandconcludedthatahighASAscore andincreasingnumberoftransfusionswerepredictorsofa majorcomplication.26Meanbloodlossinastudyofopen
rad-icalcystectomies byLowranceetal.was750mLwith38% ofpatientsrequiringbloodtransfusion.20 Inourstudy,none
ofthepatientsrequiredtransfusionsandourlowoperative bloodlosscomparesfavourablytoouropenexperienceand thatofotherreportsintheliterature,andissimilartothe bloodlossseeninotherroboticcystectomyreports.
Although complications with the robotic approach are certainlypresent, thoserelatedtoanaesthesiahave been rare.IthasbeenestablishedthatdeepTrendelenburg posi-tioningcancausedecreasesinfunctionalresidualcapacity, totallungvolume,andpulmonarycomplianceandmay facil-itatethedevelopmentofatelectasis.27Tongueswellingmay
have resulted fromthe Trendelenburg positioning, or the endotracheal cuff pressure on the tongue base. Applying pressure to the tongue base with an endotracheal tube cuff may also enhance tongue oedema. The use of the head-uprightpositionpriortoextubation,diureticusewhen necessaryandextubationitselfimprovedthesesymptoms. In the present study, themost frequent anaesthesia-and position-related complicationswere conjunctival oedema, regurgitationand‘‘upperairwayobstruction-like’’clinical symptoms (enlarged and dull, oedematous tongues, snor-ing,loudinspiration,inspiratorydifficulty)thatmightlead toorworsenrespiratoryacidosis.Ourcriteriafordischarge fromtheoperating/recoveryroomincluded improvements in these upper airway signs and symptoms. Most of the complicationsdocumentedinourstudycouldbemanaged withtheprecautionsandmedicationswithoutanyneedfor admissiontotheICU.Yeeetal.arereportedrareand tempo-raryneurologiccomplicationsonthe1stpostoperativeday thatlastedfor3days.However,inthepresentstudy,no seri-ousneurologiccomplications wereobserved.28 Arrhythmia
canbeinduced byseveralcausesinlaparoscopiccases.In ourstudy,bradycardiaaccountedformostofthearrhythmia cases,andthesecomplicationsoccurredimmediatelyafter the patients were movedinto the Trendelenburg position and/or preceding the surgical procedure. We interpreted thistimingasindicatingthatthearrhythmiaresultedfrom theTrendelenburgpositionand/or thereflexes inducedby thesuddenstretchingofthepneumoperitoneum,whichmay have caused an increase in vagal tone. Additionally, the remifentanilinfusionmayhasaroleinbradycardiainthese cases.However, thebradycardia was notobserved during
theremifentanilinfusionsinanyotherpartsofthesurgical procedures.
Tohandlethesepatients,werecommendthatthe Tren-delenburg position shouldbe given carefullyto avoid any neurologicdamage,arthralgiaordigitinjury.Shouldersand feetshouldbesupportedproperlyandchestshouldbefixed without compromising chest expansion during ventilation. Cerebraledema should beprevented; respiratory acidosis should bemanaged according toETCO2 that waschecked
withPaCO2inparallelduringpenumoperitoneum.Metabolic
acidosispossiblycausedbyfluidrestrictionuntilthe ortho-topicbladdersubstitutedilealloopandtheNaCO3lossdue
tothelossesfromandthroughthebowelshouldbeidentified andtreatedinthesedebilatedsurgicalpatients.Body tem-peratureshouldbemonitoredinthisrelativelylongsurgical proceduresasitmayaffectthemetabolicevents.Arteriel catheterisationishelpfulbutCVPcatheterisnotessential. Duringtheextubationhyperventilationmaybenecessaryto exchangetheincreasedCO2 inthelungsduetorecovered
cardiacoutputandCO2resorbtionfromthetissues.Headup
rightpositionanddiureticadministrationcanproviderelief totheupperairwayandheadandneckedema,whichcan helpasuccessfulextubationperiod.Duringthisperiod,using achecklistaswedescribedinTable1canhelpasafe extu-bationasconsideredthemostpossibleproblemstothistype ofsurgery.
ThemajorityofpatientsgenerallytoleratesRCwelland appreciates the benefits; however, anesthesiologists must have an intimate knowledge of the physiological changes associatedwithroboticurologicalprocedures.Specifically, anesthesiologists must consider the changes in the car-diopulmonarysystem thatoccurwhen patientsareplaced inTrendelenburgposition,andwhenpneumoperitoneumis created.Knowledgeofthesechangescanhelpguide appro-priate interventions and prevent complications and help speedrecoverytimeforpatients.
Conclusions
Robotic cystectomy is rapidly becoming a part of the standard surgicalrepertoirefor thetreatment ofprostate cancer.Theaimofthepresentstudywastodescribe respi-ratoryandhemodynamicchallengesandthecomplications observed in robotic cystectomy patients. Although the majority ofpatientsgenerallytolerateroboticcystectomy well and appreciate the benefits, anesthesiologists must consider the changesin the cardiopulmonarysystem that occurwhenpatientsareplacedinTrendelenburgposition, andwhenpneumoperitoneumiscreated.
Conflicts
of
interest
Theauthorsdeclarenoconflictsofinterest.
References
2.Abdel-HakimAM,BassiounyF,Abdel AzimMS,etal. Laparo-scopic radical cystectomy with orthotopic neobladder. J Endourol.2002;16:377---81.
3.PruthiRS,NielsenME,NixJ,etal.Roboticradicalcystectomy forbladdercancer:surgicalandpathologicaloutcomesin100 consecutivecases.JUrol.2010;183:510---4.
4.Menon M, Shrivastava A, Tewari A. Laparoscopic radical prostatectomy: conventional and robotic. Urology. 2005;66 Suppl:101---4.
5.Hu JC, Gu X, Lipsitz SR, et al. Comparative effectiveness of minimally invasive vs open radical prostatectomy. JAMA. 2009;302:1557---64.
6.YatesDR,VaessenC,RoupretM.FromLeonardotodaVinci: the history of robot-assisted surgery in urology. BJU Int. 2011;108:1708---13.
7.RichardsKA,KaderK,HemalAK.Roboticradicalcystectomy: wherearewetoday,wherewillwebetomorrow?SciWorldJ. 2010;10:2215---27.
8.Balick-WeberCC,NicolasP,Hedreville-MontoutM,etal. Respi-ratory and haemodynamic effects of volume-controlled vs pressure-controlled ventilation during laparoscopy: a cross-overstudywithechocardiographicassessment. BrJAnaesth. 2007;99:429---35.
9.ChoiEM,NaS,ChoiSH,etal.Comparisonofvolume-controlled and pressure-controlled ventilation in steep Trendelenburg positionforrobot-assistedlaparoscopicradicalprostatectomy. JClinAnesth.2011;23:183---8.
10.Kalmar AF, Foubert L, Hendrickx JF, et al. Influence of steepTrendelenburgpositionandCO(2)pneumoperitoneumon cardiovascular, cerebrovascular, and respiratory homeostasis duringroboticprostatectomy.BrJAnaesth.2010;104:433---9. 11.Struthers AD, Cuschieri A. Cardiovascular consequences of
laparoscopicsurgery.Lancet.1998;352:568---70.
12.KoivusaloAM,LindgrenL.Effectsofcarbondioxide pneumoperi-toneumfor laparoscopic cholecystectomy.Acta Anaesthesiol Scand.2000;44:834---41.
13.MeiningerD,WestphalK,BremerichDH,etal.Effectsofposture andprolongedpneumoperitoneumonhemodynamicparameters duringlaparoscopy.WorldJSurg.2008;32:1400---5.
14.MeiningerD,ByhahnC,MierdlS,etal.Positiveend-expiratory pressureimprovesarterialoxygenationduringprolonged pneu-moperitoneum.ActaAnaesthesiolScand.2005;49:778---83. 15.LeggettRW.Abiokineticmodelforcarbondioxideand
bicar-bonate.RadiatProtDosimetry.2004;108:203---13.
16.TorrielliR,CesariniM,WinnockS,etal.Hemodynamicchanges duringcelioscopy:astudycarriedoutusingthoracicelectric bioimpedance.CanJAnaesth.1990;37:46---51[inFrench]. 17.Walder AD, Aitkenhead AR. Role of vasopressin in the
haemodynamicresponsetolaparoscopiccholecystectomy.BrJ Anaesth.1997;78:264---6.
18.JorisJL,ChicheJD, CanivetJL,etal.Hemodynamicchanges inducedbylaparoscopyandtheirendocrinecorrelates:effects ofclonidine.JAmCollCardiol.1998;32:1389---96.
19.Falabella A, Moore-Jeffries E, Sullivan MJ, et al. Car-diac function during steep Trendelenburg position and CO2 pneumoperitoneum for robotic-assisted prostatectomy: a trans-oesophageal Doppler probe study. Int J Med Robot. 2007;3:312---5.
20.Menon M, Hemal AK, Tewari A, et al. Nerve-sparing robot-assistedradicalcystoprostatectomyandurinarydiversion.BJU Int.2003;92:232---6.
21.PruthiRS,SmithA, WallenEM.Evaluatingthelearning curve forrobot-assistedlaparoscopicradicalcystectomy.JEndourol. 2008;22:2469---74.
22.LowranceWT,RumohrJA,ChangSS,etal.Contemporaryopen radicalcystectomy:analysisofperioperativeoutcomes.JUrol. 2008;179:1313---8.
23.NgCK,KauffmanEC,LeeMM,etal.Acomparisonof postopera-tivecomplicationsinopenversusroboticcystectomy.EurUrol. 2010;57:274---81.
24.RheeJJ,LebeauS,SmolkinM,etal.Radicalcystectomywith ileal conduit diversion: early prospective evaluation of the impactofroboticassistance.BJUInt.2006;98:1059---63. 25.Kordan Y, Barocas DA, Altamar HO, et al. Comparison
of transfusion requirements between open and robotic-assistedlaparoscopicradicalprostatectomy.BJUInt.2010;106: 1036---40.
26.Boström PJ, Kössi J, Laato M, et al. Risk factors for mor-tality and morbidity related to radicalcystectomy. BJU Int. 2009;103:191---6.
27.HazebroekEJ,BonjerHJ.Effectofpatientpositionon cardio-vascularandpulmonaryfunction.In:WhelanRL,FleshmanJW, FowlerDL,editors.Thesagesperioperativecareinminimally invasivesurgery.NewYork:Springer;2006.p.410---7.