www.revportcardiol.org
Revista
Portuguesa
de
Cardiologia
Portuguese
Journal
of
Cardiology
ORIGINAL
ARTICLE
Congenital
heart
disease
in
adults:
Assessmentof
functional
capacity
using
cardiopulmonary
exercise
testing
Sílvia
Aguiar
Rosa
a,∗,
Ana
Agapito
a,
Rui
M.
Soares
a,
Lídia
Sousa
a,
José
Alberto
Oliveira
a,
Ana
Abreu
a,
Ana
Sofia
Silva
a,
Sandra
Alves
a,
Helena
Aidos
b,
Fátima
F.
Pinto
c,
Rui
Cruz
Ferreira
aaCardiologyDepartment,SantaMartaHospital,Lisbon,Portugal
bInstitutodeTelecomunicac¸ões,InstitutoSuperiorTécnico,PortugalMinalytics,AdvancedSolutionsforDataMiningand
Analytics,Lisbon,Portugal
cPaediatricCardiologyDepartment,SantaMartaHospital,Lisbon,Portugal
Received18January2017;accepted24September2017
KEYWORDS Adultcongenital heartdisease; Functionalcapacity; Cardiopulmonary exercisetesting Abstract
Aim: Theaimofthestudywastocomparefunctionalcapacityindifferenttypesofcongenital
heartdisease(CHD),asassessedbycardiopulmonaryexercisetesting(CPET).
Methods:AretrospectiveanalysiswasperformedofadultpatientswithCHDwhohad
under-goneCPETinasingletertiarycenter.DiagnosesweredividedintorepairedtetralogyofFallot,
transpositionofthegreatarteries(TGA)afterSenningorMustardproceduresorcongenitally
correctedTGA,complexdefects,shunts,leftheartvalvediseaseandrightventricularoutflow
tractobstruction.
Results:We analyzed 154 CPET cases. There were significant differences between groups,
withthelowest peakoxygenconsumption(VO2)valuesseeninpatientswith cardiacshunts
(39%withEisenmengerphysiology)(17.2±7.1ml/kg/min,comparedto26.2±7.0ml/kg/minin
tetralogyofFallotpatients;p<0.001),thelowestpercentageofpredictedpeakVO2 in
com-plexheartdefects(50.1±13.0%)andthehighestminuteventilation/carbondioxideproduction
slope incardiacshunts (38.4±13.4). Chronotropism was impaired inpatients with complex
defects.Eisenmengersyndrome(n=17)wasassociatedwiththelowestpeakVO2(16.9±4.8vs.
23.6±7.8ml/kg/min;p=0.001)andthehighestminuteventilation/carbondioxideproduction
slope(44.8±14.7vs.31.0±8.5;p=0.002).Age, cyanosis,CPETduration,peaksystolicblood
pressure,timetoanaerobicthresholdandheartrateatanaerobicthresholdwerepredictorsof
thecombinedoutcomeofall-causemortalityandhospitalizationforcardiaccause.
∗Correspondingauthor.
E-mailaddress:silviaguiarosa@gmail.com(S.AguiarRosa).
https://doi.org/10.1016/j.repc.2017.09.020
Conclusion:AcrossthespectrumofCHD,cardiacshunts(particularlyinthosewithEisenmenger
syndrome)andcomplexdefectswereassociatedwithlowerfunctionalcapacityandattenuated
chronotropicresponsetoexercise.
©2018SociedadePortuguesadeCardiologia.PublishedbyElsevier Espa˜na, S.L.U.Allrights
reserved. PALAVRAS-CHAVE Cardiopatias congénitasdoadulto; Capacidade funcional; Provadeesforc¸o cardiorrespiratória
Cardiopatiacongénitaemadultos:avaliac¸ãodacapacidadefuncionalporprovade esforc¸ocardiorrespiratória
Resumo
Objetivo:Compararacapacidadefuncionalnascardiopatiascongénitas,avaliadaporprovade
esforc¸ocardiorrespiratória.
Métodos: Análiserestrospetivadosdoentesadultoscomcardiopatiacongénita,submetidosa
provadeesforc¸ocardiorrespiratória.OsdoentesforamdivididosemtetralogiadeFallot
oper-ada,transposic¸ãodegrandesartériasapóscirurgiadeSenning/Mustard,transposic¸ãodegrandes
artérias congenitamentecorrigida, defeitos complexos, shunts,doenc¸a valvular esquerdae
obstruc¸ãodotratodesaídadoventrículodireito.
Resultados: Foramavaliadas154provascardiorrespiratórias.Osvaloresmaisbaixosdeconsumo
de oxigénio no picoforam observados nosdoentes com shunt cardíaco (39%apresentavam
síndromedeEisenmenger)(17,2±7,1ml/kg/min,emcomparac¸ãocom26,2±7,0ml/kg/min
natetralogiadeFallot;p<0,001);ovalormaisbaixodapercentagemdeconsumodeoxigénio
nopicorelativamenteaoprevistofoiobservadonosdefeitoscomplexos(50,1±13,0%)eomaior
valorderampaventilac¸ãominuto/produc¸ãodedióxidodecarbononosshuntscardíacos(38,4
±13,4).Ocronotropismofoimenoseficaznosdoentescomdefeitoscomplexos.Asíndromede
Eisenmenger(n=17)associou-seaovalormaisbaixodeconsumodeoxigénionopico(16,9±4,8
versus23,6±7,8ml/kg/min;p=0,001)eaomaiorvalorderampaventilac¸ãominuto/produc¸ão
dedióxidodecarbono(44,8±14,7versus31,0±8,5;p=0,002).Idade,cianose,durac¸ãoda
prova,pressãoarterialsistólicanopico,tempoparaolimiaranaeróbioefrequênciacardíacano
limiaranaeróbioforampreditoresdooutcomecombinadocommortalidadedetodasascausas
ehospitalizac¸ãodecausacardíaca.
Conclusão:Osshuntscardíacos(particularmentecomsíndromedeEisenmenger)eosdefeitos
complexosassociaram-seamenorcapacidadefuncionalerespostacronotrópicaatenuadaao
exercício.
©2018SociedadePortuguesadeCardiologia.PublicadoporElsevierEspa˜na,S.L.U.Todosos
direitosreservados.
Introduction
Nowadaysmostpatientswithcongenitalheartdisease(CHD) areexpectedtoreachadulthood.Becauseexercise intoler-ancehasbeendocumentedatallagesofCHD,thesepatients needclosefollow-upandanobjectiveassessmentof func-tionalcapacity.1,2
Duetolong-termadaption,themajorityofadultpatients
withCHD self-reporttheir exercisecapacitystatusas
sat-isfactory, even in the presence of significantly depressed
functionalstatus.Cardiopulmonaryexercisetesting(CPET)
is an accurate method for quantitative assessment of
exercisecapacity, including assessment of aerobic
capac-ity,chronotropicresponseandarrhythmias.1,3---6Quantifying
exercise capacity by measuring parameters such as peak
oxygen consumption (VO2) is an established technique in
the management of patients with chronic heart failure.
However, in adult CHD patients its role has been much
less studied, and interpretation of test results remains a
challenge. Previous studies have demonstrated that CPET
datahaveanimportantinfluenceonthetreatmentapproach
inCHD,includingindicationforcardiactransplantation,and
onprognosis.2,7,8
Theaimofthepresentstudywastwofold:toassessand
comparefunctionalcapacityindifferentCHDgroups,
mea-sured objectively by CPET, and to investigate a possible
associationbetweenCPETparametersandoutcome.
Methods
Studydesign
Aretrospectiveanalysiswasperformedofconsecutiveadult
patientswithCHDwhounderwentCPETforassessment of
functionalcapacity.Thedatawerecollectedinasingle
Thestudypopulationwasdividedaccordingtodiagnosis
or pathophysiological status: repaired tetralogy of Fallot,
transposition of the greatarteries (TGA)after Senning or
Mustard proceduresand congenitally corrected TGA(both
witha rightventriclefunctioningasasystemicventricle),
complexheartdefects(univentricularheart,Fontansurgery,
truncusarteriosus),shunts (atrial,ventricularor arterial),
leftheartvalvediseasewithstenosisorregurgitation
(bicus-pidaortic valve, subaorticstenosis), and right ventricular
outflowtractobstruction(RVOTO).
CPET was performed in patients with some degree of
effort intolerance,complexdefectsor significant residual
lesions.
The combined outcome of hospitalization for cardiac
causeandall-causemortalitywasanalyzed.
Cardiopulmonaryexercisetesting
Maximal symptom-limited treadmill CPET was performed
usingthemodified Bruceprotocol.CPETandtherecovery
periodweremonitoredwithcontinuous12-lead
electrocar-diogram,bloodpressurecuff,saturation probeanda face
masktomeasurerespiratorygases.Bloodpressurewas
mea-suredat rest,at each stage,at peakexercise and at the
first,thirdand sixthminuteof therecoveryphase.
Respi-ratorygaseswereanalyzed usingan Innocor® gas analyzer
and VO2, carbon dioxide production andventilation were
measuredonabreath-by-breathbasis.
Patientswereencouragedtoperformexerciseuntilthe
carbon dioxide production/oxygen consumption ratio was
1.15orhigher.
PeakVO2adjustedforbodymass,orforfat-freemassin
obesepatients(bodymassindex>30kg/m2),wasanalyzed,
aswellasthepercentageofpredictedpeakVO2forageand
genderaccordingtotheWasserman/Hansenequation.The
minute ventilation (VE)/carbon dioxideproduction (VCO2)
slopewascalculatedbyautomaticlinearregressionwith
val-uesobtainedduringCPET.TheratiobetweenVE/VCO2slope
andpeakVO2wasalsocalculated.Peakcirculatorypower
wasdetermined by multiplyingpeak VO2 by peaksystolic
bloodpressure.Bothbaselineandpeakoxygensaturations
werealsocollected.
The chronotropic index was calculated as(peak heart
rate/resting heartrate)/(220-age/resting heart rate),and
considerednormalforvaluesbetween0.8and1.3.9
Statisticalanalysis
ThestatisticalanalysiswasperformedusingSPSSStatistics
version22(IBMSPSS,Chicago,IL).Continuousvariableswere
expressedasmean±standarddeviation.CPETparameters
werecomparedbetweenstudygroupsusingone-way
analy-sisofvariancebetweenmeanvaluesorthenon-parametric
Kruskal-Wallistest,andmultiplecomparisonsbetweenthe
study groups were performed with an appropriate
post-hoc test. Pearson’s chi-square or Fisher’s exact test was
applied for categorical variables. The Student’s t test or
the Wilcoxon-Mann-Whitney test for continuous variables
wasusedforgendercomparisons.Pearson’scorrelationwas
used to estimate correlation between continuous
varia-bles.Theassociation betweenvariablesandthecombined
outcome was assessed with univariate Cox proportional
hazardsanalysis(forwardstepwise).
Results
CPET data were analyzed from 154 patients, mean age
34.8±8.8years,55.8% male. The most frequent diagnosis
wascorrectedtetralogyofFallot(36%),followedbycomplex
defects(21%)(Table1).
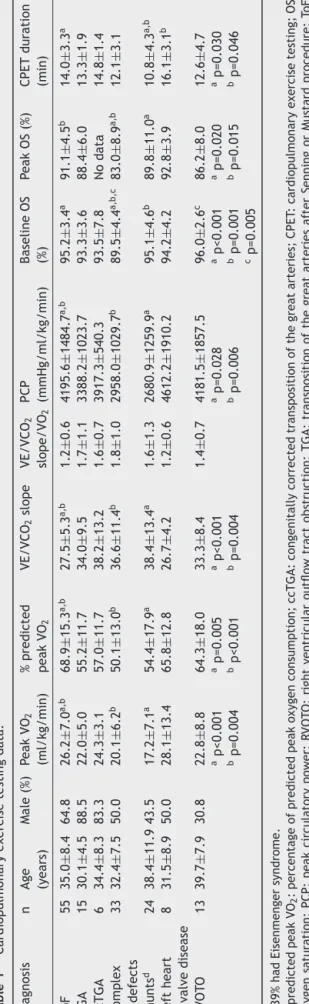
There were significant differences in CPET
parame-ters between the study groups. As shown in Table 1, the
lowest values for peak VO2 were seen in patients with
cardiac shunts, related to the fact that 39% of these
patientshadEisenmengersyndrome(17.2±7.1ml/kg/min,
compared to 26.2±7.0ml/kg/min in tetralogy of Fallot
patients;p<0.001).PeakVO2differedsignificantlybetween
genders only in the complex heart defect group (males
23.3±6.1ml/kg/min vs. females 16.9±4.6ml/kg/min;
p<0.001).Percentage of predicted peak VO2 adjusted for
age and gender was lower in the complex heart defect
group(50.1±13.0%)comparedtotheothergroups.
Patientswithcardiacshuntsandcongenitally corrected
TGAhadhigherVE/VCO2 slope(38.4±13.4and38.2±13.2,
respectively), for which the lowest value was in left
heartvalvedisease.Asignificant differencebetween
gen-ders was observed only in the complex defects group
(males32.3±12.4vs.females41.3±8.3;p<0.012).Theratio
betweenVE/VCO2slopeandpeakVO2washigherincomplex
defects.Peakcirculatorypowerwaslowerinpatientswith
shuntsandcomplexdefects.
Peakoxygensaturationbelow90% wasseen inpatients
withRVOTO,TGAandshunts,anditwasparticularlylowin
complexdefects(83.0±8.9%).
Chronotropism was impaired in patients with
com-plexdefects, among whom 71.9% presented chronotropic
incompetence,demonstratedbyachronotropicindex<0.8
(Table2).
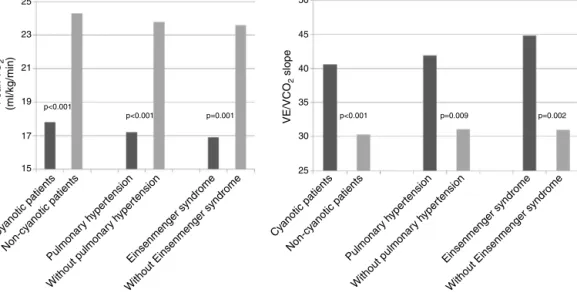
Analyzing the overall population, cyanotic patients
(n=33) presented significantly lower peak VO2 and higher
VE/VCO2 slope than non-cyanotic patients (17.8±5.4 vs.
24.3±7.9ml/kg/min;p<0.001and40.6±13.0vs.30.3±8.0;
p<0.001,respectively).Patientswithpulmonary
hyperten-sion (n=23) also presented lower peak VO2 (17.2±5.9 vs.
23.8±7.8ml/kg/min; p<0.001) and higher VE/VCO2 slope
(41.9±14.9vs.31.1±8.5;p=0.009).Eisenmengersyndrome
(n=17)wasassociatedwithevenlowerpeakVO2(16.9±4.8
vs.23.6±7.8ml/kg/min;p=0.001)andhigherVE/VCO2slope
(44.8±14.7vs.31.0±8.5;p=0.002)(Figure1).
TGA patients (after Mustard or Senning surgery)
pre-sented a negative linear correlation between time from
interventiontoCPETandpeakVO2(r=-0.564;p=0.070)and
peakcirculatorypower(r=-0.632;p=0.037),andapositive
linearPearsoncorrelationbetweentimefromintervention
toCPETandVE/VCO2slope(r=0.554;p=0.122)(Figure2).
In the overall population, 18.2% of patients (n=28)
reacheda carbon dioxideproduction/oxygen consumption
ratioof1.15orhigher.
Duringa mean follow-upof 31.9 months (minimumsix
months;maximum 79 months), the combinedoutcome of
all-causemortalityandhospitalizationforcardiaccausewas
T able 1 Cardiopulmonary exercise testing data. Diagnosis n Age (years) Male (%) P eak VO 2 (ml/kg/min) % predicted peak VO 2 VE/VCO 2 slope VE/VCO 2 slope/VO 2 PCP (mmHg/ml/kg/min) Baseline OS (%) P eak OS (%) CPET duration (min) To F 5 5 35.0 ± 8.4 64.8 26.2 ± 7.0 a,b 68.9 ± 15.3 a,b 27.5 ± 5.3 a,b 1.2 ± 0.6 4195.6 ± 1484.7 a,b 95.2 ± 3.4 a 91.1 ± 4.5 b 14.0 ± 3.3 a TGA 15 30.1 ± 4.5 88.5 22.0 ± 5.0 55.2 ± 11.7 34.0 ± 9.5 1.7 ± 1.1 3388.2 ± 1023.7 93.3 ± 3.6 88.4 ± 6.0 13.3 ± 1.9 ccTGA 6 34.4 ± 8.3 83.3 24.3 ± 3.1 57.0 ± 11.7 38.2 ± 13.2 1.6 ± 0.7 3917.3 ± 540.3 93.5 ± 7.8 No data 14.8 ± 1.4 Complex defects 33 32.4 ± 7.5 50.0 20.1 ± 6.2 b 50.1 ± 13.0 b 36.6 ± 11.4 b 1.8 ± 1.0 2958.0 ± 1029.7 b 89.5 ± 4.4 a,b,c 83.0 ± 8.9 a,b 12.1 ± 3.1 Shunts d 24 38.4 ± 11.9 43.5 17.2 ± 7.1 a 54.4 ± 17.9 a 38.4 ± 13.4 a 1.6 ± 1.3 2680.9 ± 1259.9 a 95.1 ± 4.6 b 89.8 ± 11.0 a 10.8 ± 4.3 a,b Left heart valve disease 8 31.5 ± 8.9 50.0 28.1 ± 13.4 65.8 ± 12.8 26.7 ± 4.2 1.2 ± 0.6 4612.2 ± 1910.2 94.2 ± 4.2 92.8 ± 3.9 16.1 ± 3.1 b R VOT O 13 39.7 ± 7.9 30.8 22.8 ± 8.8 64.3 ± 18.0 33.3 ± 8.4 1.4 ± 0.7 4181.5 ± 1857.5 96.0 ± 2.6 c 86.2 ± 8.0 12.6 ± 4.7 ap<0.001 bp=0.004 ap=0.005 bp<0.001 ap<0.001 b p=0.004 ap=0.028 bp=0.006 ap<0.001 b p=0.001 cp=0.005 ap=0.020 bp=0.015 ap=0.030 bp=0.046 d 39% had Eisenmenger syndrome. % predicted peak VO 2 : percentage of predicted peak oxygen consumption; ccTGA: congenitally corrected transposition of the great arteries; CPET : cardiopulmonary exercise testing; OS: oxygen saturation; PCP: peak circulatory power; R VOT O: right ventricular outflow tract obstruction; TGA: transposition of the great arteries after Senning or Mustard procedure; ToF: tetralogy of Fallot; VE/VCO 2 : minute ventilation/carbon dioxide production; VO 2 : oxygen consumption.
Table2 Assessmentofchronostropism.
Diagnosis Peakheart
rate(bpm) Chronotropic index<0.8(%) Patientsunder Beta-blockers (%) ToF 156.7±23.5 46.3 18.5 TGA 151.5±34.8 26.9 3.8 ccTGA 147.0±17.0 66.7 50.0 Complex defects 143.8±29.1 71.9 40.6 Shunts 138.7±23.7 69.9 13.0 Leftheart valve disease 168.5±27.5 37.5 12.5 RVOTO 157.7±23.7 46.2 30.8
ccTGA:congenitallycorrectedtranspositionofthegreat arter-ies; HR: heart rate; RVOTO: right ventricular outflow tract obstruction;TGA:transpositionofthegreatarteriesafter Sen-ningorMustardprocedure;ToF:tetralogyofFallot.
age,cyanosis,CPETduration,peaksystolicbloodpressure, time to anaerobic threshold and heart rate at anaero-bic threshold were predictors of the combined outcome (Table3).PeakVO2wasnotapredictorofthecombined
out-come(hazardratio0.995;confidenceinterval0.949-1.043;
p=0.829).
Discussion
AlthoughanincreasingnumberofCHDpatientsreach
adult-hood,theirexercisecapacityisoftensignificantlyimpaired.
CPETenablesmoredetailedassessmentoffunctional
capac-itybymeasuringrespiratorygases.PeakVO2,whichreflects
VO2intissuesanddependsoncardiacoutput,arterial
oxy-genandtheoxygenextractioncapacityofmuscletissue,is
anaccuratemeasureofexercisecapacity.10
In line with previous research,1,10---13 our study showed
markedlydepressedfunctionalcapacityinCHDpatients,as
shownbythefactthatallstudygroupspresentedpeakVO2
valuesbelow70%ofthosepredicted.Regardlessofthetype
ofCHD,thepeakVO2valuesreachedbythestudypopulation
were substantially lower thanthose expected for healthy
subjectsofthesameageandgender.
Another useful parameter is VE/VCO2 slope, which
expressesventilatoryefficiencyandhasbeen showntobe
anindependentpredictorofoutcome.14Theratiobetween
VE/VCO2 slope and peakVO2 integrates theseparameters
andalsohasprognosticvalue.15Byintegratingthe
hemody-namicvaluesmonitoredinthistestitispossibletocompute
peakcirculatorypower. Alltheseparameterswere
consis-tentlyabnormalinallgroups.
AcrosstheCHDspectrum,patientswithleftheartvalve
disease and repaired tetralogy of Fallotpresented better
exercisecapacity.Ontheotherhand,TGA(afterMustardor
Senningsurgery,orcongenitallycorrected),complexheart
defects and shunts were associated with more severely
impairedfunctionalcapacity.
It should also be noted that 39% of patients with
shunts presented Eisenmenger physiology, which explains
Cyanotic patients P eak V O2 (ml/kg/min) VE/VCO 2 slope Non-cy anotic patients Cyanotic patients Non-cy anotic patients Pulmonar y hyper tension Without pulmonar y hyper tension Pulmonar y hyper tension Without pulmonar y hyper tension Einsenmenger syndrome Without Einsenmenger syndrome
Einsenmenger syndrome Without Einsenmenger syndrome
25 50 45 40 35 30 25 23 21 p<0.001 p<0.001 p=0.001 p<0.001 p=0.009 p=0.002 19 17 15
Figure1 Peakoxygenconsumption(VO2)andminuteventilation/carbondioxideproduction(VE/VCO2)slopeincyanoticpatients
andinpatientswithpulmonaryhypertensionandEisenmengersyndrome.
30,0
A
P eak V O2 VE/VCO 2 slopeB
60,00 50,00 40,00 30,00 20,00 25,0 20,0 15,0 10,0 20,00 25,00 30,00 35,00Time to CPET (years) Time to CPET (years)
40,00 45,00 20,00 25,00 30,00 35,00 40,00 45,00
Figure2 Transpositionofthegreat arteries.(A)Negative linearPearson correlationbetween timefrom MustardorSenning
surgerytoCPETandpeakoxygenconsumption(VO2)(r=-0.564);(B)positivelinearPearsoncorrelationbetweentimefromMustard
orSenningsurgerytoCPETandVE/VCO2slope(r=0.554).
Table3 Predictorsofthecombinedoutcome
(hospitaliza-tionforcardiaccauseandall-causemortality)byunivariate
Coxregression.
Predictors HR 95%CI p
Age 1.065 1.019-1.113 0.005
Cyanosis 3.584 1.094-11.737 0.035
CPETduration 0.907 0.826-0.995 0.040
Peaksystolicblood
pressure 0.982 0.967-0.998 0.029 Timetoanaerobic threshold 0.819 0.717-0.935 0.003 Heartrateat anaerobicthreshold 0.973 0.955-0.993 0.007
CI:confidenceinterval;CPET:cardiopulmonaryexercisetesting; HR:hazardratio.
Irrespective of the baseline defect, cyanosis and pul-monary hypertension were associated with poor exercise
tolerance,particularlywhenthetwowerecombined,which wasassociated with lower peak VO2 and higher VE/VCO2
slope.AccordingtoDilleretal.,2patientswithEisenmenger
physiology have the most severe impairment in exercise
capacity,reflectedinthelowestpeakVO2andthehighest
VE/VCO2slope.
Ourdatademonstratedanegativecorrelation between
time from Mustard or Senning surgery to CPET and peak
VO2 and peak circulatory power, and a positive
correla-tion between time from surgery to exercise testing and
VE/VCO2slope.Thisdeleteriousevolutionandongoing
mor-biditycouldbeexplainedbyprogressivefailureofasystemic
rightventricleandalsobychronotropicincompetence.16
Furthermore, chronotropic response to exercise is an
important determinantof functional capacity, and
dimin-ished heart rate during exercise may contribute to
reductionsinpeakVO2.12,17
Exerciseintolerancehasbeenassociatedwithincreased
riskofhospitalizationandmortality.2,7,18,19However,unlike
VO2 or VE/VCO2 slope andthe combinedoutcome of
hos-pitalizationfor cardiaccauseandall-causemortality.This
couldbeduetothesmallsamplesizeandthe
heterogene-ityofthestudypopulation.Instead,ourdatashowedlower
valuesofCPETduration,peaksystolicbloodpressure,time
toanaerobicthresholdandheartrateatanaerobic
thresh-oldasbenchmarksoflowerfunctionalcapacitycorrelated
withpoorprognosis.OurresultsareinlinewithDilleretal.’s
studyof321Fontanpatients,inwhomchronotropic
capac-itywasstronglyrelatedtosurvival,contrastingwithalack
ofassociationbetweenpeakVO2orratiobetweenVE/VCO2
slopeandsurvivalorcardiactransplantation.8Therelation
betweenchronotropicincompetenceandall-causemortality
inCHDpatientscouldbesecondarytounderlyingautonomic
dysfunction,neurohormonalactivationandarrhythmias.4,7
Wealsoestablishedanassociationbetweencyanosisand
poor outcome, with a 3.6-fold increase in mortality and
hospitalizationcomparedtonon-cyanoticpatients.Similar
datawere reportedbyDimopoulos etal., whoalso
inter-estinglydemonstratedthatinadultCHDtheVE/VCO2slope
isa strong predictorof mortalityonly inpatients without
cyanosis,suggestingthat cyanoticpatients differ
substan-tiallyinpathophysiologicalprocessesandinthesepatients
theprognosticvalueoftheVE/VCO2slopeisweaker.19
Age was also related to worse prognosis in our study,
reflecting progressive impairment in left and/or right
ventricular function, increasing prevalence of pulmonary
hypertensionand occurrence of arrhythmiasin older CHD
patients.
Tothebestofourknowledge,thisisthefirstPortuguese
publicationonCPETinadultCHDpatients.Weconsiderthat
thereportofourinitialexperienceisofinterest,
highlight-ingtheimportanceofCPETinthispopulation.
Study
limitations
ThiswasaretrospectivestudyatatertiaryadultCHDcenter
that reflects daily clinical practice. There was thus
cer-tainlyabiasinpatientselection,favoringmoresymptomatic
patientsandthoseinwhichitisimportantnottorelyonly
onself-reportedfunctionalcapacity.Thiscouldexplainthe
severityseen inthe shuntsubgroup,inwhich therewasa
largeproportionofEisenmengersyndrome.
Thestudypopulationsizeinevitablyreflectsthe
limita-tionsofasingle-centerexperience.ConsideringthatCPETis
extremelyimportantintheassessmentofCHDpatientsand
shouldbeperformedroutinely,infutureweintendtostudy
morepatients,withdifferentclinicalsituations.
Conclusion
Our sample of adult CHD patients who underwent CPET
presentedexerciseintolerance,whichdifferedsignificantly
acrossthespectrumofCHD.Thesedataillustratethemore
severe impairment in functional capacity and attenuated
chronotropicresponsetoexerciseinEisenmengersyndrome
andcomplexdefects.
Inthisstudy,age,cyanosisandworsefunctionalcapacity
were,asexpected,associatedwiththecombinedoutcome
ofall-causemortalityandhospitalizationforcardiaccause.
Increasing the number of patients and the variety of
defectsandperformingserialassessmentsineach patient
willenableustoobtainmorerobustresultsinthefuture.
Conflicts
of
interest
Theauthorshavenoconflictsofinteresttodeclare.
References
1.FredriksenPM,VeldtmanG,HechterS,etal.Aerobiccapacity inadultswithvariouscongenitalheartdiseases.AmJCardiol. 2001Feb1;87:310---4.
2.Diller GP, Dimopoulos K, Okonko D, et al. Exercise intol-erance in adult congenital heart disease: comparative severity, correlates, and prognostic implication. Circulation. 2005;112:828---35.
3.BhattAB,FosterE,KuehlK,etal.AmericanHeartAssociation CouncilonClinicalCardiology.Congenitalheartdiseaseinthe olderadult: a scientificstatement from theAmerican Heart Association.Circulation.2015;131:1884---931.
4.DillerGP,DimopoulosK,OkonkoD,etal.Heartrateresponse duringexercisepredictssurvivalinadultswithcongenitalheart disease.JAmCollCardiol.2006;48:1250---6.
5.TakkenT,BlankAC,HulzebosEH,etal.Cardiopulmonary exer-cisetestingin congenitalheartdisease: equipment and test protocols.NethHeartJ.2009;17:339---44.
6.PriromprintrB,RhodesJ,SilkaMJ,etal.Prevalenceof arrhyth-miasduringexercisestresstestinginpatientswithcongenital heartdiseaseandsevererightventricularconduitdysfunction. AmJCardiol.2014;114:468---72.
7.InuzukaR,DillerGP,BorgiaF,etal.Comprehensiveuseof car-diopulmonaryexercisetestingidentifiesadultswithcongenital heartdiseaseatincreasedmortalityriskinthemediumterm. Circulation.2012;125:250---9.
8.DillerGP,GiardiniA,DimopoulosK,etal.Predictorsof morbid-ityandmortalityincontemporaryFontanpatients:resultsfrom amulticenterstudyincludingcardiopulmonaryexercisetesting in321patients.EurHeartJ.2010;31:3073---83.
9.Wilkoff BL,Corey J,Blackburn G. A mathematicalmodel of cardiac chronotropic response to exercise. J Electrophysiol. 1989;3:176---80.
10.FredriksenPM,TherrienJ,VeldtmanG,etal.Aerobiccapacity inadultswithtetralogyofFallot.CardiolYoung.2002;12:554---9. 11.HechterSJ,WebbG,FredriksenPM,BensonL,etal. Cardiopul-monaryexerciseperformanceinadultsurvivorsoftheMustard procedure.CardiolYoung.2001;11:407---14.
12.FredriksenPM,ChenA,VeldtmanG,etal.Exercisecapacityin adultpatientswithcongenitallycorrectedtranspositionofthe greatarteries.Heart.2001;85:191---5.
13.HarrisonDA,LiuP,WaltersJE,etal.Cardiopulmonaryfunction inadultpatientslateafterFontanrepair.JAmCollCardiol. 1995;26:1016---21.
14.ArenaR,MyersJ,AslamSS,etal.PeakVO2andVE/VCO2slope in patientswith heartfailure: a prognosticcomparison. Am HeartJ.2004;147:354---60.
15.GuazziM,DeVitaS,CardanoP,etal.Normalizationforpeak oxygenuptakeincreasestheprognosticpoweroftheventilatory responsetoexerciseinpatientswithchronicheartfailure.Am HeartJ.2003;146:542---8.
16.KempnyA,DimopoulosK,UebingA,etal.Referencevaluesfor exerciselimitationsamongadultswithcongenitalheartdisease. Relationtoactivitiesofdailylife–singlecentreexperienceand reviewofpublisheddata.EurHeartJ.2012;33:1386---96.
17.Schulze-NeickIM,WesselHU,PaulMH.Heartrateandoxygen uptakeresponsetoexerciseinchildrenwithlowpeakexercise heartrate.EurJPediatr.1992;151:160---6.
18.GiardiniA,HagerA,LammersAE,etal.Ventilatoryefficiency andaerobiccapacitypredictevent-freesurvivalinadultswith atrialrepairforcompletetranspositionofthegreatarteries.J AmCollCardiol.2009;53:1548---55.
19.Dimopoulos K, Okonko DO, Diller GP,et al. Abnormal venti-latory response to exercise in adults with congenital heart diseaserelatestocyanosisand predictssurvival.Circulation. 2006;113:2796---802.