w w w . r b o . o r g . b r
Original
article
Total
knee
arthroplasty
with
mobile
tibial
weight-bearing:
clinical
evaluation
after
a
minimum
of
five
years
of
postoperative
follow-up
夽
Luiz
Gabriel
Betoni
Guglielmetti
∗,
Pedro
Pereira
da
Costa,
Ricardo
de
Paula
Leite
Cury,
Victor
Marques
de
Oliveira,
Nilson
Roberto
Severino,
Osmar
Pedro
Arbix
de
Camargo
FaculdadedeCiênciasMédicasdaSantaCasaSãoPaulo(FCMSCSP),SãoPaulo,SP,Brazil
a
r
t
i
c
l
e
i
n
f
o
Articlehistory:
Received3April2014 Accepted5May2014 Availableonline30May2015
Keywords:
Replacementarthroplasty Knee
Kneeprosthesis Kneeosteoarthritis
a
b
s
t
r
a
c
t
Objective:Toevaluatethemediumandlongtermresultsfromtotalkneearthroplastywith rotatingtibialweight-bearing.
Methods:BetweenJanuary2000andJuly2007,162patientsunderwenttotalknee arthro-plastywithmobiletibialweight-bearing.Amongthese,96wereevaluatedinaprevious studywithameanfollow-upof4years.Inthepresentstudy,thesamegroupwasinvited backforreassessmentandtheresultswereanalyzed.Sixty-ninepatientsrespondedtothis call(79knees),andtheywereevaluatedinaccordancewiththeKneeSocietyRatingSystem (KSRS),afterameanfollow-upof8yearsand8months(rangingfrom5.5and13years).
Results:AmeanKSRSscoreof74.41pointswasobtained,withgoodorexcellentresults.
Conclusion:Themediumandlong-termresultsfromtotalkneearthroplastywithmobile tibialweight-bearingweregood,andameanscoreof74.41pointsintheKneeSocietyClinical RatingSystemwasattained.
©2014SociedadeBrasileiradeOrtopediaeTraumatologia.PublishedbyElsevierEditora Ltda.Allrightsreserved.
Artroplastia
total
do
joelho
com
o
apoio
tibial
móvel.
Avaliac¸ão
clínica
após
seguimento
mínimo
de
cinco
anos
de
pós-operatório
Palavras-chave:
Artroplastiadesubstituic¸ão Joelho
Prótesedojoelho Osteoartritedojoelho
r
e
s
u
m
o
Objetivo:Avaliarosresultados,emmédioelongoprazo,dasartroplastiastotaisdejoelho comapoiotibialrotatório.
Métodos:Dejaneirode2000ajulhode2007,162pacientesforamsubmetidosàartroplastia totaldojoelhocomapoiotibialmóvel.Desses,96foramavaliadosemumestudoprévio comtempodeseguimentomédiodequatroanos.Noatualtrabalho,essemesmogrupofoi
夽
WorkdevelopedintheDepartmentofOrthopedicsandTraumatology,SantaCasadeMisericórdiadeSãoPaulo,FernandinhoSimonsen Wing,SãoPaulo,SP,Brazil.
∗ Correspondingauthor.
E-mail:luizgbg@terra.com.br(L.G.B.Guglielmetti). http://dx.doi.org/10.1016/j.rboe.2015.05.004
convocado para reavaliac¸ão e os resultados foram analisados. Responderam à atual convocac¸ão69pacientes(79joelhos),queforamavaliadosconformeoKneeSociety Rat-ingSystem(KSRS),apósseguimentomédiodeoitoanoseoitomeses(variac¸ãoentre5,5e 13anos).
Resultados: Foiobtidapontuac¸ãomédiade74,41pontosnoKSRS,com78,7%deresultados bonsouexcelentes.
Conclusão: Aartroplastiatotaldojoelhocomapoiotibialmóvelobtevebonsresultadosem médioelongoprazoeatingiuamédiade74,41pontosnoKneeSocietyClinical Rating System.
©2014SociedadeBrasileiradeOrtopediaeTraumatologia.PublicadoporElsevier EditoraLtda.Todososdireitosreservados.
Introduction
Theconceptofkneearthroplastywithmobiletibial weight-bearingwasintroducedbyGoodfellowandO’Connorin1978.1 Thisinnovationwasbasedontheneedtoadaptthe compo-nentsoftheprosthesistodifferentanglesduringflexionand extension.2Itsaimwastoincreasethephysiological move-mentinthejoint andthus diminishabrasion andwearon thepolyethylenecomponent, formation ofparticles, occur-rencesofosteolysis3and,especially,patients’complaintsof pain.Thisgreaterdurabilityhasnotbeenproveninmedium andlong-termclinicalstudies.4–7However,someauthorshave achievedbetterresultsfromprostheseswithmobile weight-bearing, inrelation tostability and the actionofgoing up stairs.8,9
Biomechanicalstudies haveshownthatprostheses with mobiletibialweight-bearingreducetheincongruencecreated bynon-physiologicalrotationinimplantingthefemoral com-ponent.Severalstudies haveshown goodlong-termresults fromusingtheseimplants.However,someauthorshave indi-catedthatthereisaneedforstudieswithlong-termfollow-up andhaveproventhatthistechniquehasclinicalandsurvival advantages, in comparisonwith implants with fixed tibial weight-bearing.10–12
Theobjectiveofthispaperwastopresentthemediumand long-termclinicalresultsfromusingprostheseswithmobile tibialweight-bearinginpatientsattendedbytheKneeSurgery GroupoftheDepartmentofOrthopedicsandTraumatologyof SantaCasadeSãoPaulo.
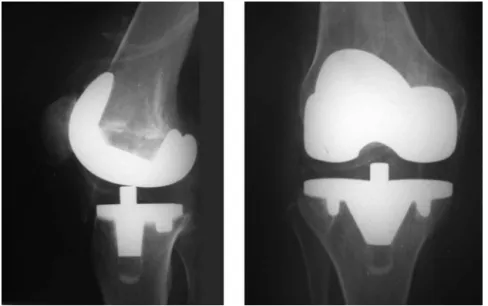
Sample
BetweenJanuary2000andJuly2007,162patientsunderwent totalkneearthroplastyinwhichpolyethylenetibial compo-nentswithrotarymovementwereused(Fig.1).Thesepatients wereinitiallyinvitedtoreturnformedium-termassessment oftheclinicalresults(meanfollow-upof4years).Onthat occa-sion,96patientsrespondedtotheinvitation,andatotalof 117knees wereevaluated.13 Thepresentstudyconsistedof reassessmentofthesesamepatientsafteraminimum post-operativeperiodof5years.
Outofthe96patientswhowereassessedintheprevious study,69respondedtotheinvitationofthepresentstudy.Ten
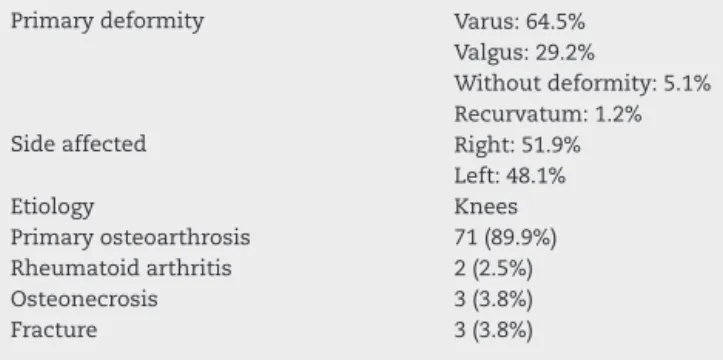
Table1–Clinicaldataandetiologyoftheosteoarthrosis ofthepatientswhounderwentarthroplasty.
Primarydeformity Varus:64.5%
Valgus:29.2%
Withoutdeformity:5.1% Recurvatum:1.2%
Sideaffected Right:51.9%
Left:48.1%
Etiology Knees
Primaryosteoarthrosis 71(89.9%)
Rheumatoidarthritis 2(2.5%)
Osteonecrosis 3(3.8%)
Fracture 3(3.8%)
ofthesehadundergonebilateralarthroplasty,andtherefore79 kneeswereevaluated.Therewere10menand59women,with agesrangingfrom53to87years(meanof75.7)and postoper-ativefollow-uprangingfrom5.5to13years(meanof8years and8months).Thedeformitiesthatformedtheindicationsfor surgeryaredescribedinTable1.Outofthe27patientswho werelostfromthefollow-up,itwasfoundthattenpatients haddiedforreasonsunrelatedtothesurgery,whiletheother losses(17)wereduetoourfailuretolocatethepatientorto patients’non-attendanceevenafterreceivingtheinvitation.
Methods
Thiswasanobservationalstudyonacohortofpatientsfrom apreviousinvestigation.13Itwasconductedinapublic uni-versity hospital (Santa Casa de São Paulo). Thestudy was approvedbytheinstitution’sethicscommittee.
Fig.1–Radiographsinanteroposterior(AP)andlateralviewsonakneethatunderwenttotalarthroplastywithmobiletibial weight-bearing.
Table2–Formforgatheringobjectivedatabasedonthe KneeSocietyRatingSystem(KSRS).14
Pain Points Deductions(atleast) Points
Absent 50 Contractureinflexion
Slightoroccasional 45 5–10◦ 2
Onlyonstairs 40 10–15◦ 5
Walkingandonstairs 30 16–20◦ 10
Severe 0 >20◦ 15
Movements Incapacitytoperform
extension
(Each5◦=1point) 25 <10◦ 5
Stability 10–20◦ 10
Anterior–posterior >20◦ 15
<5mm 10 Alignment
5–10mm 5 0–4◦ 0
>10mm 0 5–10◦ 3pt/1◦
Medial–lateral 11–15◦ 3pt/1◦
<5◦ 15 Others 20
6–9◦ 10
10–14◦ 5 Pointsdeducted
15◦ormore 0 Totalfinal
For this study, the patients were invited to come for a new clinical and functional assessment. The functional assessmentwasmadeinaccordancewiththeobjective cri-teriaestablishedbytheKneeSocietyClinicalRatingSystem (KSRS),14asshowninTable2.
Asestablishedintheassessmentsystem(KSRS),thefinal scoresrangedfrom0to100.Resultswithscoresgreaterthan 84wereconsideredtobeexcellent;from70to84,good;from60 to69,fair;andlessthan60,poor.Patientswhohadtoundergo revisionofthearthroplastywereconsideredtobetreatment failuresandreceivedthescoreofzero.
Statistical
analysis
Thedataobtainedweresubjectedtostatisticalevaluation.The chi-squaretestwas appliedforqualitativevariables,orthe
Table3–Surgicalcomplicationsandrespectivescores accordingtotheKneeSocietyClinicalRatingSystem (KSRS).
Surgicalcomplications Cases Score(KSRS)
Femoralcondylarfracture 1 0
Patellarfracture 3 83,80,68
Fibularneuropraxia 3 68,93,92
Reflexnervedystrophy 1 45
Dehiscenceofskinsuture 1 75
Infection 5 0,0,0,0,0
Asepticloosening 5 0,0,0,0,0
Fisherexacttestifnecessary.Toquantitativevariablesversus qualitativevariables,theMann–Whitneynonparametrictest wasused.TheStatisticalPackagefortheSocialSciences(SPSS) softwareversion13wasused,andthesignificancelevelwas setat5%.Theanalysiswasconductedunderguidancefrom statisticiansfromthe publicationsupportcommitteeofthe SchoolofMedicalSciences,SantaCasadeSãoPaulo.
Results
Out ofthe96patientsevaluatedinthepreviousstudy,13 69 attendedtheinvitation.Surgeryhadbeenperformed bilater-allyintenofthesepatients.Thus,79kneeswereevaluated, withameanfollow-upperiodof8yearsand8months.
Thearthroplastiesthatrequiredrevisionreceivedscores ofzero.Amongthepatientswhodidnotundergorevision,the minimumscorefoundwas40pointsandthemaximumwas 99.Themeanscorewas74.41points.
Amongtheothers,onewascomminutive(patellectomywas performed)andtheotherwasatransversefracturethatwas treated conservatively and evolved without consolidation and pain. Subsequently, this latter case was treated with partialpatellectomy. Three patients presentedneuropraxia of the fibular nerve. Two of them presented spontaneous recoveryandthethirdunderwentneurolysis2monthslater andevolvedwithtotalrecovery.Therewasalsoonecaseof dehiscenceofaskinsuture.Surgical cleaningand suturing wereperformed,andthecaseevolvedwithoutinfectionand withagoodclinicalresult.Fivecasesofinfectionoccurred,all ofthembeforereaching5yearsaftertheoperation.Onecase occurredafterarepairthatwasperformedontheextensor mechanism because of a fall to the ground that evolved withinfectionandlooseningoftheprosthesis.Inthiscase, the patientunderwent removalofthe prosthesisand then arthrodesisaftertheinfectionhadbeenresolved.Intheother four cases, revision of the arthroplasty was performed in twoprocedures,withuseofaspacer.Therewerefivecases ofaseptic loosening ofthe prosthesis,and revision ofthe arthroplastywasperformedinthesecases.
The KSRS results were distributed as excellent (KSRS greater than 84), in 55.7% of the cases (44 knees); good (between70and84),in22.8%(18knees);fair(between60and 69),in7.6%(sixknees);andpoor(lessthan60),in13.9%(11 knees).
Therelationship betweenthepresenceofcomplications andwhetherunilateralorbilateralarthroplastyhadbeen per-formed,andnostatisticallysignificantassociationwasfound (p=0.058;Fisherexacttest).
Therelationships between the patient’s sexand occur-rences ofcomplicationsand betweensexand resultswere alsoevaluated.Neitheroftheseshowedanystatistical differ-ence(p=1,Fisherexacttest;andp=0.610,Mann–Whitneytest, respectively).
The relationship between the etiology of the arthrosis and the presenceof complications was evaluated. Greater incidenceofcomplicationswasfoundincasesofsecondary arthrosis,andthiswasstatisticallysignificant(p=0.044;Fisher exacttest).Inevaluatingtherelationshipbetweentheresults andwhether theetiology wasprimary orsecondary, better results were observed in the group of patients with pri-maryosteoarthrosis,althoughwithoutstatisticalsignificance (p=0.210;Mann–Whitneytest).
Discussion
Prostheseswithmobiletibialweight-bearingemergedthrough thestudybyGoodfellowandO’Connorin1979.Theydefended theconceptthatthemobiletibialcomponent,actingsolidly withthefemoralcondyle,wouldrepresentacongruent pros-thesiswithoutrestrictionsatanymomentduringflexionand extension.1Subsequentstudiesshowedthatthisimplanthad highdurabilityand enabledmovementssimilar tothose of normalknees,withregardtokinematics,anditsindications expanded to include younger patients.1,15,16 Some studies have indicated that the survival of the implant is greater than20 yearsin97.7% ofthe cases.17,15 Nonetheless,other authorshavenotseenadvantagesofonemodelovertheother,
sincetheyfoundsimilarresultsregardingpatientsatisfaction and implant durability.Studies comparingbilateral arthro-plasties,inwhichonekneereceivedaprosthesiswithfixed weight-bearingandtheotherreceivedaprosthesiswithrotary weight-bearinghavebeenconducted,andnosignificant dif-ferenceswerefound.12,18,19
Regarding our sample, out of the original 162 patients, 96respondedtotheinvitationatthetimeofthefirst data-gathering made byour group (mean follow-up of5 years). Sixty-nineoftheserespondedtothepresentinvitation.This losswasgreaterthanthoseintheliteratureconsulted12,20and wasduetoavarietyoffactors,suchaschangesinaddressand telephonenumber,deathorsocioeconomicfactors.Itcanbe supposedthatpatientswithgoodresultsfromtheprocedure mighthaveneglectedtoreturnbecausetheyconsideredthisto beunimportant.Wealsonotedthatthelossfromthe follow-upwasvariableamongtheotherstudiesconsulted.Argenson etal.foundalossof7%fromtheirminimumfollow-upof10 yearsamongtheirpatients.20Ontheotherhand,inastudy withasimilarlengthoffollow-up,Meftahetal.11presenteda lossof23%amongtheirpatients.
Inourgroup’sfirstassessment,themeanfinalKSRSscore was78.22points.Incomparingthiswiththepresentresults (meanfinalscoreof74.41),weconsiderthatthisdecreasewas tobeexpected.Itwouldhavebeencausedbytheexpected wear on theimplant and the agingofthe patient sample. However,wedidnotfindanydataintheliterature compar-ingthesamegroupofpatientsovermediumandlong-term follow-ups.
Inrelationtocomplications,paralysisofthefibularnerve occurred inthreecasesthathadall presentedpreoperative valgusdeformity,andallofthempresentedtotalresolution. Thedataintheliteratureshowthatneuropraxiaofthefibular nerveismorecommoninkneeswithvalgusdeviation,given that atthetime ofcorrection ofthe axis,through section-ingcapsule,tendonandligamentstructures,tensionmaybe generatedinthenerveandconsequently,neuropraxia.21,22
Initially,thepatellarcomponentwasfixedtotheboneonly usingawidecircularorifice.Allofthethreecasesofpatellar fractureoccurredwithimplantsofthistype.Afterchanging theimplantsuchthattherewouldbethreesmallorifices,there werenofurtherpostoperativecasesofpatellarfracture.
Prostheseswithtibialweight-bearinghavebeenimplanted eitherwithpreservationorwithreplacementoftheposterior cruciateligament,withsimilarresults.Inourcases,the pos-teriorcruciateligamentwasreplacedwiththeaimofavoiding asymmetricaltensionandthepossibilityofrotarydislocation ofthe mobile platform (spin-out), whichneveroccurred in ourcases.Therewerefivecasesofasepticloosening(6.3%). Innoneofourcaseswasthereanypostoperative misalign-mentoftheaxisthatmighthaveacceleratedtheloosening process.Thesefivecasesunderwentrevisionoperationsand evolvedsatisfactorily.
etal.23identifiedthatsurgeryperformedinpublicservicesand lengthydurationofprocedures(>210min)wereriskfactorsfor prostheticinfections(inhiparthroplastyprocedures).
Inacaseseries withfollow-up ofgreater than 10years, Meftahetal.11foundthat96%oftheirresultsweregoodand excellent,withameanfunctionalKSRSscoreof89.1points. Argensonetal.20showedsimilarresults,withamean func-tionalKSRSscoreof88.Weconcludethatoursampleshowed alowermeanscorebecauseweincludedcasesthatunderwent revision,whichloweredthemeanscorebecausewegavethese casestheminimumscore.Inanalyzingourresultswith exclu-sionofthesecaseswithscoresofzero,weobtainedamean scoreof85pointsandconsiderablydiminishedthedifference encountered.Anotherresultthatshouldbenotedisthat78.5% ofthepatientsobtainedKSRSscores>70,i.e.goodorexcellent. Thelimitationsofthisstudyconsistofthelackofcontrol groupfor comparingthe resultsand the difficulty in com-paring patients for reevaluation after a long postoperative period.Thereisaneedfornewstudiesthatcompare func-tion,symptomsandsatisfactionamongpatientsundergoing totalkneearthroplastywithmobileandfixedweight-bearing, withfollow-upsofmorethan10years.
Conclusion
Thetotalkneeprostheseswithmobiletibialweight-bearing subjectedtoanalysisusingtheKneeSocietyClinicalRating Systemachievedgoodresultswithameanof74.41points.
Conflicts
of
interest
Theauthorsdeclarenoconflictsofinterest.
r
e
f
e
r
e
n
c
e
s
1. GoodfellowJW,O’ConnorJ.Themechanicsofthekneeand prosthesisdesign.JBoneJointSurgBr.1978;60(3):358–69. 2. BourneRB,WhitewoodCN.Theroleofrotatingplatformtotal
kneereplacements:designconsiderations,kinematics,and clinicalresults.JKneeSurg.2002;15(4):247–53.
3. DaniilidisK,HöllS,GoshegerG,DieckmannR,MartinelliN, OstermeierS,etal.Femoro-tibialkinematicsafterTKAin fixed-andmobile-bearingkneesinthesagittalplane.Knee SurgSportsTraumatolArthrosc.2013;21(10):2392–7.
4. LampeF,Sufi-SiavachA,BohlenKE,HilleE,DriesSP.Oneyear afternavigatedtotalkneereplacement,noclinicallyrelevant differencefoundbetweenfixedbearingandmobilebearing kneereplacementinadouble-blindrandomizedcontrolled trial.OpenOrthopJ.2011;5:201–8.
5. ZengY,CaoL,LiuY,PengGF,PengLB,YangDS,etal.Early clinicaloutcomesoffixed-bearingversusmobile-bearingtotal kneearthroplasty.ZhonguaYiXueZaZhi.2011;91(11):752–6. 6. LiuY,CaoL,LiG,ZengY,PengG,GongB.Comparisonof
anteriorkneepainbetweenfixed-bearingprosthesisand mobile-bearingprosthesisaftertotalkneearthroplasty. ZhongguoXiuFuChongJianWaiKeZaZhi.2011;25(3):266–71. 7. LädermannA,SaudanM,RiandN,FritschyD.Fixed-bearing
versusmobile-bearingtotalkneearthroplasty:aprospective
randomizedclinicalandradiologicalstudy.RevChirOrthop ReparatriceApparMot.2008;94(3):247–51.
8.BallST,SanchezHB,MahoneyOM,SchmalzriedTP.Fixed versusrotatingplatformtotalkneearthroplasty:a prospective,randomized,singleblindstudy.JArthroplasty. 2011;26(4):531–6.
9.LuringC,BathisH,OczipkaF,TrepteC,LufenH,PerlickL, etal.Two-yearfollow-uponjointstabilityandmuscular functioncomparingrotatingversusfixedbearingTKR.Knee SurgSportsTraumatolArthrosc.2006;14(7):605–11.
10.ColwellCWJr,ChenPC,D’LimaD.Extensormalalignment arisingfromfemoralcomponentmalrotationinknee arthroplasty:effectofrotating-bearing.ClinBiomech(Bristol, Avon).2011;26(1):52–7.
11.MeftahM,RanawatAS,RanawatCS.Ten-yearfollow-upof rotating-platform,posterior-stabilizedtotalknee
arthroplasty.JBoneJointSurgAm.2012;94(5):426–32. 12.KimYH,KimDY,KimJS.Simultaneousmobile-and
fixed-bearingtotalkneereplacementinthesamepatients.A prospectivecomparisonofmid-termoutcomesusinga similardesignofprosthesis.JBoneJointSurgBr. 2007;89(7):904–10.
13.GuglielmettiLGB,CoutoRC,CamargoOPA,SeverinoNR,Cury RPL,OliveiraVM,etal.Artroplastiatotaldojoelhocomo apoiotibialmóvel.Avaliac¸ãodosresultadosemmédioprazo [Totalkneearthroplastywithamobiletibial.Medium-term follow-upresults]].ActaOrtopBras.2010;18(6):
310–4.
14.InsallJN,DorrLD,ScottRD,ScottWN.RationaleoftheKnee Societyclinicalratingsystem.ClinOrthopRelatRes. 1989;(248):13–4.
15.McEwenHM,McNultyDE,AugerDD,FarrarR,LiaoYS,Stone MH,etal.Wear-analysisofmobilebearingknee.In: HamelynckKJ,StiehlJB,editors.LCSmobilebearingknee arthroplasty:a25yearsworldwidereview.Heidelberg: Springer-Verlag;2002.p.67–73.
16.McEwenHM,BarnettPI,BellCJ,FarrarR,AugerDD,StoneMH, etal.Theinfluenceofthedesign,materialsandkinematics ontheinvitrowearoftotalkneereplacements.JBiomech. 2005;38(2):357–65.
17.BuechelFFSr,BuechelFFJr,PappasMJ,D’AlessioJ. Twenty-yearevaluationofmeniscalbearingandrotating platformkneereplacements.ClinOrthopRelatRes. 2001;(388):41–50.
18.PriceAJ,ReesJL,BeardD,JuszczakE,CarterS,WhiteS,etal.A mobile-bearingtotalkneeprosthesiscomparedwitha fixed-bearingprosthesis.Amulticentresingle-blind randomisedcontrolledtrial.JBoneJointSurgBr. 2003;85(1):62–7.
19.ChiuKY,NgTP,TangWM,LamP.Bilateraltotalknee arthroplasty:onemobile-bearingandonefixed-bearing.J OrthopSurg(HongKong).2001;9(1):45–50.
20.ArgensonJN,ParratteS,AshourA,SaintmardB,AubaniacJM. Theoutcomeofrotating-platformtotalkneearthroplasty withcementatminimumoftenyearsoffollow-up.JBone JointSurgAm.2012;94(7):638–44.
21.DellonAL.Postarthroplasty“palsy”andsystemicneuropathy: aperipheral-nervemanagementalgorithm.AnnPlastSurg. 2005;55(6):638–42.
22.SchinskyMF,MacaulayW,ParksML,KiernanH,Nercessian OA.Nerveinjuryafterprimarytotalkneearthroplasty.J Arthroplasty.2001;16(8):1048–54.