w w w . r b o . o r g . b r
Update
Article
Turco’s
injury:
diagnosis
and
treatment
夽
,
夽夽
Ana
Paula
Simões
da
Silva
∗,
Leandro
Girardi
Shimba,
Luiz
Henrique
Boraschi
Vieira
Ribas,
Alexandre
Simmonds
de
Almeida,
Vinicius
Naves,
Aires
Duarte
Júnior
FaculdadedeCiênciasMédicasdaSantaCasadeSãoPaulo,PavilhãoFernandinhoSimonsen,SãoPaulo,SP,Brazil
a
r
t
i
c
l
e
i
n
f
o
Articlehistory:
Received2May2013
Accepted16July2013
Availableonline14May2014
Keywords:
Tarsaljoints/injuries
Metatarsalbones
Bonefractures
Dislocations
a
b
s
t
r
a
c
t
TheaimofthisstudywastoalertdoctorstotheexistenceofTurco’sinjuryanddiscusthe
existingtreatmentsthathavebeendescribedintheworldwideliterature.Abibliographic
surveyofLisfranc’sinjuryandTurco’sinjurycoveringfrom1985to2013wasconductedin
theSciELOandPubMeddatabases.Amongthe193articles,thoserelatingtobone-ligament
injuriesoftheLisfrancjointandhigh-energytraumawereexcluded,aswerethecasereports.
Thepatientsselectedwereprofessionaloramateurathleteswhosolelypresentedaligament
injurytotheLisfrancjoint(Turco’sinjury),whichwasdiagnosedfromthehistory,physical
examination,radiographsandmagneticresonanceimages.Non-athleticpatientsandthose
withassociatedboneinjurieswereexcluded(10).Accordingtotheinjuryclassification,the
patientsweretreatedbymeansofeitheranopenoraclosedprocedureandthenastandard
rehabilitationprotocol.Outofthe10patients,fiveunderwentconservativetreatmentand
fiveunderwentsurgicaltreatmentusingdifferenttechniquesandsynthesismaterials.We
obtainedtwopoorresults,onesatisfactory,fivegoodandtwoexcellent.Weconcludethat
thecorrectdiagnosishasadirectinfluenceonthetreatmentandonthefinalresultobtained,
andthatlackofknowledgeofthisinjuryisthemainfactorresponsibleforunderdiagnosing
Turco’sinjury.Thereisaneedforrandomizedprospectivestudiescomparingthetypesof
synthesisandevolutionoftreatedcases,inordertodefinethebesttreatmentforthisinjury.
©2014SociedadeBrasileiradeOrtopediaeTraumatologia.PublishedbyElsevierEditora
Ltda.Allrightsreserved.
Lesão
de
Turco:
diagnóstico
e
tratamento
Palavras-chave:
Articulac¸õestarsianas/lesões
Ossosdometatarso
Fraturasósseas
Luxac¸ões
r
e
s
u
m
o
EstetrabalhotemporobjetivosalertarosmédicossobreaexistênciadalesãodeTurcoe
discorrersobreostratamentosexistentesdescritosnaliteraturamundial.Foifeito
levan-tamentobibliográficodalesãodeLisfrancedalesãodeTurcode1985a2013nasbases
dedadosScieloePubmed.Dos193artigos,foramexcluídososcomlesão
osteoligamen-tardaarticulac¸ãodeLisfranc,osportraumasdealtaenergia,osrelatosdecaso.Foram
夽Pleasecitethisarticleas:daSilvaAPS,ShimbaLG,RibasLHBV,deAlmeidaAS,NavesV,DuarteJúniorA.Turco’sinjury:diagnosisand
treatment.RevBrasOrtop.2014;49:321–327.
夽夽
WorkperformedintheSportsTraumatologyGroup,DepartmentofOrthopedicsandTraumatology,SchoolofMedicalSciences,Santa
CasadeSãoPaulo,FernandinhoSimonsenWing.
∗ Correspondingauthor.
E-mail:apaulass@gmail.com(A.P.S.daSilva).
2255-4971/$–seefrontmatter©2014SociedadeBrasileiradeOrtopediaeTraumatologia.PublishedbyElsevierEditoraLtda.Allrightsreserved.
selecionadospacientesatletasprofissionaisouamadores,comlesãoligamentarexclusiva
daarticulac¸ãodeLisfranc(lesãodeTurco),aqualfoidiagnosticadapelahistória,peloexame
físico,pelasradiografiasepelaressonânciamagnética.Comofatoresdeexclusão,pacientes
nãoatletasecomlesõesósseasassociadas(10).Deacordocomaclassificac¸ãodalesão,os
pacientesforamtratadoscruentaouincruentamenteesubmetidosaumprotocolo-padrão
dereabilitac¸ão.Dos10pacientes,cincoforamsubmetidosatratamentoconservadorecinco
atratamentocirúrgico,pordiferentestécnicasemateriaisdesíntese.Obtiveram-sedois
resultadosruins,umsatisfatório,cincobonsedoisexcelentes.Concluímosqueo
diag-nósticocorretoinfluenciadiretamentenotratamentoenoresultadofinalobtidoequeo
desconhecimentodalesãoéoprincipalresponsávelpelosubdiagnósticodalesãodeTurco.
Hánecessidadedeestudosprospectivosrandomizadosquecomparemostiposdesíntese
eaevoluc¸ãodoscasostratadosparaumadefinic¸ãodomelhortratamentoparatallesão.
©2014SociedadeBrasileiradeOrtopediaeTraumatologia.PublicadoporElsevier
EditoraLtda.Todososdireitosreservados.
Introduction
TheLisfrancortarsometatarsaljointisthusnamedinhomage
totheFrenchphysicianJacquesLisfranc,who wasthefirst
todescribeanamputation throughthis joint.1–4 This
com-plexis formedbybone elements (base ofthe metatarsals,
cuneiformsandcuboid)andligamentsthatgivestructureand
supporttothetransverse archofthemidfoot.Betweenthe
medialcuneiformandthesecondmetatarsal,thereisastrong
obliqueligamentcalledtheLisfrancligament.This,in
asso-ciation with the effect of the most proximalfitting ofthe
secondmetatarsal,formsthemainstabilizerofthisjoint.1,3,5–8
Thecomplexanatomyofbonesandligamentsinthisregion,
inassociationwiththemultipleinjurypatterns and
mech-anisms,makesradiographic interpretation and diagnosis a
challenge,particularlyinattendingemergencycases.9
Dislocated fractures of the Lisfranc joint are unusual
injuries of the foot and occur at a rate of 1:55,000 to
60,000 per year, which corresponds to 0.1% to 0.9% of all
fractures.Approximatelyonethirdoftheseinjuriesgo
undi-agnosed,whichmayleadtochronicpaininthefootaffected,
osteoarthrosis and deformities.1,3,10–13 Among the various
injurymechanismsthathavebeendescribed,thecommonest
isplantarflexion over the metatarsals,inassociation with
rotationalstress.9Inthismanner,itisimportantfor
physi-cianstobecomefamiliar withthe typesofpresentationof
Lisfranc dislocated fractures, and specifically the one
dis-cussedinthisstudy,whichbearsthenameofTurco’sinjury,
giventhatearlydiagnosisandinterventionareessentialfor
betterprognosis.14,15 Turco’sinjuryisoneinwhichthereis
alow-energytraumamechanismthatonlycausesligament
tears,withorwithoutdislocationofthisjoint,anditoccurs
especiallyamongathletes.9
Thisinjuryisthereforecharacterizedbyanopeningofup
to5mmintheintermetatarsalspaceofthefirstandsecond
metatarsals,and itmay range inseverity, accordingtothe
classificationofNunleyandVertullo,fromstageItoIV.16
Anatomyandbiomechanics
Understandingtheanatomyofthetarsometatarsalcomplex
isessential forit tobe possible toevaluate, diagnose and
treatinjuries tothis joint.Thestability of this complex is
achieved through bone architecture and ligament support.
The first,second and thirdmetatarsals articulate with the
medial,intermediateandlateralcuneiforms,inthisorder,and
the fourthandfifthmetatarsals articulatewiththecuboid.
The second metatarsal notonlylies between the first and
third metatarsals, but also has a greater contact surface
withthebonesthatsurroundit,giventhattheintermediate
cuneiformislocatedmoreproximallythanthemedialand
lat-eralcuneiforms.Thus,ithasalock-and-boltfitthatincreases
thestability.17,18
Inadditiontothestructuredboneframework,thereisa
ligament support. Thebones ofthe metatarsus are joined
togetherbymeansofthedorsalandplantarintermetatarsal
ligaments, asare alsothe cuneiforms and the cuboid, but
thereisnoligamentthatjoinsthebaseofthefirstmetatarsal
to the second metatarsal. There is also a variable
net-work of longitudinal and oblique ligaments that secures
the last four metatarsals tothe cuneiformsand cuboid on
the plantar and dorsal sides, along with two longitudinal
ligaments that anchor the first metatarsal in the medial
cuneiform.17,18
Thelargestandstrongestligamentofthetarsometatarsal
complex isthe so-calledLisfranc ligament. Itsorigin isin
thelateralsurfaceofthemedialcuneiformanditisinserted
intothemedialfaceofthebaseofthesecondmetatarsal17,18
(Fig.1).
Physiopathology
Lisfrancinjuriescanbecausedbydirectorindirect
mecha-nisms.Direct traumatothe dorsumofthefootisrare and
maybecomplicatedthroughcontamination,vascular
impair-mentandcompartmentalsyndrome.Injuriesthroughindirect
mechanismsareresponsibleformostcasesandresultboth
fromrotationalforcesappliedtotheforefootwiththe
hind-foot fixed and from axial loads on a fixed foot in plantar
flexion.14
Thecommonestcause ofindirect traumathat hasbeen
described inthe literature iscar accidents, which account
forapproximately40%to45%oftheinjuries.17Othercauses
thathavebeendescribedincludeactsoffallingfromaheight,
accidentswithhorses,motorcycleaccidentsand injuriesin
Fig.1–Representationoftheboneanatomyofthemidfoot andhindfoot,inwhich“lock-and-bolt”fittingofthesecond metatarsalwiththecuneiformswasobserved.TheLisfranc ligamentishighlightedandthemetatarsals(ItoV)are identified.
Diagnosis
Well-conductedclinical history-taking and physical
exami-nationarefundamentalforthediagnosis.Patientsgenerally
reveal the trauma mechanism and report having pain in
themidfoot,varyinggreatlyinintensity.Theyaregenerally
asymptomaticwhenwalking,butpresentpainwhenrunning,
jumpingandmakingothersportsmovements.Itisimportant
tolocate thepainfulpoints.Painonpalpationbetweenthe
baseofthefirstandthesecond metatarsalisanimportant
finding,evenwithoutinjuriesinvolvingdiastasisofthe
inter-metatarsal space.12,15–17 Provocative testsmay alsobevery
helpful.Thetwotestsmostfrequentlyusedarelateral
com-pressiontestandtheaxialstabilitytestbetweenthefirstand
secondmetatarsals,whicharepositivewhentheyreproduce
paininthemidfoot.Shapiroetal.19concludedthatthesetwo
testsarepositivewhenthereisruptureoftheLisfranc
liga-ment.Thereisalsoaspecifictestfortarsometatarsalinjuries,
which consistsofpassive pronation withabduction ofthe
forefoot,with the hindfoot fixed. Thismaneuver produces
painatthesiteoftheinjuredligament.
Well-producedradiographsare alsofundamentalforthe
diagnosis. Anteroposterior (AP), lateral (L) and oblique (O)
viewsshouldbeproduced,withloadingifpossible.A
compar-isonwithradiographsonthecontralateralfootmaybeuseful
fordetectingsubtleinjuries.IntheAPview,themedialfaceof
theintermediatecuneiformshouldbealignedwiththemedial
faceofthesecondmetatarsal.Intheobliqueview,the
parame-terfornormalityisthemedialfaceofthecuboid,whichshould
bealignedwiththemedialfaceofthefourthmetatarsal.In
profileview,thepresenceofanteriororposteriordislocation
orsubluxationofthetarsometatarsaljointscanbeobserved.
Ifthereisanydoubt,APandlateral-viewradiographscanalso
beobtainedwithloading,whichmayhelptoshowdiastasis
betweenthefirstandsecondmetatarsalsinAPview.Inlateral
viewwithloading,adroppedplantararchordorsal
subluxa-tioncanbeseen.11,12,14–17
Classification
TheclassificationusedforTurco’sinjuryistheoneproposed
byNunleyandVertullo,whichisspecificformidfootinjuries
inathletes.Thisclassificationdividestheinjuriesintothree
stages.InsprainstageIoftheLisfrancligament,thereisno
diastasisorlossoftheplantararch.InsprainstageII,there
isadiastasisof2mmto5mmduetofailureoftheLisfranc
ligament,butthereisnolossoftheplantararch.InstageIII,
thereisadiastasisbetweenthefirstandsecondmetatarsals
andlossoftheplantararch16(Fig.2).
Materials
and
methods
ScientificarticlesthatspecificallydiscussedLisfranc’sinjury
andTurco’sinjurybetween1985and2012weresurveyedinthe
ScieloandPubmeddatabases,usingthefollowingdescriptors:
“Lisfrancjoint”,“tarsometatarsaljoint”,“injuries”,“fracture”,
“dislocation”,“treatment”and“outcome”.Onehundredand
ninety-threearticleswerefound,andarticlesdescribingthe
followingwereexcluded: boneandligamentinjuriesofthe
Lisfrancjoint;injuriesduetohigh-energytrauma;andcase
reports.Theinformationwascomparedwithcasessurveyed
inatypicalteachinghospitalinalargecitybetween2006and
2011regardingthetreatmentused,follow-up,postoperative
evaluationandreturntopre-injuryactivities.Thedatawere
organizedaccordingtosportsactivity,age,sideaffected,
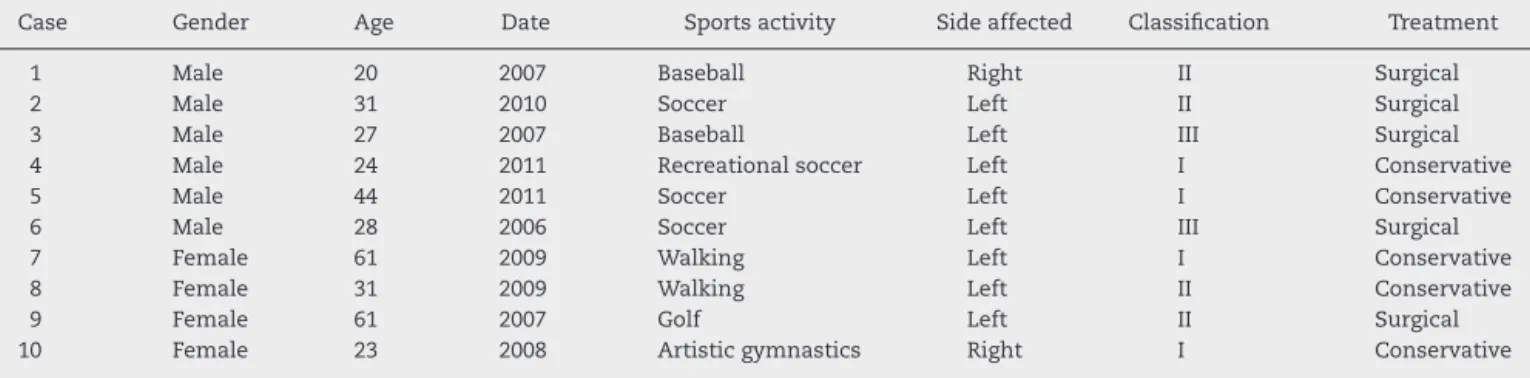
clas-sification,treatmentandfollow-up(Table1).
Thepatientsselectedforinclusioninthisstudywere
pro-fessionaloramateurathleteswithligamentinjuriessolelyin
theLisfrancjoint(Turco’sinjury),whichwerediagnosedfrom
thehistory,physicalexamination,radiographsandmagnetic
resonanceimaging.Patientswhowerenotathletesandwho
presentedassociatedbonelesionswereexcluded.Agroupof
10patientswasthusformed:sixmen(60%)andfourwomen
(40%),withameanageof35years(20to61).Theleftsidewas
affectedineightcases(80%)andtherightsideintwocases
(20%).TheassessmentsusingtheclassificationofNunleyand
Vertullo16were:fourcasesoftypeI(40%),fouroftypeII(40%)
andtwooftypeIII(20%).Themeanfollow-upwas44.9months
Lisfranc ligament sprain
No diastasis
Ruptured lisfranc ligament 2-5mm
diastasis
Diastasis & loss of longitudinal arch
height
Stage I Stage II
Stage III
Diastasis, no arch height loss
2-5mm diastasis Ruptured lisfranc
ligament
Fig.2–NunleyandVertulloclassification.16
Table1–Distributionof10patientswithTurco’sinjury,organizedaccordingtogender,sportsactivity,sideaffected, classification16andtreatment.
Case Gender Age Date Sportsactivity Sideaffected Classification Treatment
1 Male 20 2007 Baseball Right II Surgical
2 Male 31 2010 Soccer Left II Surgical
3 Male 27 2007 Baseball Left III Surgical
4 Male 24 2011 Recreationalsoccer Left I Conservative
5 Male 44 2011 Soccer Left I Conservative
6 Male 28 2006 Soccer Left III Surgical
7 Female 61 2009 Walking Left I Conservative
8 Female 31 2009 Walking Left II Conservative
9 Female 61 2007 Golf Left II Surgical
10 Female 23 2008 Artisticgymnastics Right I Conservative
The patients were treated conservatively or surgically, accordingtotheclassificationoftheinjury.
All the patients underwent our group’s standard reha-bilitation protocol,whichconsisted offourto sixweeksof immobilizationusingabrace,withoutloading,withanalgesic physiotherapyandtrainingofsportsmovements.
Toanalyzetheresults,weusedsubjectiveassessmentthat tookintoaccountpainandsportspracticeperformance,which was considered to be poor, satisfactory, good or excellent. Theresults were considered tobe poor if the patient pre-sented painand didnotreturn tothe sport;satisfactoryif thepatientcontinuedtopresentpainbutreturnedtosports practicebelowthepre-injuryperformancelevel;goodifthe patientpresentedpain butreturned tosports practiceata levelsimilartobeforetheinjury;andexcellentifthepatient didnotpresentpainandreturnedtothesportatthesame levelasbeforetheinjury.
Atthefollow-upassessments,radiographswereproduced inanteroposterior,lateralandobliqueviews,withloading,in ordertoevaluatetheevolution.
Result
After careful individualized analysis on each medical file (each patient), the cases were stratified based on the type oftreatment,postoperativecomplications,results,lengthof follow-upandradiographicsignsofarthrosis.
The patients with type I injuries (4, 5, 7 and 10) were treatedconservativelyinaccordancewithourstandard pro-tocol:patients5and7evolvedwithgoodresultsandpatients 4and10withexcellentresults.
Table2–Distributionof10patientswithTurco’sinjury,accordingtothetypeoftreatment,rehabilitation,complications presentedandreturntosportsactivity.
Case Typeoftreatment Postoperativecomplications Result Follow-up(months) Arthrosis
1 ORIFwith2parallelSFS Superficialskininfection anddehiscenceofsuture
Good 61months No
2 ORIFwith1obliqueSFS Superficialskininfection andnon-anatomical reduction
Poor 34months Yes
3 ORIFwith2divergentSFS and1Kirschnerwire
Absent Good 59months No
4 Conservative Absent Excellent 18months No
5 Conservative Absent Good 17months No
6 ORIFwith2parallelSFS Absent Satisfactory 76months Yes
7 Conservative Absent Good 36months Yes
8 Conservative Absent Poor 37months No
9 ORIFwith2parallelSFS Absent Good 60months Yes
10 Conservative Absent Excellent 51months No
ORIF,openreductionandinternalfixation;SFS,small-fragmentscrews(3.5mm).
openreductionandinternalfixation(ORIF),usingtwoparallel small-fragmentscrews(3.5mm),whichinonecasewentfrom themedialcuneiformtothebaseofthesecondmetatarsaland intheothercasefromthemedialcuneiformtothe intermedi-atecuneiform.Duringthefollow-up,bothofthempresented goodresults,althoughpatient1evolvedwithdehiscenceof thesutureandsuperficial skininfection,without arthrosis, whilepatient9hadnocomplicationsoftheoperativewound but showed radiographic signs of arthrosis. Patient 2 was treated with ORIF, using an oblique small-fragment screw goingfromthemedialcuneiformtothebaseofthesecond metatarsal.Thispatientevolvedwithsuperficialskin infec-tion duringthe postoperative periodand presenteda poor resultduringthefollow-up,whichweattributedtothe non-anatomicalreduction obtainedinthe surgery. Thispatient evolvedwitharthrosis.Patient8,whoalsohadatypeIIinjury, wastreatedinaclosedmanner,becauseoflatediagnosisand radiographicevidenceofmidfootankylosis,andpresenteda poorresult.
Thepatients with typeIII injuries (3 and 6) underwent surgicaltreatment.Patient3underwentORIFusingtwo diver-gentsmall-fragment spongy screwswith partialthreading: onefrom the medialcuneiform tothe base ofthe second metatarsalandtheotherfromthemedialcuneiformtothe intermediatecuneiform,inassociationwithaKirschnerwire fromthesecond metatarsaltotheintermediatecuneiform. During the evolution, this patientpresented agood result, without arthrosis. This patient underwent removal of the Kirschnerwireaftersixweeks.Patient6wastreatedwithORIF usingparallelscrews,withsatisfactoryevolutionandarthrosis (Table2).
Discussion
Accordingtotheliterature,morethan20%ofdislocated
Lis-francfracturesarenotdiagnosedintheinitialevaluation,3,4
whichmakessuspicionandearlydiagnosisprerequisitesfor
correctmanagementofthisinjury.Toavoidsequelaeoverthe
longterm,andfunctionalimpotenceofthisjoint,the
consen-susisthatanatomicalreductionandjointstabilizationshould
beperformed,sothatthefollow-upwillbesatisfactoryand
therecoveryadequate.20–24 Lisfrancinjuriesgenerallyresult
fromhigh-energytrauma.3Caraccidentsarethemaincause
oftheseinjuries.Inoursample,thecommonesttrauma
mech-anismwaslow-energy.Theprincipalduringsportspracticeis
plantarflexionoverthemetatarsals,inassociationwith
rota-tionalstress,inaccordancewithwhatwasdescribedinTurco’s
originalarticle.15
Thediagnosisisobtainedthroughdetailedphysical
exami-nation,whichshowsuppatientsforwhomitisdifficultoreven
impossibletobearweightontheaffectedlimb,withpainon
palpationintheregionofthejointbetweenthefirstand
sec-ondmetatarsals,andpossiblyalsoedemaandlocalsweating.
Itisveryimportanttoperformradiographswithloadingon
theaffectedfoot,inthefrontal,lateralandobliquepositions.
Incasesofdoubt,magneticresonanceimagingisindicatedfor
thediagnosis.
TheclassificationdescribedbyNunleyandVertullo16was
used to interpret and classify the injuries, and this also
guided the treatment.There is noconsensusin the
litera-tureregardingthetreatment:openorclosedreductionusing
wiresorscrews;thepositioningofthescrews;andwhether
arthrodesisisindicated.Inoursample,noneofthepatients
underwent arthrodesis.Arthrodesis isa predictable
conse-quenceofinjuriesthatare notadequatelyreduced,withor
without associatedfailureofthesynthesis,orundiagnosed
injuries that evolve with symptomatic arthrosis. However,
therewasonecase(patient8)forwhomthediagnosiswasnot
madeattheinitialattendance,whichwasatanotherservice.
Thispatientwas admittedtoourservicewithtwomonths
ofevolution ofthe injury, and conservative treatment was
chosen.Thepatientevolvedwitharthrosisandankylosis,but
withoutsymptomsthatwouldjustifyarthrodesis.
Aspublishedinrecentstudies,anatomicalreductionand
internalfixationaretheessentialfactorsforagood
therapeu-ticresultsincasesofinjuriesclassifiedastypesIIandIIIby
NunleyandVertullo.Thisisconcordantwithourresults,as
showninpatient2,inwhomanatomicalreductionwasnot
achieved, withconsequent evolutionto apoorresult.7,25–31
ConservativetreatmentwasonlyindicatedforgradeIinjuries,
ofthesofttissues,andalsobecauseofthetendencytoward
initialdisplacement.22
Grade II and III injuries can be dealt with using
sev-eral techniques and approaches, which vary according to
thesurgeon’sexperienceandpreference.Thesemayinclude
closed reductionand percutaneous fixation using wiresor
screws,32 open reductionand internal fixation using these
samematerials17,20,24,33andevenprimaryarthrodesis.30
In 2003, Perugia et al.34 treated this type of injury by
meansofclosedreductionandinternalfixationusing
percu-taneous4mmspongyscrews,in42patients:12withpurely
ligament injuries and 30 with bone and ligament injuries,
with follow-up of close to 58 months. The results were
evaluatedusingtheAOFASmidfootfunctionalscorewitha
meanof81points.Intheirstudy,thetreatmentsandresults
obtainedwere notdifferentiated betweenthe patientswith
solelyligamentinjuries(Turco’sinjury)andthosewith
bone-ligamentinjuries(Lisfrancfracture-dislocation).Furthermore,
the authors did not give any informationregarding
evolu-tionoftheircasestoarthrosis,thereturntoworkorresidual
pain.
Perezetal.,24Rammeltetal.25andTanetal.26usedopen
reductionand internalfixationwithKirschnerwires(2.5 to
3.5mm), through one or two access routes. In their study,
amongallthecomplicationspossible(infection,lossof
reduc-tion or skin necrosis),Perez et al.24 presentedonecase of
infectionandthreewithskinnecrosis,withafollow-upof76
months.Rammeltetal.25showedonecasewithskin
necro-sisandonewithinfection.Overa36-monthfollow-up,Tan
etal.26found10casesofarthrosisofthetarsometatarsaljoint,
butall thesepatientsreturned towork.Elevenout oftheir
12patientspresentedcompleteorpartialpainrelief.Noneof
theseauthorsreportedanylossofreductionoverthecourse
oftheirpatients’follow-ups,andthesynthesismaterialswere
removedeightweeksaftertheoperation.Wehadonecasein
whichmixedsynthesiswasused(screwandwire),inwhich
thewirewasremovedsixweeksaftertheoperation.There
werenocomplicationsandweobtainedagoodresult.
Thegreatmajorityoftheauthors7,25,27–30,33,34 usedopen
reductionandinternalfixationusingsmall-fragmentscrews.
OnlyMulieretal.31performedtreatmentswithlarge-fragment
screws(4.5mm).Intheirstudy,conductedon16patientswith
30monthsoffollow-up,thesynthesismaterialwasremoved
after12 weeks,afterevidenceofboneconsolidationand/or
ligamenthealingwasseen.Theresultsthattheypresented
included:twopatientswithsympathetic-reflexdystrophy,15
withevolutiontoearlyarthrosisofthisjointandtwocases
that,becauseoftheseverityoftheinjury,underwentprimary
arthrodesis.Inagreementwiththeliterature,weusedORIF
withsmall-fragmentscrews.
Among the studies in which the patients with
bone-ligament injuries to the Lisfranc joint underwent open
reductionandinternalfixationusingtwoscrews,Arntzetal.7
hadthefollowingresultsamong34patients:20evolvedwith
arthrosis,without the need forarthrodesis, 21 returned to
workand29hadcompleteorpartialpainrelief.Kuoetal.28
foundthat12oftheir48patientshadproblemswiththe
fix-ation,consistingoflooseningofthesynthesismaterialand
lossofthereduction.Thesepatientsevolvedwitharthrosis,
butonlysixofthemrequiredarthrodesis.
LyandCoetzee29performedopenreductionandinternal
fixationwithtwoscrewsontheirpatientswithpurely
liga-mentinjuries(20cases).Theyfoundsynthesisfailurein16
cases and evolutionto arthrosis in15 cases.Of these,five
patientsunderwentreoperationwitharthrodesis.Amongthe
20patientstreated,onlysixreturnedtowork.Amongour10
casesofpurelyligamentinjury,fiveweretreatedsurgicallyand
fourofthemunderwentORIFwithtwoscrews.Ofthese,one
evolvedwithinfectionanddehiscenceofthesuture(patient1),
butpresentedagoodresultwithoutarthrosis.Twopresented
goodresultsinwhichoneevolvedwithasymptomatic
arthro-sis(patient9)andtheotherwithoutarthrosis(patient3).The
lastofthesecases(patient6)presentedasatisfactoryresult
withasymptomaticarthrosis.
WedidnotusetheAOFASscoreinourevaluationbecause
thisisnotasatisfactoryevaluationmethodamongathletes.
For thisreason,wesuggestthatthereshouldbean
evalua-tion described inthe materialsandmethods thatstratifies
theresultsintopoor,satisfactory,goodandexcellent,witha
clinicalcorrelation.
Conclusion
Correctdiagnosis directlyinfluencesthetreatmentand the
finalresultobtained.Lackofknowledgeoftheinjuryisthe
main factor responsible for underdiagnosingTurco’s injury
anditscomplications.Thereisaneedforrandomized
prospec-tivestudiesthatcomparethetypesofsynthesismaterialand
the evolution ofthe casestreated withthese materials,in
ordertodefinethebesttreatment.
Conflicts
of
interest
Theauthorsdeclarenoconflictsofinterest.
r
e
f
e
r
e
n
c
e
s
1.EnglanoffG,AnglinD,HutsonHR.Lisfranc
fracture-dislocation:afrequentlymisseddiagnosisinthe emergencydepartment.AnnEmergMed.1995;26(2):229–33.
2.CassebaumWH.Lisfrancfracture-dislocations.ClinOrthop RelatRes.1963;30:116–29.
3.PereiraCJ,EspinosaEG,MirandaI,PereiraMB,CantoRS. Avaliac¸ãodotratamentocirúrgicodafraturaluxac¸ãode Lisfranc.ActaOrtopBras.2008;16(2):93–7.
4.MyersonMS,FisherRT,BurgessAR,KenzoraJE.Fracture dislocationsofthetarsometatarsaljoints:endresults correlatedwithpathologyandtreatment.FootAnkle. 1986;6(5):225–42.
5.DePalmaL,SantucciA,SabettaSP,RapaliS.Anatomyofthe Lisfrancjointcomplex.FootAnkleInt.1997;18(6):356–64.
6.BurroughsKE,ReimerCD,FieldsKB.Lisfrancinjuryofthe foot:acommonlymisseddiagnosis.AmFamPhysician. 1998;58(1):118–24.
7.ArntzCT,VeithRG,HansenJrST.Fracturesand
fracture-dislocationsofthetarsometatarsaljoint.JBoneJoint SurgAm.1988;70(2):173–81.
8.VuoriJP,AroHT.Lisfrancjointinjuries:traumamechanisms andassociatedinjuries.JTrauma.1993;35(1):40–5.
10.VanRijnJ,DorleijnDM,BoetesB,Wiersma-TuinstraS, MoonenS.MissingtheLisfrancfracture:acasereportand reviewoftheliterature.JFootAnkleSurg.2012;51(2):270–4.
11.FaciszewskiT,BurksRT,ManasterBJ.Subtleinjuriesofthe Lisfrancjoint.JBoneJointSurgAm.1990;72(10):1519–22.
12.HarwoodMI,RaikinSM.ALisfrancfracture-dislocationina footballplayer.JAmBoardFamPract.2003;16(1):69–72.
13.HardcastlePH,ReschauerR,Kutscha-LissbergE,Schoffmann W.Injuriestothetarsometatarsaljoint.Incidence,
classification,andtreatment.JBoneJointSurgBr. 1982;64(3):349–56.
14.PerronAD,BradyWJ,KeatsTE.OrthopedicpitfallsintheED: Lisfrancfracture-dislocation.AmJEmergMed.
2001;19(1):71–5.
15.TurcoVJ.Diastasisoffirstandsecondtarsometatarsalrays:a causeofpaininthefoot.BullNYAcadMed.1973;49(3):222–5.
16.NunleyJA,VertulloCJ.Classification,investigation,and managementofmidfootsprains:Lisfrancinjuriesinthe athlete.AmJSportsMed.2002;30(6):871–8.
17.ThompsonMC,MorminoMA.Injurytothetarsometatarsal jointcomplex.JAmAcadOrthopSurg.2003;11(4):260–7.
18.DesmondEA,ChouLB.Currentconceptsreview:Lisfranc injuries.FootAnkleInt.2006;27(8):653–60.
19.ShapiroMS,WascherDC,FinermanGA.RuptureofLisfranc’s ligamentinathletes.AmJSportsMed.1994;22:687–91.
20.HuntSA,RopiakC,TejwaniNC.Lisfrancjointinjuries: diagnosisandtreatment.AmJOrthop(BelleMeadNJ). 2006;35(8):376–85.
21.LovedayD,RobinsonA.Lisfrancinjuries.BrJHospMed (Lond).2008;69(7):399–402.
22.MyersonMS.Thediagnosisandtreatmentofinjurytothe tarsometatarsaljointcomplex.JBoneJointSurgBr. 1999;81(5):756–63.
23.MyersonMS,CerratoR.Currentmanagementof tarsometatarsalinjuriesintheathlete.InstrCourseLect. 2009;58:583–94.
24.PérezBlancoR,RodríguezMerchánC,CanosaSevillanoR, MunueraMartínezL.Tarsometatarsalfracturesand dislocations.JOrthopTrauma.1988;2(3):188–94.
25.RammeltS,SchneidersW,SchikoreH,HolchM,HeineckJ, ZwippH.Primaryopenreductionandfixationcomparedwith delayedcorrectivearthrodesisinthetreatmentof
tarsometatarsal(Lisfranc)fracturedislocation.JBoneJoint SurgBr.2008;90(11):1499–506.
26.TanYH,ChinTW,MitraAK,TanSK.Tarsometatarsal (Lisfranc’s)injuries–resultsofopenreductionandinternal fixation.AnnAcadMedSingapore.1995;24(6):
816–9.
27.HenningJA,JonesCB,SietsemaDL,BohayDR,AndersonJG. Openreductioninternalfixationversusprimaryarthrodesis forlisfrancinjuries:aprospectiverandomizedstudy.Foot AnkleInt.2009;30(10):913–22.
28.KuoRS,TejwaniNC,DigiovanniCW,HoltSK,BenirschkeSK, HansenJrST,SangeorzanBJ.Outcomeafteropenreduction andinternalfixationofLisfrancjointinjuries.JBoneJoint SurgAm.2000;82(11):1609–18.
29.LyTV,CoetzeeJC.Treatmentofprimarilyligamentous Lisfrancjointinjuries:primaryarthrodesiscomparedwith openreductionandinternalfixation.Aprospective, randomizedstudy.JBoneJointSurgAm.2006;88(3): 514–20.
30.RajapakseB,EdwardsA,HongT.Asinglesurgeon’s experienceoftreatmentofLisfrancjointinjuries.Injury. 2006;37(9):914–21.
31.MulierT,ReyndersP,DereymaekerG,BroosP.SevereLisfranc’ injuries:primaryarthrodesisorORIF?FootAnkleInt. 2002;23(10):902–5.
32.CoetzeeJC.MakingsenseofLisfranc’injuries.FootAnkle Clin.2008;13(4):695–704.
33.ClantonTO,McGarveyW.Athleticinjuriestothesofttissues ofthefootandankle.In:CoughlinMJ,MannRA,SaltzmanCL, editors.Surgeryofthefootandankle.8thed.Philadelphia: Mosby;2006.p.1520–7.
34.PerugiaD,BasileA,BattagliaA,StopponiM,DeSimeonibus AU.FracturedislocationsofLisfranc’jointtreatedwithclosed reductionandpercutaneousfixation.IntOrthop.