ww w . r e u m a t o l o g i a . c o m . b r
REVISTA
BRASILEIRA
DE
REUMATOLOGIA
Original
article
Association
between
demyelinating
disease
and
autoimmune
rheumatic
disease
in
a
pediatric
population
夽
Ana
Luiza
M.
Amorim
a,∗,
Nadia
C.
Cabral
b,
Fabiane
M.
Osaku
a,
Claudio
A.
Len
a,
Enedina
M.L.
Oliveira
c,
Maria
Teresa
Terreri
aaUniversidadeFederaldeSãoPaulo(Unifesp),DepartamentodePediatria,SetordeReumatologiaPediátrica,SãoPaulo,SP,Brazil
bUniversidadeFederaldeSãoPaulo(Unifesp),SãoPaulo,SP,Brazil
cUniversidadeFederaldeSãoPaulo(Unifesp),DepartamentodeNeurologiaeNeurocirurgia,SetordeDoenc¸asDesmielinizantes,São
Paulo,SP,Brazil
a
r
t
i
c
l
e
i
n
f
o
Articlehistory:
Received7January2016 Accepted19August2016 Availableonline25October2016
Keywords:
Autoimmunediseases Rheumaticdiseases Demyelinatingdiseases Childhood
a
b
s
t
r
a
c
t
Introduction:Multiplesclerosis(MS)andneuromyelitisoptica(NMO)aredemyelinating dis-easesofthecentralnervoussystem.Autoimmunityinpatientswithdemyelinatingdisease andintheirfamilieshasbeenbroadlyinvestigatedanddiscussed.Recentstudiesshowa higherincidenceofrheumaticautoimmunediseasesamongadultpatientswithMSorNMO andtheirfamilies,buttherearenostudiesinthepediatricpopulation.
Objective:ToevaluateanassociationofMSandNMOwithautoimmunerheumaticdiseases inpediatricpatients.
Method:22patientsyoungerthan21yearsoldwithMSorNMOdiagnosedbeforetheageof 18yearswereevaluatedregardingepidemiologicaldata,clinicalpresentation,association withautoimmune diseases,familyhistoryofautoimmunediseases, laboratoryfindings, imagingstudiesandpresenceofauto-antibodies.
Results:Amongthepatientsstudied,therewasaprevalenceoffemales(68.1%).Themean ageofsymptomsonsetwas8yearsand9monthsandthemeancurrentagewas16years and4months.Twopatients(9%)hadahistoryofassociatedautoimmunerheumaticdisease: onecaseofjuveniledermatomyositisinapatientwithNMOandanotherofsystemiclupus erythematosusinapatientwithMS.Threepatients(13%)hadafamilyhistoryof autoim-munityinfirst-degreerelatives.Antinuclearantibodywasfoundpositivein80%ofpatients withNMOand52%ofpatientswithMS.About15%ofantinuclearantibody-positivepatients werediagnosedwithrheumatologicautoimmunediseases.
Conclusion:Amongpatientswithdemyelinatingdiseasesdiagnosedinchildhoodincluded inthisstudytherewasahighfrequencyofantinuclearantibodypositivitybutalower asso-ciationwithrheumatologicautoimmunediseasesthanthatobservedinstudiesconducted inadults.
©2016ElsevierEditoraLtda.ThisisanopenaccessarticleundertheCCBY-NC-ND license(http://creativecommons.org/licenses/by-nc-nd/4.0/).
夽
ThisisastudyconductedwiththejointcollaborationofthePediatricRheumatologyandDemyelinatingDiseasesdivisions, Universi-dadeFederaldeSãoPaulo,SãoPaulo,SP,Brazil.
∗ Correspondingauthor.
E-mails:amorim.analuiza@gmail.com(A.L.Amorim),teterreri@terra.com.br(M.T.Terreri).
http://dx.doi.org/10.1016/j.rbre.2016.09.016
2255-5021/©2016ElsevierEditoraLtda.ThisisanopenaccessarticleundertheCCBY-NC-NDlicense(http://creativecommons.org/
Associac¸ão
entre
doenc¸a
desmielinizante
e
doenc¸a
reumática
autoimune
em
uma
populac¸ão
pediátrica
Palavras-chave:
Doenc¸asautoimunes Doenc¸asreumáticas Doenc¸asdesmielinizantes Infância
r
e
s
u
m
o
Introduc¸ão: Esclerosemúltipla(EM)eneuromieliteóptica(NMO)sãodoenc¸as desmielin-izantes do sistema nervoso central. A autoimunidade entre pacientes com doenc¸as desmielinizanteseseusparentestemsidoamplamenteinvestigadaediscutida.Estudos recentesdemonstrammaiorincidênciadedoenc¸asreumáticasautoimunesentrepacientes adultoscomEMeNMOeseusparentes,masnãoháestudosnapopulac¸ãopediátrica.
Objetivo: Avaliara associac¸ãode EMeNMO comdoenc¸asreumáticasautoimunesem pacientespediátricos.
Método: Foramincluídos22pacientesmenoresde21anoscomdiagnósticodeEMouNMO antesdos18anoseavaliadosdadosepidemiológicos,clínicos,associac¸ãocomdoenc¸as autoimunes,históriafamiliardedoenc¸asautoimunes,exameslaboratoriais,exames de imagemepresenc¸adeautoanticorpos.
Resultados: Entreospacientesestudados,houveprevalênciadosexofeminino(68,1%).A médiadeidadedeiníciodossintomasfoideoitoanosenovemeseseamédiadeidadedos pacientesnaavaliac¸ãofoi16anosequatromeses.Doispacientes(9%)apresentaramdoenc¸a reumáticaautoimuneassociada,umcasodedermatomiositejuvenilempacientecomNMO eoutrodelúpuseritematososistêmicojuvenilempacientecomEM.Trêspacientes(13%) apresentaramhistóriafamiliardeautoimunidadeemparentesdeprimeirograu.Anticorpo antinuclear(ANA)positivofoiencontradoem80%dospacientescomNMOeem52%dos pacientescomEM.Cercade15%dospacientescomANApositivoapresentaramdiagnóstico definitivodedoenc¸aautoimunereumáticaassociada.
Conclusão: Entreos pacientescomdoenc¸as desmielinizantesdiagnosticadas durantea infânciaincluídosnestapesquisahouveumaaltafrequênciadeANApositivo,masuma menortaxadeassociac¸ãocomdoenc¸asreumáticasautoimunesdoqueaencontradaem trabalhosconduzidosemadultos.
©2016ElsevierEditoraLtda.Este ´eumartigoOpenAccesssobumalicenc¸aCC BY-NC-ND(http://creativecommons.org/licenses/by-nc-nd/4.0/).
Introduction
Thetermdemyelinatingdisorderreferstoagroupofdiseases thathaveincommonthelossofthemyelinsheath,witha relativeaxonalpreservation. Amongthevarious categories, wehighlightthoseofinflammatoryorigin,inparticular, mul-tiplesclerosis(MS),the mostdisablingneurologicaldisease in young adults, and neuromyelitis optica (NMO). Clinical and pathological aspects of these conditions lead one to believethat theseare inflammatoryautoimmune diseases, which leadto aprogressive deteriorationof multiplebody functions.1–4
MS may involve any part ofthe CNSat differenttimes ofits progression. Themost common early symptoms are paresisofoneormoremembers,pyramidalsigns(spasticity, hyperreflexia,Babinskisign,andclonus),ataxia, dysarthria, paresthesias,fecal or urinary incontinenceor retention,or sexualdysfunction.5
NMO,orDevicdisease,ischaracterizedbytheproduction ofantibodiesagainsttheblood–brainbarrier.Thefirst symp-tomsoccur betweenthe3rdand4th decadesoflife,inthe formofopticneuritisand/ormyelitiswithlongitudinal exten-sion.Opticneuritisismanifestedwithanacutebilateralloss ofvisualacuity,withpartialrecovery.Myelitisischaracterized bybilateralmotorsymptoms,withsignificantlossofstrength, sensorychangesandpartialrecoveryafteroutbreaks.6
Theautoimmunitythatsurroundspatientswith demyeli-nating disease and their family members has been widely investigatedanddiscussed.Recentstudiesshowthatpatients withMS and NMO,as wellastheir families, are atgreater riskofpresenting,atsomepoint,anassociateddiagnosisof anautoimmunerheumaticdisease.However,noneofthese studieswasdirectedtothepediatricpopulation.7,8
TheaimofthisstudywastoevaluatetheassociationofMS orNMOwithautoimmunerheumaticdiseasesinapediatric populationandtheirfirst-degreerelatives.
Patients
and
methods
In this retrospective cross-sectional study we included all patients withacurrentageup to21years,diagnosedwith MSaccordingtoMcDonaldcriteria,orwithNMOaccordingto the2006revisedcriteria,monitoredinDemyelinatingDisease UnitoftheDepartmentofNeurologyandNeurosurgery,and inthePediatricRheumatologyUnitoftheDepartmentof Pedi-atrics,Unifesp/EPM.Thediagnosisofjuvenilesystemiclupus erythematosus(JSLE)andjuveniledermatomyositis(JDM)was established in accordance with published criteria.6,9–11 All
patientswereundertheageof18atdiagnosisof demyelinat-ingdiseaseorautoimmunerheumaticdisease.
Table1–Demographiccharacteristicsofthestudy population.
MS NMO Total
n=17 n=5 n=22
Femalegender 10(58.8) 5(100) 15(68.2)
Currentage(months) 223 235 224
Ageattheonsetof symptoms(months)
150 120 132
Diseaseduration(months) 12 57 24
MS,multiplesclerosis;NMO,neuromyelitisoptica. Resultsareexpressedasn(%)andmedian(range).
symptoms, and disease duration; signs and symptoms of demyelinating disease, recurrence history, number of out-breaksandintervalsbetweentheseoutbreaks;autoimmune diseasesassociated;family history ofautoimmune disease; laboratorytestsandpresenceofantinuclearantibody(ANA), rheumatoid factor (RF), extractable nuclear antigen (ENA) antibodies, anti-aquaporin, anti-cardiolipin and anti-DNA; cerebrospinalfluid(CSF)analysis,andimagingtestssuchas brain magneticresonance imaging (MRI) l and MRI of the spinalcolumn.
The demographic and clinical characteristics were described in absolute and relative frequencies, median, andminimumandmaximumvalues,accordingtothenature ofthevariablesstudied.
Results
Twenty-twopatientswithadiagnosis ofdemyelinating dis-ease were selected: 17 patients with MS (77.3%) and five patientswithNMO(22.7%). Table1summarizes the demo-graphiccharacteristicsofthesepatients.
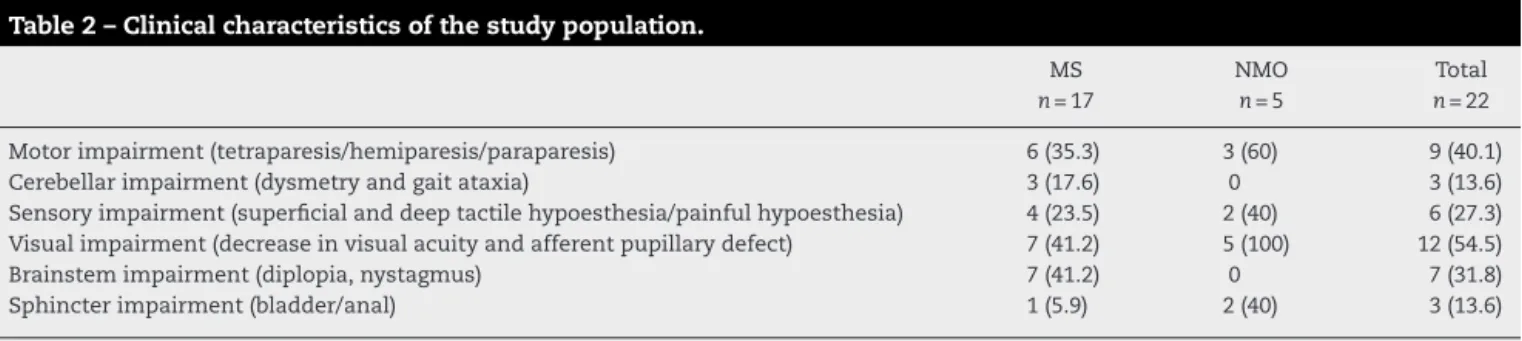
Thepredominant complaints of patients with MS were sight impairment (41%), brainstem impairment (41%), and pyramidalmotorimpairment (35%).All patients withNMO showedsightimpairmentatsomepointintheprogressionof thedisease.Otherfrequentcomplaintswerepyramidalmotor impairment(60%),sensoryimpairment(40%),andsphincter impairment(40%)(Table2).Table2describestheclinical char-acteristicsofpatientswithdemyelinatingdiseases.
FourteenpatientswithMShadrecurrenceswithan aver-ageof2.5outbreaksperpatient,withaminimumintervalof onemonthandamaximumintervalof108monthsbetween
outbreaks.AllpatientswithNMOhadahistoryofrecurrence, withameanofthreeoutbreaksperpatient,withaminimum intervaloftwomonthsandamaximumintervalof29months betweenoutbreaks.
Amongthepatientsincludedinthisstudy,onlytwo(9%) hadahistoryofassociationwithanautoimmunerheumatic disease.ThefirstpatienthadapreviousdiagnosisofMS,and aboutayearafterthefirstoutbreak,thispatientevolvedwith clinicalandlaboratoryfindingscompatiblewithJSLE.The sec-ondpatienthadadiagnosisofJDM,evolvingwithadiagnosis ofNMOabouttenyearsaftertheonsetofsymptomsofthe autoimmunedisease.
Onlythree(13%)patientshadafamilyhistoryof autoim-munityinfirst-degreerelatives.TwopatientswithMS(oneof themdiagnosedwithJSLEassociatedwiththedemyelinating disease)hadafamilyhistoryofsystemiclupus erythemato-sus.ApatientwithadiagnosisofNMOhadafamilyhistoryof rheumatoidarthritis.
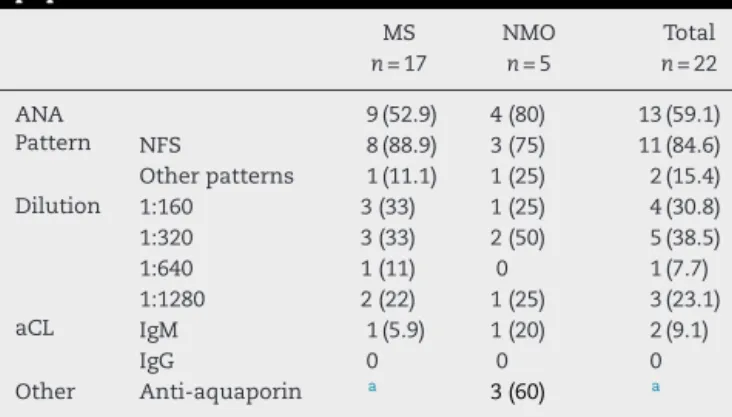
Among those patients with MS, nine (53%) were ANA-positivesubjects,includingthepatientwithJSLE.Therewas apredominanceofanuclearfinespeckledpattern(88%).The patientwithanassociateddiagnosisofJSLEalsotested pos-itive for IgManti-cardiolipin and anti-nucleosome. Among patientswithNMO,four(80%)hadapositiveANA,including thepatientwithJDM.Therewasapredominanceofanuclear fine speckledpattern(75%).Thepatientwithanassociated diagnosisofJDMwasalsopositiveforanti-cardiolipinIgM.On asubsequentexamination,theresultforthisantibodywas negative.Altogether,15%ofANA-positivepatientsshoweda conclusivediagnosisofautoimmunerheumaticdisease asso-ciatedwithademyelinatingdisease.
ThreeofthepatientsdiagnosedwithNMO(60%)were pos-itiveforanti-aquaporin.Table3summarizesthepresenceof autoantibodiesinthestudypopulation.
Noanti-ENAantibodies,anti-DNAantibodies,or rheuma-toidfactorwerefoundinthesepatients.Noneofthepatients inthisstudyhadanycytopenia(anemia,leukopenia, throm-bocytopenia),adecreaseincomplement,orkidneyfunction changes.
OnlypatientsdiagnosedwithMSweresubjectedtoa lum-bar puncture.Ofthese patients,six(35.3%)had oligoclonal bandsincerebrospinalfluid.
Four patients (23.5%) with MS were treated with glati-ramer, and nine (52.9%) patients received treatment with interferonbeta.Otherdrugsassociatedwereprednisone(5%) and immunoglobulin(5%).ThepatientdiagnosedwithJSLE
Table2–Clinicalcharacteristicsofthestudypopulation.
MS NMO Total
n=17 n=5 n=22
Motorimpairment(tetraparesis/hemiparesis/paraparesis) 6(35.3) 3(60) 9(40.1)
Cerebellarimpairment(dysmetryandgaitataxia) 3(17.6) 0 3(13.6)
Sensoryimpairment(superficialanddeeptactilehypoesthesia/painfulhypoesthesia) 4(23.5) 2(40) 6(27.3)
Visualimpairment(decreaseinvisualacuityandafferentpupillarydefect) 7(41.2) 5(100) 12(54.5)
Brainstemimpairment(diplopia,nystagmus) 7(41.2) 0 7(31.8)
Sphincterimpairment(bladder/anal) 1(5.9) 2(40) 3(13.6)
Table3–Presenceofautoantibodiesinthestudy population.
MS NMO Total
n=17 n=5 n=22
ANA 9(52.9) 4(80) 13(59.1)
Pattern NFS 8(88.9) 3(75) 11(84.6)
Otherpatterns 1(11.1) 1(25) 2(15.4)
Dilution 1:160 3(33) 1(25) 4(30.8)
1:320 3(33) 2(50) 5(38.5)
1:640 1(11) 0 1(7.7)
1:1280 2(22) 1(25) 3(23.1)
aCL IgM 1(5.9) 1(20) 2(9.1)
IgG 0 0 0
Other Anti-aquaporin a 3(60) a
MS,multiple sclerosis; NMO, neuromyelitisoptica; ANA, antin-uclearantibody; NFS, nuclear fine speckled pattern; aCL, anti-cardiolipin.Resultsareexpressedasn(%).
a Theanti-aquaporinantibodywasevaluatedonlyinpatientswith
adiagnosisofNMO.
wasalsotreatedwithacetylsalicylicacid,hydroxychloroquine, and azathioprine,aswell as withintravenous methylpred-nisoloneandcyclophosphamide.AllNMOpatientsreceived treatmentwithprednisoneandazathioprine,andonepatient wastreatedwithintravenousimmunoglobulin. Thepatient diagnosedwith anassociated JDMalso receivedtreatment withmethotrexate.
PatientsdiagnosedwithMS-JSLEandNMO-JDMhadseveral episodesofoutbreaksandremissionsthroughouttheir pro-gressionandcurrentlyareinremissionwithoutneurological sequelae.
Discussion
Differentstudieshaveshownanassociationbetween demyeli-natingdiseasesandotherautoimmunediseases.8Theresults
ofarecent systematicreviewpoint tosystemic lupus ery-thematosus(SLE)andrheumatoidarthritisastherheumatic autoimmunediseasesmostoftenassociatedwithMS.8
In2000,acase–controlstudycomparedMSpatients ver-suscontrolswithoutdemyelinatingdiseases,mostlyadults, regarding the occurrence of autoimmune diseases, which included autoimmune thyroiditis, autoimmune gastritis, Addison’sdisease,rheumatoidarthritis,pemphigusvulgaris, scleroderma,primary biliary cirrhosis, SLE,and ankylosing spondylitis.PatientswithMShadahigherprevalenceofthese conditions(20%)comparedtocontrolswithoutMS(13%)and theirfirst-degreerelatives(45%vs.27%,respectively).7In2006
acase–controlstudyfoundsimilarresultsthatfurtherpointed totheimportanceofHLA-DRgenesinthedeterminationof autoimmunityinvolvingMSpatientsandtheirfamilies.12
A study on patients (mostly adults) with NMO also showedthataboutone-third ofpatientshad adiagnosis of another autoimmune disease,suchas Sjogren’ssyndrome, primary sclerosing cholangitis, and immune thrombocy-topenicpurpura.13
On the other hand, a retrospective cohort showed no increasedriskofautoimmunerheumaticdiseasesinpatients
withMS(RR:0.9;CI:0.7–1.03),unliketheirrelatives,whowere atincreasedriskforsuchdiseases(RR:1.2;CI:1.1–1.4).14These
findingsmayberelatedtoapossiblebiasandtotheuseof differentdiagnosticcriteriaforthedifferentautoimmune dis-easesevaluated.14
Two patients (9%) with MS or NMO included in this study had autoimmune rheumaticdiseases: JSLE and JDM, respectively.AlthoughSLEhasbeendescribedinassociation withdemyelinatingdiseases,inourreviewoftheliterature we found only two publications relating these diseases to dermatomyositis.15,16 Thefirstreportreferstoamaleadult
witha previousdiagnosis ofMS that, aftertreatmentwith interferon beta-1a, cameto suffer the typical rash of der-matomyositis (Gottron’s papules and heliotrope rash) and proximal muscle weakness with a skin biopsy compatible with the diagnosis.15 The second publication consists ofa
seriesofcasesofpatientswithNMOwithitsonsetin child-hoodandadolescence,inwhichoneofthepatientshadan associateddiagnosis ofJDM.Inthispublication,neitherthe clinicalcoursenorthetreatmentreceivedbythispatientwas detailed;moreover,thefamilyhistoryofautoimmunediseases inpatientswithNMOhasnotbeenevaluated.16
TheneurologicmanifestationsofSLEpatientscanmimic thechangesfoundinpatientswithMSandNMO,especially inthoseperiodswhenthediseaseismoreactive.Transverse myelitis,forexample,althoughrare,hasbeendescribed sev-eraltimesasaneurologicalmanifestationofSLEpatients,with orwithoutopticneuritis.Inthesepatients,thedifferentiation betweenSLEactivity,orcoexistenceofMSorNMO,maybe complex.17
Szmyrka-Kaczmarek et al.describeintheir case–control study thehighestprevalenceofANAandanti-phospholipid antibodiesinpatientswithMS–without,however,any corre-lationwithsymptomssuggestiveofautoimmunerheumatic diseases or thromboembolic events.18 In the same study,
it was possible to correlate the autoantibodies to certain patterns ofclinicalpresentationofMS. Thus,ANA-positive patients, mainly with high titles, suffer from a disease of shorterduration,withlittleprogressiontodisability.Onthe otherhand,thepresenceofanti-2glycoproteinIwas asso-ciatedwithdiseasesofamoredraggedcourse,withgreater limitations.18
Intheirstudy,Hilarioetal.foundANApositivityin12.6%of healthychildrenandin36.2%ofchildrenwithseveral autoim-munerheumaticdiseases.19Studiesshowthatthepositivity
of ANA inMS patientscan vary from 20% to 60%; on the otherhand,inpatientswithNMOthispositivityapproaches 45%.18,20,21 ThepositivityofANAinpatientswith
demyeli-nating diseases included in this study was about 59%, of which15%(2patients)hadafinaldiagnosisofanassociated autoimmune rheumatic disease. It is suggested, therefore, thatpatientswithdemyelinatingdiseasesandwithANA posi-tivityreceiveamoredetailedcomplementaryinvestigationto excludethepossibilityofassociatedautoimmunedisorders.
Conflicts
of
interest
Theauthorsdeclarenoconflictsofinterest.
r
e
f
e
r
e
n
c
e
s
1. RejdakK,JacksonS,GiovannoniG.Multiplesclerosis:a
practicaloverviewforclinicians.BritMedBull.2010;95:79–104.
2. LoveS.Demyelinatingdiseases.JClinPathol.2006;59:1151–9.
3. PratE,MartinR.Theimmunopathogenesisofmultiple
sclerosis.JRehabilResDev.2002;39:187–99.
4. DeOliveiraEM,AnnesM,OliveiraAS,GabbaiAA.Multiple
sclerosis.Clinicalsurveyof50patientsfollowedatthe
AmbulatoryofNeurologyUnifesp-EPM.ArqNeuropsiquiatr.
1999;57:51–5.
5. LublinFD,ReingoldSC.Definingtheclinicalcourseof
multiplesclerosis:resultsofaninternationalsurvey.National
MultipleSclerosisSociety(USA)AdvisoryCommitteeon
ClinicalTrialsofNewAgentsinMultipleSclerosis.Neurology.
1996;46:907–11.
6. WingerchukDM.Neuromyelitisoptica.IntMSJ.2006;13:42–50.
7. HendersonRD,BainCJ,PenderMP.Theoccurrenceof
autoimmunediseasesinpatientswithmultiplesclerosisand
theirfamilies.JClinNeurosci.2000;7:434–7.
8. MarrieRA,ReiderN,CohenJ,StuveO,SorensenPS,CutterG,
etal.Asystematicreviewoftheincidenceandprevalenceof
autoimmunediseaseinmultiplesclerosis.MultSclerJ.
2014;21:282–93.
9. McDonaldWI,CompstonA,EdanG,GoodkinD,HartungHP,
LublinFD,etal.Recommendeddiagnosticcriteriaformultiple
sclerosis:guidelinesfromtheInternationalPanelonthe
DiagnosisofMultipleSclerosis.AnnNeurol.2001;50:121–7.
10.HochbergMC.UpdatingtheAmericanCollegeof
Rheumatology.ArthritisRheum.1997;40:1725.
11.BohanA,PeterJ.Polymyositisanddermatomyositis(firstof
twoparts).NEnglJMed.1975;292:344–7.
12.LaroniA,CalabreseM,PeriniP,AlbergoniMP,RanzatoF,
TiberioM,etal.Multiplesclerosisandautoimmunediseases:
epidemiologyandHLA-DRassociationinNorth-eastItaly.J
Neurol.2006;253:636–9.
13.WingerchukDM,HogancampWF,O’BrienPC,Weinshenker
BG.Theclinicalcourseofneuromyelitisoptica(Devic’s
syndrome).Neurology.1999;53:1107–14.
14.NielsenNM,FrischM,RostgaardK,WohlfahrtJ,HjalgrimH,
Koch-HenriksenN,etal.Autoimmunediseasesinpatients
withmultiplesclerosisandtheirfirst-degreerelatives:a
nationwidecohortstudyinDenmark.MultScler.
2008;14:823–9.
15.SomaniAK,SwickAR,CooperKD,McCormickTS.Severe
dermatomyositistriggeredbyinterferonbeta-1atherapyand
associatedwithenhancedtypeIinterferonsignaling.Arch
Dermatol.2008;144:1341–9.
16.FragosoYD,FerreiraMLB,OliveiraEML,DominguesRB,
RibeiroTAGJ,BrooksJBB,etal.Neuromyelitisopticawith
onsetinchildhoodandadolescence.PediatrNeurol.
2014;50:66–8.
17.Tellez-ZentenoJF,Remes-TrocheJM,Negrete-PulidoRO,
Davila-MaldonadoL.Longitudinalmyelitisassociatedwith
systemiclupuserythematosus:clinicalfeaturesand
magneticresonanceimagingofsixcases.Lupus.
2001;10:851–6.
18.Szmyrka-KaczmarekM,Pokryszko-DraganA,PawlikB,
GruszkaE,KormanL,PodemskiR,etal.Antinuclearand
antiphospholipidantibodiesinpatientswithmultiple
sclerosis.Lupus.2012;21:412–20.
19.HilárioMOE,LenCA,RojaSC,TerreriMT,AlmeidaG,Andrade
LEC.Frequencyofantinuclearantibodiesinhealthychildren
andadolescents.ClinPediatr(Phila).2004;43:637–42.
20.CollardRC,KoehlerRP,MattsonDH.Frequencyand
significanceofantinuclearantibodiesinmultiplesclerosis.
Neurology.1997;49:857–61.
21.WuL,HuangD,YangY,WuW.Combinedscreeningforserum
anti-nuclearandanti-aquaporin-4antibodiesimproves
diagnosticaccuracyfordistinguishingneuromyelitisoptica