REVISTA
BRASILEIRA
DE
ANESTESIOLOGIA
PublicaçãoOficialdaSociedadeBrasileiradeAnestesiologiawww.sba.com.br
SCIENTIFIC
ARTICLE
Patient
state
index
and
cerebral
blood
flow
changes
during
shoulder
arthroscopy
in
beach
chair
position
Mehmet
Ilke
Buget
a,∗,
Ata
Can
Atalar
b,
Ipek
Saadet
Edipoglu
a,
Zerrin
Sungur
a,
Nukhet
Sivrikoz
a,
Meltem
Karadeniz
a,
Esra
Saka
a,
Suleyman
Kucukay
a,
Mert
N.
Senturk
aa˙IstanbulUniversity,IstanbulMedicalFaculty,DepartmentofAnaesthesiology, ˙Istanbul,Turkey
b˙IstanbulUniversity,IstanbulMedicalFaculty,DepartmentofOrthopedicsandTraumatology, ˙Istanbul,Turkey
Received21December2014;accepted13February2015 Availableonline1October2015
KEYWORDS
Patientstateindex;
Cerebral;
Cerebralbloodflow;
Beachchairposition
Abstract
Backgroundandobjectives: The aim ofthe study were to demonstrate the possible hemo-dynamic changes andcerebralbloodflowalterationsinpatients who werepositioned from supinetobeachchairposition;andtodetectifthepositionchangecausesanycorticalactivity alterationasmeasuredbythe4-channeledelectroencephalographymonitor.
Methods:35patientswereincluded.Beforetheinduction,meanarterialpressureandpatient stateindexvalueswererecorded(T0).Aftertheintubation,doppler-ultrasonographyofthe patients’internalcarotidandvertebralarterieswereevaluatedtoacquirecerebralbloodflow valuesfromtheformula.Insupineposition,meanarterialpressure,patientstateindexand cerebralbloodflowvalueswererecorded(T1)andthepatientwaspositionedtobeachchair position.After5minallmeasurementswererepeated(T2).Measurementsofpatientstateindex andmeanarterialpressurewererepeatedafter20(T3),and40(T4)min.
Results:There was a significant decrease between T0 and T1 in heart rate (80.5±11.6 vs. 75.9±14.4beats/min), MAP (105.8±21.9 vs.78.9±18.4mmHg) and PSI (88.5±8.3 vs. 30.3±9.7)(allp<0.05).Meanarterialpressuredecreasedsignificantlyafterpositionchange, andremaineddecreased,comparedtoT1.Theoverallanalysisofpatientstateindexvalues (T1---T4)showednosignificantchange;however,comparingonlyT1andT2resultedina stat-icallysignificantdecreaseinpatientstateindex.Therewasasignificantdecreaseincerebral bloodflowafterbeachchairposition.
Conclusion:Beachchair positionwas associatedwithadecreaseincerebralbloodflowand patientstateindexvalues.Patientstateindexwasaffectedbythegravitationalchangeofthe cerebralbloodflow;however,bothfactorswerenotdirectlycorrelatedtoeachother.Moreover, thedecreaseinpatientstateindexvaluewastransientandreturnedtonormalvalueswithin 20min.
©2015SociedadeBrasileiradeAnestesiologia.PublishedbyElsevierEditoraLtda.Thisisan openaccessarticleundertheCCBY-NC-NDlicense( http://creativecommons.org/licenses/by-nc-nd/4.0/).
∗Correspondingauthor.
E-mail:mbuget@yahoo.com(M.I.Buget). http://dx.doi.org/10.1016/j.bjane.2015.02.002
PALAVRAS-CHAVE
PatientStateIndex; Cerebral;
Fluxosanguíneo
cerebral;
Posic¸ãodecadeira
depraia
PatientStateIndexealterac¸õesdofluxosanguíneocerebraldurante
artroscopiadoombroemposic¸ãodecadeiradepraia
Resumo
Justificativaeobjetivos: Oobjetivodoestudofoidemonstraraspossíveisalterac¸ões hemod-inâmicasedofluxosanguíneocerebral(FSC)empacientesqueforamposicionadosdesupinac¸ão para cadeira depraia (CP)edetectar seamudanc¸a deposic¸ãocausaalguma alterac¸ão na atividadecorticalcomomensuradopelomonitordeEEGcom4canais.
Métodos: Nototal,35pacientesforamincluídos.Antesdainduc¸ão,osvaloresdaPAMedoIEP foramregistrados(T0).Apósaintubac¸ão,ultrassonografiascomDopplerdacarótidainternae artériasvertebraisdospacientesforamavaliadaspara adquirirosvaloresdoFSCapartirda fórmula.Emsupinac¸ão,osvaloresdaPAM,IEPeFSCforamregistrados(T1)eopacientefoi posicionadoemCP.Após5minutos,todasasmensurac¸õesforamrepetidas(T2).Asmensurac¸ões doIEPePAMforamrepetidasapós20(T3)e40minutos(T4).
Resultados: Houveumadiminuic¸ãosignificativaentreT0eT1naFC(80,5±11,6vs.75,9±14,4 bpm),PAM(105,8±21,9vs.78,9±18,4mmHg)eIEP(88,5±8,3vs.30,3±9,7)(p<0,05para todos).APAMdiminuiusignificativamenteapósamudanc¸adeposic¸ãoepermaneceudiminuída emrelac¸ãoaT1.AanáliseglobaldosvaloresdoIEP(T1-T4)nãomostrounenhumamudanc¸a significativa, mas a comparac¸ão de apenas T1 e T2 resultou em reduc¸ão estatisticamente significativadoIEP.Houvereduc¸ãosignificativadoFSCapósoposicionadoemCP.
Conclusão:Oposicionado em CPfoi associadoàdiminuic¸ãodo FSCe dosvalores do IEP.O IEPfoiafetadopelamudanc¸agravitacionaldoFSC;noentanto,ambososfatoresnãoestavam diretamentecorrelacionadosentresi.Alémdisso,adiminuic¸ãodovalordoIEPfoitransitória evoltouaosvaloresnormaisdentrode20minutos.
©2015SociedadeBrasileiradeAnestesiologia.PublicadoporElsevierEditoraLtda.Este ´eum artigo OpenAccess sobumalicenc¸aCCBY-NC-ND( http://creativecommons.org/licenses/by-nc-nd/4.0/).
Introduction
Inshoulderarthroscopysurgeriesbeachchairposition(BCP) is often useddue tocertain advantages1: combined with
‘‘controlledhypotension’’,itprovideseasieranatomic ori-entation and set-up, better visualization of subacromial spaceandglenohumeralstructures,anditisabetterchoice than lateral decubitus position for open surgeries. It also provides optimal upper extremity rotation control,2 and
under normal circumstances many patients are operated in theBCP without any seriousadverse events;3 however,
whenthepatientsarepositionedfromsupinetoBCPunder generalanesthesia,a markedreductionin cardiacoutput, meanarterialpressure(MAP)andcerebral perfusion pres-sure(CPP)canbeencountered.1,2,4
Following its relative recent introduction into the anesthesia practice, ‘‘Monitoring the depth of anesthe-sia’’ (DoA) is nowbecoming an important part of routine anesthesiamonitoring. TheSedlineelectroencephalograph based monitor is one such DoA monitoring options, and is used to monitor the state of the brain by real-time data by processing a 4-channel EEGsignals and providing numericalvaluetermedthePatientStateIndex(PSI).PSIis processedquantitativeEEGindextoevaluatethedegreeof consciousnessduringbothgeneralanesthesiaandconscious sedation.5 Thesensitivityof thePSIindexdependsonthe
neurometrics technology it is using, and it can evaluate both the background EEG and the brain’s response to anesthetic agents.6---8 Some clinical results suggest that
there are differences between DoA monitoring devices
(includingPSI)inevaluationofneurologicaldata.6,9Several
studies have shown that changes in both hemodynamic status and cerebral perfusion can affect the accuracy of DoA measurements.10---12 In a recent study, effects of BCP
onthebispectralindexhavebeeninvestigated;13however,
therelationofBCPandcerebralbloodflow(CBF)andtheir effectsonPSIhavenotbeeninvestigatedbefore.
The hypothesis of this prospectivestudy wasthat BCP withcontrolledhypotensionwouldcauseaparalleldecrease bothinCBFandthePSI-value.Theaimsofthestudywere todemonstratethepossiblehemodynamicchangesandCBF alterationsinpatientswhowerepositionedfromsupineto beachchairposition(primaryoutcome);andtodetectifthe changefromsupinetobeachchairposition(BCP)causesany corticalactivityalterationasmeasuredbythe4channeled sedationmonitor(SedlineTM)(secondaryoutcome).Asa
ter-tiaryoutcomewehaveinvestigatedthetimecourseofPSI andbloodpressure.
Methods
differencesamongthemeanswitha0.05significancelevel (two-tailed).
Informed consentwastaken from35 patientswhohad arthroscopicshouldersurgeryandagreedtojoinourstudy. Patientsbetweenage of18---80without anycarotid steno-sisororthostatichypotensionwereincluded.Patientswith anASA status3, 4or 5 andpatientswithcerebrovascular diseaseswereexcluded.
Allpatientswerepre-hydratedpriortotheirarrivalinto theoperatingroomwith1000ccsalineandpre-medicated with 2mg of midazolam. For postoperative analgesia all patientshadasingleshotinterscaleneblockunderUSG guid-ance.StandardmonitorisationincludedECG,SpO2,arterial pressure,capnography (Draeger ˙InfinityXL,Draeger Medi-cal Inc., 3135 Quarry Road, Telford, PA 18969, USA) and fourchanneledEEGtoevaluatethebrainfunction(Sedline withPSIMasimoCorporation,Irvine,USA).Invasivearterial pressuremonitorisation wasperformed via a 20G arterial cannulainsertedradialarteryonthenon-operated extrem-ity.Thetransduceroftheinvasivearterialmonitorwaskept at the level of heart. Before the induction, MAP and PSI valueswererecorded(T0).
Forallthepatientsanesthesiawasinducedwithfentanyl 1.5g/kg;propofol2mg/kg;rocuronium0.6mg/kg;andall
patientshadtrachealintubation.Inallpatients,anesthesia wasmaintainedwithremifentanilinfusion,50%O2/N2O
mix-tureanddesfluranetokeependtidaldesfluranelevelwas keptas6%.
After the intubation, Doppler USG of the patients’ internal carotid artery (ICA) and vertebral arteries were evaluated. The time averaged mean velocity (VTAM) was measuredforthevessels.Vesseldiameterwasmeasuredon USGandthecross-sectionalareaofeachvesselwas deter-mined with the formula r2. Flow volume is the product
ofVTAMandcross-sectionalarea.Thesumoftheflow vol-umes of ICA and vertebral artery was equal to the total CBF.14
Insupineposition,MAP,PSIandCBFvalueswererecorded (T1), and the patient was positioned to BCP. Both in supine and BCP, remifentanil infusion was started with 0.05/kg/minandwastitrated tomaintain MAPbetween
50and75mmHg.After5minfollowingpositioningto beach-chair, all measurements were repeated (T2). Patients, in whoma50%ormorereductioninCBFwasobserved,were excludedfromthestudy.Theoperationstartedimmediately afterT2recordings. Throughouttheoperation,inspiratory desfluraneconcentrationwasadjustedaccordingtothe end-tidalconcentration(i.e.not toPSI).MAPwaskeptat the valueinT2viaadjustmentintheratioofremifentanil infu-sion.IfMAPdecreased below50mmHg,a bolusof 500mL of colloidal solution and/or 1mg ephedrine IVwasgiven; ifMAPincreasedabove75mmHg(with noincreaseinPSI), theinfusionrateofremifentanilwasincreased.Violationof MAPaboveandbelowthelimits(50---75mmHg)wasnotan exclusioncriterion,unlessitwaspossibletomanageitback totherange.
Measurements of PSI and MAP were repeated after 20 (T3),and 40 (T4)min. Because of application difficulties, CBFwasnotmeasuredduringtheoperation(i.e.T3andT4). Attheendoftheoperation,patientswerepositionedback tosupine;extubationwasperformedregardingthePSIvalue andclinicalevaluation.AllpatientswerekeptinthePACU
Table1 Demographiccharacteristicsofthepatients.
Gender(F/M) 24/11
(68.6%/31.4%)
Age 48.4±12
Bodyweight(kg) 78.3±11.41
Height(cm) 169.71±13.09
for30min;aftertheassessmentofmodified-AldreteScore
andVAS,thepatientsweredischargedtotheward.
Statistical
analysis
SPSS.20softwarewasusedfortheanalysis.Pairedsamplest
-testsformeanswereusedforthepreinduction(T1)andpost
induction(T1)valuesofallmeasurements.Tocomparedata
(formeanarterialpressure(MAP),heartrate(HR),andPSI
afterthe induction(T1---T4),repeatedmeasuresof ANOVA
testwereperformed withTukey-testasposthoc;whereas
changesincerebralbloodflow(CBF)(T1vs.T2)were
eval-uatedwithpaired t-test. The p-value <0.05 wasnotedas
significant. Correlation between changes in PSI, MAP and
CBF after position change (i.e. between T1 and T2) was
examinedwithlinearregressiontests.
Results
Thirty-five patients were included in the study. Patient
demographicsareshowninTable1.Noneofthepatientswas
excludedfromthestudyduetoanyintraoperativeexclusion criteria.
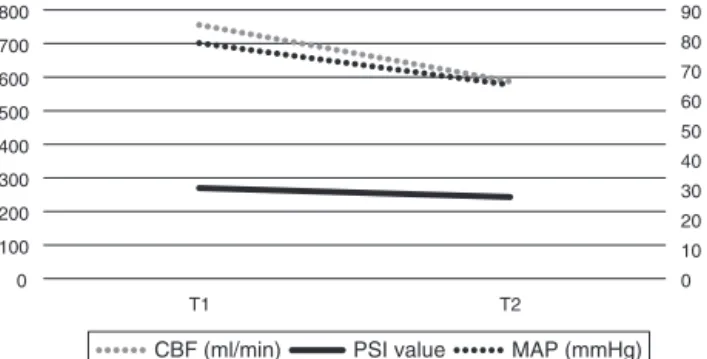
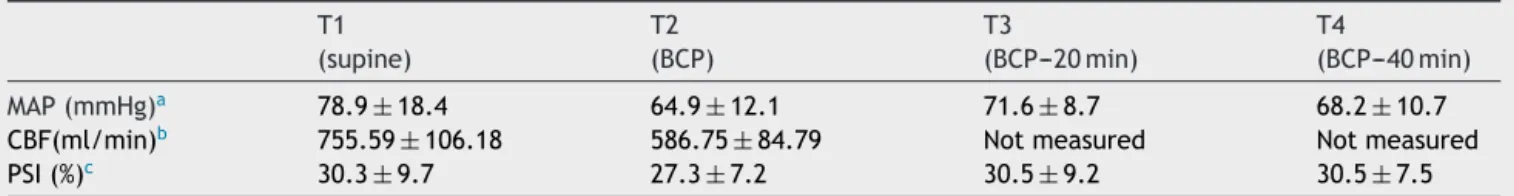
TherewasasignificantdecreasebetweenT0andT1inHR (80.5±11.6 vs. 75.9±14.4beats/min), MAP (105.8±21.9 vs. 78.9±18.4mmHg) and PSI (88.5±8.3 vs. 30.3±9.7) (allp<0.05).Results ofT1toT4canbefoundin Table2. Meanarterialpressuredecreasedsignificantlyafterposition change toBCP, andremaineddecreased, comparedtoT1. TheoverallanalysisofPSI-values(T1---T4)showedno signifi-cantchange;however,comparingonlyT1andT2(immediate change fromsupinetoBCP)resultedina statically signifi-cantdecreaseinPSI(p-value<0.05).Therewasasignificant decreaseinCBFafterBCP(Figs.1and2).
800 700 600 500 400 300 200 100 0
T1
CBF (ml/min) PSI value
90 80 70 60 50 40 30 20 10 0 T2
MAP (mmHg)
Table2 TimecourseofMAP,CBFandPSI(MAP,meanarterialpressure;CBF,cerebralbloodflow).T1,supine;T2,immediate afterbeachchairposition;T3,20minafterBCP;T4,40minafterBCP.
T1 (supine)
T2 (BCP)
T3
(BCP---20min)
T4
(BCP---40min)
MAP(mmHg)a 78.9±18.4 64.9±12.1 71.6±8.7 68.2±10.7
CBF(ml/min)b 755.59±106.18 586.75±84.79 Notmeasured Notmeasured
PSI(%)c 30.3±9.7 27.3±7.2 30.5±9.2 30.5±7.5
a p>0.0001;whereT1vsT2:p<0.001;T1vsT3:p<0.5;T1vsT4:p<0.01. b p<0.001.
c NosignificantchangewithrepeatedmeasuresofANOVA;p=0.0142whencomparedonlyT1vsT2.
90 78.9
80 70 60 50
40 30.3428
30 20 10 0
T1
64.9
27.31
T2
PSI value
71.6
30.514285
T3
MAP (mmHg)
Figure2 Timecourse ofPSI-value:T1, supine; T2, beach-chairposition(BCP);T3,BCPafter20min;T4,BCPafter40min. NotethatthereisnosignificantchangeinPSIvalues,whenall measurementsarecompared.IfonlyT1vs.T2arecompared, thereisasignificantdecrease(p=0.0142).
None of the changes in the hemodynamic parameters studiedcorrelatedwithchangesinPSIvalues.Similarly,the changesincerebralbloodflowdidnotinteractwithchanges in level of sedation (PSI) (Linear Regressions regarding changesT1---T0:MAPvs.PSI(R-squared:0.05);CBFvs.PSI (R-squared:0.02);BPvs.CBF(R-squared:0.07);forall cor-relations:p>0.05).
Discussion
Inthisstudywehaveshownthatchangingthepositionfrom supinetobeach-chairwasassociatedwithadecreaseinMAP, CBFand alsoPSI-levels; whereby the decrease in PSIwas temporaryforonly20min,theMAPvaluesweredecreased throughouttheprocess.
ItshouldbenotedthatadecreaseinMAPis‘‘warranted’’ to achieve a decrease in bleeding during the operation; therefore it was not a ‘‘variable’’ of the protocol of our study,butitwaskeptwithinafixedmarginwithremifentanil infusion. BCP offers further advantages to a ‘‘controlled hypotension’’,suchasanatomicalpositioning,reduceduse ofarmtractionanddecreasedriskofbrachialplexusinjury. The majority of the studies investigating the changes in bloodpressurehavefoundadecreaseassociatedwith posi-tion change, probably due to gravitational reasons. The standard practice is to keep the MAP within limits after changingtoBCPtoachievetheadditiveadvantagesofBCP and controlled hypotension. We have shown that after a transient decrease in PSI parallel to MAP, the PSI values returnedtoinitialvalues.
CerebralbloodflowcanaffectthePSIvaluebothdirectly orindirectlyoverMAP.StudiesregardingtheCBFalterations
have reported contradictory results. McCulloch et al.15
foundthatBCPwasassociatedwithadecreaseinCBF,whilst Soedingetal.14didnotobserveanychange.Oneofthe
pri-mary aimsof this study was todemonstrate the possible hemodynamicchangesandcerebral bloodflow alterations inpatientswhowerepositionedfromsupinetobeachchair position;wehaveshownthatbothbloodpressureandCBF decreasedsignificantlyafterpositionchange.Ourresultsare similartotheresultsfromtheMcCuloghstudy,atleastfor theinitialperiodofBCP.15
Inarecentstudy,Leeetal.13haveexaminedthe
relation-shipbetweenbispectralindex,anotherDoAmonitor (BIS), withBCP. TheyfoundadecreaseinBISafterchangingthe positiontoBCP. However,inthat studythechange inCBF wasnot investigated; moreover, the results were limited to15min afterBCP. In ourstudy,we couldshow thatthe decreaseinPSIwasparalleltodecreasesinMAPandalsoCBF. Inaddition,thisdecreasewastransientfor20min,although thedecreaseinMAPpersisted.
Several studies have shown the reliability of differ-ent DoA monitors.16---19 Obviously, there are some factors
affectingthe sensitivityandspecificity ofthesemonitors. Kawanishietal.haveshownthatBCPcanhavesomeimpact onBispectral Index,i.e. BCP cancause a decreasein BIS values.20 Kawanishi compared patients in supine position
andBCP,andinterestingly,thedifferenceinBISvalueswere observedonlyasasuccessionoftheposition,whereas end-tidalanestheticgasconcentrationandmeanbloodpressure didnotsignificantlydifferbetweenthegroupsconsistently. Itcanbeassumed thatthedecrease inCBFasaresultof gravitationalchangewouldalsocauseachangeincortical activitiesofthepatient.Ourstudyconfirmstheinformation ofthedecreaseinDoAmonitoringvaluealsofortheSedline monitor,andaddssomeimportantinformationtothisissue. First,althoughboththeBCPandthecontrolled hypoten-sionhavecontinued duringthe operation,PSIvalue hasa trendtowardthevaluesinsupinepositionandhasreached themwithinapproximately20min.Thiscanbeexplainedby ‘‘autoregulation’’ofthecerebralperfusion.Indeed,there wasalsoadecreaseinCBFimmediately aftertheposition change.Unfortunately,it wasnotpossibletomeasurethe CBFduringtheoperation.Itcanbeassumedthatthe cere-bralblood flowincreased toinitialvaluesagain, although thebloodpressureremainedlow.
(i.e.corticalactivities).Thisresultconcludesthatalthough PSIcanbeaffectedbythepositionchangetobeach-chair; clearly,itisstillaDoAmonitorandisnotsuggestedtobea monitorofperfusion.
Some case reports have shown complications of BCP regardingcerebralischemia.PohlandCullenreportedfour casesof ischemic brainand spinal cordinjury,and Bhatti reported visual loss, and external opthalmoplegia after shouldersurgeries.21,22Theauthorsofthosestudiesassumed
thatthesecomplicationswereassociatedmostlywith pos-turalhypotensionandcerebralhypoperfusion.Fortunately, thefrequencyofthesecomplicationsisratherlowinthe lit-erature;evenlowerinpatientswhohadnopreviousfindings thatcouldaffectthecerebralperfusion(e.g.carotid steno-sis,atherosclerosis,etc.).Asamatteroffact,inourstudy, onlypatientswithoutanypreviousfindingsaffectingtheCBF wereincluded.ItcanbespeculatedthattheincreaseofPSI within20minafterBCFis,(insomespecificrange)an indica-toroftheautoregulationofCBF.Inpatientswithhigherrisk ofcerebralhypoperfusion,theeffectsofCBFpluscontrolled hypotensioncanvary.
The most important limitationof the study is thatthe CBFcouldnotbemeasuredduringtheoperation;thiswas notpossiblebecauseofthecloseproximityoftheoperation area;and even if a measurement were possible, its reli-abilitywouldbequestionable.However,thetimecourseof theCBFwasnotthehypothesisofthestudy,norwasitthe secondaryoutcome.
Similarly, cerebral oximetry has not been performed, becausethedealofthestudywasregardingtheperfusion andnottheoxygenationofthecortex.Patientswitha pos-sibleimpairmentofcerebralperfusionandperhapsalsoof cerebralautoregulationhavebeenexcludedfromthestudy. Therefore,thefindingsandalsothetimecourseinthisgroup ofpatientsshouldbeexaminedinfurtherstudies.
Inconclusion,ithasbeen shownthatbeachchair posi-tionwasassociatedwithadecreaseinbothcerebralblood flowandPSIvalue.PSI(i.e.corticalelectroencephalic activ-ities)wasaffectedbythegravitationalchangeoftheCBF; however,both factors arenot directly correlated toeach other.Moreover,thedecreaseinPSIvaluewastransientand returnedtonormalvalueswithin20min.
Conflicts
of
interest
Theauthorsdeclarenoconflictsofinterest.
Acknowledgements
WewouldliketothankMasimoCorporationforloaningthe Sedlinemonitorandsensorusedduringthestudy.
References
1.Jeong H, Jeong S, Lim HJ, et al. Cerebral oxygen satu-ration measured by near-infrared spectroscopy and jugular venous bulb oxygen saturation during arthroscopic shoul-dersurgeryinbeachchairpositionundersevoflurane-nitrous oxide or propofol-remifentanil anesthesia. Anesthesiology. 2012;116:1047---56.
2.ProvencherMT,SolomonDJ,GastonTM.Positioningforshoulder arthroscopybeachchair and lateraldecubitus. In: DavidTS, AndrewsJR,editors.Arthroscopictechniquesoftheshoulder: avisualguide.SLACKInc.;2008.p.1---14[chapter1]. 3.KohJL,LevinSD,ChehabEL,etal.NeerAward2012:cerebral
oxygenationinthebeachchairposition:aprospectivestudyon theeffectofgeneralanesthesiacomparedwithregional anes-thesiaandsedation.JShoulderElbowSurg.2013;22:1325---31. 4.BuhreW,WeylandA,BuhreK,etal.Effectsofthesitting
posi-tiononthedistributionofbloodvolumeinpatientsundergoing neurosurgicalprocedures.BrJAnaesth.2000;84:354---7. 5.Chen X, Tang J, White PF, et al. A comparison of patient
stateindexandbispectralindexvaluesduringtheperioperative period.AnesthAnalg.2002;95:1669---74.
6.DroverDR,LemmensHJ,PierceET,etal.Patientstateindex titrationofdeliveryandrecoveryfrompropofol,alfentanil,and nitrousoxideanesthesia.Anesthesiology.2002;97:82---9. 7.JohnER,PrichepLS,FriedmanJ,etal.Neurometrics:computer
assisteddifferentialdiagnosis ofbraindysfunctions.Science. 1988;239:162---9.
8.ChabotRJ,GuginoLD,AglioLS,etal.QEEGand neuropsycholo-gicalprofilesofpatientsaftercardiopulmonarybypasssurgical procedures.ClinEEG.1997;28:98---105.
9.White PF,Tang J, MaH, et al.Is thepatient stateanalyzer withthePSArray2acost-effectivealternativetothebispectral indexmonitorduringtheperioperativeperiod?AnesthAnalg. 2004;99:1429---35.
10.Cavus E, Meybohm P, Doerges V, et al. Effects of cerebral hypoperfusion on bispectral index: a randomised, controlled animalexperiment duringhaemorrhagicshock.Resuscitation. 2010;81:1183---9.
11.LauwickS,EnglishM,HemmerlingTM.Anunusualcaseof cere-bral hypoperfusion detected bybispectral index monitoring. CanJAnaesth.2007;54:680---1.
12.MorimotoY,MondenY,OhtakeK,etal.Thedetectioncerebral hypoperfusionwithbispectralindexmonitoringduringgeneral anesthesia.AnesthAnalg.2005;100:158---61.
13.LeeSW,ChoiSE,HanJH,etal.Effectofbeachchairposition onbispectralindexvaluesduringarthroscopicshouldersurgery. KoreanJAnesthesiol.2014;67:235---9.
14.Soeding PF, Wang J, Hoy G, et al. The effectof thesitting uprightor ‘beachchair’ position on cerebralbloodflow dur-inganaesthesiaforshouldersurgery.AnaesthIntensive Care. 2011;39:440---8.
15.McCullochTJ,LiyanagamaK,PetchellJ.Relativehypotension inthebeach-chairposition:effectsonmiddlecerebralartery bloodvelocity.AnaesthIntensiveCare.2010;38:486---91. 16.Nguyen NK, Lenkovsky F,Joshi GP. Patient state index
dur-ing a cardiac arrest in the operating room. Anesth Analg. 2005;100:155---7.
17.JiangY,QiaoB,WuL,etal.ApplicationofNarcotrendTMmonitor
forevaluationofdepthofanesthesiaininfantsundergoing car-diacsurgery:aprospectivecontrolstudy.RevBrasAnestesiol. 2013;63:273---8.
18.SpringmanSR,AndreiAC,WillmannK,etal.Acomparisonof SNAPIIandbispectralindexmonitoringinpatientsundergoing sedation.Anaesthesia.2010;65:815---9.
19.Soehle M,Kuech M, Grube M, et al. Patient state index vs. bispectralindex asmeasures oftheelectroencephalographic effectsofpropofol.BrJAnaesth.2010;105:172---8.
20.KawanishiS,HamanamiK,TakahashiT,etal.Impactofbeach chairpositiononthevalueofbispectralindexduringgeneral anesthesia.Masui.2012;61:820---5.
21.PohlA, CullenDJ.Cerebralischemiaduringshouldersurgery in the upright position: a case series. J Clin Anesth. 2005;17:463---9.