REVISTA
BRASILEIRA
DE
ANESTESIOLOGIA
OfficialPublicationoftheBrazilianSocietyofAnesthesiologywww.sba.com.br
MISCELLANEOUS
Lumbar
spinal
anesthesia
with
cervical
nociceptive
blockade.
Critical
review
of
a
series
of
1,330
procedures
夽
Percio
Ramón
Becker
Benitez
∗,
Celso
Schmalfuss
Nogueira,
Ana
Cristina
Carvalho
de
Holanda,
José
Caio
Santos
SuperiorTitleofAnesthesiology,SociedadeBrasileiradeAnestesiologia(SBA),RiodeJaneiro,RJ,Brazil
Received6April2014;accepted26May2014 Availableonline28November2015
KEYWORDS Spinalanesthesia; Plasticsurgery; Complications; Prevention; Treatment
Abstract
Backgroundandobjectives: Themanufactureofminimallytraumaticneedlesandsynthesisof pharmacological adjunctswithsafe andeffective actiononinhibitory andneuromodulatory synapsesdistributedalongthenociceptivepathwayswerecrucialforanewexpansionphase ofspinal anesthesia. The objectivesofthis paperarepresent our clinicalexperience with 1330lumbarspinalanesthesiaperformedwithpurposefulnociceptiveblockadeofthethoracic andcervical spinalnerves correspondingto dermatomesC4 orC3; warnaboutthe method pathophysiologicalrisks,andemphasizepreventivestandardsforthesafeapplicationofthe technique.
Content: Review of the historical background and anatomical spinal anesthesia with cer-vical levels of analgesia. Description of the technique used in our institution; population anesthetized; and surgery performed with the described method. Critical exposition of the physiological, pathophysiological, and clinical effects occurred and registered during anesthesia-surgeryandpostoperativeperiod.
Conclusion:SpinalanesthesiawithnociceptiveblockadetodermatomeC4,orC3,isaneffective optionforsurgeryonsomaticstructuresdistaltothemetamerofthethirdcervicalspinalnerve, lastingnomorethanfourorfivehours.Themethodsafetydependsontheunrestrictedrespect fortheessentialrulesofproperanesthesia.
©2014SociedadeBrasileiradeAnestesiologia.PublishedbyElsevier EditoraLtda.Allrights reserved.
夽 Studycenter:MedCenterUnidadeCirúrgica,Santos,SP,Brasil.
∗Correspondingauthor.
E-mail:perbec@hotmail.com(P.R.B.Benitez).
http://dx.doi.org/10.1016/j.bjane.2014.05.016
PALAVRAS-CHAVE Raquianestesia; Cirurgiaplástica; Intercorrências; Prevenc¸ão; Tratamento
Raquianestesialombarcombloqueionociceptivocervical.Revisãocríticadeuma seriede1.330procedimentos
Resumo
Justificativaeobjetivos: A fabricac¸ão de agulhas minimamente traumáticase a síntesede coadjuvantesfarmacológicoscomac¸ãoefetivaeseguranassinapsesinibitóriase neuromodu-ladorasdistribuídasaolongodasviasnociceptivasforamdeterminantesparaumanovafasede expansãodaanestesiasubaracnoidea.Osobjetivosdesteartigosão:apresentaraexperiência clínicadosautorescomarealizac¸ãode1.330Raquianestesiaslombarescombloqueio nocicep-tivopropositaldosnervosespinhaistorácicosecervicaisatéosdermátomoscorrespondentesa C4ouC3;alertarsobreosriscosfisiopatológicosdométodoeenfatizarasnormaspreventivas paraarealizac¸ãodatécnicacomseguranc¸a.
Conteúdo: Revisãodosfundamentoshistóricoseanatomofuncionaisdaanestesiasubaracnoidea com níveis cervicais de analgesia. Descric¸ão da técnica utilizada em nossa instituic¸ão; da populac¸ãoanestesiadaedascirurgiasrealizadascomométododescrito.Exposic¸ãocríticados efeitosfisiológicos,clínicosefisiopatológicosocorridoseregistradosduranteoato anestésico-cirúrgicoenoperíodopós-operatório.
Conclusão:ARaquianestesiacombloqueionociceptivoatéodermátomodeC4,oudeC3éuma opc¸ãoefetivaparacirurgiassobreestruturassomáticasdistaisaometâmerodoterceironervo espinhalcervicalcomdurac¸ãonãosuperiora4ou5horas.Aseguranc¸adométododependedo respeitoirrestritoàsregrasessenciaisdacorretapráticaanestésica.
©2014SociedadeBrasileira deAnestesiologia.PublicadoporElsevierEditoraLtda.Todosos direitosreservados.
Introduction
Westartedtheextensivetrialofspinalanesthesia(SA)for abdominoplastyandliposuctionin2004.Whenwefindthat often the breast region, innervated by intercostal nerves fromT2toT7,longlateralthoracicnervederivativeofthe brachialplexus,andlowercervicalplexusbranches,alsohad surgicalanesthesia,itencouragedustousethemethodfor mammoplastyandsincethenSAhasbecomethetechnique ofchoiceofourServiceforsuchprocedures.1,2In2007,we
developedaSpecificAnestheticForm(SAF-SA)inwhichwe registeredtheSAperformedforcosmeticand/orabdominal andthoracicrepairproceduresandthemainintraoperative andpostoperativeevents.3---9Thisarticleistheresultofthe
SAFretrospectivereviewof1330consecutiveSAperformed betweenDecember2007andDecember2013.
Highspinalanesthesiaisnotnewinanesthesiology liter-ature.Jonnescoin1911,LeFiliartrein1921,andHKosterin 1928leftimportanthistoricallegaciesonthetechnique.10
By the 70s of last century, Reynolds, Hudges, Bonica, Melzack, and Wells, among others, performed the pio-neering studies of neuromodulation of painin spinal cord segments,suprasegmentalstructuresofthebrainstemand adjacentsubcorticalareas.Thesesynapses’inhibitory neu-rotransmitters and modulators were identified, and the pharmaceuticalindustrysynthesizedexogenousagentsable to mimic these actions.11---14 Sufentanil and clonidine are
listedastwooftheadjuvantdrugsmostexperimentallyand clinicallystudiedbythesubarachnoidroute.Extensive sci-entific documentationconfirms andsupportsthesafetyof theopioidandalpha-2adrenergicassociationto0.5% hyper-baric bupivacaine improving theSA quality,duration, and residualanalgesia.15---32
Method
The study protocol was approved by the Research Ethics CommitteeofHospitalSantaCasadeMisericórdia,Santos, SP.
Patientselection
In this series of procedures 1330 subjects were enrolled, withphysical status ASA Ior II, between 17 and 72years old,scheduledforplasticsurgeryinupperareasofthebody, withan expected maximum duration of five hours, with-outcontraindicationfor SAandwho,afterclarificationon thetechnique,record,andreviewofdatacollectedforthis study,givetheirwrittenconsent.
Techniquedescription
Performacompletecheckofallanestheticmaterialinthe operatingroom(OR).
Dilute and label50mgof ephedrine in 10mL of saline solution (SS) or distilled water (DW) and have atropine, metaraminol,andadrenalineampoulesforimmediate open-ingifrequired.
Make sure that the operating table is able to offer a 30◦head-downtiltpositionandsecurelyattachthematto
preventitfromsliding.
Confirmtheidentityofthepatient,theproceduretobe performed, the preoperative evaluation information, and theadministrationofpre-anestheticdrug(midazolam15mg orally).
Monitor vital parameters (SBP, DBP, MAP, HR), cardiac rhythm,percentageofhemoglobinsaturation,andlevelof consciousness/sedationaccordingtoRamsayScale.Record thebaselinemeasuredvaluesastimereference‘‘zero’’’in SAF-SA.
CatheterizationofupperlimbperipheralveinwithJelco 20or 22G,proceed toinstitutionalantibiotic therapyand beginrapid infusion of the first 500mL infusion of Ringer lactate.
Adaptingandfixingnasalcatheterforcontinuoussupply ofO2ataflowrateof2Lmin.Positionthepatientinasitting
and relaxed position; perform the antisepsis of the lum-bosacralregion withchlorhexidine 0.5%;choose the most favorableinterspacebetweenL2/L3orL3/L4;considerthe convenienceofthepreviouslocalinfiltrationwithlidocaine 0.5%;performthesubarachnoidpunctureandafterthefree flowofthecerebrospinalfluidinjecttheanestheticmixture ofsufentanil5g,clonidine 150g,andbupivacaine0.5% hyperbaric20mgwiththehighestpossiblespeed.Afterthe injection,thepatientshouldbeimmediatelyplacedinthe supinepositionandwiththesamepromptnesstiltthetable 30◦head-down,takingcaretopreventpatientsliding,and
keepthispositionfor15min.Measurevitalsignsandrecord themevery5minintheSAF-SA.
Afterwaiting15min,puttheoperatingtableinthe hor-izontalplane andcomplete antisepsiscareof thesurgical area,checkout the sensoryblock level withthe pinprick test(needle30×7),andauthorizethestartofsurgery.
Hemodynamiccontrol
The‘‘trigger’’forintravenousadministrationofephedrine 10mg is SBP below 85mmHg. Regarding bradycardia, atropine0.5mgadministeredwhenHRisbelow55bpm.In casesoftachyphylaxisorinsufficientresponsetoephedrine, metaraminol0.25mg administeredvery slowly with care-ful attention to HR.Fluid therapy is continued according tothe classical criteria. Hyperhydration is not necessary. Inliposuction,thesalineandadrenalinevolumesinfiltrated duringthewetortumescenttechniquemustberegistered andshouldnotcontainlidocaine.35---38
Ventilation
Ifthereishypoventilationduetoexcessivesedationor respi-ratorydepressioncausedbyanestheticblock,ensureupper airwaypatency and assistventilation tothe efficientand safereturnofspontaneousrespiration(SR).39,40
Sedation
Afterblockadeinstallation,sedationshouldbelight, com-fortable,andsafe(RamsaygradeIIIorIV)withpermanent airwaymonitoring.Intravenousadministrationof fraction-ateddosesofmidazolam(1mg)associatedornotwithdoses ofS+ketamine(2.5mg).41
Table1 DistributionofpatientsaccordingtosexandASA
classification.
Totalnumberofpatients 1330
Female:1271 Male:59
ASAI:883 ASAII:447
ASA,AmericanSocietyofAnesthesiologists.
Table2 Distributionofpatientsaccordingtoage.
<20years 19 1.4%
Between20and29years 181 13.6% Between30and39years 394 29.6% Between40and49years 446 33.5% Between50and59years 223 17.0% Between60and69years 58 4.3%
>69years 9 0.6%
Changesinsurgicalpositioning
Evaluatewhetherit isprudenttogive10mgofephedrine one minute prior to mobility, notify and request the patient cooperation during movements. Avoid abrupt maneuvers.42,43
In the final stages of the procedure, if there is no contraindication, give dipyrone 25mgkg−1 and tenoxican
0.5mgkg−1 IV. Ifthere arerisk factors for post operative
nausea and vomiting (PONV), add antiemetics. Continue monitoringuntiltheendofdressings,commandthe trans-ference tothestretcher andtake the patienttothepost anesthesiacare unit(PACU)where hemodynamic, respira-tory, and analgesic monitoring should be continuous and recorded by thenursing service. Sign thedischarge order fromPACUwithAldreteandKroulickIndex9or10,without painandPONV.
Intheward,theNursingServiceshouldrecordinthe SAF-SA thepatients’ clinical outcome,painintensity by visual numericscale(VNS),andtheoccurrenceofadverseevents relatedtotheanesthetictechnique.
Physicalandclinicalcharacteristicsofpatients
Tables1---7.
Discussion
The relative density at 37◦C and the volumes of
the administered pharmacological agents are: clonidine: 0.99940(1mL),sufentanil:0.99930(1mL),both,therefore,
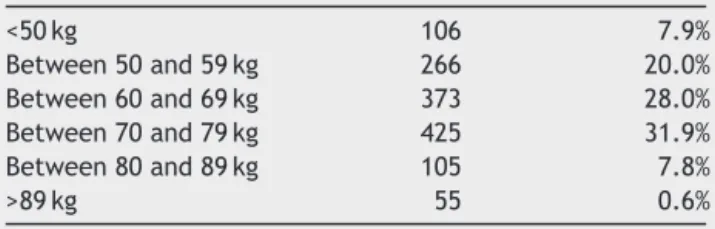
Table3 Distributionofpatientsaccordingtobodyweight.
<50kg 106 7.9%
Between50and59kg 266 20.0% Between60and69kg 373 28.0% Between70and79kg 425 31.9% Between80and89kg 105 7.8%
Table 4 Subarachnoid puncture site and degree of difficulty.
L2---L3 1237 93.1%
L3---L4 93 6.9%
1stattempt 1011 76.0%
2ndattempt 226 16.9%
>2attempts 93 6.9%
Table 5 Total number and percentage of surgeries
performed.
Typeofsurgery Total %
Mammoplasty 324 24.4
Abdominoplasty 357 26.8
Liposuctioncontouring 307 23.1
Combinedsurgeries 342 25.7
Table6 Percentageofpatientsreceivingcardiocirculatory
actingdrugs.
Drug %ofpatients
Ephedrine 100
Atropine 52
Metaraminol 8
Adrenalin 0.07
are located at the limit between the iso and hypobaric-ityregardingtheCSFofrelativedensity at37◦C,variable
between0.99440and1.00230.Thevolumeof4mLof bupi-vacaine 0.5% in hypertonic solution of glucose is frankly hyperbaric (1.02360) compared to cerebral spinal fluid (CSF).Wefoundnobibliographicreferenceontherelative densitycorrespondingtothemixtureofbupivacaine, cloni-dine,andsufentanilusedinthisstudy;however,itsobvious rostralspreadinthepatientpositionedinahead-downtilt positionendorsesitshyperbariccondition.44,45
Table7 Eventsandcomplications.
Type Percentage
SBP<85mmHgattheOR/PACU 100.00 HR<55bpmattheOR/PACU 57.00 Lipothymiaattheward 23.00
ApneaattheOR 1.30
Hbsaturation<90%attheOR 31.00 PruritusattheORandPACU 33.00 PONVatthePACUandward 7.00 Urinaryretentionattheward 3.00
Headachepost-SA 0.30
Transientneurologicalsequelae 0.07
CA 0.07
Death 0.00
Theabsenceofpaintovigorousstimulationwitha30×7 hypodermicneedleintotheskinareacorrespondingtothe sternumnotch,orslightlycephaladatthesternalnotch con-firmstheblockadeofnociceptivefibersA-deltaandCupto themetamerofthe4thor3rdpairofcervicalspinalnerves. Thislevelofsomaticanesthesiaimpliesfullthoracolumbar sympatheticblock. In approximately 30% of patients, we provedthe lack of sensitivity topinprickin facialregions innervated by afferentnociceptive branches: mandibular, maxillary,andophthalmic oftrigeminal nervethathas its first-orderneuronsintheganglionofGasser,fromwherethe afferentaxonsprojecttoward thecentralsensorynucleus located at the level of the brainstem bridge. The point ofemergence fortheX cranial nerve(CN)toward itsvast peripheralterritoryoccursatthebulblevel;therefore, cau-dallyinrelationtoV(CN).46,47Intheabsenceofanatomical
barrierbetweentheCSFofbrainandspinalcompartments, nothingpreventsthehyperbaricanestheticmixtureinjected intothe lumbar subarachnoidspace to disperse cephalad intothe brainstem40,48 andthat diluted concentrations of
thesamemixturemayinteractinascendingsequencewith thevagusautonomicBfibers,trigeminalA-deltaandC noci-ceptivefibers, andother suprasegmentalsynapsesrelated tothe emotionaland behavioralautonomic modulationof pain.Thisfeasiblepossibilityprovidestheanatomicalbasis forthefollowingclinicalsignsseeninmostpatientsinthis study:(1)attenuationofvagal‘‘exacerbation’’expectedas aresultof the totalsympatheticblockade; (2)trigeminal territoryanalgesia proved by performingsmallfacial pro-cedures,such aschin liposuction,filling expression folds, andremovalof smalltumorsfromneck andface,without additionallocalorintravenousanesthesia;(3)feelingof sat-isfactionandwell-beingreportedbypatientsattheendof surgeryandlackoffrequentshiveringuponawakeningfrom generalanesthesia.3,6,11,13,14,16,36,49
Regarding hemodynamic aspects, hypotension and decreasedheart rate (HR) arephysiological consequences inherenttospinalblocks.Inthisstudy’spatients, bradycar-diaandhypotensionresponded satisfactorilytotreatment with antimuscarinic and vasopressors. Classically, the etiologyofbradycardiaisattributedtoautonomicblockade ofsympatheticpreganglionicfibersfromT4toT1and con-sequentrelease of cardioinhibitory reflexof vagal origin. Hypotension is related to the decrease of three factors: systemic vascular resistance, venous return, and cardiac output (CO). The intensity of blood pressure (BP) fall is considered proportionalto theextent of the sympathetic thoracolumbarchain blockade.37,38,42,50 It shouldbenoted
Frank-Starlinglawoftheheartinnormovolemicconditions are able to maintain sufficient CO and HR to the basal needsasoccursindenervatedandtransplantedhearts.The microcirculation which constitutes more than 90% of the cardiovascular areahas efficient flow controls dependent onmetabolicreleasingfactorsandlocalaction,andfinally, in addition to catecholamines there are other systemic vasoactivemediators,suchasangiotensin,dopamine,and serotonin, which are not blocked by SA.6,43,50 In 1994,
Oberlander performed electrophysiological studies with newborn animals and demonstratedthat the sympathetic blockade promoted parasympathetic inhibition reflex, which partially explain the fact that normovolemic new-bornsandinfantsdonotdevelopbradycardiaorhypotension evenunder completespinal block.51 Similarly resultcould
be produced by diluted concentrations of the anesthetic mixtureadministeredinthisstudy,atthebrainstemlevel.
Withinsafelimits,decreasedHRandBPunder anesthesi-ologistcontrolarebeneficialanddesirabletoreduce intra-operativebloodloss.Allpatientsinthisstudy,atsometime ofsurgeryoratPACU,hadSBPbelow85mmHg.Theruleisto relocatethepressurelevelabovethesafetylimitwithdoses ofephedrine10mg.In8%ofpatients,ephedrinewasnot suf-ficientfor BPstabilizationandmetaraminoladministration wasrequired.Due tosudden and severebradycardia that thiseminently␣1 vasoconstrictoriscapable ofproducing, we make the following recommendations: prepare highly dilutedsolutionscontaining0.25mgofmetaraminolpermL, giveonly 1mLeach timeand,beforegiving metaraminol, have another syringe prepared with atropine 0.5mg. We giveatropinebeforemetaraminolifHRislessthan60bpm. Subsequentdosesofmetaraminolrequirethesamecare.
AllpatientsinourstudysufferedadecreaseinbasalHR. In 52% of them, HR was lower than the 55bpm adopted aslimit and trigger for the intravenous administration of atropine at doses of 0.5mg, which can and should be repeateduntil the return of HR tosafe levels. Severe or moderatebradycardiaisthemostimportantpredictor sig-nalofcardiacarrest(CA)duringSA.52Nottreatingsignificant
bradycardiaandhypotensionresultingfromSAis compara-ble togiving neuromuscularblocker or hypnotic doses of propofolwithoutpatientventilation.
In the series of 1330 consecutive SA reviewed in this paper,therewasonecaseofCA,whichoccurredinafemale ASA I patient, aged 30, who underwent liposuction. The anesthesiologist whoperformed the puncture and started theanesthesiahad toleavethe ORand leftassubstitute anotheranesthesiologistwithless experienceinthe tech-nique. In 45min of operation, the following values were measured: BP 80/40mmHg and HR 50bpm, which were not immediately corrected in accordance with the study protocol rules (ephedrine 10mg and atropine 0.5mg) on thegroundsthat,despitethehypotensionandbradycardia, hemoglobinsaturation remained satisfactory at 95%. Very severe bradycardia came next and, in sequence, asystole observed by isoelectricbaseline in cardioscope and pulse oximeter. Treatment was immediate and consisted of externalcardiaccompression (ECM)madebythe surgeon, ventilation under mask, followed by tracheal intubation (TI) and administration of intravenous adrenaline (1mg). Theresponsewasrapidandfavorablewithcardiacactivity returnin sinusrhythm, rategreater than 150bpm andBP
180/90mmHg. The patient recovered in the ICU and was later discharged without neurological sequelae. It was, therefore, an absolutelyavoidable CAin which the anes-thetic technique cannot be exclusively held responsible. SomestudiesincludeyoungandhealthypatientsinCArisk groups during SA. One needs to reconsider whether acts ofnegligenceorrecklessnessarenotunder-investigatedat theconclusionofthesestatistics.53---56
Whenthepatientsaretransferredtotherecoveryroom, they are accompanied by labeled syringe of epinephrine usedintheOR,ashypotensionislikelytocontinueduring recoveryfromanesthesiaandevenlaterinthewardswhere one of the most observed complications was lipothymia. These observationsconfirm the assumption that hemody-namic monitoring shouldbe continueduntil thecomplete blockade resolutionand hospitalizationshouldnotbe less thantwentyhoursfromthelumbarpuncture.42Specialcare
shouldbetakeninpatientsundergoingmajorliposuction.7
We noted that some moderate hypertensive patients treated with beta-blockers or angiotensin converting enzyme(ACE)inhibitorsreceivedhigherdosesofephedrine/ metaraminolandatropine,butthedatacollectedwas insuf-ficienttoqualifiedanalysisandstatisticalconclusions.39
DuringhyperbariclumbarSA inthesittingposition,the lumbosacralmotorrootsarequicklyblocked.Bypositioning thepatientsimmediatelysupineandtiltedhead-down,the hyperbaric anestheticmixtureis dispersedinthecephalic direction andtheinitialconcentrationof thesolutionwill bedilutedinthecourseasitmovesawayfromthepuncture site.5,46,47 With the sensoryblock alreadyinstalled onC3,
thereisvasodilationintheupperlimbsandmuscleactivity partiallypreserved. The patientdoes notfeelthepain of liposuctioninthearms,butcanstillmovethem.This dif-ferentialblockadehappensforthreereasons:first,the max-imumconcentration(Cm)of bupivacainethatreached the brachialplexuswasenoughtoblockthenociceptiveAdelta andCfibers,butnotenoughtoblockthemotorAlphafibers; second,insupinepositionthehyperbariclocalanestheticis distributedpreferentiallyaroundtheposteriornociceptive roots; and third, the cervical roots compared tothe tho-racic andlumbar roots has more perpendicularand short courseswithinthespinalcanal,andthereforelesserextent ofexposuretothedilutedlocalanestheticintheCSF.46---48In
thebreathingmuscles,therearethefollowingclinicalsigns: relaxationofabdominalmuscles(obliques,transverse,and rectus)auxiliaryofactiveexpiration,ofcoughingand expec-toration.Theinternalintercostalmuscles(expiratory)and external (inspiratory), due to the decreasing CM are less blockedastheyapproachT1.ThePhrenicNerve, responsi-bleforthemainmuscleofinspirationactivity,hasitsorigin intheanteriorrootsofC2andC3anditsmotoractivityis preserved for thesame reasonsindicated for thebrachial plexus motor function.57 At baseline and rest conditions,
article should be avoided in obese patients and in those withchronic lung disease.58---61 Our serieshad 17 casesof
prolongedapnea withHRandBP preserved,thus, exclud-ingthebloodreducedflowfrombulbarrespiratorycenters asa cause of the event.The episodesof apnea occurred beforethe30minafterthesubarachnoidpuncture,with pro-gressivedecreaseinrespiratoryrateandconsciousnessfor periodsoftimevaryingbetween5and35min.Patientswere ventilatedmanuallyinsemi-closedsystemwithfacialmask andoneofthemwithlaryngealmask.Spontaneous breath-ingand consciousnessgraduallyreturnedwithout memory ofthefact.Itisreasonabletodisregardthattheseperiods ofapneaandunconsciousnesswereproducedpredominantly bycriticalconcentrations oftheanestheticmixtureinthe CSFaroundthebrainstem.40,48Thirtyonepercentofpatients
atsometimeduringanesthesiahadhypoventilation charac-terizedbyreducedhemoglobinsaturation,coincidentwith deeper levelsofcentral sedationand participationof the obstructive peripheral component due to the pharyngeal muscle relaxation.All patients improved quicklywith the usualmaneuversofupperairwayclearance.Sedationisan issuethatrequiresspecialcare,asmanypatientssaythey aresleepyanddidnothearorfeelanything.Thisdilemma requires patience and persuasion strategies by the anes-thesiologist,becauseexcessivesedationisassociatedwith lower cardiorespiratory safety. When administering intra-venousfractionated andparsimoniousdosesofmidazolam (1mg)associatedornotwithdosesofketamineS+(2.5mg), one should consider the sedative action of clonidine and sufentanil used in the anesthetic mixture. Patients who receivedoralpremedicationwithmidazolam(15mg)15min beforebeingtransportedtotheORhadlessneedfor intra-venous sedatives and more stable and secure degree of sedationwithlowerincidenceofreducedhemoglobin satu-rationintheintraoperativeperiod.41,62Theuseofdroperidol
duringspinalblocksisassociatedwithreportsofarrhythmias andcardiacarrestrefractorytotreatment; thus,itshould beformallycontraindicated.
During liposuction,fat grafts,andmammoplasties, the surgical team usually asks for several changes of patient positioning.Thelossofsympatheticvasomotoractivitycan provide adaptive imbalances betweenintravascular conti-nent andcontentduringsudden movements,especiallyin thegreatvesselswithrepercussionsonrhythm,CO,andBP. Thepronepositionduringspinalblocksisrelatedtoseveral reports of serious complications. The guidelines for posi-tioning changes (see above) were effective in preventing complications.37---39,53,56,63
Facialpruritusaroundthemouth, eye,andnose during surgeryorduringrecoveryfromanesthesiawasreportedby 33%ofpatients.Mostofthetime,itistolerableunder sur-facesedation,butcanbecomeintenseandrequirecareful deepersedationorspecifictreatment.17
Incasesofcombinedsurgery,itisprudenttorequestthe initiationofsurgerybythethoracicproceduresfollowedby the abdominal,asnociceptivesensation graduallyreturns in the most cephalic areas of the blockade around the fourth hourandthen returnindirection andsequence. In mostpatients,somaticsurgicalanalgesiapersistsonT7at thefifthhourandonT10atthesixthhour.Incaseswhere anesthesiawasinsufficienttocompletethemammoplasties intheareolarregion,skinandsubcutaneousinfiltrationwas
performedwithlidocaine0.25%orweassumedventilation andincreasedsedation withketamine and midazolam S+, orwithsedativedosesofpropofolininfusionpump.41,64
In the PACU, the return of lower limbs movements occurred between the fifth and seventh hour. Fifty six percent of patients were discharged from PACU without referring any adverse effect, with cardiovascular sta-bility, without use of vasoactive drugs, conscious, and without pain. The most frequent complications in other patientswere: systolicBP<85mmHg,VNS>3, itching, HR <55bpm,andPONV(Table7).Allcomplicationssatisfactorily respondedtospecifictreatment.
Duringhospitalizationinwards,64%ofthepatients pro-gressedwithoutpainorothercomplaintsoradverseeffects. Itisworthnotingthesignificantincidenceoflipothymia dur-ingthefirstor second attempttoget outof bed bymost cases after ten hours postoperatively. All cases improved rapidlywithsupinepositionandlower limb liftingat 90◦,
withoutvasoactivedrugsandwiththerecommendationto waittwohourstoretrywalking.BPandHRmeasurements aftertheconditionimprovementandwiththepatientsupine positionshowednormalvalues.Twelvepercentofpatients reportedpain>5intheVNS,but12haftertheblockade.
A56yearoldpatientcomplainedofparesisand paresthe-siainthedistalendoftherightleginthesensoryandmotor areaofL4andL5,65withtheonsetofsymptomsbefore
hos-pitaldischarge.Thetransientneurologicalsymptomswere treated withcommon analgesics, pregabalin, and physio-therapy,andshowedprogressiveimprovementfromthe15th postoperativedayandsubsequentcompleteresolution.66,67
Our incidence of headache after typical spinal anes-thesia was 0.3%, and in most of them the puncture was single.Headachewasmildtomoderateandevolved favor-ablywithcommonpainkillers without autologousepidural bloodpatch.68,69
Conclusion
Lumbar spinal anesthesia with nociceptive blockade in cervicaldermatomesperformedwithhyperbaricmixtureof 20mgof bupivacaine0.5%combinedwith150gof cloni-dineand5gofsufentanilisaneffectiveoptiontoperform abdominoplasty, surgery on breast tissue, liposuction of bodyregionsinnervatedbydistalC3spinalnerves,provided thatthedurationoftheproceduredoesnotexceedfourto fivehours.The techniquesafety dependsonthe absolute respectto the contraindications of SA, knowledge of the physiologicaleffects,andattentiveandconstantvigilance of the anesthesiologist to the correct treatment of the potentialcomplicationsofintravenoussedationassociated withSA.
Conflicts
of
interest
Theauthorsdeclarenoconflictsofinterest.
References
2.BenitezPRB,NogueiraCS,SantoJC.Raquianalgesiatotalcom estabilidade respiratória e cardiocirculatória. Considerac¸ões clínicas sobre dez bloqueios realizados. São Paulo Med J. 2009;128Suppl:10.
3.GreeneNM.Physiologyofspinalanesthesia.4thed.Willian& Wilkins;1993.
4.CangianiLM,CangianiLH,LuttiMN,etal.Anestesia Subarac-nóidea. Tratado deAnestesiologia. SAESPSão Paulo: Editora Atheneu;2011.
5.DalensB.AnestesiaLocorregional.DorecémNascidoaoAdulto. RiodeJaneiro:Ed.Revinter;1999.
6.GuytonAC,HallJE.Textbookofmedicalphysiology.11thed. Philadelphia,Pennsylvânia:ElsevierSaunders;2006.
7.CavalcantiIL,CantinhoFAF,AssadA.AnestesiaparaCirurgia Plástica.RiodeJaneiro:SAERJ;2005.
8.NocitiJR.AnestesiaparaCirurgiaPlástica.Tratadode Aneste-siologia.SAESPSãoPaulo:EditoraAtheneu;2011.
9.BenitezPRB,Nogueira CS, OliveiraCRD.Raquianestesiapara cirurgiaplástica.In:ImbelloniLE,editor.Raquianestesia.Rio deJaneiro:Elsevier;2013.
10.Jonnesco T. General Spinal Analgesia. Br Med J. 1909;2:1396---401.
11.GebartGF.Controleretrocaudaldador.In:(Eds.).DorPrincípios ePrática,SãoPaulo:ArtmedEditoraSA.
12.GozzaniJL.Fisiopatologiadador:dorpósoperatória.Riode Janeiro:SBA;2004.
13.OliveiraLM,SilvaLFS.Mecanismosneuraisemodulac¸ãodador. Em:Neto AO,Costa CMdeC,SiqueiraJTT, TeixeiraMJ.Dor PrincípiosePrática,SãoPaulo:ArtmedEditoraSA.
14.PiresCP,PossoIP,ConstantinoE,etal.Bioeletrogêneseda Mem-brana. In: Transmissãosináptica. Tratado de Anestesiologia. SAESPSãoPaulo:EditoraAtheneu;2011.
15.OliveiraCRD,NogueiraCS.Fármacos␣2agonistas.Tratadode
Anestesiologia.SAESPSãoPaulo:EditoraAtheneu;2011.
16.Serra AP,Ashmawi HÁ. Encefalinas eEndorfinas. Tratadode Anestesiologia.SAESPSãoPaulo:EditoraAtheneu;2011.
17.SouzaAM,SlullitelA,VanettiTK,etal.AgonistaseAntagonistas opioides.TratadodeAnestesiologia.SAESPSãoPaulo:Editora Atheneu;2011.
18.YamaguchiET,CarvalhoJCA,FonsecaUS,etal.Sufentanil sub-aracnoideoassociadoàBupivacaínahiperbáricaparaanalgesia departo:épossívelreduziradosedoopióide?RevBras Aneste-siol.2004;54:142---52.
19.Belzarena SDG. Analgesia obstétrica por via subarac-noidea: comparac¸ão entre sufentanil isolado ou associado a minidose de bupivacaína. Rev Bras Anestesiol. 1995;45: 369---76.
20.ImbelloniLE.OpioidesnaRaquianestesia.In:ImbelloniLE, edi-tor.Raquianestesia.RiodeJaneiro:Elsevier;2013.
21.Seligman MM. Fármacos analgésicos não opioides na Raquianestesia.LEImbelloni.Raquianestesia.RiodeJaneiro: Elsevier;2013.
22.EisenachJC,DeKockM,KlimschaW.Alpha2-adrenergicagonists forregionalanesthesia:aclinicalreviewofclonidine. Anesthe-siology.1996;88:523---6.
23.Tamsen A, Gordh T. Clonidine is not neurotoxic. Lancet. 1984;II:876.
24.AlvarezMAP,AcostaJAG,GodoyMC.Opióidesna Raquianeste-sia.In:ImbelloniLE,editor.TratadodeAnestesiaRaquidiana. 1sted.Curitiba:MedidáticaInformáticaLtda;2001.
25.Schechtmann G, Wallin J, Meyerson BA, et al. Intrathecal clonidinepotentiatessuppressionoftactilehypersensitivityby spinalcordstimulationinamodelneuropathy.AnesthAnalg. 2004;99:135---9.
26.BrazJRC,KogutiES,BrazLG,etal.Efeitosdaassociac¸ãoda clonidinaàbupivacaínahiperbáricanaanestesiasubaracnóidea alta.RevBrasAnestesiol.2003;53:561---72.
27.FörsterJG,RosembergPH.Smalldoseofclonidinemixedwith low-doseropivacaineandfentanylforepiduralanalgesiaafter totalkneearthroplasty.BrJAnaesth.2004;93:670---7.
28.FonsecaNM,OliveiraCA.Efeitodaclonidinaassociadaà bupiva-caínaa0,5%hiperbáricanaanestesiasubaracnóidea.RevBras Anestesiol.2001;51:483---92.
29.Simonetti MPB, Vale NB. Farmacologia dos agentes espinais. Anestésicos locais e opiáceos. LE Imbelloni. In: Tratado de AnestesiaRaquidiana.Posigraf;Curitiba2.001ImbelloniLE ---TratadodeAnestesiaRaquidiana.Curitiba:EditoraMedidática InformáticaLtda;2001.
30.Simonetti MPB, Valinetti EA, Ferreira FMC. Clonid-ina: De Descongestionante Nasal a Analgésico Potente. Considerac¸õesHistóricaseFarmacológicas.RevBrasAnestesiol. 1997;47:37---47.
31.FilosKS,GoudasLC,PatroniO,etal.Intratecalclonidineasa soleanalgesicforpainreliefaftercesareansection. Anesthesi-ology.1992;77:267---74.
32.TebaldiTC,MalbouissonLMS,KondoMM,etal.Efeitodaadic¸ão declonidinasubaracnoideaàsoluc¸ãoanestésicadesufentanile bupivacaínahiperbáricaouhipobáricaparaanalgesiadeparto. RevBrasAnestesiol.2008;68:593---601.
33.ImbeloniLE.Materialutilizadoemraquianestesia.In:Imbelloni LE,editor.Raquianestesia.RiodeJaneiro:Elsevier;2013.
34.CuriEF,CarneiroAF.ChecklistemRaquianestesia.In:Imbelloni LE,editor.Raquianestesia.RiodeJaneiro:Elsevier;2013.
35.Malqvist LA, Bengtsson M, Bjoernsson G, et al. Simpathetic activityanddynamicvariablesduringspinalanalgesiainman. ActaAnaesthesiolScand.1987;31:467---73.
36.GoulartAP,AnatomiadoSNA.TratadodeAnestesiologia.SAESP SãoPaulo:EditoraAtheneu;2011.
37.TsudaGF,SartoriJÁ,FisiologiadoSNA.Tratadode Anestesiolo-gia.SAESPSãoPaulo:EditoraAtheneu;2011.
38.AulerJOC Jr,Messias ERR,Galas FRBG.Fisiologia Cardiovas-cular. Tratado de Anestesiologia. SAESP São Paulo: Editora Atheneu;2011.
39.Carmona MJC, Kim SM. Complicac¸ões Cardiorrespiratórias. TratadodeAnestesiologia.SAESPSãoPaulo:EditoraAtheneu; 2011.
40.CarneiroHM,OliveiraB,ÁvilaMP, etal.Anestesiadotronco EncefálicoapósBloqueioretrobulbarextraconal.Épossível evi-tar?Relatodecaso.RevBrasAnestesiol.2007;57:391---400.
41.CavalcantiSLE,NunesR.Sedac¸ãoemRaquianestesia.In: Imbel-loniLE,editor.Raquianestesia.RiodeJaneiro:Elsevier;2013.
42.OliveiraFilhoGR.Alterac¸õescardiovascularesda raquianeste-sia. LE Imbelloni. Raquianestesia. Rio de Janeiro: Elsevier; 2013.
43.Goldman&Gilman.ManualdeFarmacologiaeTerapêutica.Porto Alegre2.010AMGHEditoraLtda.
44.CangianiLM.Determinac¸ãodaDensidadeedaBaricidadedas misturas para anestesia subaracnoidea. Rev Bras Anestesiol. 2000;50:92---4.
45.Imbelloni LE, Moreira AD, Gaspar FC, et al. Assessment of the densities of Local Anesthetic and their combination withadjuvants: anexperimental study. Rev BrasAnestesiol. 2009;59:154---65.
46.PutzR,PabstR.AtlasdeAnatomiaHumanaSobotta.21sted. RiodeJaneiro:Ed.GuanabaraKoogan;2000.
47.HansenJT,KoeppenBM.AtlasdeFisiologiaHumanadeNetter. PortoAlegre:ArtmedEditoraAS;2002.
48.DuarteLTD,SaraivaRA.Raquianestesiatotalapósbloqueiodo plexobraquialporviaposterior:relatodecaso.RevBras Aneste-siol.2006;56:518---23.
49.CangianiLH.FisiologiadoSistemaNervosoCentral.Tratadode Anestesiologia.SAESPSãoPaulo:EditoraAtheneu;2011.
51.Oberlander TF, Berde CB, Lam KH, et al. Infants tolerate Spinal anesthesia com minimal overall autonomic chabges: analysisofheartratevariabilityinformerpremature infants during.
52.LimonguiJA,LinsRS.Cardiopulmonaryarrestinspinal anesthe-sia.RevBrasAnestesiol.2011;61:110---20.
53.CaplanRA,WardsRS,PosnerK,etal.Unexpectedcardiacarrest daringspinalanesthesiaaclosedclaimanalysisofpredisposing factors.Anesthesiology.1988;65:5---11.
54.Pollard JB. Cardiac Arrest During Spinal Anesthesia: com-monmechanismsandstrategiesforprevention.AnesthAnalg. 2001;92:252---6.
55.PereiraID,GrandoMN,ViannaPT,etal.Retrospective analy-sisofriskfactorsapredictorsofintraoperativecomplications inneuroaxial bloocksatFaculdadedeMedicinade Botucatu-UNESP.RevBrasAnestesiol.2011;61:568---81.
56.Martins CAS. Adrenérgicos e Anti adrenérgicos. Tratado de Anestesiologia.SAESPSãoPaulo:EditoraAtheneu;2011.
57.Cangiani LH, Rezende LAE, Neto AG. Bloqueio do Nervo Frênicoapós realizac¸ão de bloqueio do plexo Braquial pela via interescalênica. Relato de caso. Rev Bras Anestesiol. 2008;58:152---9.
58.SantosLM, Malbouisson LMS, Auler JOC Jr. Mecânica Respi-ratória.Tratadode Anestesiologia. SAESPSão Paulo: Editora Atheneu;2011.
59.ImbelloniLE.Avaliac¸ãodafunc¸ãomotoraabdominale parâmet-rosventilatóriosapósperiduraltorácica.RevBrasAnestesiol. 1988:233---6.
60.Delfino J. Efeitos respiratórios, gastrointestinais, genitour-inárioseendócrinosdaRaquianestesia.In:Imbelloni,Tratado deAnestesiaRaquidiana.Curitiba:Posigraf;2001.
61.BicalhoGP, BrazJRC. Efeitosrespiratórios, gastrointestinais, geniturinárioseendócrinosdaRaquianestesia.In:ImbelloniLE. Raquianestesia.RiodeJaneiro:Elsevier;2013.
62.Santos ETM. Benzodiazepínicos. Tratado de Anestesiologia. SAESPSãoPaulo:EditoraAtheneu;2011.
63.Vieira ZEG, Imbelloni LE. Efeitos cardiocirculatórios da Raquianestesia.LEImbelloni,TratadodeAnestesiaRaquidiana. Curitiba:Posigraf;2001.
64.PraxedesH,OlivaFAL.FalhasnaAnestesiaSubaracnoidea.Rev BrasAnestesiol.2010;1:90---7.
65.GanemEM.Complicac¸õesneurológicasdaRaquianestesia.In: ImbelloniLE,editor.Raquianestesia.RiodeJaneiro:Elsevier; 2013.
66.VasconcellosF◦ PO,PossoIP,CapelozziM,etal.Comparac¸ão
dasalterac¸õeshistológicasdaMedulaEspinaleneurológicasde cobaiasapósAnestesiasubaracnóideacomgrandesvolumesde BupivacaínaRacêmica.MisturacomexcessoEnantiomêricode 50%delevobupivacaína.RevBrasAnestesiol.2008;58:234---45.
67.ZuglianiA.BloqueiodosNervosperiféricosdosmembros super-ioreseinferiores.RiodeJaneiro:EditoraRevinterLtda;2007.
68.CarvalhoJCA,Cardoso MMSC.Raquianestesiaparacesariana: avaliac¸ãodacefaleiacomagulhasdeQuinckeeWhitacre25G e27G.VerBrasAnestesiol.1999;49:368---9.